Abstract
Henoch-Schönlein purpura is one of the most common forms of systemic vasculitis of childhood. We report the response to anakinra, the interleukin-1 receptor antagonist, in a 9 year old girl without prior medical problems who developed life-threatening Henoch-Schönlein vasculitis that produced renal failure, pulmonary hemorrhage and vasculitis of the brain. Her response supports the theory that interleukin-1 may be an important mediator in this disease. Further study of interleukin-1 antagonists in severe Henoch-Schönlein purpura may be warranted.
Similar content being viewed by others
Background
Henoch-Schönlein purpura (HSP) is the most common form of childhood vasculitis [1–8] affecting 10-20 per 100,000 children annually [1–3, 5]. It occurs most frequently in children between the ages of 2 and 11 years [1]. HSP produces a broad array of clinical features resulting from widespread IgA deposition in the walls of small vessels [3]. Purpura of the skin, joint pain and swelling, gastrointestinal symptoms, and renal involvement are the most common manifestations with frequencies of 100% [2, 3, 9], 75% [2, 3, 8], 50-75%, and 40-50% [1–8] of the patient population, respectively. Less often, neurologic complications, pulmonary hemorrhage, and testicular vasculitis may occur [1–3]. Of these, glomerulonephritis remains the strongest indicator of poor prognosis [1, 6, 8]. Most series show that 1-7% of children with HSP glomerulonephritis will develop chronic renal failure [10–12]. Although reports describe the use of oral and parenteral corticosteroids, pulse methylprednisolone, dapsone, azathioprine, cyclophosphamide, cyclosporine, and plasmapheresis, researchers still lack strong evidence that confirms the superiority of any treatment regime in preventing tissue damage [4–6, 13–15]. A recent metanalysis supports the use of glucocorticoids during acute disease, however [5].
Henoch-Schönlein purpura is typically a benign and self-limited systemic vasculitis. Perhaps because it does not frequently cause permanent damage, its pathogenesis remains relatively poorly understood. IgA deposition in vessel walls is a consistent pathologic finding, and is the hallmark of the disease [3]. The triggers that promote the IgA production and tissue deposition, those that determine why some individuals get the disease while most do not, and those that dictate why the disease can be life-threatening in a minority of affected children are not known.
A variety of therapeutic agents that target specific inflammatory cytokines are available for the treatment of rheumatic diseases. Biologic agents including soluble receptors and monoclonal antibodies that block the action of a variety of cytokines including tumor necrosis alpha, interleukin-1, interleukin-6 have been used with variable success in Kawasaki disease[16–19], granulomatosis with polyangiitis (Wegener granulomatosis) [20, 21] and other severe forms of vasculitis [22–28]. Experimental evidence suggests inflammatory cytokines such as IL-1, TNF and IL-6 are involved in the pathogenesis of HSP [29]. Reports over the last 3 decades suggest that autoinflammatory diseases characterized by high interleukin-1 production such as familial Mediterranean fever may be associated with an increased incidence of HSP, and with more severe disease [7, 30–39], making IL-1 an potential target in refractory disease.
Lead by data supporting an important role for IL-1 in HSP pathogenesis, we present a case that may indicate a direction for future research into novel therapies for severe Henoch-Schönlein purpura.
Case Report
A 9 year old girl presented with a one week history of abdominal pain, vomiting, swelling and pain of the left ankle, dark colored urine and purpuric rash on her buttocks and lower extremities, consistent with a diagnosis of Henoch-Schönlein purpura nephritis. Her initial serum creatinine was normal at 0.5 mg/dL, but she had hypoalbuminemia (serum albumin was 2.7 mg/dL) and high grade proteinuria with urine protein:creatinine ratio of 15.1. After a three day course of 2 mg/kg/day methylprednisolone, her abdominal pain and rash improved. She was discharged on 2 mg/kg/day oral prednisone with plans to follow-up with her nephrologist in two weeks. Within a week, her HSP rash, abdominal pain and arthralgia returned, so she was admitted again to the hospital (see time course of her illness and treatment in Figure 1). She had nephrotic range proteinuria with a fall in serum albumin from 2.7 to 1.2 g/dL. Her serum creatinine had risen to 1.7 mg/dL, with blood urea nitrogen of 55 mg/dL. A kidney biopsy revealed crescents in more than half of the glomeruli, with sclerosing lesions and abundant IgA deposits indicative of severe HSPN. She received a three day course of 30 mg/kg/day methylprednisolone and began mycophenolate mofetil but failed to improve, with progressive rise in serum creatinine over four days to 2.5 mg/dL.
