Abstract
Background
Cardiac magnetic resonance (CMR) T1 mapping has been used to characterize myocardial diffuse fibrosis. The aim of this study is to determine the reproducibility and sample size of CMR fibrosis measurements that would be applicable in clinical trials.
Methods
A modified Look-Locker with inversion recovery (MOLLI) sequence was used to determine myocardial T1 values pre-, and 12 and 25min post-administration of a gadolinium-based contrast agent at 3 Tesla. For 24 healthy subjects (8 men; 29 ± 6 years), two separate scans were obtained a) with a bolus of 0.15mmol/kg of gadopentate dimeglumine and b) 0.1mmol/kg of gadobenate dimeglumine, respectively, with averaged of 51 ± 34 days between two scans. Separately, 25 heart failure subjects (12 men; 63 ± 14 years), were evaluated after a bolus of 0.15mmol/kg of gadopentate dimeglumine. Myocardial partition coefficient (λ) was calculated according to (ΔR1myocardium/ΔR1blood), and ECV was derived from λ by adjusting (1-hematocrit).
Results
Mean ECV and λ were both significantly higher in HF subjects than healthy (ECV: 0.287 ± 0.034 vs. 0.267 ± 0.028, p=0.002; λ: 0.481 ± 0.052 vs. 442 ± 0.037, p < 0.001, respectively). The inter-study ECV and λ variation were about 2.8 times greater than the intra-study ECV and λ variation in healthy subjects (ECV:0.017 vs. 0.006, λ:0.025 vs. 0.009, respectively). The estimated sample size to detect ECV change of 0.038 or λ change of 0.063 (corresponding to ~3% increase of histological myocardial fibrosis) with a power of 80% and an alpha error of 0.05 for heart failure subjects using a two group design was 27 in each group, respectively.
Conclusion
ECV and λ quantification have a low variability across scans, and could be a viable tool for evaluating clinical trial outcome.
Similar content being viewed by others
Background
Diffuse myocardial fibrosis (DMF) is a common histological feature of the failing heart and is present in many conditions, ranging from advanced aging to hypertension or hypertrophic cardiomyopathy [1–3]. DMF is thought to be primarily responsible for increased myocardial stiffness and diastolic dysfunction: an increasingly common condition in the elderly [4, 5]. Endomyocardial biopsy (EMB) is the standard of reference for quantifying DMF, but is an invasive procedure and prone to sampling error [6, 7].
Myocardial composition may be probed noninvasively by measuring the T1 time of the myocardium, termed T1 mapping. DMF results in increased collagen content with expansion of the extracellular space to a greater extent than that of normal myocardium [8, 9], resulting in accumulation of gadolinium-based contrast agents (GBCA). This, in turn, lowers the T1 time of the myocardium. Altered myocardial T1 times have been demonstrated in a range of nonischemic cardiomyopathies [10], including chronic aortic regurgitation [11], heart failure [7], aortic stenosis [12], and adult congenital heart disease [13].
Unfortunately, absolute quantification of T1 time is influenced by many factors, including the relaxivity of the GBCAs, the delay time after injection, and renal function (glomerular filtration rates, GFR) [14]. As an alternative, other indices of DMF have been considered, such as extracellular volume fraction (ECV) and partition coefficient (λ) [15–18]. Of note, there is considerably less change in ECV over time at steady state compared to relatively large changes in T1 values as a function of time after GBCA injection [19, 20]. In addition, ECV is relatively robust as a function of field strength [21]. Thus, ECV and partition coefficient are likely to be more favorable measures to determine change in DMF as a result of treatment or disease.
Therapeutic agents targeted at reducing DMF have been actively investigated in animal models [22–24]. To date, no human prospective studies with the goal of reducing DMF have been reported. In order to provide utility as a biomarker for longitudinal studies, one must estimate the test, re-test (inter-study) reproducibility of ECV and partition coefficient. Inter-study reproducibility in turn is affected by factors such as measurement error (e.g. due to patient motion or reader variability), variation in MRI scanner performance or pulse sequences and contrast agents. Knowledge of inter-study reproducibility can be used to estimate the sample size needed to demonstrate a statistically significant change in ECV or partition coefficient.
The purpose of this study was to estimate the variability of quantitative T1 measurements and, in particular, of the derived values of ECV and partition coefficient. We then provide sample size estimates to determine the potential of cardiac magnetic resonance (CMR) T1 data to be used as a noninvasive biomarker aimed at identifying reduction of DMF in response to a therapeutic intervention.
