Abstract
Several lines of evidence point to a significant role of neuroinflammation in Parkinson's disease (PD) and other neurodegenerative disorders. In the present study we examined the protective effect of celecoxib, a selective inhibitor of the inducible form of cyclooxygenase (COX-2), on dopamine (DA) cell loss in a rat model of PD. We used the intrastriatal administration of 6-hydroxydopamine (6-OHDA) that induces a retrograde neuronal damage and death, which progresses over weeks. Animals were randomized to receive celecoxib (20 mg/kg/day) or vehicle starting 1 hour before the intrastriatal administration of 6-OHDA. Evaluation was performed in vivo using micro PET and selective radiotracers for DA terminals and microglia. Post mortem analysis included stereological quantification of tyrosine hydroxylase, astrocytes and microglia. 12 days after the 6-OHDA lesion there were no differences in DA cell or fiber loss between groups, although the microglial cell density and activation was markedly reduced in animals receiving celecoxib (p < 0.01). COX-2 inhibition did not reduce the typical astroglial response in the striatum at any stage. Between 12 and 21 days, there was a significant progression of DA cell loss in the vehicle group (from 40 to 65%) that was prevented by celecoxib. Therefore, inhibition of COX-2 by celecoxib appears to be able, either directly or through inhibition of microglia activation to prevent or slow down DA cell degeneration.
Similar content being viewed by others
Background
The role of microglia in the pathogenesis of neurodegenerative disorders is not clear [1]. Increasing evidence suggests that an inflammatory reaction accompanies the pathological processes seen in many neurodegenerative disorders, including Parkinson's disease (PD) [2–4]. Glial activation is part of a defense mechanism to remove debris and pathogens and promote tissue repair. However, inflammatory activation of microglial cells may contribute to the neurodegenerative process through structural invasion and the release of pro-inflammatory cytokines, reactive oxygen species (ROS), nitric oxide (NO) and excitatory amino acids at synapses and cell bodies. In cell culture and animal models, inflammation contributes to neuronal damage, and anti-inflammatory drugs have been shown to provide some neuroprotection in different paradigms [5–7] including PD models [8, 9]. Reactive microglia inhibit neuronal cell respiration via NO and cause neuronal cell death in vitro [10] and in vivo [11]. Interestingly, microglial cell activation by chronic infusion of lipopolysaccharide (LPS) appears to be capable of inducing a selective degeneration of nigral dopamine (DA) neurons [11]. Intranigral injection of LPS, but not of cytokines, induces DA degeneration [11, 12]. LPS induces NO production and release from microglia and also release of pro-inflammatory cytokines such as IL-1β and TNF-α, which may also participate in cytotoxicity [13].
In PD there is evidence of an increase in oxidative and inflammatory nigral environment [2, 14–16]that includes the presence of cyclooxygenase (COX)-immunoreactive activated microglial cells in the substantia nigra (SN) [17], elevated levels of TNF-α and other pro-inflammatory cytokines in the cerebrospinal fluid (CSF) [18, 19]. DA neurons in the SN express TNF-α receptor 1 [3] which may contribute to the selective susceptibility of DA neurons to microglial toxicity. Supporting a role of inflammation in DA degeneration, mice deficient in TNF-α receptors are resistant to selective DA toxins [20]. In PD patients, a polymorphism in the TNF-α gene, leading to high production of TNF-α, was found to be more frequent than in matched healthy controls and to be related to earlier onset of the disease [21]. In addition, the results of a recent epidemiological study suggest that nonsteroidal anti-inflammatory drugs (NSAID) might delay or prevent onset of PD [22]. NSAIDs target p38 mitogen-activated protein kinase (MAPK) in addition to their main target COX [23] and inhibition of p38MAPK phosphorylation blocks NO release from activated microglial cells [24].
Selective COX-2 inhibitors lack the adverse effects of conventional NSAIDs, which inhibit both isoforms of COX (constitutive and inducible). COX-2 is induced by pro-inflammatory stimuli and cytokines [25]. Inhibition of the inducible form (COX-2) accounts largely for the therapeutic (anti-inflammatory) actions of NSAIDs whereas inhibition of the constitutively expressed form (COX-1) is responsible for the gastrointestinal side effects [25].
In this study we used the intrastriatal administration of 6-OHDA in the rat to evaluate the protective effect of selective COX-2 inhibition by celecoxib. Like other toxic and genetic models, this model has limitations, but it provides a time window to test neuroprotective strategies, as DA neurons die retrogradely over the course of several weeks [26–29]. We have previously shown that, in this model, DA cell death is accompanied by microglial cell activation [28].
Methods
6-OHDA lesion model
To produce progressive and selective degeneration of the nigro-striatal DA system, Sprague Dawley rats (200 – 250 g, Charles River, Wilmington, MA) received unilateral intrastriatal stereotaxic injections of 6-OHDA (Sigma, St. Louis, USA) using a 10 μl Hamilton syringe as previously described [28, 30]. Acepromazine (3.3 mg/kg, PromAce, Fort Dodge, IA) and atropine sulfate (0.2 mg/kg, Phoenix Pharmaceuticals, St. Joseph, MO) were given i.m. 10 min before animals were anesthetized with ketamine/xylazine (60 mg/kg, Fort Dodge Animal Health, Fort Dodge, IA and 3 mg/kg, Phoenix, respectively, i.m.). A concentration of 3.0 μg/μl free base 6-OHDA dissolved in 0.2% ascorbic acid/saline (Sigma) was injected into 3 locations (2.5 μl/site, total dose 22.5 μg) in the right striatum over 8 min per site at the following coordinates (calculated from bregma): site 1, AP +1.3, L -2.8, DV -4.5, IB -2.3; site 2, AP +0.2, L -3.0, DV -5.0, IB -2.3; site 3, AP -0.6, L -4.0, DV -5.5, IB -2.3 mm. Rate of injection was 0.5 μl/min, leaving the needle in place for an additional 3 min before withdrawal. Following surgery, animals received 2 injections of buprenorphine (0.032 mg/kg, s.c., Sigma) 10 hours apart as post-operative analgesia. Rats were treated via oral intubation with a COX-2 inhibitor (celecoxib, 20 mg/kg/day, Pharmacia, Skokie, IL), n = 12 or vehicle (0.5 % methyl cellulose aqueous solution, Sigma), n = 13, beginning approximately one hour prior to lesion and continuing once per day for 14 or 21 days. To functionally evaluate the DA lesion, forepaw use was examined using the cylinder test 3 weeks after the striatal lesion. All animals showed a marked asymmetry (~90% of the contacts were made using the ipsilateral paw).
