Abstract
Background
The United States Preventive Services Task Force (USPSTF) recommends screening adults for depression in primary care settings when staff-assisted depression management programs are available. This recommendation, however, is based on evidence from depression management programs conducted with patients already identified as depressed, even though screening is intended to identify depressed patients not already recognized or treated. The objective of this systematic review was to evaluate whether there is evidence from randomized controlled trials (RCTs) that depression screening benefits patients in primary care, using an explicit definition of screening.
Methods
We re-evaluated RCTs included in the 2009 USPSTF evidence review on depression screening, including only trials that compared depression outcomes between screened and non-screened patients and met the following three criteria: determined patient eligibility and randomized prior to screening; excluded patients already diagnosed with a recent episode of depression or already being treated for depression; and provided the same level of depression treatment services to patients identified as depressed in the screening and non-screening trial arms. We also reviewed studies included in a recent Cochrane systematic review, but not the USPSTF review; conducted a focused search to update the USPSTF review; and reviewed trial registries.
Results
Of the nine RCTs included in the USPSTF review, four fulfilled none of three criteria for a test of depression screening, four fulfilled one of three criteria, and one fulfilled two of three criteria. There were two additional RCTs included only in the Cochrane review, and each fulfilled one of three criteria. No eligible RCTs were found via the updated review.
Conclusions
The USPSTF recommendation to screen adults for depression in primary care settings when staff-assisted depression management programs are available is not supported by evidence from any RCTs that are directly relevant to the recommendation. The USPSTF should re-evaluate this recommendation.
Please see related article: http://www.biomedcentral.com/1741-7015/12/14
Registration
PROSPERO (#CRD42013004276)
Similar content being viewed by others
Background
Screening for depression in primary care settings is controversial [1–3]. Prior to 2002, no major guidelines recommended depression screening. Then, in 2002, the United States Preventive Services Task Force (USPSTF) recommended routine depression screening when staff-assisted depression care programs are in place to ensure accurate diagnosis and effective treatment and follow-up [4]. In 2009, the USPSTF reiterated this recommendation, based on evidence from nine randomized controlled trials (RCTs) [5, 6].
By contrast, a 2008 Cochrane review [7, 8] reported that the effect of depression screening on depressive symptoms in five RCTs was virtually zero (standardized mean difference = -0.02, 95% confidence interval -0.25 to 0.20) [7]. Consistent with this, in 2010, the UK National Institute for Health and Care Excellence recommended that clinicians be alert to possible depression, but not screen [9]. In 2013, the Canadian Task Force on Preventive Health Care similarly recommended against routine depression screening [10].
Existing systematic reviews on depression screening have been criticized for not defining the characteristics of depression screening trials [11, 12]. Depression screening involves the use of depression symptom questionnaires to identify patients who may have depression but have not sought treatment and have not otherwise been recognized as depressed by healthcare providers. For screening to benefit patients, patients must agree to be screened, the screening test must accurately identify a significant number of previously unrecognized patients, and clinicians must engage these patients in treatment and obtain sufficiently positive results to justify costs and potential harms [3].
A trial of depression screening must be able to separate the effect of screening from the effect of providing additional treatment resources not otherwise available. In addition to screening, depression symptom questionnaires may be used for tracking symptom severity or detecting relapse among patients with already-recognized depression. However, in a trial, only patients not already under care for depression prior to the trial should be included in assessing the effect of screening, since screening is done to identify previously unrecognized cases. Thus, for a trial to test the effects of depression screening on depression outcomes, at least three key criteria must be fulfilled. The trial must:
-
1.
determine patient eligibility and randomize patients prior to screening;
-
2.
exclude patients already diagnosed with a recent episode of depression or being treated for depression at the time of trial enrollment;
-
3.
provide similar depression management options to patients with depression in the screening arm of the trial and patients in the non-screening arm identified as depressed via other mechanisms, such as patient report or unaided physician diagnosis.
The 2009 USPSTF systematic review [5, 6] did not explicitly define characteristics of a screening trial. The 2008 Cochrane review [7, 8] excluded trials where depression care was substantially enhanced for patients in the intervention group only, but did not require randomization prior to screening or address the inclusion of already-treated patients.
The objective of the present systematic review was to determine whether the USPSTF depression screening guideline is supported by evidence that depression screening improves depression outcomes in primary care. To do this, we re-evaluated the nine RCTs included in the 2009 USPSTF systematic review on depression screening [5, 6] to determine if they fulfilled the three key criteria necessary for a test of depression screening. In addition, we reviewed trials included in the 2008 Cochrane review [7, 8] and conducted a focused search to determine if any depression screening trials have been conducted since those reviews.
