Abstract
Background
Although most pregnancies after IVF result in normal healthy outcomes, an increased risk for a number of obstetric and neonatal complications, compared to naturally conceived pregnancies, has been reported. While there are many studies that compare pregnancies after assisted reproductive techniques with spontaneously conceived pregnancies, fewer data are available that evaluate the differences between IVF and ICSI-conceived pregnancies. The aim of our present study was, therefore, to compare obstetric and perinatal outcomes in pregnancies conceived after in vitro fertilization (IVF) versus intracytoplasmatic sperm injection (ICSI).
Methods
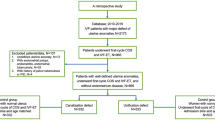
Three-hundred thirty four women who had become pregnant after an IVF or ICSI procedure resulted in a total of 530 children referred between 2003 und 2009 to the Department of Obstetrics and Gynecology of the Medical University of Vienna, a tertiary care center, and were included in this retrospective cohort study. We assessed maternal and fetal parameters in both groups (IVF and ICSI). The main study outcomes were preterm delivery, the need for neonatal intensive care, and congenital malformations. Moreover, we compared the course of pregnancy between both groups and the occurrence of complications that led to maternal hospitalization during pregnancy.
Results
There were 80 children conceived via ICSI and 450 children conceived via IVF.
Mean gestational age was significantly lower in the ICSI group (p = 0.001). After ICSI, the birth weight (p = 0.008) and the mean APGAR values after 1 minute and after 10 minutes were lower compared to that of the IVF group (p = 0.016 and p = 0.047, respectively). Moreover, ICSI-conceived children had to be hospitalized more often at a neonatal intensive care unit (p = 0.004). There was no difference in pH of the umbilical artery or in major congenital malformations between the two groups. Pregnancy complications (i.e., premature rupture of membranes, cervical insufficiency, and premature uterine contractions) and the need for maternal hospitalization during pregnancy were found significantly more often after IVF (p = 0.0016 and p = 0.0095, respectively), compared to the ICSI group.
Conclusions
When comparing IVF versus ICSI-conceived pregnancies at a tertiary care center, we found the course of pregnancy to be more complicated after IVF, whereas the primary fetal outcome seemed to be better in this group than after ICSI treatment.
Similar content being viewed by others
Background
In many countries, there is a tendency for more and more women to delay childbearing until an age when their fertility begins to decline. Therefore, in vitro fertilization (IVF) procedures have become accepted as an alternative to natural conception, and pregnancies subsequent to assisted reproductive techniques (ART) are common in obstetrical departments.
Although most pregnancies after IVF result in normal healthy outcomes, an increased risk for a number of obstetric and neonatal complications (such as preeclampsia, preterm delivery, lower average birth weight, and congenital malformations), compared to naturally conceived pregnancies, has been reported among singletons and twins [1–9]. This fact can be explained partly by the high rate of multiple pregnancies as a result of these procedures, and by advanced maternal age [10], but past research has also focused on the potential negative impact of micromanipulation techniques, extended culture systems, and medications used in the context of IVF/ICSI [11, 12].
While there are many studies that compare pregnancies after ART with spontaneously conceived pregnancies, fewer data are available that evaluate the differences between IVF and ICSI-conceived pregnancies. A recent study from Norway found that IVF pregnancies were associated with an increased risk of iatrogenic preterm delivery compared to ICSI pregnancies [13].
The aim of the present study was to report systematically on the course of 334 IVF or ICSI-conceived pregnancies and to focus on the differences between both groups with regard to maternal and fetal outcome parameters.
Methods
Between September 2003 and January 2009, 482 pregnant women with 722 fetuses, who had conceived via ART were referred to the Department of Obstetrics and Gynecology, Division of Obstetrics and Fetomaternal Medicine, Medical University of Vienna, Austria. Seventeen of the 722 fetuses were stillborn in the early gestational weeks, and, in 175 cases, there was insufficient information about the further course of pregnancy, and the status of birth and neonatal outcome, because patients were lost to follow-up. Therefore, after excluding cases of stillbirth and subjects lost to follow-up, a total of 334 pregnancies and 530 children could be included in our retrospective cohort study.