Methods
Study population
This study was approved by our institutional review board. All study participants provided written informed consent. Twenty-four healthy volunteers (8 men; 29 ± 6 years) without a history of cardiovascular or systemic disease were enrolled. The ECG obtained prior to the CMR exam did not show any abnormality and the physical exam performed by a physician did not reveal any pathologic finding. Normal left ventricular (LV) and right ventricular (RV) volumes and systolic functions were confirmed by CMR. The healthy subjects’ data has been previous published by our group [25]. In addition, twenty-five heart failure (HF) subjects (12 men; mean age ± SD, 63 ± 14 years) with NYHA classification II or greater were enrolled.
CMR protocol
All CMR exams were performed using a 3-Tesla scanner (Verio, Siemens Medical Systems, Erlangen, Germany) with a 32-channel cardiovascular array coil. T1 quantification was performed with a modified Look-Locker with inversion recovery (MOLLI) sequence [26] acquired during end-expiratory apnea in a mid-ventricular short axis view before and 12, and 25 minutes after GBCA. The MOLLI protocol has two inversion blocks; three images are acquired after the first inversion pulse, followed by a pause of three heart beats, then five images are acquired after a second inversion pulse [20]. Other CMR parameters were: non-segmented, steady state free precession read out in mid-diastole; FOV 290 to 360 mm; readout resolution 192; phase resolution 75% to 85%; slice thickness 8 mm; TR/TE 1.9/1.0ms, minimum inversion time 110ms, inversion time increment 80ms, flip angle 35°; GRAPPA parallel imaging factor 2, no partial Fourier in the phase encode dimension.
GBCA was injected intravenously at 2 ml/sec using a power injector and followed by a 20ml saline bolus administered at the same flow rate. Both healthy and HF subjects underwent CMR examination with 0.15mmol/kg of gadopentate dimeglumine. Healthy volunteers also underwent another CMR examination with the same CMR protocol with 0.1mmol/kg of gadobenate dimeglumine. The mean delay between the two studies was 51 ± 34 days.
Left ventricular volume and function were evaluated with steady state free precession cine imaging in short axis stack and in three long axis views. Late gadolinium enhancement (LGE) was acquired in the same position as cine images using a phase sensitive inversion recovery gradient echo sequence [27] after 15min of GBCA injection. Blood samples were taken 1 to 4 hours prior to the CMR to determine the HCT and creatinine.
Image analysis
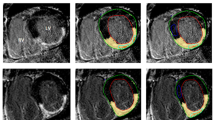
T1 maps were generated by three points pixel-wise curve fitting [28] and stored in Digital Imaging and Communications in Medicine (DICOM) Format. To extract myocardial T1 value, endocardial and epicardial contours were manually traced using QMass MR 7.2 (Medis, Leiden, Netherlands), and the myocardial circumference was divided into segments according to the American Heart Association 17-segment model [29]. Care was taken to exclude epicardial structures and blood from the contours. T1 value of the blood pool was measured by manually drawing a region of interest in the left ventricular cavity excluding papillary muscles. The image quality for all segments was visually rated using a scale in which a score of 3 indicated that image quality was good, with no artifacts; a score of 2, that image quality was satisfactory, with minor artifacts; and a score of 1, that an image was non-evaluable with major artifact, as described by Messroghli [30]. T1 values from segments that were rated as non-evaluable were excluded from analysis. ECV and λ values were calculated according to the following formulae [15]:
Where ECV, λ, and HCT are given as percentages.
Statistical analysis
Statistical analyses were performed using SAS 9.1 (Cary, North Carolina, USA) and MedCalc 12.2 (MedCalc Software, Mariakerke, Belgium). Sample size estimation was performed using PASS 2008 (Kaysville, Utah, USA). For comparison of the means between groups, one-way analysis of variance with post-hoc comparison was performed. Data are presented as mean ± standard deviation. Statistical significance was defined as P < 0.05.
The intra-study and inter-study reproducibility were assessed by calculating the difference and standard deviation between results. The coefficient of variability was calculated as the standard deviation of the difference divided by the mean of the parameter under consideration. Intra-study reproducibility compares the difference of ECV and partition coefficient at the 12-minute and 25-minute time points of the same study session: this is the best case scenario for testing ECV and partition coefficient reproducibility. Inter-study reproducibility, which compares ECV and partition coefficient results of two different study sessions, is the standard test-retest reliability. The inter-study reproducibility – the standard deviation of the mean difference – is the key factor for determining the ability of a technique to perform longitudinal examinations to detect a change. High reproducibility (low inter-study standard deviation) leads to greater reliability of observed changes in a parameter and a smaller sample size in clinical trials.