Timeline of Response to Therapy. Time in weeks after the onset of first symptoms of HSP is shown on the horizontal axis. The vertical axis shows serum creatinine in mg/dl (red), and therapeutic measures used. The daily dose of glucocorticoid in mg/kg/day is in blue; methylprednisolone pulse therapy is represented by blue arrows (30 mg/kg/day for 5 days, each arrow); and in the upper portion of the figure, anakinra dose is illustrated. Note that the serum creatinine rose when the anakinra dose was decreased, both at week eleven and at week thirty.
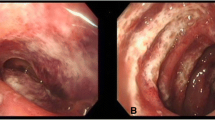
At the time she was readmitted, she had mild dyspnea and hypoxemia. Despite vigorous diuresis and broad spectrum antimicrobial coverage, her condition progressed to respiratory failure by the second week. Chest radiography showed diffuse patchy infiltrates (Figure 2). Bronchoalveolar lavage confirmed pulmonary hemorrhage grossly, with fresh blood and hemosiderin laden macrophages identified in the lavage fluid. Because of the child's rising creatinine and lack of response to more conventional treatments, she received IVIG therapy and a 2 week course of plasmapheresis, but had little clinical response. After a week of plasmapheresis she developed initially focal, then generalized seizures and required anticonvulsant therapy. She had altered mental status with sluggish cognition. MRI of the brain showed numerous regions of vasogenic edema consistent with cerebral vasculitis (Figure 3). The pattern of edema was not suggestive of posterior reversible encephalopathy syndrome secondary to hypertension. By this time, the serum creatinine was 4.8 mg/dL.
Brain Magnetic Resonance Imaging. These two coronal FLAIR images demonstrate increased signal intensity within the cortical gray matter of the parietal, occipital and frontal lobes, with minimal involvement of the sub-cortical white matter. The deep white matter is spared. This picture is consistent with scattered regions of vasogenic edema most consistent with vasculitis, and not indicative of posterior reversible encephalopathy from hypertension.
Based on evidence that severe HSP may be characterized by interleukin-1 (IL-1) over-production [7, 34, 40], a planned one-day trial of anakinra (recombinant IL-1 receptor antagonist) was initiated in the hopes of avoiding the toxicity of cyclophosphamide therapy. Accordingly, her renal function rapidly improved and serum creatinine fell from 4.8 mg/d to 2.4 in 48 hours, and further to 1.0 in 10 days. Both neurologic and pulmonary dysfunction cleared rapidly, and she was weaned from ventilator within 24 hours. Anakinra was continued daily for 6 weeks, and then it was discontinued, because the child objected strongly to the injections, her serum creatinine was stable at 0.8 mg/dL, and it was unclear whether anakinra was the cause of her improvement.
Within one week of stopping the anakinra, the serum creatinine rose to 3.26 mg/dL despite continuous prednisone (1 mg/kg/day) and mycophenolate mofetil. Renal biopsy at this time again showed active vasculitis with evidence of progression with early interstitial fibrosis and tubular atrophy, as well as progression from cellular to fibrous crescents, and global glomerulosclersosis of 20% of glomeruli. Because of the rising creatinine and biopsy findings, she resumed daily anakinra at twice her previous dose (100 mg/day) and received another course of plasmapheresis. She had persistent hypertension during this period requiring a variety of medications. After resuming anakinra, her renal function and hypertension improved and remained stable with serum creatinine between 1.0 and 1.8 mg/dL (higher levels with lower prednisone doses).
Four months after resuming anakinra, an attempt was made to wean the injections to every other day. The creatinine rose from 1.8 to 2.5 mg/dL within two weeks, so she returned to daily dosing (100 mg/day). Unfortunately, her renal function improved only transiently, and her creatinine again rose. Her glomerulonephritis was unresponsive to higher doses of glucocorticoid, and renal failure ensued. Eleven months after her initial diagnosis, a renal biopsy was performed to determine whether further aggressive immunosuppression was warranted. This biopsy revealed global glomerulosclerosis involving nearly 100% of the glomeruli and marked interstitial fibrosis with tubular atrophy. She began dialysis two weeks later. Fourteen months after her initial diagnosis, she received a successful renal transplant.