Histological and stereological procedure
Animals were terminally anesthetized by an i.p. injection of sodium pentobarbital (100 mg/kg) and perfused intracardially with heparin saline (0.1% heparin in 0.9% saline; 100 ml/rat) followed by paraformaldehyde (4% in phosphate buffer). The brains were removed and post-fixed for 8 hours in 4% paraformaldehyde solution. Following post-fixation, the brains were equilibrated in 20% sucrose in PBS, sectioned at 40 μm on a freezing microtome, and serially collected in PBS.
All immunohistochemistry was performed on randomly selected series of sections that represented 1/6th of the total brain per primary antibody. Sections were treated for 10 minutes in 3% hydrogen peroxide (Humco, Texarkana, TX), washed 3 times in PBS, and incubated in 2% normal goat serum (NGS) and 0.1 % Triton X-100 for 30 minutes prior to overnight incubation at 4°C with the primary antibody diluted in 2% NGS and 0.1 % Triton X-100. The primary antibodies utilized were rabbit anti-tyrosine hydroxylase (TH) (Pel Freez, Rogers, AK; 1:300), mouse anti-rat CD11b (OX42) (Accurate Chemical & Scientific Corporation, Westbury, NY; 1:100), and rabbit anti-glial fibrillary acidic protein (GFAP) (Dako A/S, Denmark; 1:500). After a 3 × 10 minute rinse in PBS, the sections were incubated in biotinylated goat anti-mouse/rabbit secondary antibody (Vector Laboratories, Burlingame, CA; 1:300) diluted in 2% NGS in PBS at room temperature for 60 min. The sections were rinsed three times in PBS and incubated in streptavidin-biotin complex (Vectastain ABC Kit Elite, Vector Laboratories) for 60 min at room temperature. Following thorough rinsing with PBS, staining was visualized by incubation in 3, 3'-diaminobenzidine solution with nickel enhancement (Vector Laboratories). Controls with omission of the primary antibody were performed on selected sections that verified the specificity of staining. After immunostaining, floating tissue sections were mounted on glass slides and counterstained with cresyl violet before dehydrating, clearing and coverslipping.
Design based stereology was performed on the stained sections using an integrated Axioskop 2 microscope (Carl Zeiss, Thornwood, NY) and Stereo Investigator image capture equipment and software (MicroBrightField, Williston, VT). Quantification of TH fibers was performed utilizing a Cavalieri estimator probe. The quantification of GFAP and CDllb positive cells in separate section series was performed using an optical fractionator probe. The precision of the serial section analyses was assessed by the coefficient of error (p < 0.05). TH positive cell bodies were counted utilizing the above system, which ensured cells were not omitted or counted twice. For TH fibers and cell counts results were expressed as percentage of contralateral (unlesioned) side. For GFAP and CD11b positive cell counts, estimation of total numbers was performed using the Microbrightfield software and cell density was calculated for striatal and midbrain volumes. The striatum was outlined according to anatomical landmarks following the Paxinos atlas[31]. To avoid bias in the outline of the substantia nigra based on cresyl violet counterstain, the midbrain sections were divided in quadrants and the area ventral to the aqueduct was included for quantification of CD11b cell density and identified as ventral midbrain. Stereological analysis was performed by investigators blind to treatment group.
Group comparisons were performed using ANOVA to evaluate treatment, side and time effects. Post hoc analyses were performed whenever a significant effect (p < 0.05) was found. Simple regression analyses were performed to evaluate correlation between fiber and cell density. Statistical analyses were made using Statview software (SAS Institute Inc, Carny, North Carolina).
PET imaging
A total of 3 saline-injected and 11 6-OHDA lesioned rats were imaged by PET using 11C-CFT (2β-carbomethoxy-3β-(4-fluorophenyl) tropane), a specific ligand for presynaptic DA transporters (DAT)[32, 33]. To explore activation of microglia/macrophage function, imaging studies were conducted in the same rats with 11C-PK11195 (N-sec-butyl-1-(2-chlorophenyl)-N-methylisoquinoline-3-carboxamide), a specific ligand for activated microglia [28, 34]. Imaging studies were performed 2 or 3 weeks after 6-OHDA injections using an in-house-built, super high-resolution rodent PET system[35]. 11C-CFT was prepared according to previously published procedures [33, 36]. 11C-PK11195 was synthesized with a modified method of Camsonne et al [36]. Briefly, 1 mg of the precursor (N-sec-butyl-1-(2-chlorophenyl) isoquinoline-3-carboxamide) was dissolved in 500 μL DMSO with 5–10 mg KOH, after trapping the C-11 methyl iodide, the vessel was heated at 80°C for 3 min and purified by HPLC system comprising a mobile phase pump (Hitachi), an automatic sample injector with 5 ml loop (Merck) and a radioactivity detector (in-house construction). Separation was performed on a μ-Bondapak C-18 column (7.8–300 mm, Waters) using methanol and 0.01 M phosphoric acid (700 / 300, v/v) as the mobile phase with a flow of 8 ml/min. The radioactivity peak with a retention time of 5.6 min, similar to a reference standard was collected. After addition of 50 μL 5 M HCl, the collected fraction was evaporated and the residue was dissolved in saline buffer and sterilized by filtration through a 0.2-μm filter (Millex®-GV). About 50% of the radioactivity was trapped in the filter because of the high lipophilicity of PK11195. The average yield of the final product was 20 mCi within 45 min.
