Abstract
Background
Follow-up epidemiologic studies are needed to assess trends and patterns of disease spread. No follow-up epidemiologic study has been done in the Kingdom of Saudi Arabia to assess the current prevalence of major chronic, noncommunicable diseases, specifically in the urban region, where modifiable risk factors remain rampant. This study aims to fill this gap.
Methods
A total of 9,149 adult Saudis ages seven to eighty years (5,357 males (58.6%) and 3,792 females (41.4%)) were randomly selected from the Riyadh Cohort Study for inclusion. Diagnosis of type 2 diabetes mellitus (DMT2) and obesity were based on the World Health Organization definitions. Diagnoses of hypertension and coronary artery disease (CAD) were based on the Seventh Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure and American Heart Association criteria, respectively.
Results
The overall crude prevalence of DMT2 was 23.1% (95% confidence interval (95% CI) 20.47 to 22.15). The age-adjusted prevalence of DMT2 was 31.6%. DMT2 prevalence was significantly higher in males, with an overall age-adjusted prevalence of 34.7% (95% CI 32.6 to 35.4), than in females, who had an overall age-adjusted prevalence of 28.6% (95% CI 26.7 to 29.3) (P < 0.001). The overall crude prevalence of obesity was 31.1% (95% CI 30.1 to 32.0). The age-adjusted prevalence of obesity was 40.0%. The prevalence of obesity was higher in females, with an overall prevalence of 36.5% (95% CI 35.1 to 37.83), than in males (25.1% (95% CI 23.7 to 26.3)) (P < 0.001). The age-adjusted prevalence of hypertension and CAD were 32.6% (95% CI 31.7 to 33.6) and 6.9% (95% CI 6.4 to 7.4), respectively.
Conclusion
Comparisons of our findings with earlier data show that the prevalence of DMT2, hypertension and CAD in Riyadh, Saudi Arabia, has alarmingly worsened. Aggressive promotion of public awareness, continued screening and early intervention are pivotal to boosting a positive response.
Similar content being viewed by others
Background
If the prevalence of diabetes mellitus type 2 (DMT2) continues to increase at the current rate, the global burden of this disease will swell between 2000 to 2030 from 171 million to 366 million patients [1]. Furthermore, healthcare expenditures on DMT2 alone will skyrocket from US$376 billion in 2010 to US$490 billion in 2030 [2]. The Middle East region has not been spared from this scourge and currently is among those worst-hit [1]. This global epidemic, shared by both industrialized and developing countries, has stimulated increased public awareness of the disease, the identification of risk factors and the knowledge that DMT2 can be delayed and, even better, prevented [3–5]. Recognition of the importance of glycemic control in the prevention of the complications and morbidity of DMT2 has led to worldwide campaigns for modifications in lifestyle and an intensive search for better antidiabetes medications [6–8].
In the Kingdom of Saudi Arabia (KSA), the rise in the prevalence of DMT2 started to gain attention years after rapid industrialization took place in the country [9]. Studies done since the late 1980s have shown an increasing trend among adult Saudis [10–12], the last of which, conducted in a large cohort of patients assembled from 1995 to 2000, revealed that one of five adult Saudis had DMT2 [13]. The same cohort showed an alarming prevalence of obesity at 40.0%, hypertension at 30% and coronary artery disease (CAD) at 6.2% [14–16]. A decade passed, and a follow-up epidemiologic study was designed to assess the current status of the population and whether the efforts of the Ministry of Health and the healthcare community have borne fruit.
Methods
The patients were part of the capital-wide Biomarker Screening in Riyadh (BSR), an ongoing collaborative effort between the Biomarkers Research Program (BRP) of King Saud University and the Ministry of Health in Riyadh, KSA (RIYADH Cohort). In brief, BSR was launched to identify and employ novel biomarkers of chronic noncommunicable diseases, including diabetes mellitus (DM), cardiovascular diseases, hypertension and obesity, among consenting Saudis. Ethical approval was obtained from the Ethics Committee of the College of Science Research Center of King Saud University, Riyadh, KSA.
