Abstract
T-cell receptor excision circles (TRECs) and kappa-deleting recombination excision circles (KRECs) are circular DNA segments generated in T and B cells during their maturation in the thymus and bone marrow. These circularized DNA elements persist in the cells, are unable to replicate, and are diluted as a result of cell division, thus are considered markers of new lymphocyte output. The quantification of TRECs and KRECs, which can be reliably performed using singleplex or duplex real-time quantitative PCR, provides novel information in the management of T- and B-cell immunity-related diseases. In primary immunodeficiencies, when combined with flow cytometric analysis of T- and B-cell subpopulations, the measure of TRECs and KRECs has contributed to an improved characterization of the diseases, to the identification of patients’ subgroups, and to the monitoring of stem cell transplantation and enzyme replacement therapy. For the same diseases, the TREC and KREC assays, introduced in the newborn screening program, allow early disease identification and may lead to discovery of new genetic defects. TREC and KREC levels can also been used as a surrogate marker of lymphocyte output in acquired immunodeficiencies. The low number of TRECs, which has in fact been extensively documented in untreated HIV-infected subjects, has been shown to increase following antiretroviral therapy. Differently, KREC number, which is in the normal range in these patients, has been shown to decrease following long-lasting therapy. Whether changes of KREC levels have relevance in the biology and in the clinical aspects of primary and acquired immunodeficiencies remains to be firmly established.
Similar content being viewed by others
Review
V(D)J recombination and formation of excision circles
Thymus and bone marrow (BM) are the primary anatomic sites for new T- and B-cell generation from undifferentiated hematopoietic precursors (Figure 1). Throughout this process, a highly heterogeneous lymphocyte repertoire is generated allowing the resulting cells to respond to a wide variety of antigenic stimuli [1–3]. Physiologically, T-cell maturation in the thymus progresses through distinct stages that are phenotypically defined by the expression of the T-cell receptor (TR) and the CD4 and CD8 co-receptors. On the basis of a programmed expression of distinct cell surface markers and of ordered gene rearrangements, thymocytes undergo different maturation steps before reaching the end stage [4]. B-lymphocyte development is divided into two main phases: an initial antigen-independent phase, in which precursor B cells mature into functional B lymphocytes in the BM, and an antigen-dependent phase, in which the mature B-cell compartment is maintained by regeneration, turnover and selection processes [5].
New T- and B-cell generation. A) Lymphoid progenitors migrate to the thymus, where they progressively rearrange T-cell receptor (TR) genes. Before the rearrangements of the TR alpha (TRA) locus, the TR delta (TRD) locus, which lies within the TRA locus, must be excised by DNA recombinations. Among them, the δREC–ψJα recombination, which occurs in about 70% of thymocytes [13], leads to the generation of a δREC–ψJα coding joint (CJ) in the chromosome and of a δREC–ψJα signal joint (SJ) in a circle of DNA called TR excision circle (TREC). Maturing thymocytes undergo 3–4 intrathymic divisions, in which TRECs cannot be duplicated; thus, only a fraction (about 1:8–1:16) of the originally TREC+ cells will leave the thymus as TREC+ recent-thymic emigrants (RTE) [6,13,15]. Peripheral proliferation will determine further TREC dilution. B) In the bone marrow, progenitor B cells undergo V(D)J rearrangements of the Ig heavy chain (IGH) locus followed by those of the light chains (IGK and IGL). After successful IGH rearrangements at the Pre-B stage, a VJ recombination on the IGK locus is initiated. If it is not productive, another recombination between the Ig kappa deleting element or like (IGKDEL) and one of the upstream recombination signal sequences (RSS) renders the IGK allele non-functional. In 30%-50% of cases, this occurs through the intronRSS-IGKDEL rearrangement, by which the IGKC exon and its enhancers (iEκ, 3’Eκ) are excised, with the creation of the so-called kappa-deleting recombination excision circles (KRECs). Thus, KRECs carry an intronRSS-IGKDEL SJ, and remain in the cells, but, as they cannot be replicated, they will be diluted during peripheral expansion of mature B cells. Instead, an intronRSS-IGKDEL CJ is formed and stably retained in the genomic DNA [7,8,10], because, due to the enhancer loss, any further rearrangement in the IGK locus is precluded.
During the maturation processes of TR alpha/beta chains and of B-cell receptor (BcR) heavy and light chains, genomic rearrangements of antigen receptor genes generate functional receptors. This process is necessary because the gene complexes encoding the TR and BcR components do not contain a functional first exon, while including multiple variable (V), diversity (D), and joining (J) genes. In the antigen-independent differentiation phase, stepwise rearrangements are introduced into the genome to couple one of each segment together to form a functional first exon. The rearrangement of the TR alpha (TRA) genes has the peculiarity of involving the excision of delta-coding segments that, being nestled in the TRA locus between the TRAV and TRAJ genes, must be removed in order to allow the generation of the TRA chain. The excised DNA is circularized due to the ligation of the blunt DNA signal ends, thereby forming a signal joint (SJ) within the stable circular excision products termed TR excision circles (TRECs) [6]. Therefore, TRECs are the excised DNA circles formed during the process of TRA chain VJ recombination (Figure 1A). In B-cell maturation, K-deleting recombination excision circles (KRECs) are the products of recombination events determining the allelic and isotypic exclusion of the Ig kappa (IGK) locus [7–9]. They are created in those B lymphocytes that, after completing the IG heavy gene rearrangement, have failed to productively rearrange IGK genes on one or both alleles [10]. In these cells, the IGK locus becomes non-functional through the deletion of the IGK constant gene (IGKC) resulting from the recombination of the Ig kappa deleting element or like (IGKDEL), which is a sequence located approximately 24 kb downstream of the IGKC, with one of the upstream recombination signal sequences (RSS) located either at the 3’ side of a IGK variable gene segment (IGKV) or in the intron between the IGK joining segments (IGKJ) and the IGKC[10]. When the IGKDEL recombines with the RSS located in the IGKJ-IGKC intron (intronRSS), the formation of a coding joint (CJ) precludes any further rearrangements in the IGK locus. Thus, the CJ remains present in the genome, whereas an intronRSS-IGKDEL SJ is formed in the portion of DNA that is removed, thus forming the excision circle KREC (Figure 1B) [7, 8].
Quantification of TRECs and KRECs
Assays for quantification of TRECs and KRECs in peripheral blood are now performed in clinical and research laboratories to monitor naive T and B cells emigrating from the thymus and BM, respectively. Although TRECs are not markers of recent thymic emigrants by definition, because a small part remains present in peripheral blood in the so-called “old” thymic emigrants [6, 11–14], several properties identify them as “bona fide” useful markers of thymic output. They are stable, do not replicate upon cell division and therefore are diluted in the progeny, do not degrade easily over time, and are (almost) exclusively of thymic origin, without extrathymic sources of TR rearrangements [6]. In particular, approximately 70% of T cells differentiating in the thymus contain TRECs [11], before being diluted 1:8–1:16 because of intrathymic divisions occurring during the last steps of maturation [13, 15]. The TREC quantitative assay, initially proposed by Douek DC et al. [6], has been later modified in different ways and TREC number has been evaluated in different biological samples or calculated by different approaches, resulting into hardly comparable results. In fact, a more accurate TREC measurement has been obtained when quantification was performed relative to a control gene, such as chemokine (C-C motif) receptor 5, albumin, or TRA constant (TRAC) gene [12, 16, 17]. Furthermore, TREC content in peripheral blood has been reported either relative to peripheral blood mononuclear cells (PBMC), or quantified within sorted individual T-cell subsets [12, 18]. In addition, the quantity of TRECs has been expressed either as absolute number of TREC molecules per μg of DNA within PBMC or T lymphocytes [16, 19, 20], or per 106 cells, on the basis of the theoretical recovery of 1 μg of DNA from approximately 150,000 cells [21, 22]. Because in adults’ samples TREC calculation per 106 PBMC can lead to erroneous interpretations due to the diluting effect of peripheral T-cell divisions, this limitation has been, at least in part, overcome by expressing TRECs per ml of blood [23, 24]. Finally, in spite of the present lack of information regarding TREC half-life [13], several mathematical models, which have taken into consideration confounders such as cell death, longevity of naive T cells, and intracellular degradation, have been recently proposed to identify the actual thymic output as a function of the TREC number [22, 24].