For PET imaging studies, animals were anaesthetized with halothane (1 - 1.5%) using an oxygen flow rate of 3 L/min. Tail vein was catheterized for infusion of the labelled ligands. The animal was placed in the imaging position and the head was adjusted into an in-house-built stereotaxic head-holder. Imaging studies of microglia and DAT were conducted in the same imaging session. 11C-PK11195 (1–2 mCi iv.) was administered first and dynamic data were acquired at two different coronal brain levels for an hour. After an additional hour of decay time 11C-CFT (2 – 3 mCi iv.) was administered and data were acquired as above. Calibration of the positron tomograph was performed in each study session using a cylindrical plastic phantom (diameter of 3 cm) and 18F-solution. Imaging data were corrected for uniformity, sensitivity, attenuation, decay and acquisition time [32]. PET images were reconstructed using Hanning-weighted convolution backprojection and overlaid on atlas templates to confirm anatomical location. Regions of interest, including the left and right striatum and cerebellum were drawn and activity per unit volume, percentage activity of injected dose and ligand concentration were calculated [32]. Binding ratios and left-right side differences were calculated as described previously[37].
Results
Following the 6-OHDA intrastriatal infusion, rats received either celecoxib at 20 mg/kg (COXIB group, N = 12) or vehicle (N = 13) by oral gavage daily until the time of sacrifice at 12 (n = 4/5) or 21(n = 8/8) days post surgery. First, we examined in vivo the effect of celecoxib compared to vehicle using micro PET and 11C PK11195, a peripheral benzodiazepine receptor ligand that binds to microglia [28] and 11C CFT, a cocaine analog that binds to the DAT. At 12 days we observed a decrease in CFT binding (~60% of contralateral BP) in the 6-OHDA lesioned striatum of both experimental groups (Fig. 1A). No striatal 11C PK11195 binding was present in the COXIB group (n = 3) while in the vehicle group (n = 2) there was binding ipsilateral to the 6-OHDA lesion, as described previously. No differences between COXIB (n = 3) and vehicle (n = 3) were observed at 21 days at the striatal level (Fig. 1A).
A) Using micro-PET and selective radioactive tracers we measured in vivo the extent of dopamine terminal loss and inflammatory response 12 (top panel) and 21 (bottom panel) days after the 6-OHDA lesion. Color-coded images of 11C-CFT ((2β-carbomethoxy-3β-(4-fluorophenyl) tropane, a dopamine transporter ligand) and 11C-PK11195 (a peripheral-type benzodiazepine ligand that binds to microglia) in a representative animal of each group. As reported in our previous study [28] 6-OHDA injection resulted in a marked decrease of 11C-CFT binding in the striatum and a parallel increase in 11C PK-11195 binding in the control (vehicle) group. The increase in 11C PK 11195 binding was absent in COXIB treated animals and in both groups at 21 days post lesion. B-C) Microphotographs of TH fiber density in the striatum in representative animals (same as shown in A). D) Volumetric analysis of fiber loss in the lesioned striatum showed a marked reduction at 12 days, that partially recovered at 21 days post-lesion (*, p < 0.01). TH striatal volumes were significantly larger in COXIB treated than in the vehicle group (#, p < 0.01). E) At 12 days post-lesion, both treatment groups displayed a ~40% loss of TH positive cell bodies in the SN. The progressive loss of DA cell bodies between 12 and 21 days post-lesion in the vehicle treated rats was significant (* p< 0.01) while there was no significant difference in DA cell bodies in the COXIB treated rats between 12 and 21 days. At 21 days the DA cell loss in the SN was significantly higher in vehicle treated animals (#, p < 0.05). Scale bar: 30 μm.
Next we examined the effect of celecoxib on the DA system. We analyzed the striatal volume of TH+ fibers (Fig. 1B,1C,1D) and quantified the number of TH+ cell bodies in the SN (Fig. 1E). At 12 days there was a severe (~85%) decrease in TH immunoreactive fibers in the striatum and less marked loss of TH+ cells (~40%) in the SN, and there were no differences between groups in either of these measures (Fig 1B,1D). However, at 21 days animals in the COXIB group displayed significantly larger volumes of DA terminal fibers in the striatal areas (> 50%, t = 7.8, p = 0.01) and corresponding larger number of TH+ cell bodies in the SN (t = 5, p < 0.05, Fig. 1B,1C,1D). In the vehicle group there was a significant progression of TH+ cell loss from 12 to 21 days (t = 3.5, p < 0.01) (Fig. 1E), which is consistent with previous studies [26–29]. This progression did not occur in the COXIB group (p = 0.7). In addition to the treatment effect, there was a significant recovery of striatal fiber density at 21 days in both groups. At this time point, the striatal TH fiber volume was directly correlated with the number of remaining DA cells in the SN (p < 0.01).
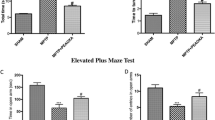
Using a selective antibody directed against CD11b (C3R), we studied activated microglia by morphological analysis and performed stereological quantification in the striatum (Fig. 2) and ventral midbrain (Fig. 3). In the COXIB group, a significant reduction in the number of activated microglia was seen in both striata (treatment effect F1,32 = 7, p = 0.01). This effect of selective COX-2 inhibition was more pronounced in the striatum at the 12-day time point after the toxin injection than at 21 days after 6-OHDA (Fig 2A,2B,2C). In addition to a significant increase in cell density, in the vehicle group the predominant morphology of microglial cells was amoeboid (activated) as opposed to ramified (resting) (Fig 2B and 2D). In the ventral midbrain microglial cell density was significantly higher ipsilateral to the 6-OHDA injection in the vehicle group at 21 days. ANOVA revealed a significant effect of time (F1,24 = 809, p < 0.001), lesion side (F1,24 = 17. p < 0.001) and treatment (F1,24 = 11.6, p < 0.01) on microglial density (Fig 3E,3F). Astrocytes immuno-labeled with GFAP were also quantified in the striatum. There was a significant astrogliosis ipsilateral to the 6-OHDA injection (F1,28 = 28, p < 0.001, Fig 4). This lesion effect decreased but was still noticeable at 21 days in the vehicle group. Interestingly, no effect of treatment (p = 0.9) was observed for astrocyte density (GFAP+ cells/mm3) (Fig 4E,4F). These results show that celecoxib produced a selective reduction of local microglial reaction in response to the neurotoxin.
