Abstract
Background
Physicians occupy an important position as tobacco control exemplars and their own smoking habits are known to influence how effective they may be in such a role.
Methods
A comprehensive review of all published manuscripts describing tobacco usage rates and tobacco control activities in the Australian medical profession between 1964 and 1997.
Results
Some of the earliest surveys revealed that around one-quarter of Australian physicians were smoking in the mid twentieth century, a rate which rapidly declined in the 1970s and 1980s, with reductions beyond that achieved by the general population.
Conclusion
Overall, our review suggests that not only do contemporary Australian physicians smoke at very low rates when compared internationally, but that an active professional community can also make a real difference to the lifestyle choices of its own members.
Similar content being viewed by others
Background
Tobacco control represents a key facet of public health. Worldwide, smoking is the second most common cause of death and the fourth most common risk factor for disease. If smoking trends continue at the current rate, tobacco will be causing approximately 10 million deaths per annum by the year 2020, with around 650 million fatalities overall [1]. Global tobacco control is therefore very important, a realization which led to the World Health Organization Framework Convention on Tobacco Control (WHO-FCTC), an evidence-based treaty focusing on demand reduction and tobacco supply issues from a global perspective [2]. At a local level, individual physicians and scientists have often been at the forefront of tobacco control, due to the now well-known links between smoking and ill-health, as well as the direct evidence of sick patients whom they treat in daily practice. Physicians themselves have also played a key role in tobacco research, with one of the earliest epidemiological studies linking tobacco smoking with adverse health outcomes being conducted among a group of British doctors [3]. So groundbreaking was the original investigation by Doll and colleagues that it was republished 50 years later [4] and remains a cornerstone of preventive medicine literature [5–7]. Being on the frontlines of primary health care, physicians have always occupied a key position in tobacco control and are often viewed as healthy lifestyle role models by their patients, their colleagues and the communities in which they live. As early as thirty years ago, it had been suggested that physicians would be more effective at persuading patients to quit smoking, if they themselves did not smoke [8].
Despite these facts, medical professionals have not always set a good example for patients with regard to smoking [9, 10]. In the early to mid 20th century for example, some tobacco companies even used physicians to help advertise their products [11, 12]. The relative success of certain campaigns in the United States (US) and Japan was most likely due to the fact that smoking rates among local physicians were reasonably high at the time. In the US for example, some of the earliest epidemiological research found that around 40% of physicians were smoking in 1959 [8], although their smoking rate had dropped dramatically by the 1980s [13]. A large study conducted in 1965 [14] revealed that 68% of male physicians in Western Japan were current smokers. By the mid to late 20th century however, physicians in many countries had begun to heed a growing body of scientific evidence linking smoking with ill health, and many active smokers among them had begun to quit [15]. As the medical profession was early to notice the dangers of tobacco use, the national smoking rate of physicians in the US, for example, fell dramatically during this time [16–18]. Tobacco use among their Japanese medical counterparts was also seen to decline last century [19], albeit at a less rapid rate than some of their Western counterparts. Regardless of what country they live in, the ongoing collection and interpretation of epidemiological data on smoking habits among physicians continues to serve at least two important functions relevant for tobacco control. Firstly, this kind of data can help predict how effective any potential anti-smoking campaigns in a given country may actually be [9]. That is, it would be difficult to convince the general public not to smoke if physicians continued to do so. Secondly, it allows policy makers to determine how 'mature' a country's smoking epidemic currently is, and thus, how soon the overall community prevalence rate might decline [9].
As a nation, Australia has set many positive examples in the field of tobacco control. It was one of the first countries to test the tar and nicotine content of cigarettes, one of the first democracies to ban all forms of tobacco advertising, one of the first nations to introduce explicit health warnings on cigarette packets, and one of the first countries to run large scale anti-smoking campaigns for the public [20]. Partly due to these restrictions, Australia has now become a relatively difficult region for tobacco industries to operate in, with a wide variety of anti-smoking laws and an aggressive and well-organized anti-smoking movement [20]. Australia's community smoking rate has been steadily declining in recent years [21] and is currently one of the lowest in the developed world [1]. Although part of the impetus for these changes can be attributed to the efforts of Australian physicians, few authors have systematically investigated tobacco smoking rates within this occupational subgroup [22]. The aim of our current review therefore, was to undertake a comprehensive and systematic review of tobacco smoking habits within the Australian medical profession during the mid to late 20th century.
