Abstract
Background
In maternal medicine, research evidence is scattered making it difficult to access information for clinical decision making. Systematic reviews of good methodological quality are essential to provide valid inferences and to produce usable evidence summaries to guide management. This review assesses the methodological features of existing systematic reviews in maternal medicine, comparing Cochrane and non-Cochrane reviews in maternal medicine.
Methods
Medline, Embase, Database of Reviews of Effectiveness (DARE) and Cochrane Database of Systematic Reviews (CDSR) were searched for relevant reviews published between 2001 and 2006. We selected those reviews in which a minimum of two databases were searched and the primary outcome was related to the maternal condition. The selected reviews were assessed for information on framing of question, literature search and methods of review.
Results
Out of 2846 citations, 68 reviews were selected. Among these, 39 (57%) were Cochrane reviews. Most of the reviews (50/68, 74%) evaluated therapeutic interventions. Overall, 54/68 (79%) addressed a focussed question. Although 64/68 (94%) reviews had a detailed search description, only 17/68 (25%) searched without language restriction. 32/68 (47%) attempted to include unpublished data and 11/68 (16%) assessed for the risk of missing studies quantitatively. The reviews had deficiencies in the assessment of validity of studies and exploration for heterogeneity. When compared to Cochrane reviews, other reviews were significantly inferior in specifying questions (OR 20.3, 95% CI 1.1–381.3, p = 0.04), framing focussed questions (OR 30.9, 95% CI 3.7- 256.2, p = 0.001), use of unpublished data (OR 5.6, 95% CI 1.9–16.4, p = 0.002), assessment for heterogeneity (OR 38.1, 95%CI 2.1, 688.2, p = 0.01) and use of meta-analyses (OR 3.7, 95% CI 1.3–10.8, p = 0.02).
Conclusion
This study identifies areas which have a strong influence on maternal morbidity and mortality but lack good quality systematic reviews. Overall quality of the existing systematic reviews was variable. Cochrane reviews were of better quality as compared to other reviews. There is a need for good quality systematic reviews to inform practice in maternal medicine.
Similar content being viewed by others
Background
Maternal medicine has emerged as an increasingly important area for the obstetricians dealing with high risk pregnancies. It involves care of women with medical complications of pregnancy which may be specific to or predate the pregnancy [1]. Approximately half of complex pregnancies are related to an abnormal fetal or obstetric factor, whereas medical diseases constitute the remainder of this high risk obstetric population. Scientific developments in internal or general medicine have led to newer diagnostic and therapeutic strategies to manage medical diseases. The physiological changes during pregnancy can affect not only the clinical presentation of a medical problem but may give rise to difficulties in diagnosing and managing these problems. In order to provide the best possible quality of care to women with complicated pregnancies obstetricians dealing with the high risk obstetric cases should have evidence based knowledge on the diagnostic, therapeutic and prognostic aspects of maternal medicine.
Recently there has been a proliferation of systematic reviews as one of the key tools for evidence-based medicine [2]. As maternal medicine covers the issues related to pregnancy as well as general medicine, research evidence is scattered in the literature making it difficult to access information for clinical decision making. Systematic reviews provide a way forward as individual pieces of research can be collected within literature reviews and if appropriate subjected to meta-analysis [3]. Good methodological quality is essential for these reviews to have valid inferences and to produce usable evidence summaries to guide the obstetric management [4]. This study examines the methodological features of recently published systematic reviews in maternal medicine and specifically compares Cochrane to non-Cochrane reviews.
Methods
To determine the quality of current systematic reviews in maternal medicine, we developed a priori protocol based on recommended methods [2, 5–7].
A computerised search of publicly available databases was conducted. Ovid Medline (1996 to date), Embase (1996 to date), Database of Reviews of Effectiveness and Cochrane Database of Systematic Reviews were searched for relevant reviews published between 2001 and 2006. Key word combinations like Pregnan$, Matern$, Gestation$, Obstetric$, Complication$, Systematic review$ and Meta analys$ were used for the search strategy in addition to word variants, subject headings and free text. The $ sign is a truncator used to capture any word that begin with the letters in front of the $ sign in the search terms used. Additionally common and specific medical problems related to pregnancy were searched using key words describing names of the disease such as Pre eclampsia, Hypertension, Diabetes, Cholestasis, Anaemia, Thrombocytopaenia, Thrombophilia, and Thromboembolism. Hand search of reference lists was conducted of all relevant articles to identify any missing reviews. The searches were limited to reviews between 2001 and 2006 due to increasing developments in the field of maternal medicine in recent years. Inclusion criteria required a minimum of two publicly available databases searched for a medical condition specific to or predating pregnancy and maternal factor as the primary outcome. We searched without language restrictions. All the reviews with fetal or neonatal factor as the primary outcome were excluded.