The microglial response to 6-OHDA injection was significantly attenuated in the striatum of COXIB treated animals. Photomicrographs of activated microglia immunohistochemistry in a representative striatal section of a vehicle (A, B) and a COXIB (C, D) treated animal 12 days after the injection of 6-OHDA. All images are ipsilateral to the injection side. E, F) Bar graphs showing the stereological quantification of activated microglia cell density at 12 (E) and 21 days (F). Microglial density was significantly reduced in the striatum of COXIB treated rats (treatment effect p < 0.05) both in the lesioned and in the contralateral striata. However, the microglia response was not completely abolished in COXIB treated animals, as microglia density was significantly higher in the 6-OHDA injected striatum (p < 0.01) and the density was higher in the lesioned/treated striatum than in the contralateral/untreated striatum (p < 0.05). Scale bar: 100 μm for A and C and 25 μm for B and D.
Microglial density in the ventral midbrain. Photomicrographs of activated microglia immunohistochemistry in a representative midbrain section of a vehicle (A, B) and a COXIB (C, D) treated animal 21 days after the injection of 6-OHDA. E, F) Bar graphs showing the stereological quantification of activated microglia cell density at 12 (E) and 21 days (F). Microglial density was significantly reduced in the ventral midbrain of COXIB treated rats (treatment effect F= 6.28, p < 0.05) both in the lesioned and in the contralateral striata. Microglial density was higher at 21 days in all groups and was significantly higher in the vehicle group ipsilateral to the lesion (p < 0.05). Scale bar: 25 μm.
Astroglial response in the striatum. Photomicrographs of representative sections of the ipsilateral (A, B) and contralateral (C, D) striatum of an animal receiving COXIB at 21 days. E, F) Bar graphs showing the GFAP positive density in the striatum. E) Astroglial density was significantly higher in the lesioned striatum (P < 0.01), with no significant differences between treatment groups. F). Scale bar: 25 μm.
Discussion
Regular intake of nonaspirin NSAIDs (and high dose of aspirin) has been reported to be associated to a 45% lower risk of PD in 2 large cohorts [22]. In this study we found that COX-2 inhibition by celecoxib decreased microglial activation and was associated with a prevention of the progressive degeneration seen in the 6-OHDA retrograde lesion model of PD. We used the striatal administration of 6-OHDA because neuronal damage and death, characteristically progress over weeks. This provides a close (although accelerated) model for the cascade of degenerative events that occurs in PD. Between weeks 2 and 3, DA cell loss progressed from 40 to 65 % in vehicle treated animals, as previously described for this model [26, 27, 29, 38]. In contrast, we did not observe such a progression of DA neuronal cell loss in the COXIB group. It is worth noting that TH striatal fiber density was not correlated (more extensive) with DA cell numbers at 12 days, likely reflecting TH down-regulation in the acute stage of degeneration. Consistent with this explanation, there was a significant recovery of TH fibers in both groups at 21 days (Fig 1B,1C,1D) to levels that matched and corresponded to the number of DA neurons remaining in the substantia nigra. Based on this temporal pattern we propose that COX-2 inhibition protects a nigral neuronal cell population with reversible damage [15, 39, 40]. Such neurons are damaged and have reduced axonal TH expression at 2 weeks. Left to the natural evolution of the progressive degeneration half of these DA neurons will eventually die [26–29]. Our results show that COX-2 inhibition resulted in a complete protection of these damaged DA neurons. This effect can be dependent on specific intraneuronal effects of celecoxib and/or related to a classical anti-inflammatory mechanism, through microglial cell inhibition. Interestingly, the reduction of microglia activation by celecoxib was stronger at 12 days (Fig. 2E), while at this time point there were no differences in DA markers between groups. The reduction in microglia was not accompanied by changes in astroglial reaction to the striatal injury (Fig. 4).
With infectious or tissue injury stimuli, including inflammatory or selective DA terminal lesions of the striatum, microglia can both proliferate and transform morphologically into reactive forms [28, 41]. The reactive microglia's amoeboid movement and activities in injured neural tissue include macrophage activity and presumed synaptic stripping along dendrites [42]. In the current PD model, microglial invasion and continued presence in the lesioned striatum and substantia nigra could contribute to long-term synaptic disconnection of the damaged DA terminal afferents. Such loss of normal neuron target interactions and trophic support can lead to DA neuronal vulnerability, atrophy or death [43, 44]. In experimental in vivo PD models with delayed DA neuronal death, various exogenous trophic factor support of DA neurons [29, 43–46] or intracellular signalling related to neuroimmunophilins [30] can prevent long-term progressive DA degeneration to a similar degree to that seen by COX-2 inhibition in the present study. In chronic degenerative situations involving the striatum and midbrain and during marked fluctuations in neuronal ionic, metabolic and functional status, astroglia are thought to play a more homeostatic, trophic and protective role for DA neurons and terminals than microglia [47, 48]. Our evidence clearly demonstrate that selective COX-2 inhibition did not reduce the typical astroglial response to injury in the striatum, while to a large extent preventing expression of the morphologically activated microglial phenotype. In fact, COX-2 inhibition had by 3 weeks of treatment (compared to vehicle) caused a mild elevation of the number of reactive astrocytes in the striatum contralateral to the lesion (Fig. 4). In the period of progressive DA neuronal death between the 2nd and 3rd week after DA terminal injury by 6-OHDA, our data indicate that nigro-striatal DA terminals were restored in striatum, and a significant population of DA neurons where spared from cell death in the substantia nigra by COX-2 inhibition. These results point to an altered reactive astroglial to reactive microglial cell ratio by COX-2 inhibition that may provide insights for how to create favorable conditions for prevention of progressive neurodegenerative cascades during and after neuronal injury similar to that seen in PD.