Methods
Methods for this systematic review were registered in the PROSPERO prospective register of systematic reviews (#CRD42013004276).
Identification of eligible RCTs from the 2009 USPSTF and Cochrane systematic reviews
We evaluated nine RCTs from the USPSTF 2009 review and two additional RCTs that were included in one or both published versions of a Cochrane review [7, 8] but not the USPSTF review. Eligible RCTs had to use a depression screening tool with a defined cut-off score to make decisions regarding further assessment or treatment of depression. In addition, patient eligibility and randomization had to occur prior to administering the screening test; patients with a recent diagnosis of depression and patients being treated for depression close to the time of trial enrollment had to have been excluded from the trial; and similar depression management resources had to have been available to patients identified as depressed in both trial arms. We included RCTs that compared depression symptom outcomes or, if not available, number of cases post-screening, but not RCTs that only reported rates of depression recognition or treatment. This is because recommendations for screening should be based on evidence of improved outcomes. Increased treatment without improved depression outcomes would expose patients to costs and potential harms but not benefit [3].
Two investigators independently reviewed full-text publications of RCTs from the USPSTF and Cochrane reviews with any disagreements resolved by consensus.
Updated search
We searched for RCTs from any country that met eligibility criteria. The focused database search was designed based on a surveillance technique found to be the most effective method for finding new evidence to update systematic reviews in a comparison of several different methods [13]. It involved using a combination of two separate search strategies. The first was a subject search in the MEDLINE database using relevant Medical Subject Headings and text words. The second search was a ‘related citations’ search in PubMed based on the three most recent and three largest trials included in either the USPSTF or Cochrane reviews, only including studies that were described in the original publications as related to screening. Both searches were limited to RCTs by using a validated methodological hedge. The search was peer-reviewed prior to implementation on 24 April 2013, using the Ovid SP interface for MEDLINE (search 1) and the National Library of Medicine interface, PubMed (search 2). See Additional file 1.
We also searched the ClinicalTrials.gov trial registry (‘depression AND screen*’ in any field, where * retrieves terms with zero to more characters) and the World Health Organization International Clinical Trials Registry Platform (‘depression AND screen*’ in the ‘title’ field) from inception to 30 April 2013. The World Health Organization registry platform is a central database that provides access to many different clinical trial registries from around the world.
The updated review was similarly done independently by two investigators.
Data presentation and synthesis
Since we did not identify any trials that met all three criteria necessary for tests of depression screening, synthesis of outcome data on the effect of depression screening was not possible. Instead, we reported the results of our evaluation to determine if RCTs from the USPSTF and Cochrane reviews or the updated search fulfilled the three criteria. We did not conduct an assessment of trial quality or risk of bias because no trials met criteria to be considered a test of depression screening. Two investigators independently extracted data with any disagreement resolved by consensus.
Results
Re-assessment of randomized controlled trials from 2009 USPSTF and Cochrane systematic reviews
As shown in Table 1, there were five RCTs [14–18] included in only the USPSTF review, four [19–22] included in both the USPSTF and Cochrane reviews, and two [23, 24] included in at least one version of the Cochrane review, as well as a 2002 version of the USPSTF review [25] but not the 2009 USPSTF review. Of the 11 RCTs included in either the 2009 USPSTF or Cochrane reviews, one [20] fulfilled two of the three key criteria for a depression screening trial, six [16, 17, 21–24] fulfilled one, and four [14, 15, 18, 19] did not fulfill any. Of the 11 RCTs, only two [20, 21] determined trial eligibility and randomized prior to screening; only two [16, 17] excluded already diagnosed and treated patients; and only four [20, 22–24] provided similar depression management options to patients in both trial arms.
Of the five RCTs [14–18] that were included in the USPSTF review but not the Cochrane review, four [14–17] were trials of complex depression care quality improvement programs and required a positive score on a depression screening tool plus a diagnosis of depression for enrolment. The other RCT [18], also a complex management intervention, was excluded from the Cochrane review because it was not specific to depression. For eligibility, elderly patients were required to have four of ten problems indicative of a potentially poor general prognosis, but not necessarily depression.
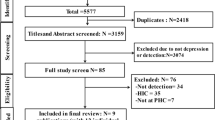
Results from the updated search
The trial registration search included 405 unique trial registrations, but none described RCTs that met eligibility criteria. The database search identified 347 unique citations, of which 342 were excluded after title and abstract review and five after full-text review (Figure 1). Of the five studies that underwent full-text review, two studies were clearly not relevant, and three RCTs [30–32] were similar in design to trials included in the USPSTF or Cochrane reviews and met at least one criterion (see Table 1). Of these three RCTs, one [30] met one, and two [31, 32] met two of the three criteria.