Methods
An extensive literature review was conducted which targeted all manuscripts published in peer-reviewed journals relating to the topic of tobacco smoking among Australian physicians. As the official language of Australia is English, and studies from this region could be expected to be published in such a format, only English-language manuscripts were included. The review itself began with a search of relevant Medical Subject Headings (MeSH) such as 'smoking', 'Australia', 'tobacco' and 'physician' on the PubMed database from the US National Library of Medicine [23]. After identifying some initial studies, the search was repeated using keyword variations such as 'smoke' and 'doctor'. As there were relatively few older manuscripts on this topic listed in PubMed, the reference lists of journal papers located using our initial criteria were subsequently examined to find additional publications. Manuscripts were then arranged in descending order, depending on the year in which the smoking survey had actually been undertaken, rather than the year it was published. Where the year of study was not listed or was otherwise unclearly stated in the text, the manuscript's corresponding author was contacted for clarification, wherever possible. The publication year for all studies was eventually determined using either the manuscript itself or by direct contact with the authors. After sourcing the original article, all manuscripts were assigned a reference number based on the abovementioned criteria. For consistency, all smoking prevalence rates were rounded to the nearest whole number. Response rates for each study were also rounded to the nearest whole number for standardization purposes. To gain some perspective on physician's tobacco smoking habits over time, with respect to physicians in other countries and the general Australian population, smoking rates for these subgroups were also sourced from various scientific reports.
Main findings and discussion
A total of 11 studies which investigated tobacco smoking habits among Australian physicians appear to have been published in the past 50 years [24–34], as shown in Table 1. All had been conducted as self-reporting postal surveys. The earliest study we located was from 1964 [24], with the most recent being conducted in 1997 [34]. Five investigations had sourced their participants from lists of registered medical practitioners [24–27, 32], two had sent surveys to readers of their specific journal [28, 29], two studies recruited physicians who were enrolled in postgraduate training programs [30, 31], one study targeted physicians on a commercial mailing list [34], while the recruitment method of one other investigation was not clearly specified [33]. Response rates ranged from 14% [29] to 80% [27], with most above 50% [26, 27, 30–34]. Most studies listed the current prevalence of cigarette smoking among their physicians, although some earlier research suggested that a certain proportion also smoked pipes and cigars during the mid-twentieth century. This latter result was not entirely surprising, as Doll et al [35] has previously documented how a large proportion of their British physicians smoked pipes or cigars rather than cigarettes, similar to Fowler et al's [36] earlier finding in the same country. In contemporary Australian society however, pipe and cigar smoking is comparatively rare, with most active smokers consuming only cigarettes [37].
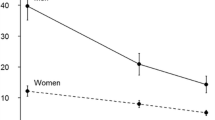
The historical decline of tobacco of cigarette smoking among Australian physicians is displayed in Figure 1. In the early 1960s, research suggests that a large proportion of the general Australian population was consuming tobacco, with almost two-thirds of males and over one-third of females smoking cigarettes. Almost thirty percent of physicians were smoking in the 1960s, although their prevalence rate had declined dramatically by the 1970s, and was roughly half of what it had been by 1974 and 1978. By 1982 only about one-tenth of Australian physicians were still smoking, and this rate declined even further in later years. By the 1990s, only one-in-twenty Australian physicians reported themselves to be current smokers. On the other hand, tobacco usage rates among the general Australian population between 1962 and 1986 were less encouraging. Marked differences were found between the genders for example, with the male smoking rate being roughly halved during this period [37–44]. Female smoking rates in the general population increased slightly however, between the 1960s and the 1980s, before declining to about one-in-five by the 1990s. When compared to the general population, it can be seen that Australian physicians were only half as likely to be cigarette smokers in the 1960s, and only one-seventh as likely to be active tobacco smokers by the 1990s. The two most recent surveys that we located [33, 34] suggest that smoking is now very rare within the Australian medical profession.
Even so, it is important to consider our results within the limitations of collected data, namely the fact that all studies relied on self-reported measures of smoking. As such, the possibility of systematic under-reporting of smoking habits by physicians cannot be totally excluded, and may have occurred for at least two reasons. Firstly, underreporting is a known confounder in population surveys that deal with personal habits, about which people may feel embarrassed. Secondly, and perhaps more importantly, is the fact that throughout the latter half of last century the increasing weight of scientific evidence had made it clear that physicians should not be smoking. While the overall community data no doubt suggests that fewer Australians are smoking than ever before, exactly how many of the physicians who claim to be 'non smokers' never use tobacco at all, cannot be established. As such, it is reasonable to assume that at least some physicians who smoked might have been reluctant to admit the fact during a survey. While we cannot be sure exactly what proportion of smoking doctors would incorrectly report themselves to be non-smokers, we anticipate it should be a relatively low proportion of the total. Furthermore, as this unique bias would presumably be occurring whenever physicians were surveyed in any country, international comparisons between them remain valid.