Microglial cells can also produce and release pro-inflammatory cytokines, in particular TNFα, and cytotoxic molecules including ROS and NO [34] although such responses are non-specific to lesion type [41]. After 6-OHDA intrastriatal infusion, there is an acute increase in TNF-α in the striatum [49]. Pro-inflammatory cytokines IL-1β and TNF-α activate the p38MAPK cascade and NFkB translocation to the nucleus, resulting in transcriptional upregulation of COX-2. TNF-α activates COX-2 via the JNK pathway [50] and induction of NFkB [51]. Importantly p38 MAPK stabilizes the mRNA of COX-2 and other pro-inflammatory factors [52, 53]. Activated microglia cells release NO [54, 55] and superoxide free radical [11]. DA neurons are particularly vulnerable to this type of inflammation induced oxidative stress as DA metabolism and DA autoxidation generate ROS [56]. Celecoxib (at low dose) [57, 58] and other NSAIDs (and minocycline) inhibit p38MAPK leading to a decrease in COX-2 production, decreased mRNA stability and decreased PGE2 release. It is possible that celecoxib, by blocking COX-2 enzymatic activity and by inhibition of the p38MAPK pathway, constrained the inflammatory response induced by striatal 6-OHDA thus limiting, to a certain extent, the progressive DA neuronal death. Similar protective effects of selective COX-2 inhibitors have been reported in excitotoxicity and ischemia models [7, 59–61].
The benefit we observed can also stem directly from neuronal inhibition of COX-2, which is one of several enzymes capable of oxidizing DA to reactive DA quinone [62]. DA quinones can deplete the cells of antioxidants, inactivate enzymes and increase α-synuclein protofibrils [56, 63]. Induction of COX-2 results in an inflammatory cascade accompanied by formation of ROS. Recent work using the mouse MPTP model of PD suggests that an intraneuronal mechanism can be sufficient to achieve neuroprotection in that specific acute paradigm [64, 65]. Therefore the reported effects could be attributed to a direct decrease of inflammatory mediators inside the neuron or to inhibition of release of proinflammatory and toxic factors from microglia [24, 40]. The temporal relationship between glial activation and neurodegeneration suggests that microglial activation plays a key role in amplifying the toxic effect and thereby exacerbating DA cell loss, although it cannot be determined by these experiments whether microglia inhibition is absolutely required to achieve neuroprotection. Massive and prolonged microglial cell activation has been observed in aged mice exposed to MPTP, associated with a progressive loss of TH+ neurons [66]. Sugama et al. and our data strongly suggest that microglia activation prolongs an oxidative environment after the initial toxic insult, leading to the subsequent loss of neurons that have a reversible damage [39, 40]. Specifically, in the retrograde 6-OHDA lesion paradigm that we used here, ~50% of the DA neurons with reversible damage will die between weeks 2 and 3 after the initial injury. In this study celecoxib treatment rescued this population. Therefore inhibition of COX-2 by celecoxib appears to be able, directly, and through inhibition of microglia activation to result in a reduction of DA cell degeneration.
The presence of activated microglia in the brain of PD patients [2] and after MPTP exposure both in humans [67]and monkeys [4] supports the existence of an ongoing inflammatory process that can contribute to the progression of the disease. The origin of neuroinflammation is unknown and is probably different for different individuals, being a common response to a variety of pathogenic insults. If indeed chronic neuroinflammation contributes to the progression of the degenerative process [15], anti-inflammatory drugs could prevent or slow down the disease, independently of the causative factors.
Abbreviations
- 6-OHDA:
-
6-hydroxydopamine
- ANOVA:
-
analysis of variance
- BP:
-
binding potential
- CFT:
-
2β-carbomethoxy-3β-(4-fluorophenyl) tropane
- COX:
-
cyclooxygenase
- COX-2:
-
cyclooxygenase type 2 isoform
- COXIB:
-
COX inhibitor
- DA:
-
dopamine
- DAT:
-
dopamine transporters
- DMSO:
-
dimethyl sulfoxide
- GFAP:
-
glial fibrillary acidic protein
- HCl:
-
hydrogen chloride
- HPLC:
-
high performance liquid chromatography
- IL-1β:
-
interleukin-1 beta
- LPS:
-
lipopolysaccharide
- MAPK:
-
mitogen-activated protein kinase
- MPTP:
-
N-methyl 1,2,3,6 tetrahydropyridine
- NGS:
-
normal goat serum
- NO:
-
nitric oxide
- NSAID:
-
nonsteroidal anti-inflammatory drugs
- OX42:
-
CD11b
- PBS:
-
phosphate buffered saline
- PD:
-
Parkinson's disease
- PET:
-
positron emission tomography
- PK-11195:
-
N-sec-butyl-1-(2-chlorophenyl)-N-methylisoquinoline-3-carboxamide
- ROS:
-
reactive oxygen species
- SN:
-
substantia nigra
- TH:
-
tyrosine hydroxylase
- TNFα:
-
tumor necrosis factor alpha
References
Liu B, Hong JS: Role of microglia in inflammation-mediated neurodegenerative diseases: mechanisms and strategies for therapeutic intervention. J Pharmacol Exp Ther. 2003, 304: 1-7. 10.1124/jpet.102.035048.
McGeer PL, Itagaki S, Boyes BE, McGeer EG: Reactive microglia are positive for HLA-DR in the substantia nigra of Parkinson's and Alzheimer's disease brains. Neurology. 1988, 38: 1285-1291.
Hirsch EC, Breidert T, Rousselet E, Hunot S, Hartmann A, Michel PP: The role of glial reaction and inflammation in Parkinson's disease. Ann N Y Acad Sci. 2003, 991: 214-228.
McGeer PL, Schwab C, Parent A, Doudet D: Presence of reactive microglia in monkey substantia nigra years after 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine administration. Ann Neurol. 2003, 54: 599-604. 10.1002/ana.10728.
Drachman DB, Rothstein JD: Inhibition of cyclooxygenase-2 protects motor neurons in an organotypic model of amyotrophic lateral sclerosis. Ann Neurol. 2000, 48: 792-795. 10.1002/1531-8249(200011)48:5<792::AID-ANA14>3.3.CO;2-X.