Randomized controlled trials that randomized patients prior to screening
Among RCTs included in the USPSTF or Cochrane reviews or identified in the updated search, only four [20, 21, 31, 32] determined eligibility and randomized patients prior to screening. Among those, one [31] provided enhanced depression care to only patients in the screening arm, which did not allow an assessment of the effect of screening. Another [21] randomized patients to physician notification of positive screens versus usual care. Intervention arm patients with positive depression screens were offered six weekly depression education sessions, although only 12% of eligible patients attended. Outcome data were analyzed from only the 14% of patients in the trial with positive screening scores at baseline, including patients on antidepressants pre-trial. There were no significant differences in the mean change of depression symptoms between groups (-2.4 versus -2.1 points on Geriatric Depression Scale, P = 0.50).
Two trials [20, 32] met two of the three criteria, but included already diagnosed or treated patients. One [20] analyzed data from only 23% of patients randomized, including patients determined to have major depression at baseline plus a small sample of patients without major depression at baseline. Only 27% of depression diagnoses post-screening were new diagnoses, and the mean reduction in the number of depressive symptoms did not differ between the two groups (1.6 versus 1.5 symptoms, P = 0.21). The other [32] was a cluster RCT in which primary care practices were randomized to screen versus provide usual care to patients at high risk of depression due to a history of depression, unexplained somatic symptoms, psychological comorbidities, drug abuse or chronic pain. The number of patients already treated pre-trial was not reported. Rates of depression post-screening were similar in the screening (15.0%) and usual care (15.8%) trial arms.
Discussion
The main finding of this systematic review was that no RCTs have compared depression outcomes between patients randomized to be screened versus not screened for depression in trials that met the necessary criteria: determined eligibility and randomized patients prior to screening; excluded patients already known to have depression or already being treated for depression; and provided similar depression management options to patients identified as depressed via screening or via other methods in the comparison group.
The 2009 USPSTF recommendation to screen when collaborative care depression management programs are available was based primarily on the results of three trials [14, 15, 18]. Two of these trials [14, 15] compared complex collaborative care depression management programs to usual care among patients required to have depression to enroll in the trials. In one of the trials, 44% of enrolled patients were described as receiving appropriate mental health care in the 6 months prior to trial enrollment [14]. In the other, 44% of enrolled patients were prescribed antidepressant medication or had a specialty mental health care visit in the 6 months prior to enrolling in the trial [15]. The third trial tested whether telephone case management improved a series of geriatric outcomes (depression, cognitive impairment, urinary incontinence, falls, functional impairment) among elderly patients determined to be at risk for poor health outcomes prior to trial enrollment, most of whom did not report symptoms of depression [18]. None of these trials met any of the three criteria used in the present systematic review to characterize trials of depression screening programs.
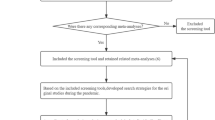
The trials that were used to support the USPSTF recommendation provided evidence that collaborative care programs improve outcomes compared to usual care for patients already identified as depressed. They did not, however, address the question of whether screening improves outcomes for patients who would not otherwise be identified as depressed in the context of these programs. To address this question, RCTs are needed that randomize primary care practices to screen patients for depression versus not screening them. All patients in either trial arm who are identified as depressed via screening or other mechanisms, such as unaided clinician recognition or patient report, should be provided with the same depression care to determine whether screening is linked to improved depression outcomes in the context of depression care of similar quality (Figure 2).
Without such evidence, the USPSTF should consider several factors that suggest that depression screening, even in the context of collaborative depression care, may not be straightforward or effective, and may, in fact, expose some patients to avoidable risk. These factors have been discussed in detail elsewhere [3], but include the already high rate of antidepressant use in primary care settings [33, 34]; the likely overestimation in the research literature of the accuracy of depression screening tools for identifying previously unrecognized cases of depression [35]; and the limited effectiveness of antidepressant medication among patients with only mild symptoms of depression [36–41], including patients without obvious depression who would likely be identified via screening.
Although it is not clear that depression screening would improve depression outcomes, it would harm some patients [42]. Most patients treated for depression in primary care are treated with antidepressants [43], and common side effects include diarrhea, dizziness, dry mouth, fatigue, headache, nausea, sexual dysfunction, excessive sweating, tremors and weight gain [44]. Less common but potentially more serious adverse effects, particularly for patients in primary care with heart disease, may include increased risk of bleeding and unwanted effects on blood pressure and heart rate [45–49], as well as drug-drug interactions with cardiac medications [50, 51]. For patients with generally low levels of depression, who are most likely to be newly identified through screening, the side effect burden and potential risk profile of antidepressants need to be carefully considered, particularly given that screening has not been shown to reduce symptoms of depression.