Scanty information are presently available regarding the quantification of KRECs. Because the CJ remains in the genome, whereas the SJ present in the KREC is diluted after each cell division, the difference between the cycle threshold (Ct) values of the SJ and the CJ, obtained by real-time PCR, has been initially exploited to calculate the average number of divisions in a pool of B cells. In particular, because the intronRSS-IGKDEL rearrangement occurs late during BM differentiation, this measure is a good estimate of the average number of divisions performed by mature B cells after leaving the precursor B-cell compartment [7]. Furthermore, the frequency of B-cells that contain an intronRSS–IGKDEL rearrangement can be determined when a control gene is quantified together with the CJ [8]. A modified technique was used to determine the number of developing B lymphocytes in the BM of children with B-precursor acute lymphoblastic leukemia treated with allogeneic human stem-cell transplantation (HSCT) [25]. In this assay, KRECs were calculated by using the ΔCt method with a calibrator sample and by correcting the quantity and quality of DNA in the samples employing albumin as reference gene. The final number of KRECs relative to the calibrator was expressed as: 2Ctcalibrator-Ctsample + log2(DNAconc. calibrator/DNAconc. sample).
More recently, we modified this newly proposed KREC assay and the widely used TREC assay by setting up a duplex quantitative real-time PCR that, by measuring together TRECs and KRECs, allows the quantification of newly produced T and B lymphocytes [26, 27]. The main advantage of the combined assay is that the variability related to direct DNA quantification is eliminated by the use of a unique standard curve obtained by diluting the triple-insert plasmid, which contains TREC, KREC and TRAC fragments in a 1:1:1 ratio [26]. The last serves as a control for both the quality and quantity of genomic DNA in the sample. Furthermore, the simultaneous quantification of the two targets in the same reaction, results into a containment of laboratory costs. The duplex TREC/KREC assay is performed on DNA extracted from PBMC isolated from heparinized blood using primers and probes specific for TRECs, KRECs and TRAC. TRECs or KRECs per 106 PBMC are calculated as the ratio between the mean number of TRECs or KRECs and the mean copy number of TRAC divided by 2, which is the number of TRAC copies per cell, and multiplied by 106. This value, in conjunction with the combined lymphocyte - monocyte number in one ml of blood (which are the cells contained in a PBMC preparation), is used to calculate the number of TRECs or KRECs per ml of blood (TRECs or KRECs per 106 PBMC) × (lymphocyte plus monocyte count in one ml of blood)/106[26].
TRECs and KRECs as markers of primary and acquired immunodeficiencies
TREC level has been extensively assayed in children with primary immunodeficiencies (PID) in whom the decreased number and function of T and/or B cells result into significant impairment of immunity. These rare, genetically determined disorders, which characteristically manifest during infancy and childhood with increased frequency of infections caused by unusual pathogens, are often accompanied by immunoregulatory defects [28]. Severe combined immunodeficiency (SCID), the most serious and lethal form of PID, is characterized by profound deficiencies of T- and B-cell functions and a low number of natural killer (NK) cells [29, 30]. Infants with SCID develop failure to thrive, chronic diarrhea, and infections in the first few months of life. Graft-versus-host disease (GVHD), caused by maternal T-cell engraftment, may occur in these patients, who also show skin rash and organomegaly. All infants with the typical form of SCID, as well as those with another form of SCID, known as the Omenn syndrome, show extremely low or undetectable TREC levels (see Table 1, which completes and extends the data reported by van Zelm et al.) [8, 26, 31–42]. Despite the normal number of circulating T cells, abnormally low TREC levels were also observed in patients with zeta-chain (TCR) associated protein kinase 70kDa (ZAP70) deficiency and with the 22q11.2 deletion syndrome, especially in those without an identifiable thymus [31, 38]. In contrast, patients with mutations in CD40 ligand, forkhead box protein 3 (FOXP3), and interleukin 10 receptor alpha chain, as well as patients with the p.R222C mutation in the interleukin 2 receptor gamma gene, display normal TREC levels [31]. As in SCID patients, the TREC assay contributed to understand the pathophysiology of other PID such as CD4+ T lymphocytopenia. In these patients, TREC levels correlated to the severity of the T-cell immunodeficiency [43]. Finally, TREC quantification has been used to improve our understanding of the T-cell abnormality that is sometimes observed in common variable immunodeficiency (CVID), although its precise role in this condition is still a matter of debate. While in fact some authors reported that the median TREC level in these patients was significantly higher than in healthy subjects, others found that this number was significantly reduced, in particular in patients characterized by a low number of switched/memory B cells (sIgD-CD27+), by a large proportion of CD19hiCD21lo cells, and by an increased risk of autoimmunity and splenomegaly [41, 44–46].
KREC level has been evaluated only very recently in children with PID, and mainly in patients affected by X-linked or non X-linked agammaglobulinemia (XLA and non-XLA, respectively), and in those with CVID. While XLA, the most severe form of B-cell defects, results from a mutation in the Bruton agammaglobulinemia tyrosine kinase (BTK) gene that causes a B-cell differentiation arrest in the BM, with consequent absence of mature B cells and serum Ig, non-XLA is characterized by hypogammaglobulinemia with decreased B-cell counts in the absence of the BTK gene mutation [47]. In both forms, which account for about 20% of all B-cell defects, recurrent infections appear between 3 and 18 months of age [48]. KREC measurement has been proposed as a potential tool for the identification of these two diseases, because B-cell maturation defects occur before IGKDEL events, and therefore KRECs should be not produced/detected in these patients. Indeed, a study performed by analyzing KRECs derived from dried blood spots revealed that no KRECs were detected in 30 XLA and 5 non-XLA patients [40]. We employed the combined TREC/KREC assay to measure the extent of T- and B-cell neoproduction in CVID adult patients with no acute infections and undergoing Ig passive immunotherapy. The number of TREC+ lymphocytes, which depended on age and gender, was significantly reduced. At the same time, KREC number was lower than in controls, but it did not change with age and was not influenced by the gender. Of note, 35% of CVID patients had less KRECs/ml than the 5th percentile calculated in controls [41]. On the contrary, newborns affected by CVID (and those with some other typical SCID, see Table 1) displayed a number of KRECs comparable to that of healthy newborns [34]. Very recently, Kamae et al. [42] showed that the amount of TRECs and KRECs can be a useful marker to assess the pathogenesis and clinical severity of CVID in distinct patients.
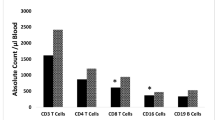
While the quantification of TRECs has been performed for years and is used as a surrogate marker of thymic output in HIV-infected patients [6], the precise interpretation of TREC data obtained in acquired immunodeficiency subjects is more challenging. Indeed, it depends heavily on the assumed fate of naive T cells, recent thymic emigrants in particular [12, 24, 49], and on the different clinical-pathological parameters of infected subjects, such as age and plasma HIV-1 RNA. Although several studies have shown that HIV-infected subjects have a lower number of TRECs than that found in age-matched uninfected individuals [6, 12, 16, 50], the TREC number is variable among patients and overlaps with that of controls [16]. Using the TREC/KREC assay we found that the number of TREC+ cells of patients that need antiretroviral therapy was significantly lower not only when compared to controls, but also when compared to HIV-infected patients with a relatively conserved CD4 cell number and not requiring treatment according to the current guidelines. In this latter group, the number of KRECs was significantly higher than that found in patients needing treatment, but similar to that found in age-matched healthy controls [51].