Two reviewers independently extracted and assessed the data according to a checklist formulated as part of our protocol (Table 1). The methodological quality of each review was assessed by focussing on framing of the question, literature search and review methods scrutinising methods of literature search and data synthesis. The items assessed internal validity and explicitness of reporting, both of which are important issues in quality of reviews. Differences between reviewers were resolved by discussion. We computed rates of compliance with the items in our checklist and compared Cochrane and non-Cochrane reviews. Odds ratios and their 95% confidence intervals were computed. All statistical analysis was performed using Stata 8.0 statistical package.
Results
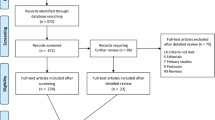
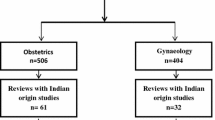
The initial literature search resulted in 2864 citations. Of these 68 reviews [8–75] fulfilled the inclusion criteria and were selected for detailed study (Fig 1). A total of 39 (57%) Cochrane reviews [8–46] and 29 (43%) non Cochrane reviews [47–75] were included. Most of the reviews assessed therapeutic interventions (50/68, 74%), and the rest were reviews on prognosis (12/68, 17%) and diagnosis (6/68, 9%). The range of clinical topics dealt with by the reviews is shown in Fig 2.
Overall quality of the existing systematic reviews was variable (Fig 3). Majority of the reviews (62/68, 91%) specified the question and 54/68 (79%) had a focussed question with clearly defined population and outcome measures. A large population of the reviews (64/68, 94%) had a detailed search description including databases searched and key words used. Almost half of the reviews (32/68, 47%) attempted to include unpublished data. However only 11/68 (16%) assessed the risk of missing studies quantitatively and 17/68 (25%) searched without language restriction. Almost all the reviews had good tabulation of results and characteristics of included studies (65/68, 96%).
The quality of Cochrane and non Cochrane reviews is given in Fig 3. Cochrane reviews [8–46] had specified the questions more often than non Cochrane reviews [47–51, 53–55, 58–60, 62–71, 73–75] (OR 20.3, 95% CI 1.1–381.3, p = 0.04) and were also framed narrowly focussed questions specifying the population, interventions and comparisons, outcome of the study and the study design (OR 30.9, 95% CI 3.7- 256.2, p = 0.001). Cochrane reviews attempted more often to include unpublished data in literature search (OR 5.6, 95% CI 1.9–16.4, p = 0.002). Twelve out of 29 non-Cochrane reviews [48, 50, 53–55, 64–66, 68–71] performed a meta-analysis, but there was good awareness of where this technique was valuable and where it was not applicable. Meta analysis technique (OR 3.7, 95% CI 1.3–10.8, p = 0.02) and assessment for heterogeneity (OR 38.1, 95%CI 2.1, 688.2, p = 0.01) was found to be employed significantly more often by Cochrane reviews.
Discussion
Our study showed that the Cochrane reviews [8–46] were of consistently high methodological quality and had a greater level of assessment for quality of included studies. They always did a meta-analysis [9, 12, 17, 19–25, 27–40, 44–46] where applicable. This is reassuring for clinicians who rely on them for decision-making. It is possible that the restriction on the length of published non Cochrane reviews by journals could have influenced their quality scores. However this issue has been addressed by increase in the web publishing of additional material in the electronic format by many journals in recent years.