Outcome variables included maternal parameters: i.e., age; BMI; gravity; number of fetuses; pregnancy complications such as pregnancy-induced hypertension, preeclampsia, premature rupture of membranes, cervical insufficiency, and premature uterine contractions; and number of hospitalizations; and fetal parameters: i.e., gestational age; birth weight; birth height; pH of the umbilical artery; APGAR after one minute; APGAR after 10 minutes; congenital malformation; admission of the newborn to a neonatal intensive care unit (NICU); and death of the infant.
Institutional Review Board approval was obtained for the study, and women had given informed consent for the analysis of their data in the context of any retrospective evaluation. The present study was performed after approval of the responsible ethics committee. Ethikkommission der Universität Wien / Ethics commission of the Medical University of Vienna.
Statistical analysis was performed by the Center for Medical Statistics, Informatics and Intelligent Systems, Section for Medical Statistics of the Medical University of Vienna.
Descriptive results are given as mean ± standard deviation (or median and range) or frequencies and percentages. Spearman correlation coefficients were calculated.
Comparisons between IVF and ICSI pregnancies for variables that were considered maternal parameters were performed using t-tests (Wilcoxon-tests) or chi2-tests (Fisher’s exact tests). Comparisons between the two groups for fetal variables were performed using linear or generalized linear mixed models (ANOVA/ANCOVA).
In addition, based on correlations and information from the literature, some of the models were adjusted for other known influence factors and, hence, are analyzed using linear or generalized linear regression models.
As a secondary analysis, considering only singleton pregnancies, differences in gestational age between the two groups were calculated using the t-test (or Wilcoxon- test).
Analyses were performed using SAS 9.2 and SPSS 20 software. P-values <0.05 were considered statistically significant.
Results
A total of 530 children of 334 mothers were included in our data analysis, 80 conceived via ICSI, and 450 via conventional IVF treatment.
In 155 cases (21 ICSI/ 134 IVF), we found a singleton pregnancy, in 160 cases (25 ICSI/135 IVF) twins, in 17 cases triplets (3 ICSI/ 14 IVF), and in one case a quadruplet after conventional IVF treatment.
The distribution between singleton and multiple pregnancies was not significantly different between IVF and ICSI.
Maternal characteristics and outcome parameters are given in Tables 1 and 2.
Women with IVF showed statistically significantly more frequent pregnancy complications, such as premature rupture of membranes, premature uterine contractions, or cervix insufficiency (p = 0.0016), and had to be hospitalized more often during the second and third trimester of pregnancy (p = 0.0095).
Neonatal outcome parameters are shown in Tables 3 and 4 (for all fetuses) and Tables 5 and 6 (results for singleton and multiple pregnancies given separately).
Mean gestational age was significantly lower in the ICSI group when including all pregnancies (p = 0.001, ƞ2p = .019). Moreover, the gestational age was statistically significantly lower in the group of multiple gestations (p < 0.001, ƞ2p = .080) compared to singletons, but also when comparing multiples after ICSI with multiples after IVF (p = 0.009, ƞ2p = .019). Focusing only on singleton pregnancies, we found no significant difference in gestational age.
We also determined gestational age categories to assess the risk of preterm delivery among deliveries and defined extremely preterm as < 28 weeks (age group 1), and moderately preterm from 28 to 34 weeks (age group 2), and compared the early age groups against children born after week 34 (age group 3). There was a statistically significant difference in distribution between ICSI with 7.9%, 46.05%, and 46.05% children, and IVF with 4.7%, 24.2%, and 85.5% children in the three age groups (p = 0.0039). Considering only singleton pregnancies, there were no children in the lowest age group, and 14.3% and 85.7% children in the higher groups after ICSI. In the IVF group, 0.8%, 8.1%, and 91.1% singletons were found in the three age groups. These distributions were not statistically significant (p = 0.62).
Birth weight was statistically significantly lower within the ICSI group (p = 0.008, ƞ2p = .016) when considering all fetuses; multiples had a lower birth weight compared to singletons in both groups, but there was no difference between IVF and ICSI-conceived pregnancies.
Mean APGAR 1 and APGAR 10 indices were slightly lower within the ICSI group for singletons as well as for multiples.
Admission to NICU was significantly more often observed within the ICSI group.
(χ2 = 8.13, p = 0.004); moreover, multiples had to be more often hospitalized compared to singletons (χ2 = 32.21, p < 0.001).
No differences between the groups could be found regarding the number of major congenital malformations and infant deaths.
Concerning the distribution of female and male sex between the neonates, we found no significant difference between the IVF and the ICSI group (IVF: 45.6% baby girls, ICSI: 50.6% baby girls).