TREC/KREC assay for detection of neonatal primary immunodeficiency diseases
Early recognition of SCID should be considered a pediatric emergency, because a diagnosis before the vaccination programs and the onset of recurrent infections allows lifesaving HSCT, enzyme replacement, or gene therapy [52–60]. Similarly, early diagnosis and treatment, including periodical intravenous Ig replacement therapy, are essential to improve the prognosis and the quality of life of patients with B-cell defects. However, infants with SCID or agammaglobulinemia often appear normal at birth, have no family history of immunodeficiency [61], and, consequently, many of them are not identified until life-threatening infections occur.
The demonstration that the TREC assay detects SCID patients regardless of the underlying genetic defects [33] and that agammaglobulinemia patients can be identified with KREC quantification [40], suggested that the TREC and KREC assays can be used for the detection of SCID and agammaglobulinemia in newborn screening (NBS) programs. This is particularly true for SCID, which satisfies the criteria recommended by the Secretary’s Advisory Committee on Heritable Disorders in Newborns and Children [62]. The TREC assay was the first to be modified and calibrated to allow the test to be performed on DNA extracted from small spots of dried blood, to be highly sensitive and specific for SCID, cost-effective, reproducible and, therefore, amenable to be used in a population-based screening [63]. Pilot studies of NBS for SCID, integrated with diagnosis and management guidelines, have been performed in some U.S. states [61]. Accordingly, in 2008, Wisconsin became the first state to implement mandatory NBS for T-cell deficiencies [37], followed, in February 2009, by Massachusetts [32, 64] and, later, by New York, Navajo Nation, California, Puerto Rico and Louisiana [65]. By using in-house modifications of the TREC assay (with the exception of California, where a TREC assay kit under development by a company was used), these pilot studies identified, among the 961,925 newborns screened, several cases of T-cell deficits, 14 of which resulted to be SCID at the confirmatory tests, 6 SCID variants, and 40 T-cell lymphopenia not related to SCID [32, 35, 63–65]. All infants with SCID identified in Wisconsin and Massachusetts have undergone transplantation or enzyme replacement therapy and are all alive [36, 37]. More recently, also the TREC/KREC assay was modified, making it suitable to be performed on a single Guthrie card punch. This assay has been validated in a cohort of 2,560 NBS cards from healthy neonates and used to identify patients with SCID, XLA, ataxia-telangiectasia, and Nijmegen-breakage-syndrome [34]. The early diagnosis of children with XLA is expected to significantly improve their quality of life and contribute to a reduction of health care costs. Indeed, because their clinical phenotype is less severe than that in SCID, the risk of undiagnosed disease in their first years of life in absence of a screening program would foster the development of more severe organ damage.
Conclusively, considering that the TREC measurement is performed at the relatively low cost of approximately $ 5.50 per assay [37], that the inclusion of KREC detection in the TREC assay barely increases the costs, and that SCID and agammaglobulinemia have a combined estimated incidence of 1:30,000-1:50,000 births, a single assay capable of screening for both conditions should further improve the cost-effectiveness of the NBS for PID. The importance of introducing PID in NBS programs has been underlined by the guidelines very recently proposed by Borte et al. [66].
Quantification of TRECs and KRECs for therapy monitoring of primary and acquired immunodeficiencies
Patients with SCID have a very short life-expectancy if they are not promptly treated with HLA-identical or HLA-haploidentical HSCT [67, 68], which frequently results into a durable engraftment of all hematopoietic cell lineages that leads to a restoration of immunological functions in the absence of GVHD [68, 69]. Therefore, the success of HSCT mainly depends on the rate of cellular immune reconstitution [70–75]. However, while innate immunity shows a full phenotypic and functional recovery within a month from transplantation [76], the recovery of T cells can be significantly delayed, even in comparison to that of B cells, which can occur within 6–9 months (although a fully functional reconstitution encompassing the synthesis of all Ig isotypes may require up to 2 years) [76–80]. Therefore, due to the impairment of both T- and B-cell functions, HSCT recipients are more prone to infections and relapse of malignancies [81, 82], and the risk of developing these complications notably correlates with the recovery of CD4+ T cells [83]. Because it is known that, in these patients, the appearance of TRECs is the most predictive indicator for long-term T-cell reconstitution [84], a frequent monitoring of the T-cell immunity and TREC number after HSCT can help identify those patients who will eventually fail to be properly reconstituted, thus requiring additional therapies that could be more timely initiated. The use of the TREC assay may be also relevant to verify the outcome of unconditioned transplantations with matched sibling and family donors. In these cases, which are highly successful in terms of survival outcome, the assay may be informative in detecting a long-term thymopoiesis, or to establish whether the T-cell reconstitution is due to an engraftment of mature T cells that will ultimately be exhausted, thus leading to a long-term T-cell deficiency [83]. Indeed, a low TREC number has been found after unconditioned procedures, indicating the occurrence of only a limited prethymic progenitor-cell engraftment. Therefore, in these transplantations, the long term T-cell immunity is likely to be sustained by a pool of mature T cells [85]. Finally, the progressive decline of thymopoiesis observed after HSCT has been attributed to a number of factors. These include: a defective thymic microenvironment, which is derived from pre-existing alterations or GVHD-induced damages; the lack of an adequate reservoir of healthy donor stem cells (associated with the lack of conditioning); an insufficient HSC dose; or the recipient’s age [83, 86, 87].
The long-term (functional) immune recovery was particularly difficult to assess in Adenosine deaminase (ADA)-SCID patients. Treatments of these patients have included HSCT from an HLA-identical sibling donor without conditioning regimen, when available [88], enzyme replacement therapy [89], transplantation with unrelated donor cells [88], and gene therapy [90, 91]. Using the TREC/KREC assay, we conducted a detailed evaluation of T- and B-cell reconstitution in patients with broadly overlapping immunologic parameters, treated with HSCT or with polyethylene glycol-conjugated (PEG)-ADA. We found that the TREC level rose in both groups, but then quickly declined and persisted at low levels in the PEG-ADA group. The B-cell generation, studied both by B-cell subset phenotyping and KREC quantification, was more often impaired in the PEG-ADA group, and homeostatic proliferation could only partly compensate the decreased BM output [27].
TRECs/KRECs were also measured in patients with other PID (SCID T-B-NK+, SCID T-B-NK-, SCID T-B+NK+, SCID T-B+NK-, X-linked hyper IgM, Wiskott-Aldrich syndrome and familial hemophagocytic lymphohistiocytosis) who underwent HSCT and were followed up for a period ranging from 12 to 79 months. These children were heterogeneous with respect to sex, immunodeficiency type, graft donor, age of the donors and recipients of HSCT, type of conditioning, and occurrence and grade of GVHD. We found that the post-transplantation increase of TRECs and KRECs could be either strictly associated or independent of each other, and it was followed by the normalization of the T-cell repertoire and Ig production. Some patients showed a sharp, but transitory increase in new lymphocyte output which declined later on; in other patients, the TREC and KREC number remained very low for the entire period of surveillance [26].
An early output of B and T lymphocytes from the production and maturation sites, which is indicative of successful clinical outcome, was demonstrated, using a similar approach, also in transplanted SCID patients with a deficient recombination-activating gene 2 [92].
The TREC assay was also extensively used to evaluate the immune reconstitution in HIV-infected patients treated with antiviral therapy [6, 93–96]. Common knowledge is that thymic immune reconstitution of HIV-infected patients is more successful in children than in adults, suggesting that increased thymic output could play, at least in the formers, a predominant role in immune recovery [97]. TREC number increases in both virological responder and non-responder children, indicating that the persistence of viremia during therapy does not impair the increase in thymic function and the subsequent output of naive cells [98]. In adult patients with HIV-related lymphoma highly responder to antiretroviral therapy, the analysis of the kinetics and the extent of T-cell reconstitution before and after HSCT demonstrated that the very low level of TRECs before transplantation significantly increased following treatment [99], due to an extent of immune recovery close to that observed in transplanted HIV-negative patients with lymphoma [100]. Similarly, TREC monitoring in HIV-infected patients, long-term treated with low-doses of recombinant human growth hormone therapy, showed a recovery of thymopoiesis, as confirmed also by thymic index, density and area quantification [101]. Only few data are available on the number of KRECs in treated HIV-infected patients. One year of therapy did not modify the KREC number, while the long-lasting treatment (6 years) resulted in a significant decrease in new B-cell release from the BM [51]. However, due to the scarcity of available data, the usefulness of KREC quantification in these patients remains to be firmly established.