Patients' information was taken from the existing database of more than 17,000 individuals. In this cross-sectional, observational study, a total of 9,149 Saudis (5,357 males (58.6%) and 3,792 females (41.4%)) ages seven to eighty years old were included. Patients were recruited randomly from their homes using the cluster sampling strategy. They were invited to visit the nearest primary healthcare center (PHCC). These centers span the entire Riyadh region. The population of each PHCC was taken as a cluster, and the allocations of the required numbers of patients were proportional to the populations served by the PHCCs. No expatriates were included in the conduct of this study. Each participating patient filled in a general questionnaire containing demographic, past and present medical history, as well as diet information from the food frequency questionnaire. This questionnaire was developed, pretested and validated in a pilot study. Informed written consent was obtained from each patient prior to inclusion.
Anthropometrics
Anthropometry included height (rounded off to the nearest 0.5 cm) and weight (rounded off to the nearest 0.1 kg), which were measured using an appropriate international standard scale (Digital Person Scale; ADAM Equipment, Milford, CT, USA), as well as waist and hip circumference in centimeters, which were measured using a standard tape measure. Mean systolic and diastolic blood pressure readings (in mmHg; average of two readings) were taken using appropriate cuffs.
Biochemical measurements
Consenting adults were invited to their respective PHCCs after a 10-hour overnight fast. Blood was drawn, centrifuged and processed on the same day. Both whole blood and serum were placed in plain polystyrene tubes. Serum was delivered to BRP for storage at -20°C. Fasting serum glucose was quantified using routine laboratory analysis (Konelab, Espoo, Finland). This biochemical analyzer was calibrated routinely prior to the analysis of all serum samples using quality control samples provided by the manufacturer (ThermoFisher Scientific, Espoo, Finland). The glucose-measuring method employed a glucose oxidase and modified Trinder color reaction catalyzed by the enzyme peroxidase.
Diagnosis of chronic noncommunicable diseases
The World Health Organization (WHO)-proposed cutoffs for DMT2 and impaired fasting glucose (IFG) were used. DMT2 was associated with a fasting plasma glucose (FPG) level ≥7.0 mmol/L (126 mg/dL), IFG with FPG level between 6.1 and 6.9 mmol/L (110 to 125 mg/dL) and normal with a FPG level < 6.1 mmol/L (110 mg/dL). All patients whose glucose levels exceeded the cutoffs were referred back to their respective PHCC physician for further tests and classification of DM. Screening for adult hypertension was based on the recommendations of the Seventh Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure [17]. Body Mass Index (BMI) was calculated as body weight in kilograms divided by height in square meters. Overweight was defined as a BMI of 25 to 29.9 kg/m2, and obesity was defined as a BMI ≥30. For patients ages 7 to 17 years, the cutoffs proposed by Cole and colleagues [18] were used for the definition of overweight and obesity. Diagnosis of hypertension in children was based on percentile [19]. CAD patients were known cases based on a medical history of angiography and intake of antiarrhythmic drugs.
Data analysis
Statistical analyses were carried out using SPSS 16.0 for Windows software (SPSS Inc., Chicago, IL, USA). The prevalence data for each of the various patient groups are shown with 95% confidence intervals. Prevalence was also calculated for gender and various age strata.
Results
The overall crude prevalence of DMT2 was 23.1% (95% confidence interval (95% CI) 20.47 to 22.15). The age-adjusted prevalence of DMT2 was 31.6%. The overall prevalence of IFG, on the other hand, was 9.0% (95% CI 8.37 to 9.53), with an age-adjusted prevalence of 10.2%. The prevalence of DMT2 was significantly higher in males, with an overall age-adjusted prevalence of 34.7% (95% CI 32.6 to 35.4), than in females (28.6% (95% CI 26.7 to 29.3)) (P < 0.001). The overall crude prevalence of obesity was 31.1% (95% CI 30.1 to 32.0). The age-adjusted prevalence of obesity was 40.0%. The overall prevalence of overweight, on the other hand, was 26.3% (95% CI 25.3 to 27.2), with an age-adjusted prevalence of 30.8%. The prevalence of obesity was significantly higher in females, with an overall prevalence of 36.5% (95% CI 35.1 to 37.83), than in males (25.1% (95% CI 23.7 to 26.3)) (P < 0.001). The overall prevalence of CAD was 4.2% (95% CI 3.9 to 4.7), with an age-adjusted prevalence of 6.9% (95% CI 6.4 to 7.4). The overall prevalence of hypertension was 25.7% (95% CI 24.8 to 26.6), with an age-adjusted prevalence of 32.6% (95% CI 31.7 to 33.6).