Methodological limitations notwithstanding, the proportion of Australian physicians who reported themselves as non-smokers or ex-smokers over the years is displayed historically in Figure 2. In 1964 over half were apparently non-smokers, a rate which had risen dramatically by 1982. The proportion of Australian physicians who had quit smoking also appeared to rise during this period, from 18% in 1964 to 38% between 1970 and 1974. By the late 1970s to early 1980s, around one-third reported themselves to be ex-smokers, although the increasing number of physicians who had never smoked was naturally reducing the overall proportion who could be ex-smokers. For these reasons, the proportion of ex-smokers remained relatively stable after 1970, as shown in Figure 2. The anti-smoking counseling behavior of Australian physicians also appeared to improve dramatically between 1964 and 1982. In 1964 for example [24], less than half of those surveyed (39%) were actively advising their patients not to smoke. By 1982 however, almost all physicians (91%) reported that they were counseling patients in this regard [28]. As with most countries, the intrinsic dangers of tobacco smoking had been almost universally accepted by Australian physicians by the mid-to-late 20th century. Indeed, the two earliest studies identified during our investigation had actually asked their participants such a question. In 1964 for example, 96% of Australian physicians believed that cigarette smoking was a health hazard [24]. Encouragingly, the proportion of affirmative responses to this question had increased to 98% by 1970 [25]. These results suggest that physicians who continued to smoke after 1970 (over 10% of the group) were no doubt aware of the personal health hazards they faced.
Aside from changes to individual behavior, the Australian Medical Association (AMA) also became increasingly active in its opposition to tobacco usage throughout the 20th century. Although many different reasons can be proposed as to why physicians would choose to be involved in the anti-smoking movement, it is reasonable to assume that physicians were probably the first health care providers to graphically witness tobacco induced diseases among patients in their care. Immediately following the Second World War for example, Gallup polls suggested that around three-quarters of all Australian adult males were current smokers [37]. This situation no doubt inspired physicians who were interested in preventive medicine, particularly as the scientific evidence against tobacco mounted. Changes of opinion in the Australian medical community were also reflected in the scientific evidence published in relevant Australian medical journals. In 1953 for example, the Medical Journal of Australia published its first article suggesting a tentative link between smoking and lung cancer [45]. In 1962, the National Health and Medical Research Council (NHMRC) issued an official statement on the suspected relationship between cigarette smoking and lung cancer [46]. Two years later in 1964, the first study on physicians' smoking habits was published in Modern Medicine of Australia [24], and three years after that, the AMA released their official policy on the topic [47]. By 1970, it appears that most of the Australian medical community had accepted the dangers of tobacco use [25].
Tobacco smoking research also appears to have begun on a national scale around this time, with the first national data on Australia's smoking demographic being published in the MJA during 1975 [38]. The Australian Bureau of Statistics (ABS) then conducted a national survey of alcohol and tobacco usage, publishing their results in a large report three years later, in 1978 [48]. Around this time, some Australian physicians became actively opposed to smoking at an individual level. By 1983 for example, at least four had been charged after defacing cigarette billboards with anti-smoking messages [49]. Australian health professions also adopted a more unified, national front, with nine of Australia's professional health bodies endorsing a national newspaper advertisement condemning cigarette promotion in 1987 [50]. In 1988, an article in the Medical Journal of Australia went one step further to suggest that a smoke-free Australia could be a bicentennial resolution for the year 2000 [51]. The introduction and approval of pharmaceutical products to help smokers quit their habit was instrumental in the fight against tobacco. In 1993, Nicotine patches were first approved for use in Australia, if prescribed by medical practitioners. From a policy perspective, the Australian medical profession became increasingly active in its opposition to smoking. In recent years for example, professional medical societies such as the Australian Medical Association [52], the Royal Australian College of General Practitioners [53] and the Royal Australasian College of Physicians [54] have all published their official policies on tobacco smoking and tobacco control. With regard to contemporary smoking interventions from a global perspective, the aforementioned WHO-FCTC [2] represents an important treaty and one to which Australia is a signatory.