Discussion
In the child described in this report with life-threatening systemic vasculitis that caused renal failure, pulmonary hemorrhage and diffuse vasculitis of the brain with seizures and impaired cognition, there was no prior medical history to suggest an underlying autoinflammatory condition characterized by over-production of interleukin-1. In fact, subsequent DNA analysis was negative for the common familial Mediterranean fever gene mutations. The severe HSP complications occurred despite plasmapheresis, pulse methylprednisolone and high dose mycophenolate mofetil. In an attempt to avoid the toxicity of cyclophosphamide [41–43], a one-day trial of subcutaneous anakinra was undertaken with rapid and dramatic improvement. The HSP relapsed twice when the anakinra was tapered, and she improved with reinstitution of the drug. Unfortunately, the disease ultimately progressed to irreversible renal failure. Thus in retrospect, either the dose of anakinra should not have been decreased, or cyclophosphamide might have proved a wiser choice of treatment.
Conclusions
Although this single case report does not provide sufficient evidence to indicate that treatment with an interleukin-1 antagonist is either effective or safe in severe HSP, it does suggest that disease may be ameliorated with anakinra, and moreover, that further study of the role of interleukin-1 in HSP and of IL-1 antagonism in severe disease might be appropriate.
Consent
The parent of this minor child has given written informed consent for the publication of the child's case report and accompanying de-identified images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
- DNA:
-
deoxyribonucleic acid
- FMF:
-
familial Mediterranean fever
- HSP:
-
Henoch-Schönlein purpura
- IgA:
-
immunoglobulin A
- IL-1:
-
interleukin-1
- IL-1RA:
-
interleukin-1 receptor antagonist
- IVIG:
-
intravenous immunoglobulin
- MEFV:
-
gene encoding pyrin, mutated in familial Mediterranean fever
- MR:
-
magnetic resonance
- MRI:
-
magnetic resonance imaging.
References
Mir S, Yavascan O, Mutlubas F, Yeniay B, Sonmez F: Clinical outcome in children with Henoch-Schönlein nephritis. Pediatric Nephrology. 2007, 22 (1): 64-70. 10.1007/s00467-006-0278-0.
Saulsbury FT: Clinical update: Henoch-Schönlein purpura. Lancet. 2007, 369 (9566): 976-8. 10.1016/S0140-6736(07)60474-7.
Saulsbury FT: Henoch-Schönlein purpura in children. Report of 100 patients and review of the literature. Medicine. 1999, 78 (6): 395-409. 10.1097/00005792-199911000-00005.
Weiss PF, Klink AJ, Localio R, Hall M, Hexem K, Burnham JM: Corticosteroids may improve clinical outcomes during hospitalization for Henoch-Schönlein purpura. Pediatrics. 2010, 126 (4): 674-81. 10.1542/peds.2009-3348.
Weiss PF, Feinstein JA, Luan X, Burnham JM, Feudtner C: Effects of corticosteroid on Henoch-Schönlein purpura: a systematic review. Pediatrics. 2007, 120 (5): 1079-87. 10.1542/peds.2007-0667.
Shenoy M, Bradbury MG, Lewis MA, Webb NJ: Outcome of Henoch-Schönlein purpura nephritis treated with long-term immunosuppression. Pediatric Nephrology. 2007, 22 (10): 1717-22. 10.1007/s00467-007-0557-4.
Gershoni-Baruch R, Broza Y, Brik R: Prevalence and significance of mutations in the familial Mediterranean fever gene in Henoch-Schönlein purpura. Journal of Pediatrics. 2003, 143 (5): 658-61. 10.1067/S0022-3476(03)00502-X.
Butani L, Morgenstern BZ: Long-term outcome in children after Henoch-Schönlein purpura nephritis. Clinical Pediatrics. 2007, 46 (6): 505-11. 10.1177/0009922806298896.
Saulsbury FT: Henoch-Schönlein purpura. Current Opinion in Rheumatology. 2001, 13 (1): 35-40. 10.1097/00002281-200101000-00006.
Soylemezoglu O, Ozkaya O, Ozen S, Bakkaloglu A, Dusunsel R, Peru H: Henoch-Schönlein nephritis: a nationwide study. Nephron. 2009, 112 (3): c199-c204.
Mills JA, Michel BA, Bloch DA, Calabrese LH, Hunder GG, Arend WP: The American College of Rheumatology 1990 criteria for the classification of Henoch-Schönlein purpura. Arthritis & Rheumatism. 1990, 33 (8): 1114-21.