This work has highlighted that literature searches in reviews are currently generally poor. A search that is not thorough risks giving biased inferences. We identified considerable room for improvement in certain methodological features of non Cochrane reviews. However all the selected reviews were similar in searches without language restriction and assessment for risk of missing studies. Interestingly use of reference list of the selected papers to identify any other eligible studies for inclusion in the review was found to be more frequent in non Cochrane reviews (OR 0.2, 95% CI 0.1–0.7, p < 0.007). This could be a result of the generic search strategy employed by Cochrane reviews with unclear mention of the use of reference lists in individual reviews. Cochrane reviews were found more likely to attempt to include unpublished data compared to non Cochrane reviews (OR 5.6, 95% CI 1.9–16.4, p < 0.002). This attempt to avoid publication bias is significant as the odds of publication are higher if the results are found to be significant compared to studies with non-significant results.[76]
This study identified areas of maternal medicine that lack good quality systematic reviews. Majority of the reviews were on hypertensive disorders [8, 10, 11, 17, 19–23, 31–34, 37, 48, 53, 55, 58, 64, 65, 69, 70], psychiatry [15, 27, 43, 47, 50–52, 56, 57, 59, 61, 74, 75], or thromboembolism [26, 42, 62–66, 68]. Even among these commonly addressed areas, a very narrow spectrum of diseases was covered. For example reviews in psychiatry were solely focussed on depression during pregnancy and reviews in hypertension focussed mainly on pre eclampsia. Reviews for some very common medical problems during pregnancy were missing or of poor quality. We found very few reviews on diabetes mellitus [12, 39, 49, 73] and chronic hypertension and none on thyroid disorders.
With advancement in neonatology and paediatric medicine, more and more women with congenital problems such as congenital heart disease and inherited metabolic diseases are reaching child bearing age and considering pregnancy. There is an urgent need to have some cumulative evidence on management of this high risk group in the best possible way.
This study has some potential limitations. With our strict criteria to include reviews conducted with two publicly available databases, it is possible that some of the good quality reviews in maternal medicine using single database are missed. Another limitation relates to maternal outcome as the main focus of our study. We excluded all those reviews in which association between maternal disease and perinatal outcome was assessed. Keeping in mind the primary goal of an obstetrician being directed towards achieving a healthy and safe outcome for both mother and fetus, good quality evidenced based information on medical problems during pregnancy can only be achieved by reviewing methodological features of all aspects of maternal medicine irrespective of the endpoint. Due to the absence of blinding of the reviewers to the source of the review it is difficult to completely rule out any resultant bias.
Conclusion
Evidence based healthcare continues to make important contributions to the well being of pregnant women. This study has identified areas in maternal medicine that lack good quality systematic reviews. Overall quality of the existing systematic reviews was variable, with Cochrane reviews better than other reviews. To achieve better understanding and provide high quality obstetric care for pregnant women with medical problems, it is important to ensure that systematic reviews in maternal medicine are conducted to cover wider spectrum of diseases, and are reported at the highest possible quality.
Funding
None
References
Department of Health: Specialised Services National Definition Set: 4 Specialised services for women's health. Department of health. 2006, [http://www.dh.gov.uk/en/PolicyAndGuidance/HealthAndSocialCareTopics/SpecialisedServicesDefinition]
Oxman AD, Cook DJ, Guyatt GH: Users' guides to the medical literature. VI. How to use an overview. Evidence-Based Medicine Working Group. JAMA. 1994, 272: 1367-1371. 10.1001/jama.272.17.1367.
Sacks HS, Reitman D, Pagano D: Meta-analysis: an update. Mt Sinai J Med. 1996, 63: 216-224.
Petticrew M: Systematic reviews from astronomy to zoology: myths and misconceptions. BMJ. 2001, 322: 98-101. 10.1136/bmj.322.7278.98.
Clarke M: The QUORUM statement. Lancet. 2000, 355: 756-757. 10.1016/S0140-6736(05)72172-3.
Jadad AR, Cook DJ, Jones A, et al: Methodology and reports of systematic reviews and meta-analyses: a comparison of Cochrane reviews with articles published in paper-based journals. JAMA. 1998, 280: 278-280. 10.1001/jama.280.3.278.
Oxman AD, Guyatt GH: Validation of an index of the quality of review articles. J Clin Epidemiol. 1991, 44: 1271-1278. 10.1016/0895-4356(91)90160-B.