Although few contemporary physicians appear to be smoking in Australia, it is interesting to compare the progression of their tobacco usage trends with physicians in other developed countries. Although the current paper is not intended as a systematic review of tobacco smoking in all countries, a few brief comparisons with other regions are appropriate. Some interesting contrasts can be seen when current tobacco smoking trends among physicians in four developed countries are juxtaposed with the five Australian studies during this time period [30–34]. Between 1990 and 2002 for example, at least five separate studies from the US [55–59] found that American physicians smoked tobacco at very low rates, similar to their Australian counterparts. From the publications we located, it appears that the prevalence rate of smoking among US physicians is currently between 2% and 4%, very similar to their Australian counterparts, where it ranges from 3% to 6%. Interestingly, three of the aforementioned US investigations also looked at smoking among dentists at the same time [55, 56, 59]. All three found that smoking was similarly rare among US dentists. These studies suggest therefore, that tobacco smoking is probably uncommon among medically-trained health care workers in the United States. As such, a summary of these studies suggests that fewer than one-in-ten American or Australian physicians, currently smokes tobacco. Physicians in both countries therefore, could be described as tobacco control exemplars, at least with regard to anti-smoking health promotion.
On the other hand, contemporary tobacco smoking rates among physicians in some other developed countries is less encouraging, with research among Italian doctors warranting particular concern [60]. Between 1995 and 2000 for example, five separate investigations by Italian researchers found that between 24% and 39% of physicians reported themselves to be active smokers [61–65]. From these studies it appears that Italian physicians may not be setting a good example as role models for their patients, at least as far as tobacco smoking is concerned. Somewhat disturbingly, La Vecchia et al [64] also reported that female Italian physicians may even be smoking at higher rates than the community in which they live. On the other hand, an Italian study by Nardini et al [63] found that while 39% of the physicians surveyed were current smokers, their rate was actually one of the lowest of all staff at a general hospital, particularly when compared to nursing students and auxiliaries. Future reductions of tobacco usage among Italian health care workers may therefore be difficult to achieve, although exactly how Italian physicians can and should move forward is beyond the scope of the current paper.
While a detailed discussion of smoking in Japan is beyond the scope of the current paper, some comparisons between the smoking habits of Australian physicians and their Japanese counterparts is still worthwhile. At least five English-language studies have looked at tobacco smoking among Japanese physicians in recent years [66–70]. The highest prevalence rate appears to have been documented in 1990, when 32% of Fukuoka physicians reported themselves to be smokers [66]. High smoking rates were also found among physicians during local surveys conducted in Tokyo [67], Okayama [68] and Fukui [69]. A nationwide survey of Japanese physicians during the year 2000 revealed that 27% of male physicians and 7% of female physicians smoked, a rate which was about half that of the national average for the general population, at the time [70]. Even so, from these results it can be seen that at least one-in-five Japanese physicians still consumes tobacco on a regular basis. The continued high prevalence of smoking among them is somewhat ironic, as it was a Japanese physician, Takeshi Hirayama, who published some of the first scientific evidence linking lung cancer to passive smoking [71]. Hirayama's work has withstood the test of time and has now become a classic paper in tobacco control [72]. Similar to Australia, the Japanese tobacco control environment did improve somewhat in the late 20th century. In recent years, more anti-smoking measures have been introduced to Japan, particularly after 1998 when lung cancer rose to become the leading cause of death, ahead of stomach cancer [73]. Although this is clearly a step in the right direction, further efforts will still need to be made to encourage Japanese physicians and the medical students who precede them, to quit smoking [74, 75].
In leading the fight against tobacco, it is important for physicians in all countries to recognize their unique role as tobacco control exemplars. One reason that Japanese physicians continue to smoke at high rates may be because they lack awareness of their status as public role models [70]. But physicians do occupy a very important role in preventive medicine, in all countries, both as health care providers and as public health exemplars. Physicians are not only responsible for smoking cessation treatment, but also for anti-smoking campaigns [76]. The impact of their preventive efforts should not be underestimated, as it is well-known that medical interventions can be effective in helping patients to quit smoking [77]. Aside from being a non-smoking role model in public, the physicians' clinic and hospital should also be a model of non-smoking behavior [78]. Similarly, medical and dental students need to be encouraged not to smoke [79, 80].
Although smoking rates within the Australian medical profession have clearly declined in recent years, there remains some debate as to whether physicians are doing enough to stop their patients smoking [81]. It has been suggested that physicians are not always successful in recognizing which of their patients actually smoke, with a study of Australian general practitioners for example [82], finding that only 56% of current smokers were correctly identified as such. Additional work to help convince the Australian public of the important role that physicians play in tobacco control may also be appropriate in future. In a survey conducted in the early 1990s for example, 52% of people still believed that 'a lot of doctors smoke' [83]. Despite these potential caveats, smoking rates in the Australian medical profession have clearly declined, with one of the more recent surveys of hospital personnel for example [84] finding that staff in the 'medical' job category still had the lowest smoking rate of all (around 2%). Significant reductions in the smoking rates of physicians in some other countries has also been occurring, particularly in the US [13]. From a historical perspective America was the first country to introduce health warnings on cigarette packets in 1966 [85], and by later that decade, the US Public Health Service had began to publicly promote physicians as non-smoking role models. Community smoking rates subsequently declined, and at least part of the credit for these achievements could be given to physicians.