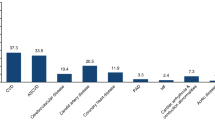
Tables 1 and 2 show the overall prevalence of DMT2 and the rest of the nonchronic diseases, as well as the gender-stratified prevalence according to age. Figure 1 shows the increasing trend of DMT2 from 1997 to 2011, as well as data for other chronic noncommunicable diseases in comparison to previous estimates.
Trends in the prevalence of chronic noncommunicable diseases in the Kingdom of Saudi Arabia from 2000 to 2010. (A) Age-adjusted prevalence of type 2 diabetes mellitus in Saudi Arabia according to gender (1997 [36], 2004 [7], 2011 (present study)). (B) Coronary artery disease. (C) Hypertension. (D) Obesity. Previous estimates shown are from the central region (Riyadh) and do not include other regions.
Discussion
The last overall crude prevalence of DMT2 in the KSA, as well as the central region in particular (Riyadh), was 23.7%, with an age-adjusted prevalence of 21.9% [7]. In the present study, the crude prevalence was 21.3%, with a calculated age-adjusted prevalence of 31.6%. The slight decrease in crude prevalence in the current study is negligible, considering the age range of the previous study, which was ages 30 to 70 years compared to ages 7 to 80 years in this study. Of note, in the previous report, 3,883 patients from the central region were studied, as opposed to the 9,149 patients included in this study. Interestingly, the age-adjusted prevalence of obesity in the central region was previously 40.0%, the same prevalence observed in the current study. These findings suggest that obesity is a major contributor to DMT2, but not the only one, and, in this instance, cannot explain the observed rise in the prevalence of the disease in the KSA.
It is apparent that the prevalence of DMT2 in the region has worsened, and the war against DMT2 in the kingdom is still far from over. Sadly, our results are beyond the predicted estimates of Shaw and colleagues [20], who stated that the biggest increase in the number of patients with DMT2 will be in developing nations. Several reasons may account for the higher prevalence of DMT2 in the KSA. The prevalence of conventional risk factors for DMT2, such as the full metabolic syndrome (MetS) and its individual manifestations, are still alarming among adult Saudis, 37% of whom have the full MetS [21], while just recently partial Metabolic syndrome (MetS) and isolated MetS manifestations were documented to be extremely high even among Saudi children [22]. In both cases, dyslipidemia accounted for almost 90% of the patient population [21, 22].
The emergence of novel risk factors for insulin resistance in this population has also come into play and includes, but is not limited to, vitamin D deficiency [23, 24], smoking cessation [25] and deficient sleep [26]. Treatment-wise, diabetes care in the primary care setting remains far from desirable [27], and, while limited studies have been done to assess public health awareness of DMT2 in the KSA, one recent study revealed poor knowledge of DMT2 risk factors and preventive measures among Saudi patients in the eastern region [28]. In addition, the general population still has an extremely high prevalence of physical inactivity, which is a major risk factor for all the diseases included in the study, including hypertension [29, 30]. Last, granted that DMT2 and other chronic diseases are polygenic disorders, the high consanguinity marriages among the Saudi population might be a contributing factor [31]. Any combination of the above risk factors, as well as an increase in the exposure to stress, might explain why the prevalence of chronic diseases in Saudi adults has increased even in the absence of a change in the prevalence of obesity [32].
In our study, there was an apparent gender difference in the prevalence of DMT2, with the prevalence in men higher than that in women. Such a difference was documented in a similar screening program done in the central region in the 1990s [33]. While it is known that men generally have a shorter life expectancy than women, several studies have highlighted lifestyle risk factors that are more frequent among Saudi males, including tobacco smoking [34], obesity and eating habits [35] and, just recently, vitamin D deficiency [36]. These factors cumulatively, but not completely, explain why there are more Saudi men than women with DMT2 and other chronic noncommunicable diseases. Furthermore, perhaps, the KSA and the Arabian Peninsula in general maintain a highly patriarchal society, which may place men at higher levels of chronic psychological stress than women, which in turn may contribute to metabolic and inflammatory stress over time, leading to several cell aging mechanisms and ultimately to chronic noncommunicable diseases such as DMT2 and CAD [37, 38].