Screening would also consume scarce healthcare resources [52, 53] that will not then be available for other activities, such as providing treatment to the large number of patients already diagnosed with depression but receiving poor-quality care. Canadian healthcare costs are generally lower than those in the US. Nonetheless, a recent population-based study from the province of Quebec found that overall healthcare costs were approximately $2,000 (CAD) higher for patients prescribed antidepressants, with a large proportion of increased costs attributed to patients without a recent history of depression or anxiety [54]. The cost of treatment, however, is only part of the cost of screening. Beyond administering depression symptom questionnaires, the cost of depression screening would include follow-up assessments to determine which patients are true positive screens and which are false positives; consultations with patients who are identified as having depression to determine management options and, if treatment is advised, the best treatment option; as well as treatment and follow-up services. The USPSTF guideline does not specify how often patients should be screened, and we do not know of any studies that have examined cumulative false positive rates from repeat screenings, but this is an important factor that needs to be considered.
Recommendations have been made for depression screening of special patient populations, including postpartum women [55] and patients with heart disease [56]. However, these recommendations are controversial [57, 58] and not supported by evidence of benefit from RCTs [59–62]. In the UK, depression screening in primary care of patients with heart disease and diabetes was incentivized from 2006 to 2013. An analysis of more than a million patient records from Scottish primary care practices, however, found that almost 1,000 screens were necessary for a new depression diagnosis and almost 700 for a new antidepressant prescription [63]. In the US, at least 10 states have legislation encouraging or requiring postpartum depression screening [64]. Although no depression outcomes have been reported, a study of the first of these programs to be initiated, the New Jersey Postpartum Wellness Initiative, which has required postpartum depression screening since 2006, did not find any increase in depression treatment or follow-up care following implementation [64].
The only RCT in the present review that screened high-risk patients [32] did not find that screening reduced the presence of depression, although it is not known what proportion of patients in the trial were receiving treatment for depression pre-trial. One prospective cohort study from the Netherlands [65] documented the results of a program designed to screen and provide collaborative depression care for primary care patients with a history of mental health problems, unexplained somatic complaints, or a high level of service utilization. In that study, 1,687 patients were sent a screening questionnaire and letter from their general practitioner: 780 returned the screening questionnaire and 226 screened positive, but only 17 patients were newly diagnosed with depression and attended even one session of the offered treatment. Depression outcomes were not reported.
The present systematic review is a focused update of existing systematic reviews and did not include a complete search as in earlier reviews. Therefore, it is possible that we could have missed eligible trials. However, the updating method that we used has been validated as highly sensitive [16], and the likelihood that we have missed eligible studies that would have changed results appears to be very low.
Conclusions
We did not find any directly relevant evidence from RCTs to support the USPSTF recommendation to screen patients for depression in primary care when staff-assisted, collaborative depression care programs are in place. This result is consistent with recent guidelines from the UK [9] and Canada [10] that concluded that routine depression screening is not supported by existing evidence. Our results differ from those of a 2008 Cochrane review [7, 8], which reported that depression screening is not effective based on evidence from five trials by clarifying that there have not been any well-designed trials to directly address the question of whether depression screening may be effective, particularly in the context of collaborative care. RCTs of depression screening that are designed to directly assess whether screening of previously unidentified patients will reduce rates of depression are needed.
Over-diagnosis and over-treatment of depression are common in community and primary care settings in the US [66–68], and there is a real risk that depression screening could exacerbate this problem without contributing to better mental health. We hope that the USPSTF will re-evaluate evidence on depression screening, applying the three basic criteria that we have used in this review. Before screening for depression is recommended, there should be evidence of improved depression outcomes from well-conducted depression RCTs that are directly relevant to the question of screening.
Although our findings show that there is not enough evidence to recommend that healthcare practitioners use screening to attempt to identify patients who may have depression, depression is a disabling condition with a major impact on quality of life. Thus, clinicians should be aware of signs that depression may be present, such as low mood, loss of interest in activities, insomnia and fatigue [10]. Healthcare practitioners should be particularly vigilant among patients who may be at high risk of depression, including patients with a chronic medical condition, a past history of depression, a pattern of unexplained somatic symptoms and frequent use of medical services, or substance abuse [9, 10, 32, 65].