Limitations of the use TRECs and KRECs as immunological markers of immunodeficiency
Because TRECs and KRECs are not produced if maturation of T cells and B cells ceases at early steps, they are diluted out after cell division, they can persist in old thymic emigrant cells, and they disappear after cell death, caution is warranted in interpreting their number in the clinical setting. Therefore, even though expressing the amount of TRECs or KRECs per ml of blood overcomes the issue of peripheral dilution [24, 102], this measurement alone cannot still be considered a direct clinical marker of immune disease. Indeed, TRECs can be decreased in subjects that are not immunodeficient, such as premature babies and Down syndrome patients [103, 104]. Therefore, it must be also emphasized that TREC/KREC determination is only the first-tier assay, that must be followed by appropriate second-tier assays defining the disease (if any) that results in the low TREC/KREC values.
Conclusions
The increasing laboratory and clinical evidences reported in this review, which extends and completes the recent one by van Zelm et al. [8], indicate that the quantification of TRECs and KRECs can be very informative in the management of patients with primary and acquired immunodeficiencies. It appeared that it is technically feasible to introduce the TREC/KREC assay into routine laboratory practice both for NBS and for a more critical monitoring of the rate of T- and B-cell immune reconstitution following HSCT and antiretroviral therapy.
Abbreviations
- ADA:
-
Adenosine deaminase
- BcR:
-
B-cell receptor
- BM:
-
bone marrow
- BTK:
-
Bruton agammaglobulinemia tyrosine kinase
- CJ:
-
Coding joint
- Ct:
-
Cycle threshold
- CVID:
-
common variable immunodeficiency
- D:
-
Diversity
- FOXP3:
-
Forkhead box protein 3
- GVHD:
-
Graft-versus-host disease
- HSCT:
-
Human stem-cell transplantation
- IGK:
-
Ig kappa
- IGKC:
-
IGK constant gene
- IGKDEL:
-
IGK deleting element or like
- IGKJ:
-
IGK joining genes
- J:
-
Joining
- KRECs:
-
Kappa-deleting recombination excision circles
- NBS:
-
Newborn screening
- NK:
-
Natural killer
- PBMC:
-
Peripheral blood mononuclear cells
- PEG:
-
Polyethylene glycol
- PID:
-
Primary immunodeficiencies
- RSS:
-
Recombination signal sequences
- SCID:
-
Severe combined immunodeficiency
- SJ:
-
Signal joint
- TR:
-
T-cell receptor
- TRA:
-
TR alpha
- TRAC:
-
TRA constant gene
- TRECs:
-
T-cell receptor excision circles
- V:
-
Variable
- XLA:
-
X-linked agammaglobulinemia
- ZAP70:
-
zeta-chain (TCR) associated protein kinase 70kDa.
References
Nossal GJ: Negative selection of lymphocytes. Cell. 1994, 76: 229-239. 10.1016/0092-8674(94)90331-X. Review
Fry AM, Jones LA, Kruisbeek AM, Matis LA: Thymic requirement for clonal deletion during T cell development. Science. 1989, 246: 1044-1046. 10.1126/science.2511630.
Hodes RJ, Sharrow SO, Solomon A: Failure of T cell receptor V beta negative selection in an athymic environment. Science. 1989, 246: 1041-1044. 10.1126/science.2587987.
Dik WA, Pike-Overzet K, Weerkamp F, de Ridder D, de Haas EF, Baert MR, van der Spek P, Koster EE, Reinders MJ, van Dongen JJ, Langerak AW, Staal FJ: New insights on human T cell development by quantitative T cell receptor gene rearrangement studies and gene expression profiling. J Exp Med. 2005, 201: 1715-1723. 10.1084/jem.20042524.
Ghia P, Ten Boekel E, Rolink AG, Melchers F: B-cell development: a comparison between mouse and man. Immunol Today. 1998, 19: 480-485. 10.1016/S0167-5699(98)01330-9. Review
Douek DC, McFarland RD, Keiser PH, Gage EA, Massey JM, Haynes BF, Polis MA, Haase AT, Feinberg MB, Sullivan JL, Jamieson BD, Zack JA, Picker LJ, Koup RA: Changes in thymic function with age and during the treatment of HIV infection. Nature. 1998, 396: 690-695. 10.1038/25374.
van Zelm MC, Szczepanski T, van der Burg M, van Dongen JJ: Replication history of B lymphocytes reveals homeostatic proliferation and extensive antigen-induced B cell expansion. J Exp Med. 2007, 204: 645-655. 10.1084/jem.20060964.
van Zelm MC, van der Burg M, Langerak AW, van Dongen JJ: PID comes full circle: applications of V(D)J recombination excision circles in research, diagnostics and newborn screening of primary immunodeficiency disorders. Front Immunol. 2011, 2: 12-
Siminovitch KA, Bakhshi A, Goldman P, Korsmeyer SJ: A uniform deleting element mediates the loss of kappa genes in human B cells. Nature. 1985, 316: 260-262. 10.1038/316260a0.
Beishuizen A, de Bruijn MA, Pongers-Willemse MJ, Verhoeven MA, van Wering ER, Hählen K, Breit TM, de Bruin-Versteeg S, Hooijkaas H, van Dongen JJ: Heterogeneity in junctional regions of immunoglobulin kappa deleting element rearrangements in B cell leukemias: a new molecular target for detection of minimal residual disease. Leukemia. 1997, 11: 2200-2207. 10.1038/sj.leu.2400904.
Verschuren MC, Wolvers-Tettero IL, Breit TM, Noordzij J, van Wering ER, van Dongen JJ: Preferential rearrangements of the T cell receptor-delta-deleting elements in human T cells. J Immunol. 1997, 158: 1208-1216.
Hazenberg MD, Otto SA, Cohen Stuart JW, Verschuren MC, Borleffs JC, Boucher CA, Coutinho RA, Lange JM, Rinke de Wit TF, Tsegaye A, van Dongen JJ, Hamann D, de Boer RJ, Miedema F: Increased cell division but not thymic dysfunction rapidly affects the T-cell receptor excision circle content of the naive T cell population in HIV-1 infection. Nat Med. 2000, 6: 1036-1042. 10.1038/79549.
Hazenberg MD, Verschuren MC, Hamann D, Miedema F, van Dongen JJ: T cell receptor excision circles as markers for recent thymic emigrants: basic aspects, technical approach, and guidelines for interpretation. J Mol Med. 2001, 79: 631-640. 10.1007/s001090100271. Review
Sodora DL, Douek DC, Silvestri G, Montgomery L, Rosenzweig M, Igarashi T, Bernacky B, Johnson RP, Feinberg MB, Martin MA, Koup RA: Quantification of thymic function by measuring T cell receptor excision circles within peripheral blood and lymphoid tissues in monkeys. Eur J Immunol. 2000, 30: 1145-1153. 10.1002/(SICI)1521-4141(200004)30:4<1145::AID-IMMU1145>3.0.CO;2-7.
van der Weerd K, Dik WA, Schrijver B, Bogers AJ, Maat AP, van Nederveen FH, van Hagen PM, van Dongen JJ, Langerak AW, Staal FJ: Combined TCRG and TCRA TREC analysis reveals increased peripheral T-lymphocyte but constant intra-thymic proliferative history upon ageing. Mol Immunol. 2013, 53: 302-312. 10.1016/j.molimm.2012.08.019.