Abalos E, Duley L, Steyn DW, Henderson-Smart D: Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database of Systematic Reviews. 2001, CD002252-2
Adab N, Tudur SC, Vinten J, Williamson P, Winterbottom J: Common antiepileptic drugs in pregnancy in women with epilepsy. Cochrane Database of Systematic Reviews. 2004, CD004848-3
Atallah AN, Hofmeyr GJ, Duley L: Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database of Systematic Reviews. 2002, CD001059-1
Bergel E, Carroli G, Althabe F: Ambulatory versus conventional methods for monitoring blood pressure during pregnancy. Cochrane Database of Systematic Reviews. 2002, CD001231-2
Boulvain M, Stan C, Irion O: Elective delivery in diabetic pregnant women. Cochrane Database of Systematic Reviews. 2001, CD001997-2
Brocklehurst P: Antibiotics for gonorrhoea in pregnancy. Cochrane Database of Systematic Reviews. 2002, CD000098-2
Cuervo LG, Mahomed K: Treatment for iron deficiency anaemia in pregnancy. Cochrane Database of Systematic Reviews. 2001, CD003094-2
Dennis CL, Creedy D: Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database of Systematic Reviews. 2004, CD001134-4
Burrows RF, Clavisi O, Burrows E: Interventions for treating cholestasis in pregnancy. Cochrane Database of Systematic Reviews. 2001, CD000493-4
Churchill D, Duley L: Interventionist versus expectant care for severe pre-eclampsia before term. Cochrane Database of Systematic Reviews. 2002, CD003106-3
Dodd J, Dare MR, Middleton P: Treatment for women with postpartum iron deficiency anaemia. Cochrane Database of Systematic Reviews. 2004, CD004222-4
Duley L, Henderson-Smart DJ: Drugs for treatment of very high blood pressure during pregnancy. Cochrane Database of Systematic Reviews. 2002, CD001449-4
Duley L, Henderson-Smart D: Magnesium sulphate versus phenytoin for eclampsia. Cochrane Database of Systematic Reviews. 2003, CD000128-4
Duley L, Henderson-Smart D: Magnesium sulphate versus diazepam for eclampsia. Cochrane Database of Systematic Reviews. 2003, CD000127-4
Duley L, Gulmezoglu AM, Henderson-Smart DJ: Magnesium sulphate and other anticonvulsants for women with pre-eclampsia. Cochrane Database of Systematic Reviews. 2003, CD000025-2
Duley L, Henderson-Smart D, Meher S: Altered dietary salt for preventing pre-eclampsia, and its complications. Cochrane Database of Systematic Reviews. 2005, CD005548-4
French L, Smaill F: Antibiotic regimens for endometritis after delivery. Cochrane Database of Systematic Reviews. 2004, CD001067-4
Garner P, Gulmezoglu A: Drugs for preventing malaria-related illness in pregnant women and death in the newborn. Cochrane Database of Systematic Reviews. 2002, CD000169-4
Gates S, Brocklehurst P, Davis LJ: Prophylaxis for venous thromboembolic disease in pregnancy and the early postnatal period. Cochrane Database of Systematic Reviews. 2002, CD001689-2
Howard LM, Hoffbrand S, Henshaw C, Boath L, Bradley E: Antidepressant prevention of postnatal depression. Cochrane Database of Systematic Reviews. 2005, CD004363-2
Jewell D, Young G: Interventions for nausea and vomiting in early pregnancy. Cochrane Database of Systematic Reviews. 2002, CD000145-1
Jewell D, Young G: Interventions for treating constipation in pregnancy. Cochrane Database of Systematic Reviews. 2001, CD001142-2
Kroner C, Turnbull D, Wilkinson C: Antenatal day care units versus hospital admission for women with complicated pregnancy. Cochrane Database of Systematic Reviews. 2001, CD001803-4
Magee L, Sadeghi S: Prevention and treatment of postpartum hypertension. Cochrane Database of Systematic Reviews. 2005, CD004351-1
Magee LA, Duley L: Oral beta-blockers for mild to moderate hypertension during pregnancy. Cochrane Database of Systematic Reviews. 2003, CD002863-3
Matchaba P, Moodley J: Corticosteroids for HELLP syndrome in pregnancy. Cochrane Database of Systematic Reviews. 2004, CD002076-1
Meher S, Abalos E, Carroli G: Bed rest with or without hospitalisation for hypertension during pregnancy. Cochrane Database of Systematic Reviews. 2005, CD003514-4
Orton L, Garner P: Drugs for treating uncomplicated malaria in pregnant women. Cochrane Database of Systematic Reviews. 2005, CD004912-3