Abbreviations
- RCT:
-
Randomized controlled trial
- USPSTF:
-
United States Preventive Services Task Force.
References
Palmer SC, Coyne JC: Screening for depression in medical care: pitfalls, alternatives, and revised priorities. J Psychosom Res. 2003, 54: 279-287. 10.1016/S0022-3999(02)00640-2.
Gilbody S, Sheldon T, Wessely S: Should we screen for depression?. BMJ. 2006, 332: 1027-1030. 10.1136/bmj.332.7548.1027.
Thombs BD, Coyne JC, Cuijpers P, de Jonge P, Gilbody S, Ioannidis JP, Johnson BT, Patten SB, Turner EH, Ziegelstein RC: Rethinking recommendations for screening for depression in primary care. CMAJ. 2012, 184: 413-418. 10.1503/cmaj.111035.
US Preventive Services Task Force: Screening for depression: recommendations and rationale. Ann Intern Med. 2002, 136: 760-764.
O’Connor EA, Whitlock EP, Gaynes B, Beil TL: AHRQ Publication No. 10-05143-EF-1. Screening for depression in adults and older adults in primary care: an updated systematic review. Evidence Synthesis No. 75. 2009, Rockville, MD: Agency for Healthcare Research and Quality
O’Connor EA, Whitlock EP, Beil TL, Gaynes BN: Screening for depression in adult patients in primary care settings: a systematic evidence review. Ann Intern Med. 2009, 151: 793-803. 10.7326/0003-4819-151-11-200912010-00007.
Gilbody SD, Sheldon TA, House AD: Screening and case-finding instruments for depression: a meta-analysis. CMAJ. 2008, 178: 997-1003. 10.1503/cmaj.070281.
Gilbody S, House AO, Sheldon TA: Screening and case finding instruments for depression. Cochrane Database Syst Rev. 2005, 4: CD002792.
National Collaborating Center for Mental Health: The NICE guideline on the management and treatment of depression in adults (Updated edition). 2010, Manchester, UK: NICE
Joffres M, Jaramillo A, Dickinson J, Lewin G, Pottie K, Shaw E, Connor Gorber S, Tonelli M, Canadian Task Force on Preventive Health Care: Recommendations on screening for depression in adults. CMAJ. 2013, 185: 775-782.
Goodyear-Smith FA, van Driel ML, Arroll B, Del Mar C: Analysis of decisions made in meta-analyses of depression screening and the risk of confirmation bias: a case study. BMC Med Res Methodol. 2012, 12: 76-2288-12-76.
Bland RC, Streiner DL: Why screening for depression in primary care is impractical. CMAJ. 2013, 185: 753-754. 10.1503/cmaj.130634.
Sampson M, Shojania KG, McGowan J, Daniel R, Rader T, Iansavichene AE, Ji J, Ansari MT, Moher D: Surveillance search techniques identified the need to update systematic reviews. J Clin Epidemiol. 2008, 61: 755-762. 10.1016/j.jclinepi.2007.10.003.
Wells KB, Sherbourne C, Schoenbaum M, Duan N, Meredith L, Unutzer J, Miranda J, Carney MF, Rubenstein LV: Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA. 2000, 283: 212-220. 10.1001/jama.283.2.212.
Rost K, Nutting P, Smith J, Werner J, Duan N: Improving depression outcomes in community primary care practice: a randomized trial of the quEST intervention. Quality Enhancement by Strategic Teaming. J Gen Intern Med. 2001, 16: 143-149. 10.1111/j.1525-1497.2001.00537.x.
Jarjoura D, Polen A, Baum E, Kropp D, Hetrick S, Rutecki G: Effectiveness of screening and treatment for depression in ambulatory indigent patients. J Gen Intern Med. 2004, 19: 78-84. 10.1111/j.1525-1497.2004.21249.x.
Bosmans J, de Bruijne M, van Hout H, van Marwijk H, Beekman A, Bouter L, Stalman W, van Tulder M: Cost-effectiveness of a disease management program for major depression in elderly primary care patients. J Gen Intern Med. 2006, 21: 1020-1026. 10.1111/j.1525-1497.2006.00555.x.
Rubenstein LZ, Alessi CA, Josephson KR, Trinidad Hoyl M, Harker JO, Pietruszka FM: A randomized trial of a screening, case finding, and referral system for older veterans in primary care. J Am Geriatr Soc. 2007, 55: 166-174. 10.1111/j.1532-5415.2007.01044.x.
Callahan CM, Hendrie HC, Dittus RS, Brater DC, Hui SL, Tierney WM: Improving treatment of late life depression in primary care: a randomized clinical trial. J Am Geriatr Soc. 1994, 42: 839-846.