Tizard EJ: Henoch-Schönlein purpura. Archives of Disease in Childhood. 1999, 80 (4): 380-3. 10.1136/adc.80.4.380.
Gibson KL, Amamoo MA, Primack WA: Corticosteroid therapy for Henoch Schönlein purpura. Pediatrics. 121 (4): 870-1.
Kawasaki Y, Suzuki J, Nozawa R, Suzuki S, Suzuki H: Efficacy of methylprednisolone and urokinase pulse therapy for severe Henoch-Schönlein nephritis. Pediatrics. 2003, 111 (4:Pt 1): t-9.
O'Neil KM: Progress in pediatric vasculitis. Current Opinion in Rheumatology. 2009, 21 (5): 538-46. 10.1097/BOR.0b013e32832f13f1.
Burns JC, Best BM, Mejias A, Mahony L, Fixler DE, Jafri HS: Infliximab treatment of intravenous immunoglobulin-resistant Kawasaki disease. Journal of Pediatrics. 2008, 153 (6): 833-8. 10.1016/j.jpeds.2008.06.011.
Portman MA, Olson A, Soriano B, Dahdah N, Williams R, Kirkpatrick E: Etanercept as adjunctive treatment for acute Kawasaki disease: study design and rationale. American Heart Journal. 2011, 161 (3): 494-9. 10.1016/j.ahj.2010.12.003.
Shirley DA, Stephens I: Primary treatment of incomplete Kawasaki disease with infliximab and methylprednisolone in a patient with a contraindication to intravenous immune globulin. Pediatric Infectious Disease Journal. 2010, 29 (10): 978-9. 10.1097/INF.0b013e3181e05564.
Son MB, Gauvreau K, Burns JC, Corinaldesi E, Tremoulet AH, Watson VE: Infliximab for intravenous immunoglobulin resistance in Kawasaki disease: a retrospective study. Journal of Pediatrics. 2011, 158 (4): 644-9. 10.1016/j.jpeds.2010.10.012.
Antoniu SA: Treatment options for refractory Wegener's granulomatosis: a role for rituximab?. Current Opinion in Investigational Drugs. 2007, 8 (11): 927-32.
Wegener's Granulomatosis Etanercept Trial (WGET) Research Group: Etanercept plus standard therapy for Wegener's granulomatosis. New England Journal of Medicine. 2005, 352 (4): 351-61.
Arbach O, Gross WL, Gause A: Treatment of refractory Churg-Strauss-Syndrome (CSS) by TNF-alpha blockade. Immunobiology. 2002, 206 (5): 496-501. 10.1078/0171-2985-00197.
Botsios C, Sfriso P, Punzi L, Todesco S: Non-complementaemic urticarial vasculitis: successful treatment with the IL-1 receptor antagonist, anakinra. Scandinavian Journal of Rheumatology. 2007, 36 (3): 236-7. 10.1080/03009740600938647.
Eleftheriou D, Melo M, Marks SD, Tullus K, Sills J, Cleary G: Biologic therapy in primary systemic vasculitis of the young. Rheumatology. 2009, 48 (8): 978-86. 10.1093/rheumatology/kep148.
Huugen D, Tervaert JW, Heeringa P: TNF-alpha bioactivity-inhibiting therapy in ANCA-associated vasculitis: clinical and experimental considerations. Clinical Journal of The American Society of Nephrology: CJASN. 2006, 1 (5): 1100-7. 10.2215/CJN.02181205.
Lamprecht P, Till A, Steinmann J, Aries PM, Gross WL: Current state of biologicals in the management of systemic vasculitis. Annals of the New York Academy of Sciences. 2007, 1110: 261-70. 10.1196/annals.1423.028.
Lee RW, D'Cruz DP: Novel therapies for anti-neutrophil cytoplasmic antibody-associated vasculitis. Drugs. 2008, 68 (6): 747-70. 10.2165/00003495-200868060-00003.
Seitz M, Reichenbach S, Bonel HM, Adler S, Wermelinger F, Villiger PM: Rapid induction of remission in large vessel vasculitis by IL-6 blockade. A case series. Swiss Medical Weekly. 2011, 141: w13156-
Besbas N, Saatci U, Ruacan S, Ozen S, Sungur A, Bakkaloglu A: The role of cytokines in Henoch Schönlein purpura. Scandinavian Journal of Rheumatology. 1997, 26 (6): 456-60. 10.3109/03009749709065719.