On the other hand, tobacco use remains problematic in Japanese society, an issue that will require additional government commitment to help reduce the current burden [76]. From a philosophical perspective it is difficult to understand why any physicians would smoke at all, given that they are well-placed to not only receive information about the adverse effects of smoking, but also to understand the science behind it and act accordingly. As such, it is important that this type of health information reaches physicians promptly, both via government networks and professional medical associations. Even so, up-to-date epidemiological data on the smoking habits of physicians remains important for two reasons. Firstly, it helps predict how effective anti-smoking campaigns may be. That is, it would be very difficult to convince the general public not to smoke if their physician role models continued to do so [9]. Secondly, it allows policy makers to determine how 'mature' a particular country's smoking epidemic currently is, and thus, how soon the community prevalence rate may be expected to decline. Historical data on physician's smoking rates is particularly useful, as it permits analysis of social trends regarding tobacco use, and also allows policy makers to see what control strategies were successful in the past, and what policies might be appropriate in the future.
Conclusion
Overall, this review suggests that the prevalence of smoking among Australian physicians has fallen dramatically throughout the latter half of the 20th century, with reductions beyond that achieved by the general population. While tobacco usage rates in the community have generally declined over time, credit should be given to the small number of physicians who encouraged their patients to quit, long before the health risks had been widely accepted by the general community. Such behavior has not been universal, however, with some international comparisons suggesting that while Australian trends are generally similar to those seen in the US, further effort is still required in countries such as Japan and Italy. While a detailed discussion of why physicians in some countries smoke at higher rates than others is beyond the scope of this paper, it nevertheless, highlights an important topic for future research in tobacco control. Whatever their geographical region, the fact that any physicians continue to smoke is unfortunate given their status as exemplars, and implies that further preventive efforts will need to be focused on personal health behaviors. It is important that smoking in the Australian medical profession continues its decline in future years, so that physicians in all countries can lead the way as tobacco control exemplars in the 21st century.
References
World Health Organization (WHO): Why is tobacco a public health priority?. [http://www.who.int/tobacco/health_priority/en/index.html]
World Health Organization (WHO): WHO framework convention on Tobacco control (WHO FCTC). [http://www.who.int/fctc/en/index.html]
Doll R, Hill AB: The mortality of doctors in relation to their smoking habits: A preliminary report. BMJ. 1954, 1 (4877): 1451-1455.
Doll R, Hill AB: The mortality of doctors in relation to their smoking habits: A preliminary report. 1954. BMJ. 2004, 328: 1529-1533. 10.1136/bmj.328.7455.1529.
Doll R, Peto R, Boreham J, Sutherland I: Mortality in relation to smoking: 50 years' observations on male British doctors. BMJ. 2004, 328: 1519-1528. 10.1136/bmj.38142.554479.AE.
Doll R, Peto R, Boreham J, Sutherland I: Mortality from cancer in relation to smoking: 50 years observations on British doctors. Br J Cancer. 2005, 92: 426-429. 10.1038/sj.bjc.6602450.
Stampfer M: New insights from the British doctors study. BMJ. 2004, 328: 1507-10.1136/bmj.328.7455.1507.
Garfinkel L: Cigarette smoking among physicians and other health professionals, 1959–1972. CA Cancer J Clin. 1976, 26: 373-375. 10.3322/canjclin.26.6.373.
Davis RM: When doctors smoke. Tob Control. 1993, 2: 187-188. 10.1136/tc.2.3.187.
Smith D, Leggat P: An international review of tobacco smoking in the medical profession: 1974–2004. BMC Public Health. 2007, 7 (1): 115-10.1186/1471-2458-7-115.
Gardner MN, Brandt AM: The Doctors' Choice Is America's Choice: The Physician in US Cigarette Advertisements, 1930–1953. Am J Public Health. 2006, 96: 222-232.
Kawane H: When doctors advertised cigarettes. Tob Control. 1993, 2: 45.
Smith DR: The historical decline of tobacco smoking among United States physicians: 1949–1984. Tob Induc Dis. 2008, 4 (1): 9-10.1186/1617-9625-4-9.