Williams JW, Mulrow CD, Kroenke K, Dhanda R, Badgett RG, Omori D, Lee S: Case-finding for depression in primary care: a randomized trial. Am J Med. 1999, 106: 36-43. 10.1016/S0002-9343(98)00371-4.
Whooley MA, Stone B, Soghikian K: Randomized trial of case-finding for depression in elderly primary care patients. J Gen Intern Med. 2000, 15: 293-300. 10.1046/j.1525-1497.2000.04319.x.
Bergus GR, Hartz AJ, Noyes R, Ward MM, James PA, Vaughn T, Kelley PL, Sinift SD, Bentler S, Tilman E: The limited effect of screening for depressive symptoms with the PHQ-9 in rural family practices. J Rural Health. 2005, 21: 303-309. 10.1111/j.1748-0361.2005.tb00099.x.
Dowrick C: Does testing for depression influence diagnosis or management by general practitioners?. Fam Pract. 1995, 12: 461-465. 10.1093/fampra/12.4.461.
Lewis G, Sharp D, Bartholomew J, Pelosi AJ: Computerized assessment of common mental disorders in primary care: effect on clinical outcome. Fam Pract. 1996, 13: 120-126. 10.1093/fampra/13.2.120.
Pignone MP, Gaynes BN, Rushton JL, Burchell CM, Orleans CT, Mulrow CD, Lohr KN: Screening for depression in adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002, 136: 765-776. 10.7326/0003-4819-136-10-200205210-00013.
Dowrick C, Buchan I: Twelve month outcome of depression in general practice: does detection or disclosure make a difference?. BMJ. 1995, 311: 1274-1276. 10.1136/bmj.311.7015.1274.
Wells K, Sherbourne C, Schoenbaum M, Ettner S, Duan N, Miranda J, Unutzer J, Rubenstein L: Five-year impact of quality improvement for depression: results of a group-level randomized controlled trial. Arch Gen Psychiatry. 2004, 61: 378-386. 10.1001/archpsyc.61.4.378.
Rost K, Nutting PA, Smith J, Werner JJ: Designing and implementing a primary care intervention trial to improve the quality and outcome of care for major depression. Gen Hosp Psychiatry. 2000, 22: 66-77. 10.1016/S0163-8343(00)00059-1.
Rost K, Nutting P, Smith JL, Elliott CE, Dickinson M: Managing depression as a chronic disease: a randomised trial of ongoing treatment in primary care. BMJ. 2002, 325: 934-10.1136/bmj.325.7370.934.
Yeung A, Shyu I, Fisher L, Wu S, Yang H, Fava M: Culturally sensitive collaborative treatment for depressed Chinese Americans in primary care. Am J Public Health. 2010, 100: 2397-2402. 10.2105/AJPH.2009.184911.
Yawn BP, Dietrich AJ, Wollan P, Bertram S, Graham D, Huff J, Kurland M, Madison S, Pace WD, TRIPPD practices: TRIPPD: a practice-based network effectiveness study of postpartum depression screening and management. Ann Fam Med. 2012, 10: 320-329. 10.1370/afm.1418.
Romera I, Montejo AL, Aragones E, Arbesu JA, Iglesias-Garcia C, Lopez S, Lozano JA, Pamulapati S, Yruretagoyena B, Gilaberte I: Systematic depression screening in high-risk patients attending primary care: a pragmatic cluster-randomized trial. BMC Psychiatry. 2013, 13: 83-244X-13-83.
Olfson M, Marcus SC: National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009, 66: 848-856. 10.1001/archgenpsychiatry.2009.81.
Mojtabai R, Olfson M: National patterns in antidepressant treatment by psychiatrists and general medical providers: results from the National Comorbidity Survey replication. J Clin Psychiatry. 2008, 69: 1064-1074. 10.4088/JCP.v69n0704.
Thombs BD, Arthurs E, El-Baalbaki G, Meijer A, Ziegelstein RC, Steele R: Risk of bias from inclusion of already diagnosed or treated patients in diagnostic accuracy studies of depression screening tools: A systematic review. BMJ. 2011, 343: d4825-10.1136/bmj.d4825.
Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT: Initial severity and antidepressant benefits: a meta-analysis of data submitted to the Food and Drug Administration. PLoS Med. 2008, 5: e45-10.1371/journal.pmed.0050045.
Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, Fawcett J: Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010, 303: 47-53. 10.1001/jama.2009.1943.