Zhang L, Lewin SR, Markowitz M, Lin HH, Skulsky E, Karanicolas R, He Y, Jin X, Tuttleton S, Vesanen M, Spiegel H, Kost R, van Lunzen J, Stellbrink HJ, Wolinsky S, Borkowsky W, Palumbo P, Kostrikis LG, Ho DD: Measuring recent thymic emigrants in blood of normal and HIV-1-infected individuals before and after effective therapy. J Exp Med. 1999, 190: 725-732. 10.1084/jem.190.5.725.
Zubakov D, Liu F, van Zelm MC, Vermeulen J, Oostra BA, van Duijn CM, Driessen GJ, van Dongen JJ, Kayser M, Langerak AW: Estimating human age from T-cell DNA rearrangements. Curr Biol. 2010, 20: R970-R971. 10.1016/j.cub.2010.10.022.
Ponchel F, Toomes C, Bransfield K, Leong FT, Douglas SH, Field SL, Bell SM, Combaret V, Puisieux A, Mighell AJ, Robinson PA, Inglehearn CF, Isaacs JD, Markham AF: Real-time PCR based on SYBR-green I fluorescence: an alternative to the TaqMan assay for a relative quantification of gene rearrangements, gene amplifications and micro gene deletions. BMC Biotechnol. 2003, 3: 18-10.1186/1472-6750-3-18.
Nobile M, Correa R, Borghans JA, D'Agostino C, Schneider P, De Boer RJ, Pantaleo G, Swiss HIV Cohort Study: De novo T-cell generation in patients at different ages and stages of HIV-1 disease. Blood. 2004, 104: 470-477. 10.1182/blood-2003-12-4265.
Hug A, Korporal M, Schröder I, Haas J, Glatz K, Storch-Hagenlocher B, Wildemann B: Thymic export function and T cell homeostasis in patients with relapsing remitting multiple sclerosis. J Immunol. 2003, 171: 432-437.
Hazenberg MD, Otto SA, de Pauw ES, Roelofs H, Fibbe WE, Hamann D, Miedema F: T-cell receptor excision circle and T-cell dynamics after allogeneic stem cell transplantation are related to clinical events. Blood. 2002, 99: 3449-3453. 10.1182/blood.V99.9.3449.
Bains I, Thiébaut R, Yates AJ, Callard R: Quantifying thymic export: combining models of naive T cell proliferation and TCR excision circle dynamics gives an explicit measure of thymic output. J Immunol. 2009, 183: 4329-4336. 10.4049/jimmunol.0900743.
Krenger W, Schmidlin H, Cavadini G, Holländer GA: On the relevance of TCR rearrangement circles as molecular markers for thymic output during experimental graft-versus-host disease. J Immunol. 2004, 172: 7359-7567.
Ribeiro RM, Perelson AS: Determining thymic output quantitatively: using models to interpret experimental T-cell receptor excision circle (TREC) data. Immunol Rev. 2007, 216: 21-34. Review
Fronkova E, Muzikova K, Mejstrikova E, Kovac M, Formankova R, Sedlacek P, Hrusak O, Stary J, Trka J: B-cell reconstitution after allogeneic SCT impairs minimal residual disease monitoring in children with ALL. Bone Marrow Transplant. 2008, 42: 187-196. 10.1038/bmt.2008.122.
Sottini A, Ghidini C, Zanotti C, Chiarini M, Caimi L, Lanfranchi A, Moratto D, Porta F, Imberti L: Simultaneous quantification of recent thymic T-cell and bone marrow B-cell emigrants in patients with primary immunodeficiency undergone to stem cell transplantation. Clin Immunol. 2010, 136: 217-227. 10.1016/j.clim.2010.04.005.
Serana F, Sottini A, Chiarini M, Zanotti C, Ghidini C, Lanfranchi A, Notarangelo LD, Caimi L, Imberti L: The different extent of B and T cell immune reconstitution after hematopoietic stem cell transplantation and enzyme replacement therapies in SCID patients with adenosine deaminase deficiency. J Immunol. 2010, 185: 7713-7722. 10.4049/jimmunol.1001770.
Notarangelo LD: Primary immunodeficiencies. J Allergy Clin Immunol. 2010, 125 (2 Suppl 2): S182-S194.
Buckley RH: Molecular defects in human severe combined immunodeficiency and approaches to immune reconstitution. Annu Rev Immunol. 2004, 22: 625-655. 10.1146/annurev.immunol.22.012703.104614. Review
Fischer A, Le Deist F, Hacein-Bey-Abina S, André-Schmutz I, Basile Gde S, de Villartay JP, Cavazzana-Calvo M: Severe combined immunodeficiency. A model disease for molecular immunology and therapy. Immunol Rev. 2005, 203: 98-109. 10.1111/j.0105-2896.2005.00223.x. Review
Roifman CM, Somech R, Kavadas F, Pires L, Nahum A, Dalal I, Grunebaum E: Defining combined immunodeficiency. J Allergy Clin Immunol. 2012, 130: 177-183. 10.1016/j.jaci.2012.04.029.
Gerstel-Thompson JL, Wilkey JF, Baptiste JC, Navas JS, Pai SY, Pass KA, Eaton RB, Comeau AM: High-throughput multiplexed T-cell-receptor excision circle quantitative PCR assay with internal controls for detection of severe combined immunodeficiency in population-based newborn screening. Clin Chem. 2010, 56: 1466-1474. 10.1373/clinchem.2010.144915.
Morinishi Y, Imai K, Nakagawa N, Sato H, Horiuchi K, Ohtsuka Y, Kaneda Y, Taga T, Hisakawa H, Miyaji R, Endo M, Oh-Ishi T, Kamachi Y, Akahane K, Kobayashi C, Tsuchida M, Morio T, Sasahara Y, Kumaki S, Ishigaki K, Yoshida M, Urabe T, Kobayashi N, Okimoto Y, Reichenbach J, Hashii Y, Tsuji Y, Kogawa K, Yamaguchi S, Kanegane H, Miyawaki T, Yamada M, Ariga T, Nonoyama S: Identification of severe combined immunodeficiency by T-cell receptor excision circles quantification using neonatal Guthrie cards. J Pediatr. 2009, 155: 829-833. 10.1016/j.jpeds.2009.05.026.
Borte S, von Döbeln U, Fasth A, Wang N, Janzi M, Winiarski J, Sack U, Pan-Hammarström Q, Borte M, Hammarström L: Neonatal screening for severe primary immunodeficiency diseases using high-throughput triplex real-time PCR. Blood. 2012, 119: 2552-2555. 10.1182/blood-2011-08-371021.
Chan K, Puck JM: Development of population-based newborn screening for severe combined immunodeficiency. J Allergy Clin Immunol. 2005, 115: 391-398. 10.1016/j.jaci.2004.10.012.
Hale JE, Bonilla FA, Pai SY, Gerstel-Thompson JL, Notarangelo LD, Eaton RB, Comeau AM: Identification of an infant with severe combined immunodeficiency by newborn screening. J Allergy Clin Immunol. 2010, 126: 1073-1074. 10.1016/j.jaci.2010.08.043.
Routes JM, Grossman WJ, Verbsky J, Laessig RH, Hoffman GL, Brokopp CD, Baker MW: Statewide newborn screening for severe T-cell lymphopenia. JAMA. 2009, 302: 2465-2470. 10.1001/jama.2009.1806.
Lima K, Abrahamsen TG, Foelling I, Natvig S, Ryder LP, Olaussen RW: Low thymic output in the 22q11.2 Deletion syndrome measured by CCR9+CD45RA+ T cell counts and T cell receptor rearrangement excision circles. Clin Exp Immunol. 2010, 161: 98-107.
van der Burg M, Pac M, Berkowska MA, Goryluk-Kozakiewicz B, Wakulinska A, Dembowska-Baginska B, Gregorek H, Barendregt BH, Krajewska-Walasek M, Bernatowska E, van Dongen JJ, Chrzanowska KH, Langerak AW: Loss of juxtaposition of RAG-induced immunoglobulin DNA ends is implicated in the precursor B-cell differentiation defect in NBS patients. Blood. 2010, 115: 4770-4777. 10.1182/blood-2009-10-250514.