The sample size required by ECV or λ to show a clinical change with a power of 80% and an α error of 0.05 were calculated using the following formula:
Where n is the sample size needed, α is the significant level, P is the study power required, and f is the value of the factor for different values of α and P, with σ as the inter-study standard deviation and δ as the desired difference to be detected [31, 32].
Results
Study subject characteristics are given in Table 1. CMR was well tolerated by all subjects in the study. Both ECV and λ were significantly higher in the heart failure group compared to the healthy group (ECV: 0.287 ± 0.034 vs. 0.267 ± 0.028, p = 0.002; λ: 0.481 ± 0.052 vs.442 ± 0.037, p < 0.001). For the healthy group, there was no statistical difference between 12 minute and 25 minute ECV and λ (ECV: 0.264 ± 0.028 vs. 0.271 ± 0.028, p = NS; λ:0.436 ± 0.038 vs. 0.447 ± 0.037, p = NS). In addition, there was no significant difference for these parameters between gadopentetate dimeglumine and gadobenate dimeglumine (ECV: 0.271 ± 0.027 vs. 0.264 ± 0.029, p = NS; λ: 0.449 ± 0.039 vs. 0.435 ± 0.035, p=NS). Similarly, there was no statistical difference between 12 minute and 25 minute ECV and λ (ECV, 0.282 ± 0.033 vs. 0.289 ± 0.034, p = NS; λ: 0.475 ± 0.053 vs. 0.487 ± 0.051, p = NS) in the heart failure group. These results confirm the stability of ECV over moderate time intervals, and suggest a similar biodistribution of the two contrast agents. Of note, the image quality of T1 maps was significantly better in healthy group (2.8 ± 0.2 for healthy, 2.6 ± 0.4 for heart failure, p < 0.001).
Repeat measures of ECV and λ, intra-study assessment
The intra-study data of ECV and λ for both normal and HF groups are shown in Table 2. As expected, the correlation between the 12 minute and 25 minute of ECV and λ in the same study session was better in healthy subjects (0.98, 0.97) compared with that of the heart failure patients (0.88, 0.86). ECV has smaller Bland-Altman limits of agreement and intra-study standard deviation compared with partition coefficient (Table 2). The intra-study variability of both ECV and λ was larger in the heart failure group compared to that of the healthy group.
Inter-study difference and sample size estimation
The inter-study data of ECV and λ of the healthy group are shown in Table 3. Compared with the same intra-study data parameters, the correlation coefficients were lower for data acquired at a different study session. As expected, the CV and Bland-Altman limits of agreement of inter-study were also greater compared with that of the intra-study. Pre-contrast myocardial T1 exhibits high agreement between two study sessions.
In healthy subjects, the inter-study SD of ECV and λ were about 2.8-fold greater than the intra-study (ECV: 0.017 vs. 0.006; λ 0.025 vs. 0.009). In heart failure subjects, the intra-study of ECV and λ were 0.017 and 0.028, respectively. The sample size needed for the heart failure group was estimated for three different cases:
Case 1 Inter-study SD of ECV and λ estimated at 2.8 times greater than the intra-study SD (SD1 and N1 in Table 4),
Case 2 50% more variation than Case 1: Inter-study SD of ECV and λ estimated at 4.2 times greater than the intra-study SD (SD2 and N2 in Table 4),
Case 3 100% more variation than Case 1: Inter-study SD of ECV and λ estimated at 5.6 times greater than the intra-study SD (SD3 and N3 in Table 4),
Sample size estimation
In patients without LGE, the median percent histological fibrosis was 6.5% with inter-quartile range of 3.0 – 9.0% at endomyocardial biopsy [34]. Therefore, a 3% increase of histological fibrosis represents 25% more myocardial fibrosis over baseline would be clinically meaningful. The correlation coefficient between ECV quantification and histological fibrosis was 0.69 in a rat hypertension model [35]; and 0.89 in aortic stenosis and hypertrophic cardiomyopathy patients [12]. Take the average ECV correlation coefficient and the proposed 3% increase of histological fibrosis translates into a clinically meaningfully ECV change of 0.038 or lambda change of 0.063, assuming a hematocrit of 0.4.