With the exception of gestational diabetes mellitus (GDM) and CAD, the burden of otherwise adult-onset, chronic, noncommunicable diseases mentioned in this study is most striking and alarming in the pediatric cohort. This finding further expands and complicates the already challenging burden of these diseases. Aside from the environmental factors already mentioned, we recently demonstrated, in families from the same cohort, that multiple metabolic parameters, including circulating levels of key adipocytokines such as leptin and adiponectin, are significantly transmitted from parents to their offspring, with this phenomenon manifesting as early as the preteen years [39]. This finding, compounded by a metabolically adverse gestational and postnatal environment, which is prevalent in the KSA [40], adds to the susceptibility of the already genetically predisposed individual to a lifetime of insulin resistance and related morbidities.
We acknowledge several limitations of the present study. The prevalence of CAD was based only on the number of known cases, so the true prevalence of CAD in the cohort is expected to be higher. Furthermore, while current estimates may not necessarily reflect the true prevalence at a national level, since patients were recruited only in the central region, the findings are, on their own, strongly indicative of the need for a more aggressive approach to battle this epidemic.
Conclusions
In conclusion, this follow-up epidemiologic study shows that the prevalence of DMT2 in the KSA, specifically in its central region, has increased by a whopping 10.0% in just a decade, while it shows no improvement in the age-adjusted prevalence of obesity and a modest increase in the prevalence of hypertension and CAD. Translating these findings to aggressive health policies at the grassroots level and strict implementation of diabetes care is necessary to efficiently restrain the disease. Emerging risk factors for DMT2 specific to the Saudi population should also be addressed and further explored.
References
Wild S, Rogli G, Green A, Sicree R, King H: Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004, 27: 1047-1053. 10.2337/diacare.27.5.1047.
Zhang P, Zhang X, Brown J, Vistisen D, Sicree R, Shaw J, Nichols G: Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010, 87: 293-301. 10.1016/j.diabres.2010.01.026.
Cole A, Nathan DM, Spavaria-Porter E, Copeland P, Turchin A, Brunt M, Zusman R, Barrett JA, Wexler D, Case E, McMahon GT, Mort E: An algorithm for the care of type 2 diabetes. Crit Pathw Cardiol. 2009, 8: 156-165.
Rodbard HW, Jellinger PS, Davidson JA, Einhorn D, Garber AJ, Grunberger G, Handelsman Y, Horton ES, Lebovitz H, Levy P, Moghissi ES, Schwartz SS: Statement by an American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel on type 2 diabetes mellitus: an algorithm for glycemic control. Endocr Pract. 2009, 15: 540-559.
Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, Zinman B: Medical management of hyperglycemia in type 2 diabetes mellitus: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia. 2009, 52: 17-30. 10.1007/s00125-008-1157-y.
Warsy AS, el-Hazmi MA: Diabetes mellitus, hypertension and obesity: common multi-factorial disorders in Saudis. East Mediterr Health J. 1999, 5: 1236-1242.
Al-Nozha MM, Al-Maatouq MA, Al-Mazrou YY, Al-Harthi SS, Arafah MR, Khalil MZ, Khan NB, Al-Khadra A, Al-Marzouki K, Nouh MS, Abdullah M, Attas O, Al-Shahid MS, Al-Mobeireek A: Diabetes mellitus in Saudi Arabia. Saudi Med J. 2004, 25: 1603-1610.
Yamaoka K, Tango T: Efficacy of lifestyle education to prevent type 2 diabetes. Diabetes Care. 2005, 28: 2780-2786. 10.2337/diacare.28.11.2780.
Alzaid A: Time to declare war on diabetes. Ann Saudi Med. 1997, 17: 154-155.
Fatani HH, Mira SA, El-Zubier AG: Prevalence of diabetes mellitus in rural Saudi Arabia. Diabetes Care. 1987, 10: 180-183. 10.2337/diacare.10.2.180.