Hara K, Kong DL, Sharp FR, Weinstein PR: Effect of selective inhibition of cyclooxygenase 2 on temporary focal cerebral ischemia in rats. Neurosci Lett. 1998, 256: 53-56. 10.1016/S0304-3940(98)00755-1.
Nakayama M, Uchimura K, Zhu RL, Nagayama T, Rose ME, Stetler RA, Isakson PC, Chen J, Graham SH: Cyclooxygenase-2 inhibition prevents delayed death of CA1 hippocampal neurons following global ischemia. Proc Natl Acad Sci U S A. 1998, 95: 10954-10959. 10.1073/pnas.95.18.10954.
Teismann P, Ferger B: Inhibition of the cyclooxygenase isoenzymes COX-1 and COX-2 provide neuroprotection in the MPTP-mouse model of Parkinson's disease. Synapse. 2001, 39: 167-174. 10.1002/1098-2396(200102)39:2<167::AID-SYN8>3.0.CO;2-U.
Wu DC, Jackson-Lewis V, Vila M, Tieu K, Teismann P, Vadseth C, Choi DK, Ischiropoulos H, Przedborski S: Blockade of microglial activation is neuroprotective in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model of Parkinson disease. J Neurosci. 2002, 22: 1763-1771.
Bal-Price A, Brown GC: Inflammatory neurodegeneration mediated by nitric oxide from activated glia-inhibiting neuronal respiration, causing glutamate release and excitotoxicity. J Neurosci. 2001, 21: 6480-6491.
Gao HM, Jiang J, Wilson B, Zhang W, Hong JS, Liu B: Microglial activation-mediated delayed and progressive degeneration of rat nigral dopaminergic neurons: relevance to Parkinson's disease. J Neurochem. 2002, 81: 1285-1297. 10.1046/j.1471-4159.2002.00928.x.
Castano A, Herrera AJ, Cano J, Machado A: Lipopolysaccharide intranigral injection induces inflammatory reaction and damage in nigrostriatal dopaminergic system. J Neurochem. 1998, 70: 1584-1592.
Shibata H, Katsuki H, Nishiwaki M, Kume T, Kaneko S, Akaike A: Lipopolysaccharide-induced dopaminergic cell death in rat midbrain slice cultures: role of inducible nitric oxide synthase and protection by indomethacin. J Neurochem. 2003, 86: 1201-1212.
Hirsch EC, Hunot S, Damier P, Faucheux B: Glial cells and inflammation in Parkinson's disease: a role in neurodegeneration?. Ann Neurol. 1998, 44 (3 Suppl 1): S115-20.
Hunot S, Hirsch EC: Neuroinflammatory processes in Parkinson's disease. Ann Neurol. 2003, 53 Suppl 3: S49-58; discussion S58-60. 10.1002/ana.10481.
Hartmann A, Mouatt-Prigent A, Faucheux BA, Agid Y, Hirsch EC: FADD: A link between TNF family receptors and caspases in Parkinson's disease. Neurology. 2002, 58: 308-310.
Knott C, Stern G, Wilkin GP: Inflammatory regulators in Parkinson's disease: iNOS, lipocortin-1, and cyclooxygenases-1 and -2. Mol Cell Neurosci. 2000, 16: 724-739. 10.1006/mcne.2000.0914.
Nagatsu T, Mogi M, Ichinose H, Togari A: Cytokines in Parkinson's disease. J Neural Transm Suppl. 2000, 143-151.
Nagatsu T, Mogi M, Ichinose H, Togari A: Changes in cytokines and neurotrophins in Parkinson's disease. J Neural Transm Suppl. 2000, 277-290.
Sriram K, Matheson JM, Benkovic SA, Miller DB, Luster MI, O'Callaghan JP: Mice deficient in TNF receptors are protected against dopaminergic neurotoxicity: implications for Parkinson's disease. Faseb J. 2002, 16: 1474-1476.
Nishimura M, Mizuta I, Mizuta E, Yamasaki S, Ohta M, Kaji R, Kuno S: Tumor necrosis factor gene polymorphisms in patients with sporadic Parkinson's disease. Neurosci Lett. 2001, 311: 1-4. 10.1016/S0304-3940(01)02111-5.
Chen H, Zhang SM, Hernan MA, Schwarzschild MA, Willett WC, Colditz GA, Speizer FE, Ascherio A: Nonsteroidal anti-inflammatory drugs and the risk of Parkinson disease. Arch Neurol. 2003, 60: 1059-1064. 10.1001/archneur.60.8.1059.
Shannon KM, Penn RD, Kroin JS, Adler CH, Janko KA, York M, Cox SJ: Stereotactic pallidotomy for the treatment of Parkinson's disease. Efficacy and adverse effects at 6 months in 26 patients. Neurology. 1998, 50: 434-438.
Ono K, Han J: The p38 signal transduction pathway: activation and function. Cell Signal. 2000, 12: 1-13. 10.1016/S0898-6568(99)00071-6.
Vane JR, Bakhle YS, Botting RM: Cyclooxygenases 1 and 2. Annu Rev Pharmacol Toxicol. 1998, 38: 97-120. 10.1146/annurev.pharmtox.38.1.97.
Sauer H, Oertel WH: Progressive degeneration of nigrostriatal dopamine neurons following intrastriatal terminal lesions with 6-hydroxydopamine: a combined retrograde tracing and immunocytochemical study in the rat. Neuroscience. 1994, 59: 401-415. 10.1016/0306-4522(94)90605-X.
Oiwa Y, Sanchez-Pernaute R, Harvey-White J, Bankiewicz KS: Progressive and extensive dopaminergic degeneration induced by convection-enhanced delivery of 6-hydroxydopamine into the rat striatum: a novel rodent model of Parkinson disease. J Neurosurg. 2003, 98: 136-144.
Cicchetti F, Brownell AL, Williams K, Chen YI, Livni E, Isacson O: Neuroinflammation of the nigrostriatal pathway during progressive 6-OHDA dopamine degeneration in rats monitored by immunohistochemistry and PET imaging. Eur J Neurosci. 2002, 15: 991-998. 10.1046/j.1460-9568.2002.01938.x.