For Case 1, 27 patients would be needed to detect a 0.038 change in ECV or 0.063 change in λ with 80% of power. For a “worst case” scenario with more variability as in Case 3 (e.g., a multi-center trial), 100 patients would be needed to detect a 0.038 change in ECV or 0.063 change in λ with 80% of power. For studies comparing active treatment vs. placebo, these sample size numbers need to be doubled. Figure 1 and Figure 2 show the sample sizes required for detection of a certain ECV or λ difference with a power of 80% and an alpha error of 0.05 under different inter-study standard deviations.
Sample size required in each group to detect a certain ECV difference with a two group design of 80% power and an alpha error of 0.05. The X axis values corresponding to the ECV difference need to be detected like the first column in Table 4. The three curves corresponding to case 1, 2 and 3 of Table 4. The smaller ECV difference and higher inter-study SD, the larger the sample size needed. The dashed line corresponding to the sample size needed to detect a 0.038 ECV difference for the three cases as showed in Table 4.
Sample size required in each group to detect a certain partition coefficient difference with a two group design of 80% power and an alpha error of 0.05. The X axis values corresponding to the partition coefficient difference need to be detected like the first column in Table 4. The three curves corresponding to case 1, 2 and 3 of Table 4. The smaller partition coefficient difference and higher inter-study SD, the larger the sample size needed. The dashed line corresponding to the sample size needed to detect a 0.063 partition coefficient difference for the three cases as showed in Table 4.
Discussion
DMF is a common endpoint associated with a wide range of cardiomyopathies. Preclinical studies have shown a reduction in DMF in response to angiotensin converting enzyme inhibitors [24, 36, 37] and N-acetylcysteine [22, 23]. For a similar human clinical trial, a paired study design offers more power to assess treatment response than an unpaired design. In this analysis, we provide estimates that are useful for such a paired study design, allowing the following conclusions: a) sample size needed to detect a meaningful clinical change are similar for ECV and partition coefficient; b) sample size estimates become highly sensitive to the inter-study reproducibility for a target change in ECV of less than 0.04-0.05; and c) sample sizes of 50-100 subjects in each study arm are likely to be necessary to detect changes of 0.03-0.05 in ECV for inter-study standard differences on the order of 0.05. Note that these sample size estimates would be equally applicable to a scenario that sought to halt progression of DMF, under the assumption that DMF would otherwise show a defined rate of increase over time.
CMR using LGE technique has been the standard of reference for detecting focal myocardial replacement fibrosis or scarring fibrosis in conditions such as myocardial infarction and hypertrophic cardiomyopathy [38, 39]. LGE relies on the differences in signal intensity between scarred and adjacent normal myocardium to generate image contrast [27, 40]. In an animal model of hypertension-induced DMF, LGE failed to detect any hyper-enhancement while histology analysis revealed an average of 9.9% collagen volume fraction [35]. Similarly, in cardiomyopathy patients, endomyocardial biopsy revealed the presence up to 20% diffuse myocardial fibrosis in patients without evidence of LGE [10]. Therefore, the detection of subtle DMF poses a significant challenge to LGE.
Extracellular volume fraction by CMR is a promising tool for visualization and quantification of local and diffuse myocardial abnormalities [15, 16, 41]. An animal study has demonstrated that elevated ECV was associated with increased collagen deposition [35]. Several human studies have been published using ECV as a surrogate biomarker for DMF [12, 13, 17, 18]. The reproducibility of a technique determines the sample size required to demonstrate a clinical change [42], which is a major cost in clinical trials. Messroghli reported the reproducibility data of myocardial T1 in a group of healthy volunteers [30], but there is a lack of data with regard to the reproducibility of ECV and partition coefficient.
In this study, there is good intra-study agreement between 12 minute and 25 minute ECV and partition coefficient in healthy volunteers, and this compares favorably with previous reports that ECV and partition coefficient are relatively stable after reaching the dynamic equilibrium between myocardium and blood pool [19, 43]. The intra-study variability of ECV and λ is higher in heart failure subjects. The primary reason for this was reduced image quality for heart failure subjects. Such patients have reduced capacity for breath-holding, resulting in motion artifacts. The MOLLI protocol used in this study requires a 11-heart-beat breath-hold, 5 heart beats shorter than the classic 17 heart beats MOLLI [44]. An even faster MOLLI protocol, like shMOLLI with 9 heart beats might be helpful in this regard [45]. Xue et al. [46] demonstrated a motion correction algorithm using image registration with synthetic image estimation to suppress the motion-induced artifacts in T1 maps. Robust motion correction was achieved by registering synthetic images to the corresponding MOLLI frames, and this method has been incorporated into the inline T1 mapping calculation of some scanners. In the future, a free-breathing T1 acquisition with motion correction would be ideal for the heart failure patients.