El-Hazmi M, Warsy A, Al-Swailem A, Sulaimani R: Diabetes mellitus as a health problem in Saudi Arabia. East Mediterr Health J. 1998, 4: 58-67.
Gilles CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, Hsu RT, Khunti K: Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ. 2007, 334: 299-10.1136/bmj.39063.689375.55.
Wilson GA, Gyi AA: The status and perspective of diabetes health education in China: inspiration from Australia. Int J Nurs Pract. 2010, 16: 92-98. 10.1111/j.1440-172X.2010.01817.x.
Al-Nozha MM, Al-Mazrou YY, Al-Maatouq MA, Arafah MR, Khalil MZ, Khan NB, Al-Marzouki K, Abdullah MA, Al-Khadra AH, Al-Harthi SS, Al-Shahid MS, Al-Mobeireek A, Nouh MS: Obesity in Saudi Arabia. Saudi Med J. 2005, 26: 824-829.
Al-Nozha MM, Arafah MR, Al-Mazrou YY, Al-Maatouq MA, Khan NB, Khalil MZ, Al-Khadra AH, Al-Marzouki K, Abdullah MA, Al-Harthi SS, Al-Shahid MS, Nouh MS, Al-Mobeireek A: Coronary artery disease in Saudi Arabia. Saudi Med J. 2004, 25: 1165-1171.
Al-Nozha MM, Abdullah M, Arafah MR, Khalil MZ, Khan NB, Al-Mazrou YY, Al-Maatouq MA, Al-Marzouki K, Al-Khadra A, Nouh MS, Al-Harthi SS, Al-Shahid MS, Al-Mobeireek A: Hypertension in Saudi Arabia. Saudi Med J. 2007, 28: 77-84.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ, Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee: Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003, 42: 1206-1252. 10.1161/01.HYP.0000107251.49515.c2.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH: Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000, 320: 1240-1246. 10.1136/bmj.320.7244.1240.
Falkner B, Daniels SR: Summary of the Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Hypertension. 2004, 44: 387-388. 10.1161/01.HYP.0000143545.54637.af.
Shaw JE, Sicree RA, Zimmet PZ: Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010, 87: 4-14. 10.1016/j.diabres.2009.10.007.
Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Sabico SL, Chrousos GP: Decreasing prevalence of the full metabolic syndrome but a persistently high prevalence of dyslipidemia among adult Arabs. PLoS One. 2010, 5: e12159-10.1371/journal.pone.0012159.
Al-Daghri NM: Extremely high prevalence of metabolic syndrome manifestations among Arab youth: a call for early intervention. Eur J Clin Invest. 2010, 40: 1063-1066. 10.1111/j.1365-2362.2010.02341.x.
Elsammak MY, Al-Wosaibi AA, Al-Howeish A, Alsaeed J: Vitamin D deficiency in Saudi Arabs. Horm Metab Res. 2010, 42: 364-368. 10.1055/s-0030-1248296.
Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Al-Yousef MA, Nadhrah HM, Sabico SB, Chrousos GP: Severe hypovitaminosis D is widespread and more common in non-diabetics than diabetics in Saudi adults. Saudi Med J. 2010, 31: 775-780.
Al-Daghri NM: Acute post cessation smoking: a strong predictive risk factor for metabolic syndrome among adult Saudis. Saudi Med J. 2009, 30: 267-271.
Bawazeer NM, Al-Daghri NM, Valsamakis G, Al-Rubeaan KSA, Sabico SL, Kumar S, McTernan PG, Harte AL: Sleep duration and quality associated with obesity among Arab children. Obesity (Silver Spring). 2009, 17: 2251-2253. 10.1038/oby.2009.169.
Al-Hussein FA: Diabetes control in a primary care setting: a retrospective study of 651 patients. Ann Saudi Med. 2008, 28: 267-271. 10.4103/0256-4947.51700.
Aljoudi AS, Taha AZ: Knowledge of diabetes risk factors and preventive measures among attendees of a primary care center in eastern Saudi Arabia. Ann Saudi Med. 2009, 29: 15-19. 10.4103/0256-4947.51813.