Bjorklund A, Rosenblad C, Winkler C, Kirik D: Studies on neuroprotective and regenerative effects of GDNF in a partial lesion model of Parkinson's disease. Neurobiology of Disease. 1997, 4: 186-200. 10.1006/nbdi.1997.0151.
Costantini LC, Isacson O: Neuroimmunophilin ligand enhances neurite outgrowth and effect of fetal dopamine transplants. Neuroscience. 2000, 100: 515-520. 10.1016/S0306-4522(00)00312-2.
Paxinos G, Watson C: The Rat Brain in Stereotaxic Coordinates. 1986, San Diego, Academic Press
Brownell A-L, Jenkins BG, Elmaleh DR, Deacon TW, Spealman RD, Isacson O: Combined PET/MRS studies of the brain reveal dynamic and long-term physiological changes in a Parkinson's disease primate model. Nature Med. 1998, 4: 1308-1312. 10.1038/3300.
Hantraye P., Brownell, A.-L., Elmaleh, D., Spealman, R.D., Wullner, U., Brownell, G.L., Isacson, O.: Dopamine fiber detection by [11C]-CFT and PET in a primate model of parkinsonism. NeuroReport. 1992, 3: 265-268.
Banati RB, Goerres GW, Myers R, Gunn RN, Turkheimer FE, Kreutzberg GW, Brooks DJ, Jones T, Duncan JS: [11C](R)-PK11195 positron emission tomography imaging of activated microglia in vivo in Rasmussen's encephalitis. Neurology. 1999, 53: 2199-2203.
Brownell AL, Livni E, Galpern W, Isacson O: In vivo PET imaging in rat of dopamine terminals reveals functional neural transplants. Annals of Neurology. 1998, 43: 387-390.
Camsonne R, Crouzel C, Comar D, Maziere M, Prenant C, Sastre J, Moulin MA, Syrota A: Synthesis of N-(11-C) Methyl, N-(Methyl-1 Propyl), (Chloro-2 Phenyl)-1 Isoquinoleine Carboxamide-3 (PK 11195): A new ligand for peripheral benzodiazepine receptors. Journal of Labelled Compounds and Radiopharmaceuticals. 1984, XXI: 985-991.
Correia J., Burnham, C., Kaufman, D., Fischman, A.: Development of a small animal PET imaging device with resolution approaching 1mm. IEEE Trans Nucl Sci. 1999, 46: 631-635. 10.1109/23.775590.
Cicchetti F, Costantini L, Belizaire R, Burton W, Isacson O, Fodor W: Combined inhibition of apoptosis and complement improves neural graft survival of embryonic rat and porcine mesencephalon in the rat brain. Exp Neurol. 2002, 177: 376-384. 10.1006/exnr.2002.8007.
Isacson O: On Neuronal Health. Trends Neurosci. 1993, 16: 306-308. 10.1016/0166-2236(93)90104-T.
Hartmann A, Hunot S, Hirsch EC: Inflammation and dopaminergic neuronal loss in Parkinson's disease: a complex matter. Exp Neurol. 2003, 184: 561-564. 10.1016/j.expneurol.2003.08.004.
Depino AM, Earl C, Kaczmarczyk E, Ferrari C, Besedovsky H, del Rey A, Pitossi FJ, Oertel WH: Microglial activation with atypical proinflammatory cytokine expression in a rat model of Parkinson's disease. Eur J Neurosci. 2003, 18: 2731-2742. 10.1111/j.1460-9568.2003.03014.x.
Schiefer J, Kampe K, Dodt HU, Zieglgansberger W, Kreutzberg GW: Microglial motility in the rat facial nucleus following peripheral axotomy. J Neurocytol. 1999, 28: 439-453. 10.1023/A:1007048903862.
Isacson O, Brundin P, Gage FH, Bjorklund A: Neural grafting in a rat model of Huntington's disease: Progressive neurochemical changes after neostriatal ibotenate lesions and striatal tissue grafting. Neuroscience. 1985, 16: 799-817. 10.1016/0306-4522(85)90095-8.
Volpe BT, Wildmann J, Altar CA: Brain-derived neurotrophic factor prevents the loss of nigral neurons induced by excitotoxic striatal-pallidal lesions. Neuroscience. 1998, 83: 741-748. 10.1016/S0306-4522(97)00424-7.
Connor B, Kozlowski DA, Schallert T, Tillerson JL, Davidson BL, Bohn MC: Differential effects of glial cell line-derived neurotrophic factor (GDNF) in the striatum and substantia nigra of the aged Parkinsonian rat. Gene Ther. 1999, 6: 1936-1951. 10.1038/sj.gt.3301033.
Frim DM, Uhler TA, Galpern WR, Beal MF, Breakefield XO, Isacson O: Implanted fibroblasts genetically engineered to produce brain-derived neurotrophic factor prevent 1-methyl-4-phenylpyridinium toxicity to dopaminergic neurons in rat. Proc Nat Acad Sci U S A. 1994, 91: 5104-5108.
Cunningham LA, Su C: Astrocyte delivery of glial cell line-derived neurotrophic factor in a mouse model of Parkinson's disease. Exp Neurol. 2002, 174: 230-242. 10.1006/exnr.2002.7877.
Isacson O, Fischer W, Wictorin K, Dawbarn D, Bjorklund A: Astroglial response in the excitotoxically lesioned neostriatum and its projection areas in the rat. Neuroscience. 1987, 20: 1043-1056. 10.1016/0306-4522(87)90262-4.
Mladenovic A, Perovic M, Raicevic N, Kanazir S, Rakic L, Ruzdijic S: 6-Hydroxydopamine increases the level of TNFalpha and bax mRNA in the striatum and induces apoptosis of dopaminergic neurons in hemiparkinsonian rats. Brain Res. 2004, 996: 237-245. 10.1016/j.brainres.2003.10.035.
Adams FS, LaRosa FG, Kumar S, Edwards-Prasad J, Kentroti S, Vernadakis A, Freed CR, Prasad KN: Characterization and transplantation of two neuronal cell lines with dopaminergic properties. Neurochemical Research. 1996, 21: 619-627.