Flatau E, Kohn D, Schiller D, Lurie M, Levy E: Schönlein -Henoch syndrome in patients with familial Mediterranean fever. Arthritis & Rheumatism. 1982, 25 (1): 42-7. 10.1002/art.1780250107.
Caglar MK: Familial Mediterranean fever after recovery from Schönlein - Henoch syndrome. Arthritis & Rheumatism. 1983, 26 (12): 1536-
Lange-Sperandio B, Mohring K, Gutzler F, Mehls O: Variable expression of vasculitis in siblings with familial Mediterranean fever. Pediatric Nephrology. 2004, 19 (5): 539-43. 10.1007/s00467-004-1440-1.
Soylu A, Kasap B, Turkmen M, Saylam GS, Kavukcu S: Febrile myalgia syndrome in familial Mediterranean fever. JCR: Journal of Clinical Rheumatology. 2006, 12 (2): 93-6. 10.1097/01.rhu.0000208635.64537.10.
Tekin M, Yalcinkaya F, Tumer N, Cakar N, Kocak H, Ozkaya N: Familial Mediterranean fever--renal involvement by diseases other than amyloid. Nephrology Dialysis Transplantation. 1999, 14 (2): 475-9. 10.1093/ndt/14.2.475.
Ozdogan H, Arisoy N, Kasapcapur O, Sever L, Caliskan S, Tuzuner N: Vasculitis in familial Mediterranean fever. Journal of Rheumatology. 1997, 24 (2): 323-7.
Saatci U, Ozen S, Ozdemir S, Bakkaloglu A, Besbas N, Topaloglu R: Familial Mediterranean fever in children: report of a large series and discussion of the risk and prognostic factors of amyloidosis. European Journal of Pediatrics. 1997, 156 (8): 619-23. 10.1007/s004310050677.
Ozkaya O, Bek K, Alaca N, Ceyhan M, Acikgoz Y, Tasdemir HA: Cerebral vasculitis in a child with Henoch-Schönlein purpura and familial Mediterranean fever. Clinical Rheumatology. 2007, 26 (10): 1729-32. 10.1007/s10067-006-0485-x.
Balbir-Gurman A, Nahir AM, Braun-Moscovici Y: Vasculitis in siblings with familial Mediterranean fever: a report of three cases and review of the literature. Clinical Rheumatology. 2007, 26 (7): 1183-5. 10.1007/s10067-006-0323-1.
Unal S, Gucer S, Kale G, Besbas N, Ozen S, Gumruk F: Severe Henoch-Schönlein purpura in a thalassemic patient under deferiprone treatment. American Journal of Hematology. 2008, 83 (2): 165-6. 10.1002/ajh.21052.
Wickiser JE, Saulsbury FT: Henoch-Schönlein purpura in a child with hyperimmunoglobulinemia D and periodic fever syndrome. Pediatric Dermatology. 2005, 22 (2): 138-41. 10.1111/j.1525-1470.2005.22210.x.
Tarshish P, Bernstein J, Edelmann CM: Henoch-Schönlein purpura nephritis: course of disease and efficacy of cyclophosphamide. Pediatric Nephrology. 2004, 19 (1): 51-6. 10.1007/s00467-003-1315-x.
Oner A, Tinaztepe K, Erdogan O: The effect of triple therapy on rapidly progressive type of Henoch-Schönlein nephritis. Pediatric Nephrology. 1995, 9 (1): 6-10. 10.1007/BF00858954.
Besbas N, Duzova A, Topaloglu R, Gok F, Ozaltin F, Ozen S: Pulmonary haemorrhage in a 6-year-old boy with Henoch-Schönlein purpura. Clinical Rheumatology. 2001, 20 (4): 293-6. 10.1007/PL00011205.
Acknowledgements and funding
The authors would like to acknowledge the patient and her family for their consent to publish this report. The efforts of MT and KMO were supported by the Department of Pediatrics, Universityof Oklahoma Health Sciences Center, Oklahoma City, OK, US.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
EMB reviewed the medical records of this child, drafted the manuscript and designed the figure. MT was the nephrologist managing the patient throughout her course, and contributed to writing the manuscript. KMO was the rheumatologist consulting on this patient, and wrote the literature review and background of the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Boyer, E.M., Turman, M. & O'Neil, K.M. Partial response to anakinra in life-threatening Henoch-Schönlein purpura: case report. Pediatr Rheumatol 9, 21 (2011). https://doi.org/10.1186/1546-0096-9-21
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1546-0096-9-21