Nishizumi M, Kuratsune M: A survey of smoking habits of physicians in Western Japan. Nippon Koshu Eisel Zasshi. 1967, 14: 1273-1294.
Adriaanse H, van Reek J: Physicians' smoking and its exemplary effect. Scand J Prim Health Care. 1989, 7: 193-196. 10.3109/02813438909088663.
Lee DJ, LeBlanc W, Fleming LE, Gomez-Marin O, Pitman T: Trends in US smoking rates in occupational groups: The National Health Interview Survey 1987–1994. J Occup Environ Med. 2004, 46: 538-548. 10.1097/01.jom.0000128152.01896.ae.
Nelson DE, Emont SL, Brackbill RM, Cameron LL, Peddicord J, Fiore MC: Cigarette smoking prevalence by occupation in the United States. A comparison between 1978 to 1980 and 1987 to 1990. J Occup Med. 1994, 36: 516-525.
Nelson DE, Giovino GA, Emont SL, Brackbill R, Cameron LL, Peddicord J: Trends in cigarette smoking among US physicians and nurses. JAMA. 1994, 271: 1273-1275. 10.1001/jama.271.16.1273.
Kaetsu A, Fukushima T, Moriyama M, Shigematsu T: Smoking behavior and related lifestyle variables among physicians in Fukuoka, Japan: A cross sectional study. J Epidemiol. 2002, 12: 199-207.
Chapman S, Byrne F, Carter SM: "Australia is one of the darkest markets in the world": the global importance of Australian tobacco control. Tob Control. 2003, 12 (Suppl 3): iii1-3.
Hill DJ, White VM, Gray NJ: Measures of tobacco smoking in Australia 1974–1986 by means of a standard method. Med J Aust. 1988, 149 (1): 10-12.
Magnus P: Cigarette smoking and the Australian medical profession. Med J Aust. 1989, 150 (8): 437.
US National Library of Medicine: PubMed database. [http://www.ncbi.nlm.nih.gov/entrez]
Anonymous: 4,776 answer MM smoking survey. Modern Medicine of Australia. 1964, 8 (August): 1-4.
Anonymous: 5,976 answer MM smoking survey. Modern Medicine of Australia. 1970, 17 (August): 1-4.
Rankin DW, Gray NJ, Hill DJ, Evans DR: Attitudes and smoking habits of Australian doctors. Med J Aust. 1975, 2: 822-824.
Dodds AM, Rankin DW, Hill DJ, Gray NJ: Attitudes and smoking habits of doctors in Victoria. Community Health Stud. 1979, 3 (1): 28-31.
Anonymous: You're setting the pace in the fitness stakes. Medical Practice. 1983, 9 (September): 22-24.
Nyman K: The health of general practitioners. A pilot survey. Aust Fam Physician. 1991, 20 (5): 637-641. 644–635
Roche AM, Parle MD, Stubbs JM, Hall W, Saunders JB: Management and treatment efficacy of drug and alcohol problems: What do doctors believe?. Addiction. 1995, 90: 1357-1366. 10.1111/j.1360-0443.1995.tb03553.x.
Roche AM, Parle MD, Saunders JB: Managing alcohol and drug problems in general practice: A survey of trainees' knowledge, attitudes and educational requirements. Aust NZ J Public Health. 1996, 20 (4): 401-408. 10.1111/j.1467-842X.1996.tb01053.x.
McCall L, Maher T, Piterman L: Preventive health behaviour among general practitioners in Victoria. Aust Fam Physician. 1999, 28 (8): 854-857.
Young JM, Ward JE: Declining rates of smoking among medical practitioners. Med J Aust. 1997, 167: 232.
Young JM, Ward JE: Implementing guidelines for smoking cessation advice in Australian general practice: opinions, current practices, readiness to change and perceived barriers. Fam Pract. 2001, 18 (1): 14-20. 10.1093/fampra/18.1.14.
Doll R, Peto R, Wheatley K, Gray R, Sutherland I: Mortality in relation to smoking: 40 years' observations on male British doctors. BMJ. 1994, 309: 901-911.
Fowler G, Mant D, Fuller A, Jones L: The "Help Your Patient Stop" initiative. Evaluation of smoking prevalence and dissemination of WHO/UICC guidelines in UK general practice. Lancet. 1989, 1: 1253-1255. 10.1016/S0140-6736(89)92342-8.
Woodward SD: Trends in cigarette consumption in Australia. Aust N Z J Med. 1984, 14 (4): 405-407.