Nakagawa N, Imai K, Kanegane H, Sato H, Yamada M, Kondoh K, Okada S, Kobayashi M, Agematsu K, Takada H, Mitsuiki N, Oshima K, Ohara O, Suri D, Rawat A, Singh S, Pan-Hammarström Q, Hammarström L, Reichenbach J, Seger R, Ariga T, Hara T, Miyawaki T, Nonoyama S: Quantification of κ-deleting recombination excision circles in Guthrie cards for the identification of early B-cell maturation defects. J Allergy Clin Immunol. 2011, 128: 223-225.e2. 10.1016/j.jaci.2011.01.052.
Serana F, Airò P, Chiarini M, Zanotti C, Scarsi M, Frassi M, Lougaris V, Plebani A, Caimi L, Imberti L: Thymic and bone marrow output in patients with common variable immunodeficiency. J Clin Immunol. 2011, 31: 540-549. 10.1007/s10875-011-9526-6.
Kamae C, Nakagawa N, Sato H, Honma K, Mitsuiki N, Ohara O, Kanegane H, Pasic S, Pan-Hammarström Q, van Zelm MC, Morio T, Imai K, Nonoyama S: Common variable immunodeficiency classification by quantifying T-cell receptor and immunoglobulin κ-deleting recombination excision circles. J Allergy Clin Immunol. in press
Amariglio N, Lev A, Simon A, Rosenthal E, Spirer Z, Efrati O, Broides A, Rechavi G, Somech R: Molecular assessment of thymus capabilities in the evaluation of T-cell immunodeficiency. Pediatr Res. 2010, 67: 211-216. 10.1203/PDR.0b013e3181c6e554.
Warnatz K, Wehr C, Dräger R, Schmidt S, Eibel H, Schlesier M, Peter HH: Expansion of CD19(hi)CD21(lo/neg) B cells in common variable immunodeficiency (CVID) patients with autoimmune cytopenia. Immunobiology. 2002, 206: 502-513. 10.1078/0171-2985-00198.
Guazzi V, Aiuti F, Mezzaroma I, Mazzetta F, Andolfi G, Mortellaro A, Pierdominici M, Fantini R, Marziali M, Aiuti A: Assessment of thymic output in common variable immunodeficiency patients by evaluation of T cell receptor excision circles. Clin Exp Immunol. 2002, 129: 346-353. 10.1046/j.1365-2249.2002.01893.x.
Moratto D, Gulino AV, Fontana S, Mori L, Pirovano S, Soresina A, Meini A, Imberti L, Notarangelo LD, Plebani A, Badolato R: Combined decrease of defined B and T cell subsets in a group of common variable immunodeficiency patients. Clin Immunol. 2006, 121: 203-214. 10.1016/j.clim.2006.07.003.
Conley ME, Rohrer J, Minegishi Y: X-linked agammaglobulinemia. Clin Rev Allergy Immunol. 2000, 19: 183-204. 10.1385/CRIAI:19:2:183. Review
Kanegane H, Futatani T, Wang Y, Nomura K, Shinozaki K, Matsukura H, Kubota T, Tsukada S, Miyawaki T: Clinical and mutational characteristics of X-linked agammaglobulinemia and its carrier identified by flow cytometric assessment combined with genetic analysis. J Allergy Clin Immunol. 2001, 108: 1012-1020. 10.1067/mai.2001.120133.
Hazenberg MD, Borghans JA, de Boer RJ, Miedema F: Thymic output: a bad TREC record. Nat Immunol. 2003, 4: 97-99. 10.1038/ni0203-97. Review
Hatzakis A, Touloumi G, Karanicolas R, Karafoulidou A, Mandalaki T, Anastassopoulou C, Zhang L, Goedert JJ, Ho DD, Kostrikis LG: Effect of recent thymic emigrants on progression of HIV-1 disease. Lancet. 2000, 355: 599-604. 10.1016/S0140-6736(99)10311-8.
Quiros-Roldan E, Serana F, Chiarini M, Zanotti C, Sottini A, Gotti D, Torti C, Caimi L, Imberti L: Effects of combined antiretroviral therapy on B- and T-cell release from production sites in long-term treated HIV-1+ patients. J Transl Med. 2012, 10: 94-10.1186/1479-5876-10-94.
Buckley RH, Schiff SE, Schiff RI, Markert L, Williams LW, Roberts JL, Myers LA, Ward FE: Hematopoietic stem-cell transplantation for the treatment of severe combined immunodeficiency. N Engl J Med. 1999, 340: 508-516. 10.1056/NEJM199902183400703.
Kane L, Gennery AR, Crooks BN, Flood TJ, Abinun M, Cant AJ: Neonatal bone marrow transplantation for severe combined immunodeficiency. Arch Dis Child Fetal Neonatal Ed. 2001, 85: F110-F113. 10.1136/fn.85.2.F110.
Myers LA, Patel DD, Puck JM, Buckley RH: Hematopoietic stem cell transplantation for severe combined immunodeficiency in the neonatal period leads to superior thymic output and improved survival. Blood. 2002, 99: 872-878. 10.1182/blood.V99.3.872.
Buckley RH: Transplantation of hematopoietic stem cells in human severe combined immunodeficiency: longterm outcomes. Immunol Res. 2011, 49: 25-43. 10.1007/s12026-010-8191-9. Review
Hershfield MS, Buckley RH, Greenberg ML, Melton AL, Schiff R, Hatem C, Kurtzberg J, Markert ML, Kobayashi RH, Kobayashi AL, Abuchowski A: Treatment of adenosine deaminase deficiency with polyethylene glycol-modified adenosine deaminase. N Engl J Med. 1987, 316: 589-596. 10.1056/NEJM198703053161005.
Aiuti A, Cattaneo F, Galimberti S, Benninghoff U, Cassani B, Callegaro L, Scaramuzza S, Andolfi G, Mirolo M, Brigida I, Tabucchi A, Carlucci F, Eibl M, Aker M, Slavin S, Al-Mousa H, Al Ghonaium A, Ferster A, Duppenthaler A, Notarangelo L, Wintergerst U, Buckley RH, Bregni M, Marktel S, Valsecchi MG, Rossi P, Ciceri F, Miniero R, Bordignon C, Roncarolo : Gene therapy for immunodeficiency due to adenosine deaminase deficiency. N Engl J Med. 2009, 360: 447-458. 10.1056/NEJMoa0805817.
Hacein-Bey-Abina S, Hauer J, Lim A, Picard C, Wang GP, Berry CC, Martinache C, Rieux-Laucat F, Latour S, Belohradsky BH, Leiva L, Sorensen R, Debré M, Casanova JL, Blanche S, Durandy A, Bushman FD, Fischer A, Cavazzana-Calvo M: Efficacy of gene therapy for X-linked severe combined immunodeficiency. N Engl J Med. 2010, 363: 355-364. 10.1056/NEJMoa1000164.
Gaspar HB, Cooray S, Gilmour KC, Parsley KL, Adams S, Howe SJ, Al Ghonaium A, Bayford J, Brown L, Davies EG, Kinnon C, Thrasher AJ: Long-term persistence of a polyclonal T cell repertoire after gene therapy for X-linked severe combined immunodeficiency. Sci Transl Med. 2011, 3: 97ra79-10.1126/scitranslmed.3002715.
Brown L, Xu-Bayford J, Allwood Z, Slatter M, Cant A, Davies EG, Veys P, Gennery AR, Gaspar HB: Neonatal diagnosis of severe combined immunodeficiency leads to significantly improved survival outcome: the case for newborn screening. Blood. 2011, 117: 3243-3246. 10.1182/blood-2010-08-300384.