Yamamoto S, Yamamoto K, Kurobe H, Yamashita R, Yamaguchi H, Ueda N: Transcriptional regulation of fatty acid cyclooxygenases-1 and -2. Int J Tissue React. 1998, 20: 17-22.
Ridley SH, Dean JL, Sarsfield SJ, Brook M, Clark AR, Saklatvala J: A p38 MAP kinase inhibitor regulates stability of interleukin-1-induced cyclooxygenase-2 mRNA. FEBS Lett. 1998, 439: 75-80. 10.1016/S0014-5793(98)01342-8.
Monick MM, Robeff PK, Butler NS, Flaherty DM, Carter AB, Peterson MW, Hunninghake GW: Phosphatidylinositol 3-kinase activity negatively regulates stability of cyclooxygenase 2 mRNA. J Biol Chem. 2002, 277: 32992-33000. 10.1074/jbc.M203218200.
Wang MJ, Lin WW, Chen HL, Chang YH, Ou HC, Kuo JS, Hong JS, Jeng KC: Silymarin protects dopaminergic neurons against lipopolysaccharide-induced neurotoxicity by inhibiting microglia activation. Eur J Neurosci. 2002, 16: 2103-2112. 10.1046/j.1460-9568.2002.02290.x.
Minghetti L, Levi G: Microglia as effector cells in brain damage and repair: focus on prostanoids and nitric oxide. Prog Neurobiol. 1998, 54: 99-125. 10.1016/S0301-0082(97)00052-X.
Stokes AH, Hastings TG, Vrana KE: Cytotoxic and genotoxic potential of dopamine. J Neurosci Res. 1999, 55: 659-665. 10.1002/(SICI)1097-4547(19990315)55:6<659::AID-JNR1>3.0.CO;2-C.
Niederberger E, Tegeder I, Vetter G, Schmidtko A, Schmidt H, Euchenhofer C, Brautigam L, Grosch S, Geisslinger G: Celecoxib loses its anti-inflammatory efficacy at high doses through activation of NF-kappaB. Faseb J. 2001, 15: 1622-1624.
Tegeder I, Niederberger E, Vetter G, Brautigam L, Geisslinger G: Effects of selective COX-1 and -2 inhibition on formalin-evoked nociceptive behaviour and prostaglandin E(2) release in the spinal cord. J Neurochem. 2001, 79: 777-786. 10.1046/j.1471-4159.2001.00613.x.
Nogawa S, Zhang F, Ross ME, Iadecola C: Cyclo-oxygenase-2 gene expression in neurons contributes to ischemic brain damage. J Neurosci. 1997, 17: 2746-2755.
Kunz T, Oliw EH: The selective cyclooxygenase-2 inhibitor rofecoxib reduces kainate-induced cell death in the rat hippocampus. Eur J Neurosci. 2001, 13: 569-575. 10.1046/j.1460-9568.2001.01420.x.
Scali C, Giovannini MG, Prosperi C, Bellucci A, Pepeu G, Casamenti F: The selective cyclooxygenase-2 inhibitor rofecoxib suppresses brain inflammation and protects cholinergic neurons from excitotoxic degeneration in vivo. Neuroscience. 2003, 117: 909-919. 10.1016/S0306-4522(02)00839-4.
Hastings TG: Enzymatic oxidation of dopamine: the role of prostaglandin H synthase. J Neurochem. 1995, 64: 919-924.
Conway KA, Rochet JC, Bieganski RM, Lansbury P. T., Jr.: Kinetic stabilization of the alpha-synuclein protofibril by a dopamine-alpha-synuclein adduct. Science. 2001, 294: 1346-1349. 10.1126/science.1063522.
Teismann P, Tieu K, Choi DK, Wu DC, Naini A, Hunot S, Vila M, Jackson-Lewis V, Przedborski S: Cyclooxygenase-2 is instrumental in Parkinson's disease neurodegeneration. Proc Natl Acad Sci U S A. 2003, 100: 5473-5478. 10.1073/pnas.0837397100.
Hunot S, Vila M, Teismann P, Davis RJ, Hirsch EC, Przedborski S, Rakic P, Flavell RA: JNK-mediated induction of cyclooxygenase 2 is required for neurodegeneration in a mouse model of Parkinson's disease. Proc Natl Acad Sci U S A. 2004, 101: 665-670. 10.1073/pnas.0307453101.
Sugama S, Yang L, Cho BP, DeGiorgio LA, Lorenzl S, Albers DS, Beal MF, Volpe BT, Joh TH: Age-related microglial activation in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced dopaminergic neurodegeneration in C57BL/6 mice. Brain Res. 2003, 964: 288-294. 10.1016/S0006-8993(02)04085-4.
Langston JW, Forno LS, Tetrud J, Reeves AG, Kaplan JA, Karluk D: Evidence of active nerve cell degeneration in the substantia nigra of humans years after 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine exposure. Ann Neurol. 1999, 46: 598-605. 10.1002/1531-8249(199910)46:4<598::AID-ANA7>3.0.CO;2-F.
Acknowledgements
This work was supported by the NIH grants, R01NS41263 and Udall Parkinson's Disease Research Center P50NS39793 (OI). The support of the Kinetics Foundation, the Parkinson Foundation National Capital Area and the Consolidated Anti-Aging Foundation is also gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors' contributions
RSP participated in the design, surgical procedures, statistical analysis and manuscript preparation. AF participated in the surgeries and did all the treatments. OC carried out most of the histological and stereological procedures and analysis. MY carried out the HPLC and tracer synthesis procedures in the PET studies. ALB carried out and analyzed the PET studies. OI conceived the study and design analyzed the data and prepared the manuscript. All authors read, discussed and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Sánchez-Pernaute, R., Ferree, A., Cooper, O. et al. Selective COX-2 inhibition prevents progressive dopamine neuron degeneration in a rat model of Parkinson's disease. J Neuroinflammation 1, 6 (2004). https://doi.org/10.1186/1742-2094-1-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1742-2094-1-6