High reproducibility (low inter-study standard deviation) leads to greater reliability of observed changes in a parameter. This also results in cost-efficiency, as smaller sample size is required in clinical trials. Our sample size calculation demonstrates that a reasonable sample size is needed to detect a clinically meaningful change in ECV and partition coefficient.
Previously, CMR has successfully shown group differences in parameters such as T1 time or ECV between normal versus diseased study subjects [7, 15]. In this study, we also demonstrated statistically significant group differences in ECV using a relatively small sample size (24 normal subjects versus 25 HF subjects). However, the mean ECV value of the HF subjects (0.286) was within the observed range of values in normal subjects, previously reported to be 0.24-0.27 [13, 15, 19, 20]. Using a cut-value for normal ECV of 0.267, the sensitivity to detect abnormal ECV in HF subjects was only 38%. Thus, ECV is less likely to be useful as single cut-off value to identify abnormal versus normal subjects. However, change in ECV within an individual may be a more promising approach to assess, for example, a therapeutic response.
There are several limitations to this study. First, we estimated inter-study standardized differences for the heart failure patients using the healthy subjects as a reference group. Repeat gadolinium-enhanced MRI scans over a short interval was not performed due to below normal renal function in the HF group. Our estimates nevertheless appear to be of the correct magnitude. We experimentally detected a statistical significance in ECV with a total sample size of 49 in the study (24 in healthy group and 25 in heart failure group), similar to the 54 total sample size we estimated (27 subjects in each arm with 80% of power and an alpha error of 0.05). In addition, this is a single-center study. All scans were preformed on a single scanner with good adherence to the study protocol. For multi-center studies involving multiple scanners, a higher degree of variation is expected because of the difference of sequences, imagers, coil systems, and field strengths [47]. The inter-study reproducibility is related to sample size by a square function, therefore a much larger sample size is needed to compensate the increased variation in a multi-center study to detect ECV or partition coefficient change (Figure 1 and Figure 2).
Conclusion
In conclusion, ECV and partition coefficient have a relatively low variability for repeat scans, and could be a viable tool for evaluating clinical trial outcome. Sample size estimation showed that a study with 27 participants in each group could detect a 0.038 change in ECV or 0.063 change in partition coefficient with 80% of power, which corresponding to about 3% increase in histological collagen tissue.
Funding sources
Funded by the National Institutes of Health (NIH) intramural program.
References
Marijianowski MM, Teeling P, Mann J, Becker AE: Dilated cardiomyopathy is associated with an increase in the type I/type III collagen ratio: a quantitative assessment. J Am Coll Cardiol. 1995, 25: 1263-1272. 10.1016/0735-1097(94)00557-7.
Gazoti Debessa CR, Mesiano Maifrino LB, de Mesiano Maifrino LB: Age related changes of the collagen network of the human heart. Mech Ageing Dev. 2001, 122: 1049-1058. 10.1016/S0047-6374(01)00238-X.
Mewton N, Liu CY, Croisille P, Bluemke D, Lima JA: Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol. 2011, 57: 891-903. 10.1016/j.jacc.2010.11.013.
Brooks A, Schinde V, Bateman AC, Gallagher PJ: Interstitial fibrosis in the dilated non-ischaemic myocardium. Heart. 2003, 89: 1255-1256. 10.1136/heart.89.10.1255.
Udelson JE: Heart failure with preserved ejection fraction. Circulation. 2011, 124: e540-e543. 10.1161/CIRCULATIONAHA.111.071696.
Cooper LT, Baughman KL, Feldman AM, Frustaci A, Jessup M, Kuhl U, Levine GN, Narula J, Starling RC, Towbin J, Virmani R: The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Endorsed by the Heart Failure Society of America and the Heart Failure Association of the European Society of Cardiology. J Am Coll Cardiol. 2007, 50: 1914-1931. 10.1016/j.jacc.2007.09.008.
Iles L, Pfluger H, Phrommintikul A, Cherayath J, Aksit P, Gupta SN, Kaye DM, Taylor AJ: Evaluation of diffuse myocardial fibrosis in heart failure with cardiac magnetic resonance contrast-enhanced T1 mapping. J Am Coll Cardiol. 2008, 52: 1574-1580. 10.1016/j.jacc.2008.06.049.