Gray NJ, Hill DJ: Patterns of tobacco smoking in Australia. Med J Aust. 1975, 2 (22): 819-822.
Gray NJ, Hill DJ: Patterns of tobacco smoking in Australia. 2. Med J Aust. 1977, 2 (10): 327-328.
Hill DJ, Gray NJ: Patterns of tobacco smoking in Australia. Med J Aust. 1982, 1 (1): 23-25.
Hill D, Gray N: Australian patterns of tobacco smoking and related health beliefs in 1983. Community Health Stud. 1984, 8 (3): 307-316.
Hill DJ: Australian patterns of tobacco smoking in 1986. Med J Aust. 1988, 149 (1): 6-10.
Hill DJ, White VM, Gray NJ: Australian patterns of tobacco smoking in 1989. Med J Aust. 1991, 154 (12): 797-801.
Australian Institute of Health and Welfare (AIHW): Statistics on drug use in Australia 2004. 2005, AIHW Report No. PHE 62, Canberra
Anonymous: SMOKER'S respiratory syndrome. Medical Journal of Australia. 1953, 2 (9): 343-344.
National Health and Medical Research Council (NHMRC): Smoking and lung cancer: Report of the 53rd session of the NHMRC. 1962, Canberra
Rieger C: Correspondence: The A.M.A.'s policy on smoking tobacco. Med J Aust. 1967, 1967 (2 Suppl): 66.
Australian Bureau of Statistics (ABS): Alcohol and tobacco consumption patterns, February 1977. 1978, ABS Cat No. 4312.0, Canberra
Margo J: The doctors who fight cancer with spray cans. The Sydney Morning Herald. 1983, 19 Feb: 32.
Woodward S: Everything Dick Smith said (and wanted to say) is true. The Australian. 1987, 23 April : 3.
Armstrong BK, Daube MM, Shean RE: A smoke-free Australia – our bicentenary resolution?. Med J Aust. 1988, 149 (1): 1-2.
Australian Medical Association (AMA): AMA position statement: Tobacco smoking – 2005. [http://www.ama.com.au/node/2241]
Royal Australian College of General Practitioners (RACGP): SNAP: Smoking, nutrition, alcohol and physical activity. [http://www.racgp.org.au/guidelines/snap]
The Royal Australasian College of Physicians (RACP) and The Royal Australian and New Zealand College of Psychiatrists (RANZCP): Tobacco policy: Using evidence for better outcomes. [http://www.racp.edu.au/download.cfm?DownloadFile=A955EED6-2A57-5487-D35E68AC78E06E42]
Brink SG, Gottlieb NH, McLeroy KR, Wisotzky M, Burdine JN: A community view of smoking cessation counselling in the practices of physicians and dentists. Public Health Rep. 1994, 109: 135-142.
Hill HA, Braithwaite RL: Attitudes, beliefs, and practices regarding smoking and smoking cessation among African-American physicians and dentists. J Natl Med Assoc. 1997, 89: 745-751.
An LC, Bernhardt TS, Bluhm J, Bland P, Center B, Ahluwalia JS: Treatment of tobacco use as a chronic medical condition: Primary care physicians' self-reported practice patterns. Prev Med. 2004, 38: 574-585. 10.1016/j.ypmed.2003.11.016.
Misra R, Vadaparampil ST: Personal cancer prevention and screening practices among Asian Indian physicians in the United States. Cancer Detect Prev. 2004, 28: 269-276. 10.1016/j.cdp.2004.02.004.
Kenna GA, Wood MD: The prevalence of alcohol, cigarette and illicit drug use and problems among dentists. J Am Dent Assoc. 2005, 136: 1023-1032.
Smith DR, L'Abbate N, Lorusso A: Tobacco smoking among Italian physicians and the role of occupational medicine. Med Lav. 2008, 99 (1): 3-7. [http://www.lamedicinadellavoro.it/]
Nardini S, Bertoletti R, Rastelli V, Donner CF: The influence of personal tobacco smoking on the clinical practice of Italian chest physicians. Eur Respir J. 1998, 12: 1450-1453. 10.1183/09031936.98.12061450.
Zanetti F, Gambi A, Bergamaschi A, Gentilini F, De Luca G, Monti C: Smoking habits, exposure to passive smoking and attitudes to a non-smoking policy among hospital staff. Public Health. 1998, 112: 57-62. 10.1016/S0033-3506(98)00208-X.
Nardini S, Bertoletti R, Rastelli V, Ravelli L, Donner CF: Personal smoking habit and attitude toward smoking among the health staff of a general hospital. Monaldi Arch Chest Dis. 1998, 53: 74-78.