Barbui C, Cipriani A, Patel V, Ayuso-Mateos JL, van Ommeren M: Efficacy of antidepressants and benzodiazepines in minor depression: systematic review and meta-analysis. Br J Psychiatry. 2011, 198: 11-16. 10.1192/bjp.bp.109.076448.
Khan A, Leventhal RM, Khan SR, Brown WA: Severity of depression and response to antidepressants and placebo: an analysis of the Food and Drug Administration database. J Clin Psychopharmacol. 2002, 22: 40-45. 10.1097/00004714-200202000-00007.
Khin NA, Chen YF, Yang Y, Yang P, Laughren TP: Exploratory analyses of efficacy data from major depressive disorder trials submitted to the US Food and Drug Administration in support of new drug applications. J Clin Psychiatry. 2011, 72: 464-472. 10.4088/JCP.10m06191.
Driessen E, Cuijpers P, Hollon SD, Dekker JJ: Does pretreatment severity moderate the efficacy of psychological treatment of adult outpatient depression? A meta-analysis. J Consult Clin Psychol. 2010, 78: 668-680.
U.S. Preventive Services Task Force: Screening for depression in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2009, 151: 784-792.
Marcus SC, Olfson M: National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010, 67: 1265-1273. 10.1001/archgenpsychiatry.2010.151.
Gartlehner G, Hansen RA, Morgan LC, Thaler K, Lux L, Van Noord M, Mager U, Thieda P, Gaynes BN, Wilkins T, Strobelberger M, Lloyd S, Reichenpfader U, Lohr KN: Comparative benefits and harms of second-generation antidepressants for treating major depressive disorder: an updated meta-analysis. Ann Intern Med. 2011, 155: 772-785. 10.7326/0003-4819-155-11-201112060-00009.
Labos C, Dasgupta K, Nedjar H, Turecki G, Rahme E: Risk of bleeding associated with combined use of selective serotonin reuptake inhibitors and antiplatelet therapy following acute myocardial infarction. CMAJ. 2011, 183: 1835-1843. 10.1503/cmaj.100912.
Schalekamp T, Klungel OH, Souverein PC, de Boer A: Increased bleeding risk with concurrent use of selective serotonin reuptake inhibitors and coumarins. Arch Intern Med. 2008, 168: 180-185. 10.1001/archinternmed.2007.32.
Schelleman H, Brensinger CM, Bilker WB, Hennessy S: Antidepressant-warfarin interaction and associated gastrointestinal bleeding risk in a case–control study. PLoS One. 2011, 6: e21447-10.1371/journal.pone.0021447.
Stahl SM, Grady MM, Moret C, Briley M: SNRIs: their pharmacology, clinical efficacy, and tolerability in comparison with other classes of antidepressants. CNS Spectr. 2005, 10: 732-747.
Licht CM, de Geus EJ, van Dyck R, Penninx BW: Longitudinal evidence for unfavorable effects of antidepressants on heart rate variability. Biol Psychiatry. 2010, 68: 861-868. 10.1016/j.biopsych.2010.06.032.
Spina E, Santoro V, D’Arrigo C: Clinically relevant pharmacokinetic drug interactions with second-generation antidepressants: an update. Clin Ther. 2008, 30: 1206-1227. 10.1016/S0149-2918(08)80047-1.
Goryachkina K, Burbello A, Boldueva S, Babak S, Bergman U, Bertilsson L: Inhibition of metoprolol metabolism and potentiation of its effects by paroxetine in routinely treated patients with acute myocardial infarction (AMI). Eur J Clin Pharmacol. 2008, 64: 275-282. 10.1007/s00228-007-0404-3.
Valenstein M, Vijan S, Zeber JE, Boehm K, Buttar A: The cost-utility of screening for depression in primary care. Ann Intern Med. 2001, 134: 345-360.
Paulden M, Palmer S, Hewitt C, Gilbody S: Screening for postnatal depression in primary care: cost effectiveness analysis. BMJ. 2009, 339: b5203-10.1136/bmj.b5203.
Vasiliadis HM, Latimer E, Dionne PA, Preville M: The costs associated with antidepressant use in depression and anxiety in community-living older adults. Can J Psychiatry. 2013, 58: 201-209.
National Institute for Clinical Excellence: Antenatal and postnatal mental health: clinical management and service guidance. 2007, London, UK: NICE
Whooley M: To screen or not to screen? Depression in patients with cardiovascular disease. J Am Coll Cardiol. 2009, 54: 891-893. 10.1016/j.jacc.2009.05.034.