Pereira RS, Prato FS, Wisenberg G, Sykes J: The determination of myocardial viability using Gd-DTPA in a canine model of acute myocardial ischemia and reperfusion. Magn Reson Med. 1996, 36: 684-693. 10.1002/mrm.1910360506.
Pereira RS, Prato FS, Sykes J, Wisenberg G: Assessment of myocardial viability using MRI during a constant infusion of Gd-DTPA: further studies at early and late periods of reperfusion. Magn Reson Med. 1999, 42: 60-68. 10.1002/(SICI)1522-2594(199907)42:1<60::AID-MRM10>3.0.CO;2-9.
Sibley CT, Noureldin RA, Gai N, Nacif MS, Liu S, Turkbey EB, Mudd JO, Lima JA, Halushka MK, Bluemke DA: T1 Mapping in Cardiomyopathy by Cardiac Magnetic Resonance: Comparision to Endomyocardial Biopsy. Radiology. 2012, In Press
Sparrow P, Messroghli DR, Reid S, Ridgway JP, Bainbridge G, Sivananthan MU: Myocardial T1 mapping for detection of left ventricular myocardial fibrosis in chronic aortic regurgitation: pilot study. AJR Am J Roentgenol. 2006, 187: W630-W635. 10.2214/AJR.05.1264.
Flett AS, Hayward MP, Ashworth MT, Hansen MS, Taylor AM, Elliott PM, McGregor C, Moon JC: Equilibrium Contrast Cardiovascular Magnetic Resonance for the Measurement of Diffuse Myocardial Fibrosis. Preliminary Validation in Humans. Circulation. 2010, 122: 138-144. 10.1161/CIRCULATIONAHA.109.930636.
Broberg CS, Chugh S, Conklin C, Sahn DJ, Jerosch-Herold M: Quantification of Diffuse Myocardial Fibrosis and its Association with Myocardial Dysfunction in Congenital Heart Disease. Circ Cardiovasc Imaging. 2010, 3: 727-734. 10.1161/CIRCIMAGING.108.842096.
Gai N, Turkbey EB, Nazarian S, van der Geest RJ, Liu CY, Lima JA, Bluemke DA: T1 mapping of the gadolinium-enhanced myocardium: adjustment for factors affecting interpatient comparison. Magnetic resonance in medicine: official journal of the Society of Magnetic Resonance in Medicine / Society of Magnetic Resonance in Medicine. 2011, 65: 1407-1415. 10.1002/mrm.22716.
Ugander M, Oki AJ, Hsu LY, Kellman P, Greiser A, Aletras AH, Sibley CT, Chen MY, Bandettini WP, Arai AE: Extracellular volume imaging by magnetic resonance imaging provides insights into overt and sub-clinical myocardial pathology. Eur Heart J. 2012, 33: 1268-1278. 10.1093/eurheartj/ehr481.
Nacif MS, Kawel N, Lee JJ, Chen X, Yao J, Zavodni A, Sibley CT, Lima JA, Liu S, Bluemke DA: Interstitial Myocardial Fibrosis Assessed as Extracellular Volume Fraction with Low-Radiation-Dose Cardiac CT. Radiology. 2012, 264: 876-883. 10.1148/radiol.12112458.
Sado DM, Flett AS, Banypersad SM, White SK, Maestrini V, Quarta G, Lachmann RH, Murphy E, Mehta A, Hughes DA, et al: Cardiovascular magnetic resonance measurement of myocardial extracellular volume in health and disease. Heart. 2012, 98: 1436-1441. 10.1136/heartjnl-2012-302346.
Mongeon FP, Jerosch-Herold M, Coelho-Filho OR, Blankstein R, Falk RH, Kwong RY: Quantification of Extracellular Matrix Expansion by CMR in Infiltrative Heart Disease. JACC Cardiovasc Imaging. 2012, 5: 897-907. 10.1016/j.jcmg.2012.04.006.
Schelbert EB, Testa SM, Meier CG, Ceyrolles WJ, Levenson JE, Blair AJ, Kellman P, Jones BL, Ludwig DR, Schwartzman D, et al: Myocardial extravascular extracellular volume fraction measurement by gadolinium cardiovascular magnetic resonance in humans: slow infusion versus bolus. J Cardiovasc Magn Reson. 2011, 13: 16-10.1186/1532-429X-13-16.
Lee JJ, Liu S, Nacif MS, Ugander M, Han J, Kawel N, Sibley CT, Kellman P, Arai AE, Bluemke DA: Myocardial T1 and extracellular volume fraction mapping at 3 tesla. J Cardiovasc Magn Reson. 2011, 13: 75-10.1186/1532-429X-13-75.