Al-Nozha MM, Al-Hazzaa HM, Arafah MR, Al-Khadra A, Al-Mazrou YY, Al-Maatouq MA, Khan NB, Al-Marzouki K, AL-Harthi SS, Abdullah M, Al-Shahid MS: Prevalence of physical activity and inactivity among Saudis aged 30-70 years: a population-based cross-sectional study. Saudi Med J. 2007, 28: 559-568.
Al-Hamdan N, Saeed A, Kutbi A, Choudhury AJ, Nooh R: Characteristics, risk factors, and treatment practices of known adult hypertensive patients in Saudi Arabia. Int J Hypertens. 2011, 2010: 168739.
Elhadd TA, Al-Amoudi AA, Alzahrani AS: Epidemiology, clinical and complications profile of diabetes in Saudi Arabia: a review. Ann Saudi Med. 2007, 27: 241-250. 10.4103/0256-4947.51484.
Chrousos GP: The role of stress and the hypothalamic-pituitary-adrenal axis in the pathogenesis of the metabolic syndrome: neuroendocrine and target-tissue-related causes. Int J Obes Relat Metab Disord. 2000, 24: S50-S55.
El-Hazmi MA, Al-Swailem A, Warsy AS, Al-Sudairy F, Sulaimani R, Al-Swailem A, Al-Meshari A: The prevalence of diabetes mellitus and impaired glucose tolerance in the population of Riyadh. Ann Saudi Med. 1995, 15: 598-601.
Bassiony MM: Smoking in Saudi Arabia. Saudi Med J. 2009, 30: 876-881.
Al-Rethaiaa AS, Fahmy AE, Al-Shwaiyat NM: Obesity and eating habits among college students in Saudi Arabia: a cross-sectional study. Nutr J. 2010, 9: 39-10.1186/1475-2891-9-39.
Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Yousef M, Sabico S, Chrousos GP: Hypovitaminosis D and cardiometabolic risk factors among non-obese youth. Cent Eur J Med. 2010, 5: 752-757. 10.2478/s11536-010-0045-2.
Al-Attas OS, Al-Daghri NM, Alokail MS, Al-Fadda A, Bamakhramah A, Sabico S, Pritlove D, Harte A, Tripathi G, McTernan PG, Kumar S, Chrousos GP: Adiposity and insulin resistance correlate with telomere length in middle-aged Arabs: the influence of circulating adiponectin. Eur J Endocrinol. 2010, 163: 601-607. 10.1530/EJE-10-0241.
Al-Nuaim AR: Prevalence of glucose intolerance in urban and rural communities in Saudi Arabia. Diabet Med. 1997, 17: 293-297.
Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Yakout SM, Sabico S, Gibson G, Chrousos GP, Kumar S: Parent-offspring transmission of adipocytokine levels and their associations with metabolic traits. PLoS One. 2011, 6: e18182-10.1371/journal.pone.0018182.
Al-Rowailly MA, Abolfotouh MA: Predictors of gestational diabetes mellitus in a high-parity community in Saudi Arabia. East Mediterr Health J. 2010, 16: 636-641.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1741-7015/9/76/prepub
Acknowledgements
The authors are grateful to the primary care physicians and nurses of the PHCCs in Riyadh for patient recruitment and sample collection. We extend special thanks to the laboratory technicians of the Biomarker Research Program at King Saud University, Riyadh, KSA, headed by Mr Ahmed Bamakhramah and Mr Moath Abuzagareet, for the analysis of samples. Finally, the authors thank Mr Benjamin Vinodson for statistical analyses of the data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
NMA and OSA conceived of the study. MSA, KMA and MY carried out data acquisition and interpretation. SLS and GPC analyzed the data and prepared the manuscript. All authors provided intellectual contributions to the manuscript and read and approved the final version.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Al-Daghri, N.M., Al-Attas, O.S., Alokail, M.S. et al. Diabetes mellitus type 2 and other chronic non-communicable diseases in the central region, Saudi Arabia (riyadh cohort 2): a decade of an epidemic. BMC Med 9, 76 (2011). https://doi.org/10.1186/1741-7015-9-76
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1741-7015-9-76