Quijano CE, Abalos E: Conservative management of symptomatic and/or complicated haemorrhoids in pregnancy and the puerperium. Cochrane Database of Systematic Reviews. 2005, CD004077-3
Rumbold A, Duley L, Crowther C, Haslam R: Antioxidants for preventing pre-eclampsia. Cochrane Database of Systematic Reviews. 2005, CD004227-4
Smaill F: Antibiotics for asymptomatic bacteriuria in pregnancy. Cochrane Database of Systematic Reviews. 2001, CD000490-2
Tuffnell DJ, West J, Walkinshaw SA: Treatments for gestational diabetes and impaired glucose tolerance in pregnancy. Cochrane Database of Systematic Reviews. 2003, CD003395-3
Vazquez JC, Villar J: Treatments for symptomatic urinary tract infections during pregnancy. Cochrane Database of Systematic Reviews. 2003, CD002256-4
Walker GJ: Antibiotics for syphilis diagnosed during pregnancy. Cochrane Database of Systematic Reviews. 2001, CD001143-3
Walker MC, Ferguson SE, Allen VM: Heparin for pregnant women with acquired or inherited thrombophilias. Cochrane Database of Systematic Reviews. 2003, CD003580-2
Webb RT, Howard L, Abel KM: Antipsychotic drugs for non-affective psychosis during pregnancy and postpartum. Cochrane Database of Systematic Reviews. 2004, CD004411-2
Young G, Jewell D: Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database of Systematic Reviews. 2002, CD001139-1
Young G, Jewell D: Topical treatment for vaginal candidiasis (thrush) in pregnancy. Cochrane Database of Systematic Reviews. 2001, CD000225-4
Young G, Jewell D: Interventions for leg cramps in pregnancy. Cochrane Database of Systematic Reviews. 2002, CD000121-1
Boath E, Bradley E, Henshaw C, Boath E: The prevention of postnatal depression: a narrative systematic review. Journal of Psychosomatic Obstetrics & Gynecology. 2005, 26 (3): 185-192. 10.1080/01674820400028431.
Brien T, Ray JG, Chan WS: Maternal body mass index and the risk of pre eclampsia: a systematic overview. Epidemiology. 2003, 14 (3): 368-374. 10.1097/00001648-200305000-00020.
Brody SC, Harris R, Lohr K: Screening for gestational diabetes: a summary of the evidence for the U.S. Preventive Services Task Force. Obstetrics & Gynecology. 2003, 101 (2): 380-392. 10.1016/S0029-7844(02)03057-0.
Beck CT: Predictors of postpartum depression: an update. Nursing Research. 2001, 50 (5): 275-285. 10.1097/00006199-200109000-00004.
Austin MP, Priest SR: Clinical issues in perinatal mental health: new developments in the detection and treatment of perinatal mood and anxiety disorders. Acta Psychiatrica Scandinavica. 2005, 112 (2): 97-104. 10.1111/j.1600-0447.2005.00549.x.
Beck CT: Postpartum depression: a metasynthesis. Qualitative Health Research. 2002, 12 (4): 453-472. 10.1177/104973202129120016.
Coomarasamy A, Papaioannou S, Gee H, Khan KS: Aspirin for the prevention of preeclampsia in women with abnormal uterine artery Doppler: a meta-analysis. Obstetrics & Gynecology. 2001, 98 (5 Pt 1): 861-866. 10.1016/S0029-7844(01)01569-1.
Coomarasamy A, Honest H, Papaioannou S, Gee H, Khan KS: Aspirin for prevention of preeclampsia in women with historical risk factors: a systematic review. Obstetrics & Gynecology. 2003, 101 (6): 1319-1332. 10.1016/S0029-7844(03)00169-8.
Conde-Agudelo A, Villar J, Lindhmeimer M: World health organization syustematic review of screening tests for pre eclampsia. Obstetrics & Gynecology. 2004, 104: 1367-1391.
Dennis CL: Preventing postpartum depression part II: A critical review of nonbiological interventions. Canadian Journal of Psychiatry – Revue Canadienne de Psychiatrie. 2004, 49 (8): 526-538.
Dennis CL: Preventing postpartum depression part I: a review of biological interventions. Canadian Journal of Psychiatry – Revue Canadienne de Psychiatrie. 2004, 49 (7): 467-475.
Duckitt K, Harrington D: Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies. BMJ. 2005, 330 (7491): 565-10.1136/bmj.38380.674340.E0.
Eberhard-Gran M, Eskild A, Tambs K, Opjordsmoen S, Samuelsen SO: Review of validation studies of the Edinburgh Postnatal Depression Scale. Acta Psychiatrica Scandinavica. 2001, 104 (4): 243-249. 10.1034/j.1600-0447.2001.00187.x.