Kawel N, Nacif M, Zavodni A, Jones J, Liu S, Sibley CT, Bluemke DA: T1 mapping of the myocardium: Intra-individual assessment of the effect of field strength, cardiac cycle and variation by myocardial region. J Cardiovasc Magn Reson. 2012, 14: 27-10.1186/1532-429X-14-27.
Lombardi R, Rodriguez G, Chen SN, Ripplinger CM, Li W, Chen J, Willerson JT, Betocchi S, Wickline SA, Efimov IR, Marian AJ: Resolution of established cardiac hypertrophy and fibrosis and prevention of systolic dysfunction in a transgenic rabbit model of human cardiomyopathy through thiol-sensitive mechanisms. Circulation. 2009, 119: 1398-1407. 10.1161/CIRCULATIONAHA.108.790501.
Marian AJ, Senthil V, Chen SN, Lombardi R: Antifibrotic effects of antioxidant N-acetylcysteine in a mouse model of human hypertrophic cardiomyopathy mutation. J Am Coll Cardiol. 2006, 47: 827-834. 10.1016/j.jacc.2005.10.041.
Jones ES, Black MJ, Widdop RE: Angiotensin AT2 receptor contributes to cardiovascular remodelling of aged rats during chronic AT1 receptor blockade. J Mol Cell Cardiol. 2004, 37: 1023-1030. 10.1016/j.yjmcc.2004.08.004.
Kawel N, Nacif M, Zavodni A, Jones J, Liu S, Sibley CT, Bluemke DA: T1 mapping of the myocardium: intra-individual assessment of post-contrast T1 time evolution and extracellular volume fraction at 3T for Gd-DTPA and Gd-BOPTA. J Cardiovasc Magn Reson. 2012, 14: 26-10.1186/1532-429X-14-26.
Messroghli DR, Greiser A, Frohlich M, Dietz R, Schulz-Menger J: Optimization and validation of a fully-integrated pulse sequence for modified look-locker inversion-recovery (MOLLI) T1 mapping of the heart. J Magn Reson Imaging. 2007, 26: 1081-1086. 10.1002/jmri.21119.
Kellman P, Arai AE, McVeigh ER, Aletras AH: Phase-sensitive inversion recovery for detecting myocardial infarction using gadolinium-delayed hyperenhancement. Magn Reson Med. 2002, 47: 372-383. 10.1002/mrm.10051.
Messroghli DR, Rudolph A, Abdel-Aty H, Wassmuth R, Kuhne T, Dietz R, Schulz-Menger J: An open-source software tool for the generation of relaxation time maps in magnetic resonance imaging. BMC Med Imaging. 2010, 10: 16-10.1186/1471-2342-10-16.
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS, et al: Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002, 105: 539-542. 10.1161/hc0402.102975.
Messroghli DR, Plein S, Higgins DM, Walters K, Jones TR, Ridgway JP, Sivananthan MU: Human myocardium: single-breath-hold MR T1 mapping with high spatial resolution–reproducibility study. Radiology. 2006, 238: 1004-1012. 10.1148/radiol.2382041903.
Grothues F, Smith GC, Moon JC, Bellenger NG, Collins P, Klein HU, Pennell DJ: Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am J Cardiol. 2002, 90: 29-34. 10.1016/S0002-9149(02)02381-0.
Machin D, Campbell M, Fayers P, Pinol A: Sample Size Tables for Clinical Studies. 1997, Malden, MA: Blackwell Science, 2nd
Altman DG: Practical Statistics for Medical Research. 1990, London: Chapman and Hall, 440-
Sibley CT, Noureldin RA, Gai N, Nacif MS, Liu S, Turkbey EB, Mudd JO, van der Geest RJ, Lima JA, Halushka MK, Bluemke DA: T1 Mapping in Cardiomyopathy at Cardiac MR: Comparison with Endomyocardial Biopsy. Radiology. 2012, 265: 724-732. 10.1148/radiol.12112721.
Messroghli D, Nordmeyer S, Dietrich T, Dirsch O, Kaschina E, Savvatis K, OHI D, Klein C, Berger F, Kuehne T: Assessment of Diffuse Myocardial Fibrosis in Rats Using Small Animal Look-Locker Inversion Recovery (SALLI) T1 Mapping. Circ Cardiovasc Imaging. 2011, 4: 636-640. 10.1161/CIRCIMAGING.111.966796.