Puck JM, SCID Newborn Screening Working Group: Population-based newborn screening for severe combined immunodeficiency: steps toward implementation. J Allergy Clin Immunol. 2007, 120: 760-768. 10.1016/j.jaci.2007.08.043.
Wilson JM, Jungner YG: Principles and practice of mass screening for disease. Bol Oficina Sanit Panam. 1968, 65: 281-393. Spanish
Baker MW, Grossman WJ, Laessig RH, Hoffman GL, Brokopp CD, Kurtycz DF, Cogley MF, Litsheim TJ, Katcher ML, Routes JM: Development of a routine newborn screening protocol for severe combined immunodeficiency. J Allergy Clin Immunol. 2009, 124: 522-527. 10.1016/j.jaci.2009.04.007.
Comeau AM, Hale JE, Pai SY, Bonilla FA, Notarangelo LD, Pasternack MS, Meissner HC, Cooper ER, DeMaria A, Sahai I, Eaton RB: Guidelines for implementation of population-based newborn screening for severe combined immunodeficiency. J Inherit Metab Dis. 2010, 33 (Suppl 2): S273-S281.
Buckley RH: The long quest for neonatal screening for severe combined immunodeficiency. J Allergy Clin Immunol. 2012, 129: 597-604. 10.1016/j.jaci.2011.12.964. Review
Borte S, von Döbeln U, Hammarström L: Guidelines for newborn screening of primary immunodeficiency diseases. Curr Opin Hematol. 2013, 20: 48-54. 10.1097/MOH.0b013e32835a9130.
Kenny AB, Hitzig WH: Bone marrow transplantation for severe combined immunodeficiency disease. Reported from 1968 to 1977. Eur J Paediatr. 1979, 131: 155-177. 10.1007/BF00538940.
Fischer A, Landais P, Friedrich W, Morgan G, Gerritsen B, Fasth A, Porta F, Griscelli C, Goldman SF, Levinsky R, Vossen J: European experience of bone- marrow transplantation for severe combined immunodeficiency. Lancet. 1990, 336: 850-854. 10.1016/0140-6736(90)92348-L.
Fischer A, Durandy A, de Villartay JP, Vilmer E, Le Deist F, Gerota I, Griscelli C: HLA-haploidentical bone marrow transplantation for severe combined immunodeficiency using E rosette fractionation and cyclosporine. Blood. 1986, 67: 444-449.
Guillaume T, Rubinstein DB, Symann M: Immune reconstitution and immunotherapy after autologous hematopoietic stem cell transplantation. Blood. 1998, 92: 1471-1490. Review
Koehl U, Bochennek K, Zimmermann SY, Lehrnbecher T, Sorensen J, Esser R, Andreas C, Kramm C, Grüttner HP, Falkenberg E, Orth A, Bader P, Schwabe D, Klingebiel T: Immune recovery in children undergoing allogeneic stem cell transplantation: absolute CD8+CD3+ count reconstitution is associated with survival. Bone Marrow Transplant. 2007, 39: 269-278. 10.1038/sj.bmt.1705584.
Passweg J, Baldomero H, Chapuis B, Leibundgut K, Schanz U, Gratwohl A, Swiss Transplant Working Group Blood and Marrow Transplantation Board: Haematopoietic stem cell transplantation in Switzerland. Report from the Swiss Transplant Working Group Blood and Marrow Transplantation (STABMT) Registry 1997–2003. Swiss Med Wkly. 2006, 136: 50-58.
Klingebiel T, Handgretinger R, Lang P, Bader P, Niethammer D: Haploidentical transplantation for acute lymphoblastic leukemia in childhood. Blood Rev. 2004, 18: 181-192. 10.1016/S0268-960X(03)00063-8. Review
Devine SM, Adkins DR, Khoury H, Brown RA, Devine SM, Adkins DR, Khoury H, Brown RA, Vij R, Blum W, DiPersio JF: Recent advances in allogeneic hematopoietic stem-cell transplantation. J Lab Clin Med. 2003, 141: 7-32. 10.1067/mlc.2003.5. Review
Schwinger W, Weber-Mzell D, Zois B, Rojacher T, Benesch M, Lackner H, Dornbusch HJ, Sovinz P, Moser A, Lanzer G, Schauenstein K, Ofner P, Handgretinger R, Urban C: Immune reconstitution after purified autologous and allogeneic blood stem cell transplantation compared with unmanipulated bone marrow transplantation in children. Brit J Haematol. 2006, 135: 76-84. 10.1111/j.1365-2141.2006.06244.x.
Isaacs JD, Thiel A: Stem cell transplantation for autoimmune disorders. Immune reconstitution. Best Pract Res Clin Haematol. 2004, 17: 345-358. 10.1016/j.beha.2004.04.008.
van Leeuwen JE, van Tol MJ, Joosten AM, Schellekens PT, van den Bergh RL, Waaijer JL, Oudeman-Gruber NJ, van der Weijden–Ragas CP, Roos MT, Gerritsen EJ, van den Berg H, Harraldsson A, Meera Khan P, Vossen JM: Relationship between patterns of engraftment in peripheral blood and immune reconstitution after allogeneic bone marrow transplantation for (severe) combined immunodeficiency. Blood. 1994, 84: 3936-3947.
Lau YL, Kwong YL, Lee AC, Chiu EK, Ha SY, Chan CF, Chan V, Chan TK: Mixed chimerism following bone marrow transplantation for severe combined immunodeficiency: a study by DNA fingerprinting and simultaneous immunophenotyping and fluorescence in situ hybridisation. Bone Marrow Transplant. 1995, 15: 971-976.
Friedrich W, Goldmann SF, Ebell W, Blutters–Sawatzki R, Gaedecke G, Raghavachar A, Peter HH, Belohradsky B, Kreth W, Kubanek B, Kleihauer E: Severe combined immunodeficiency: treatment by bone marrow transplantation in 15 infants using HLA- haploidentical donors. Eur J Pediatr. 1985, 144: 125-130. 10.1007/BF00451897.
Buckley RH, Schiff SE, Sampson HA, Schiff RI, Markert ML, Knutsen AP, Hershfield MS, Huang AT, Mickey GH, Ward FE: Development of immunity in human primary T cell deficiency following haploidentical bone marrow stem cell transplantation. J Immunol. 1986, 136: 2398-2407.
Wijnaendts L, Le Deist F, Griscelli C, Fischer A: Development of immunologic functions after bone marrow transplantation in 33 patients with severe combined immunodeficiency. Blood. 1989, 74: 2212-2219.
Kook H, Goldman F, Padley D, Giller R, Rumelhart S, Holida M, Lee N, Peters C, Comito M, Huling D, Trigg M: Reconstitution of the immune system after unrelated or partially matched T- cell depleted bone marrow transplantation in children: immunophenotypic analysis and factors affecting the speed of recovery. Blood. 1996, 88: 1089-1097.
Neven B, Leroy S, Decaluwe H, Le Deist F, Picard C, Moshous D, Mahlaoui N, Debré M, Casanova JL, Dal Cortivo L, Madec Y, Hacein-Bey-Abina S, de Saint Basile G, de Villartay JP, Blanche S, Cavazzana-Calvo M, Fischer A: Long-term outcome after hematopoietic stem cell transplantation of a single-center cohort of 90 patients with severe combined immunodeficiency. Blood. 2009, 113: 4114-4124. 10.1182/blood-2008-09-177923.
Borghans JA, Bredius RG, Hazenberg MD, Roelofs H, Jol-van der Zijde EC, Heidt J, Otto SA, Kuijpers TW, Fibbe WE, Vossen JM, Miedema F, van Tol MJ: Early determinants of long-term T-cell reconstitution after hematopoietic stem cell transplantation for severe combined immunodeficiency. Blood. 2006, 108: 763-769. 10.1182/blood-2006-01-009241.