Gluck JC, Gluck PA: Asthma controller therapy during pregnancy. American Journal of Obstetrics & Gynecology. 2005, 192 (2): 369-380. 10.1016/j.ajog.2004.07.056.
Goodman JH: Postpartum depression beyond the early postpartum period. JOGNN – Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2004, 33 (4): 410-420. 10.1177/0884217504266915.
Greer IA, Nelson-Piercy C: Low-molecular-weight heparins for thromboprophylaxis and treatment of venous thromboembolism in pregnancy: a systematic review of safety and efficacy. Blood. 2005, 106 (2): 401-407. 10.1182/blood-2005-02-0626.
Kujovich JL: Thrombophilia and pregnancy complications. American Journal of Obstetrics and Gynecology. 2004, 191: 412-424. 10.1016/j.ajog.2004.03.001.
Kosmas IP, Tatsioni A, Ioannidis JP: Association of Leiden mutation in factor V gene with hypertension in pregnancy and pre-eclampsia: a meta-analysis. Journal of Hypertension. 2003, 21 (7): 1221-1228. 10.1097/00004872-200307000-00002.
Kosmas IP, Tatsioni A, Ioannidis JP: Association of C677T polymorphism in the methylenetetrahydrofolate reductase gene with hypertension in pregnancy and pre-eclampsia: a meta-analysis. Journal of Hypertension. 2004, 22 (9): 1655-1662. 10.1097/00004872-200409000-00004.
Kovalevsky G, Clarisa R, Gracia R, Jesse AB, Mary DS, Kurt TB: Evaluation of the association between hereditary thrombophilias and recurrent pregnancy loss: a meta-analysis. Archives Internal Medicine. 2004, 164: 558-562. 10.1001/archinte.164.5.558.
Kwon HL, Belanger K, Bracken MB: Effect of pregnancy and stage of pregnancy on asthma severity: a systematic review. American Journal of Obstetrics & Gynecology. 2004, 190 (5): 1201-1210. 10.1016/j.ajog.2003.09.057.
Lassere M, Empson M: Treatment of antiphospholipid syndrome in pregnancy – a systematic review of randomized therapeutic trials. Thrombosis Research. 2004, 114 (5–6): 419-426. 10.1016/j.thromres.2004.08.006.
Magee LA, Cham C, Waterman EJ, Ohlsson A, von DP: Hydralazine for treatment of severe hypertension in pregnancy: meta-analysis. BMJ. 2003, 327 (7421): 955-960. 10.1136/bmj.327.7421.955.
Magee LA, Bull SB, Koren G, Logan A: The generalizability of trial data; a comparison of β-blockers in pregnancy. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2001, 94: 205-210. 10.1016/S0301-2115(00)00331-6.
Murphy VE, Clifton VL, Gibson PG: Asthma exacerbations during pregnancy: incidence and association with adverse pregnancy outcomes. Thorax. 2006, 61 (2): 169-176. 10.1136/thx.2005.049718.
Rayburn WF, Bogenschutz MP: Pharmacotherapy for pregnant women with addictions. American Journal of Obstetrics & Gynecology. 2004, 191 (6): 1885-1897. 10.1016/j.ajog.2004.06.082.
Scott DA, Loveman E, McIntyre L, Waugh N: Screening for gestational diabetes: a systematic review and economic evaluation. Health Technology Assessment. 2002, 6 (11): 1-161.
Austin MP, Lumley J: Antenatal screening for postnatal depression: a systematic review. Acta Psychiatrica Scandinavica. 2003, 107 (1): 10-17. 10.1034/j.1600-0447.2003.02024.x.
Austin MP: Targeted group antenatal prevention of postnatal depression: a review. Acta Psychiatrica Scandinavica. 2003, 107 (4): 244-250. 10.1034/j.1600-0447.2003.00086.x.
Egger M, Smith GD: Meta-analysis bias in location and selection of studies. BMJ. 1998, 316: 61-66.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1741-7015/5/10/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
LS conducted the search, extracted data and drafted the initial version. SJ performed data extraction. ST performed statistical analysis. ST, MK and KSK drafted and approved the final version.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Sheikh, L., Johnston, S., Thangaratinam, S. et al. A review of the methodological features of systematic reviews in maternal medicine. BMC Med 5, 10 (2007). https://doi.org/10.1186/1741-7015-5-10
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1741-7015-5-10