Tsutsumi Y, Matsubara H, Ohkubo N, Mori Y, Nozawa Y, Murasawa S, Kijima K, Maruyama K, Masaki H, Moriguchi Y, et al: Angiotensin II type 2 receptor is upregulated in human heart with interstitial fibrosis, and cardiac fibroblasts are the major cell type for its expression. Circ Res. 1998, 83: 1035-1046. 10.1161/01.RES.83.10.1035.
Varagic J, Susic D, Frohlich ED: Coronary hemodynamic and ventricular responses to angiotensin type 1 receptor inhibition in SHR: interaction with angiotensin type 2 receptors. Hypertension. 2001, 37: 1399-1403. 10.1161/01.HYP.37.6.1399.
Kim RJ, Fieno DS, Parrish TB, Harris K, Chen EL, Simonetti O, Bundy J, Finn JP, Klocke FJ, Judd RM: Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999, 100: 1992-2002. 10.1161/01.CIR.100.19.1992.
Mahrholdt H, Wagner A, Judd RM, Sechtem U, Kim RJ: Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur Heart J. 2005, 26: 1461-1474. 10.1093/eurheartj/ehi258.
Judd RM, Lugo-Olivieri CH, Arai M, Kondo T, Croisille P, Lima JA, Mohan V, Becker LC, Zerhouni EA: Physiological basis of myocardial contrast enhancement in fast magnetic resonance images of 2-day-old reperfused canine infarcts. Circulation. 1995, 92: 1902-1910. 10.1161/01.CIR.92.7.1902.
Robbers LF, Baars EN, Brouwer WP, Beek AM, Hofman MB, Niessen HW, van Rossum AC, Marcu CB: T1 mapping shows increased extracellular matrix size in the myocardium due to amyloid depositions. Circ Cardiovasc Imaging. 2012, 5: 423-426. 10.1161/CIRCIMAGING.112.973438.
Bottini PB, Carr AA, Prisant LM, Flickinger FW, Allison JD, Gottdiener JS: Magnetic resonance imaging compared to echocardiography to assess left ventricular mass in the hypertensive patient. Am J Hypertens. 1995, 8: 221-228. 10.1016/0895-7061(94)00178-E.
Flett AS, Hasleton J, Cook C, Hausenloy D, Quarta G, Ariti C, Muthurangu V, Moon JC: Evaluation of techniques for the quantification of myocardial scar of differing etiology using cardiac magnetic resonance. JACC Cardiovasc Imaging. 2011, 4: 150-156. 10.1016/j.jcmg.2010.11.015.
Messroghli DR, Radjenovic A, Kozerke S, Higgins DM, Sivananthan MU, Ridgway JP: Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med. 2004, 52: 141-146. 10.1002/mrm.20110.
Piechnik SK, Ferreira VM, Dall'Armellina E, Cochlin LE, Greiser A, Neubauer S, Robson MD: Shortened Modified Look-Locker Inversion recovery (ShMOLLI) for clinical myocardial T1-mapping at 1.5 and 3 T within a 9 heartbeat breathhold. J Cardiovasc Magn Reson. 2010, 12: 69-10.1186/1532-429X-12-69.
Xue H, Shah S, Greiser A, Guetter C, Littmann A, Jolly MP, Arai AE, Zuehlsdorff S, Guehring J, Kellman P: Motion correction for myocardial T1 mapping using image registration with synthetic image estimation. Magn Reson Med. 2012, 67: 1644-1655. 10.1002/mrm.23153.
Sasaki M, Yamada K, Watanabe Y, Matsui M, Ida M, Fujiwara S, Shibata E, Acute Stroke Imaging Standardization Group-Japan I: Variability in absolute apparent diffusion coefficient values across different platforms may be substantial: a multivendor, multi-institutional comparison study. Radiology. 2008, 249: 624-630. 10.1148/radiol.2492071681.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors read and critically edited the initial manuscript, added intellectual content, and approved the final version. DAB and SL designed, coordinated and conducted the study; JJ recruited subjects; SL, NK and MSN acquired images; SL, NK and MSN analyzed images; JH conducted the statistical analyses. PK assisted with pulse sequence optimization and added critical manuscript content. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Liu, S., Han, J., Nacif, M.S. et al. Diffuse myocardial fibrosis evaluation using cardiac magnetic resonance T1 mapping: sample size considerations for clinical trials. J Cardiovasc Magn Reson 14, 90 (2012). https://doi.org/10.1186/1532-429X-14-90
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1532-429X-14-90