Hill C: An evaluation of screening for postnatal depression against NSC criteria. 2010, UK: UK National Screening Committee
Ziegelstein RC, Thombs BD, Coyne JC, de Jonge P: Routine screening for depression in patients with coronary heart disease: never mind. J Am Coll Cardiol. 2009, 54: 886-890. 10.1016/j.jacc.2009.01.082.
Hewitt C, Gilbody S, Brealey S, Paulden M, Palmer S, Mann R, Green J, Morrell J, Barkham M, Light K, Richards D: Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis. Health Technol Assess. 2009, 13: 1-145, 147–230
Hewitt CE, Gilbody SM: Is it clinically and cost effective to screen for postnatal depression: a systematic review of controlled clinical trials and economic evidence. BJOG. 2009, 116: 1019-1027. 10.1111/j.1471-0528.2009.02148.x.
Thombs BD, de Jonge P, Coyne JC, Whooley MA, Frasure-Smith N, Mitchell AJ, Zuidersma M, Eze-Nliam C, Lima BB, Smith CG, Soderlund K, Ziegelstein RC: Depression screening and patient outcomes in cardiovascular care: a systematic review. JAMA. 2008, 300: 2161-2171. 10.1001/jama.2008.667.
Thombs BD, Roseman M, Coyne JC, de Jonge P, Delisle VC, Arthurs E, Levis B, Ziegelstein RC: Does evidence support the American Heart Association’s recommendation to screen patients for depression in cardiovascular care? An updated systematic review. PLoS One. 2013, 8: e52654-10.1371/journal.pone.0052654.
Burton C, Simpson C, Anderson N: Diagnosis and treatment of depression following routine screening in patients with coronary heart disease or diabetes: a database cohort study. Psychol Med. 2013, 43: 529-537. 10.1017/S0033291712001481.
Kozhimannil KB, Adams AS, Soumerai SB, Busch AB, Huskamp HA: New Jersey’s efforts to improve postpartum depression care did not change treatment patterns for women on Medicaid. Health Aff. 2011, 30: 293-301. 10.1377/hlthaff.2009.1075.
Baas KD, Wittkampf KA, van Weert HC, Lucassen P, Huyser J, van den Hoogen H, van de Lisdonk E, Bindels PE, Bockting CL, Ruhé HG, Schene AH: Screening for depression in high-risk groups: Prospective cohort study in general practice. Br J Psychiatry. 2009, 194: 399-403. 10.1192/bjp.bp.107.046052.
Mojtabai R, Olfson M: Proportion of antidepressants prescribed without a psychiatric diagnosis is growing. Health Aff. 2011, 30: 1434-1442. 10.1377/hlthaff.2010.1024.
Mojtabai R: Clinician-identified depression in community settings: concordance with structured-interview diagnoses. Psychother Psychosom. 2013, 82: 161-169. 10.1159/000345968.
Dowrick C, Frances A: Medicalising unhappiness: new classification of depression risks more patients being put on drug treatment from which they will not benefit. BMJ. 2013, 347: f7140-10.1136/bmj.f7140.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1741-7015/12/13/prepub
Acknowledgments
The authors are grateful to Margaret Sampson, MLIS, PhD, AHIP of the Children’s Hospital of Eastern Ontario, Ottawa, ON, Canada for consultation on the focused search strategy used in the study and for peer-reviewing the search strategy. BDT was supported by a New Investigator Award from the Canadian Institutes of Health Research. RCZ was supported by the Miller Family Scholar Program of the Johns Hopkins Center for Innovative Medicine. There was no specific funding for this study, and no funders had any role in the study design; in the collection, analysis and interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
BDT was responsible for the study concept and design; wrote the review protocol; contributed to the article review, selection and data extraction; contributed to the analysis, interpretation and presentation of data; and drafted the manuscript. RCZ contributed to the study concept and design; participated in data extraction; contributed to the analysis, interpretation and presentation of data; and provided a critical revision of the manuscript. MR contributed to the article review, selection and data extraction; contributed to the analysis, interpretation and presentation of data; and provided a critical revision of the manuscript. LAK designed and conducted the database searches and provided a critical revision of the manuscript. JPAI contributed to the study concept and design\ and to the analysis, interpretation and presentation of data, and provided a critical revision of the manuscript. All authors approved the final version of the manuscript.
Electronic supplementary material
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited.
About this article
Cite this article
Thombs, B.D., Ziegelstein, R.C., Roseman, M. et al. There are no randomized controlled trials that support the United States Preventive Services Task Force guideline on screening for depression in primary care: a systematic review. BMC Med 12, 13 (2014). https://doi.org/10.1186/1741-7015-12-13
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1741-7015-12-13