La Vecchia C, Scarpino V, Malvezzi I, Baldi G: A survey of smoking among Italian doctors. J Epidemiol Community Health. 2000, 54: 320-10.1136/jech.54.4.320a.
Pizzo AM, Chellini E, Grazzini G, Cardone A, Badellino F: Italian general practitioners and smoking cessation strategies. Tumori. 2003, 89: 250-254.
Kaetsu A, Fukushima T, Moriyama M, Shigematsu T: Change of the smoking behavior and related lifestyle variables among physicians in Fukuoka, Japan: A longitudinal study. J Epidemiol. 2002, 12: 208-216.
Kawakami M, Nakamura S, Fumimoto H, Takizawa J, Baba M: Relation between smoking status of physicians and their enthusiasm to offer smoking cessation advice. Intern Med. 1997, 36: 162-165. 10.2169/internalmedicine.36.162.
Kawane H, Soejima R: Smoking among doctors in a medical school hospital. Kawasaki Med J. 1996, 22: 211-216.
Kawahara K, Ohida T, Osaki Y, Mochizuki Y, Minowa M, Yamaguchi N: Study of the smoking behavior of medical doctors in Fukui, Japan and their antismoking measures. J Epidemiol. 2000, 10: 157-162.
Ohida T, Sakurai H, Mochizuki Y, Kamal AM, Takemura S, Minowa M: Smoking prevalence and attitudes toward smoking among Japanese physicians. JAMA. 2001, 285: 2643-2648. 10.1001/jama.285.20.2643.
Hirayama T: Non-smoking wives of heavy smokers have a higher risk of lung cancer: a study from Japan. Br Med J (Clin Res Ed). 1981, 282 (6259): 183-185.
Ong E, Glantz SA: Hirayama's work has stood the test of time. Bull World Health Organ. 2000, 78 (7): 938-939.
Ohida T, Kawane H, Kamal AMM, Takemura S, Sakurai H: Smoking among Japanese physicians. JAMA. 2001, 286 (8): 917-10.1001/jama.286.8.917.
Kawane H: The prevalence of smoking among physicians in Japan. Am J Public Health. 1993, 83: 1640-10.2105/AJPH.83.11.1640.
Smith DR, Takahashi K: Too many Japanese university students are still smoking tobacco. Tob Induc Dis. 2008, 4 (1): 10-10.1186/1617-9625-4-10.
Kawane H: Smoking cessation: Physician responsibility and government's role. Respir Med. 1996, 90 (7): 440-10.1016/S0954-6111(96)90124-9.
Fowler G: Educating doctors in smoking cessation. Tob Control. 1993, 2: 5-6. 10.1136/tc.2.1.5.
Nett LM: The physician's role in smoking cessation: A present and future agenda. Chest. 1990, 97 (2 Suppl): 28S-32S. 10.1378/chest.97.2_Supplement.28S.
Smith DR, Leggat PA: An international review of tobacco smoking among medical students. J Postgrad Med. 2007, 53 (1): 55-62.
Smith DR, Leggat PA: An international review of tobacco smoking among dental students in 19 countries. Int Dent J. 2007, 57 (6): 452-458.
Hill D, Borland R: Are doctors doing enough to stop their patients smoking?. Med J Aust. 1989, 150 (8): 413-414.
Dickinson JA, Wiggers J, Leeder SR, Sanson-Fisher RW: General practitioners' detection of patients' smoking status. Med J Aust. 1989, 150 (8): 420-2, 425-426.
Chapman S, Wong WL, Smith W: Self-exempting beliefs about smoking and health: differences between smokers and ex-smokers. Am J Public Health. 1993, 83 (2): 215-219. 10.2105/AJPH.83.2.215.
Jones TE, Crocker H, Ruffin RE: Smoking habits and cessation programme in an Australian teaching hospital. Aust N Z J Med. 1998, 28 (4): 446-452.
Chapman S, Carter SM: "Avoid health warnings on all tobacco products for just as long as we can": a history of Australian tobacco industry efforts to avoid, delay and dilute health warnings on cigarettes. Tob Control. 2003, 12 (Suppl 3): iii13-22.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
DS conceived the idea for the study. DS and PL wrote the manuscript. Both authors read and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Smith, D.R., Leggat, P.A. The historical decline of tobacco smoking among Australian physicians: 1964–1997. Tob. Induced Dis. 4, 13 (2008). https://doi.org/10.1186/1617-9625-4-13
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1617-9625-4-13