Hassan A, Booth C, Brightwell A, Allwood Z, Veys P, Rao K, Hönig M, Friedrich W, Gennery A, Slatter M, Bredius R, Finocchi A, Cancrini C, Aiuti A, Porta F, Lanfranchi A, Ridella M, Steward C, Filipovich A, Marsh R, Bordon V, Al-Muhsen S, Al-Mousa H, Alsum Z, Al-Dhekri H, Al Ghonaium A, Speckmann C, Fischer A, Mahlaoui N, Nichols KE, Grunebaum E, Al Zahrani D, Roifman CM, Boelens J, Davies EG, Cavazzana-Calvo M, Notarangelo L, Gaspar HB, Inborn Errors Working Party of the European Group for Blood and Marrow Transplantation and European Society for Immunodeficiency: Outcome of hematopoietic stem cell transplantation for adenosine deaminase-deficient severe combined immunodeficiency. Blood. 2012, 120: 3615-3624. 10.1182/blood-2011-12-396879.
Cavazzana-Calvo M, Carlier F, Le Deist F, Morillon E, Taupin P, Gautier D, Radford-Weiss I, Caillat-Zucman S, Neven B, Blanche S, Cheynier R, Fischer A, Hacein-Bey-Abina S: Long-term T-cell reconstitution after hematopoietic stem-cell transplantation in primary T-cell-immunodeficient patients is associated with myeloid chimerism and possibly the primary disease phenotype. Blood. 2007, 109: 4575-4581. 10.1182/blood-2006-07-029090.
Dvorak CC, Cowan MJ: Hematopoietic stem cell transplantation for primary immunodeficiency disease. Bone Marrow Transplant. 2008, 41: 119-126. 10.1038/sj.bmt.1705890. Review
Gaspar HB, Aiuti A, Porta F, Candotti F, Hershfield MS, Notarangelo LD: How I treat ADA deficiency. Blood. 2009, 114: 3524-3532. 10.1182/blood-2009-06-189209. Review
Hershfield MS: Adenosine deaminase deficiency: clinical expression, molecular basis, and therapy. Semin Hematol. 1998, 35: 291-298. Review
Aiuti A, Brigida I, Ferrua F, Cappelli B, Chiesa R, Marktel S, Roncarolo MG: Hematopoietic stem cell gene therapy for adenosine deaminase deficient-SCID. Immunol Res. 2009, 44: 150-159. 10.1007/s12026-009-8107-8.
Gaspar HB, Bjorkegren E, Parsley K, Gilmour KC, King D, Sinclair J, Zhang F, Giannakopoulos A, Adams S, Fairbanks LD, Gaspar J, Henderson L, Xu-Bayford JH, Davies EG, Veys PA, Kinnon C, Thrasher AJ: Successful reconstitution of immunity in ADA-SCID by stem cell gene therapy following cessation of PEG-ADA and use of mild preconditioning. Mol Ther. 2006, 14: 505-513. 10.1016/j.ymthe.2006.06.007.
Lev A, Simon AJ, Bareket M, Bielorai B, Hutt D, Amariglio N, Rechavi G, Somech R: The kinetics of early T and B cell immune recovery after bone marrow transplantation in RAG-2-deficient SCID patients. PLoS One. 2012, 7: e30494-10.1371/journal.pone.0030494.
Nobile M, Correa R, Borghans JA, D’Agostino C, Schneider P, De Boer RJ, Pantaleo G, Swiss HIV, Cohort Study: De novo T-cell generation in patients at different ages and stages of HIV-1 disease. Blood. 2004, 104: 470-477. 10.1182/blood-2003-12-4265.
Ometto L, De Forni D, Patiri F, Trouplin V, Mammano F, Giacomet V, Giaquinto C, Douek D, Koup R, De Rossi A: Immune reconstitution in HIV-1-infected children on antiretroviral therapy: role of thymic output and viral fitness. AIDS. 2002, 16: 839-849. 10.1097/00002030-200204120-00003.
De Rossi A, Walker AS, Klein N, De Forni D, King D, Gibb DM: Increased thymic output after initiation of antiretroviral therapy in human immunodeficiency virus type 1-infected children in the Paediatric European Network for Treatment of AIDS (PENTA) 5 Trial. J Infect Dis. 2002, 186: 312-320. 10.1086/341657.
Chavan S, Bennuri B, Kharbanda M, Chandrasekaran A, Bakshi S, Pahwa S: Evaluation of T cell receptor gene rearrangement excision circles after antiretroviral therapy in children infected with human immunodeficiency virus. J Infect Dis. 2001, 183: 1445-1454. 10.1086/320197.
Resino S, Seoane E, Pérez A, Ruiz-Mateos E, Leal M, Muñoz-Fernández MA: Different profiles of immune reconstitution in children and adults with HIV-infection after highly active antiretroviral therapy. BMC Infect Dis. 2006, 6: 112-10.1186/1471-2334-6-112.
Anselmi A, Vendrame D, Rampon O, Giaquinto C, Zanchetta M, De Rossi A: Immune reconstitution in human immunodeficiency virus type 1-infected children with different virological responses to anti-retroviral therapy. Clin Exp Immunol. 2007, 150: 442-450. 10.1111/j.1365-2249.2007.03526.x.
Benicchi T, Ghidini C, Re A, Cattaneo C, Casari S, Caimi L, Rossi G, Imberti L: T-cell immune reconstitution after hematopoietic stem cell transplantation for HIV-associated lymphoma. Transplantation. 2005, 80: 673-682. 10.1097/01.tp.0000168490.29862.b8.
Resino S, Pérez A, Seoane E, Serrano D, Berenguer J, Balsalobre P, Goméz-Chacon GF, Díez-Martin JL, Muñoz-Fernández MA: Short communication: Immune reconstitution after autologous peripheral blood stem cell transplantation in HIV-infected patients: might be better than expected?. AIDS Res Hum Retroviruses. 2007, 23: 543-548. 10.1089/aid.2006.0071.
Hansen BR, Kolte L, Haugaard SB, Dirksen C, Jensen FK, Ryder LP, Sørensen AL, Flyvbjerg A, Nielsen SD, Andersen O: Improved thymic index, density and output in HIV-infected patients following low-dose growth hormone therapy: a placebo controlled study. AIDS. 2009, 23: 2123-2131. 10.1097/QAD.0b013e3283303307.
Lorenzi AR, Patterson AM, Pratt A, Jefferson M, Chapman CE, Ponchel F, Isaacs JD: Determination of thymic function directly from peripheral blood: a validated modification to an established method. J Immunol Methods. 2008, 31: 185-194.
Baker MW, Laessig RH, Katcher ML, Routes JM, Grossman WJ, Verbsky J, Kurtycz DF, Brokopp CD: Implementing routine testing for severe combined immunodeficiency within Wisconsin's newborn screening program. Public Health Rep. 2010, 125 (Suppl 2): 88-95.
Ram G, Chinen J: Infections and immunodeficiency in Down syndrome. Clin Exp Immunol. 2011, 164: 9-16. 10.1111/j.1365-2249.2011.04335.x.
Acknowledgments
MC and CZ are supported by fellowships from Regione Lombardia-Piano Regionale Sangue and from Fondazione Rodella, Montichiari. The laboratory is supported by grants from Fondazione Berlucchi and Istituto Superiore di Sanità (n.40H2), Italy.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no conflicts of interest.
Authors’ contributions
FS discussed the outline and contributed to the drafting of the article, MC, CZ, AS, DB, AB assisted in drafting the manuscript and approved the final version; LC discussed the manuscript and approved the final version; and LI wrote the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Serana, F., Chiarini, M., Zanotti, C. et al. Use of V(D)J recombination excision circles to identify T- and B-cell defects and to monitor the treatment in primary and acquired immunodeficiencies. J Transl Med 11, 119 (2013). https://doi.org/10.1186/1479-5876-11-119
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1479-5876-11-119