High correlations, with correlation coefficients greater than 0.7, were found between the number of hospitalizations and premature rupture of membranes, gestational age and birth height, gestational age and birth weight, birth height and birth weight, APGAR1 and APGAR10, APGAR1 and infant death, and APGAR10 and infant death. Correlations between 0.4 and 0.7 could be found between gestational age and APGAR1, gestational age and APGAR10, gestational age and admission to the NICU, gestational age and infant death, birth height and APGAR1, birth height and APGAR10, birth height and admission to the NICU, birth height and infant death, birth weight and APGAR1, birth weight and APGAR10, birth weight and admission to the NICU, birth weight and infant death, number of fetuses and gestational age, and premature rupture of membranes and maternal hospitalization.
Discussion
The number of pregnancies after ART is still increasing and there is some data showing that IVF/ICSI is associated with a higher rate of complications with regard to both the course of pregnancy and neonatal outcome. Of note, the potential negative impact of micromanipulation techniques should be considered, but only a few research studies have made precise distinctions between IVF and ICSI pregnancies [11, 12, 14].
Therefore, we systematically analyzed and compared 334 pregnancies and 530 children after IVF and ICSI, and discovered that the course of pregnancy is more complicated in IVF pregnancies (leading to more frequent maternal hospitalizations), whereas the primary fetal outcome (i.e., APGAR value after one minute and the necessity for admission to a NICU) seems to be better in this group than after ICSI treatment.
The significant association between IVF pregnancies and premature rupture of membranes, premature uterine contractions, and cervical insufficiency could be seen as concordant with the results of a smaller study that reported an increased preterm delivery risk in IVF versus ICSI-conceived pregnancies [15]. Mean gestational age at the time of delivery, however, did not differ between the two groups in our study, which supports data from Bonduelle et al., who found no disproportion in preterm delivery between pregnancies after the two major methods of ART. Preeclampsia, recently linked with decreased ovarian reserve [1], was not found to be overrepresented in our IVF group, although one might have suspected a relation between female subfertility (not male subfertility, leading to ICSI) and decreased ovarian reserve, and therefore, preeclampsia.
There were significant differences between the groups concerning gestational age, fetal birth weight, and mean APGAR levels, with lower levels for all variables in the ICSI group. Moreover, children in this group had to be admitted to the NICU more often.
A plausible explanation for this phenomenon is lacking; one might, however, speculate that early manipulation of the egg cell for ICSI could have a long-term negative impact.
When analyzing age groups, we found the risk of preterm delivery to be higher after ICSI treatment, but the fact that this observation no longer existed when focusing only on singleton pregnancies led to the conclusion that this might be predominantly due to multiple gestations within the ICSI group. Of note, the average gestational age in multiples was significantly lower in the ICSI group compared to the IVF group; this was not true of singleton pregnancies, as shown in Tables 5 and 6.
Concerning major fetal malformations, there was no statistically significant difference between the two groups, which is in accordance with other studies [14, 16, 17]. Wen et al. recently performed a meta-analysis that included more than 124000 ART pregnancies [12], and found no difference in the risk for malformations between children conceived by IVF and/or ICSI, although ART-conceived pregnancies were generally at increased risk for birth defects, compared to naturally conceived pregnancies (OR: 1.37). This is in line with the results of Pinborg et al., who suspected subfertility per se as a major risk factor for adverse perinatal outcomes after ART [18]. The fact, however, that, even in the same mother, an ART singleton has a poorer outcome than a non-ART sibling, leads to the presumption that factors related to the hormonal stimulation, embryo culture, or cryopreservation may also have a potentially negative impact on the offspring. In contrast, a smaller case-controlled study revealed no increase in congenital malformations in ICSI-conceived pregnancies compared to naturally conceived pregnancies [11]—possibly because of the small sample size.
A Chinese study analyzing birth defects in over 15400 children after ART found that the distribution of birth defects reflects the distribution in the general population, while the total frequency of birth defects was not significantly higher within the ICSI group, compared to insemination or conventional IVF [19].
In our ICSI group, there was one case of a heart malformation and two cases of facial malformation, and, in the IVF group, two cases of heart malformation, one case of facial malformation, and one case of omphalocele combined with malformation of the limbs.
Notably, the number of children after ICSI was unusually low (15%) in our collective. A possible explanation could be that all women whose data were analyzed in the present retrospective study were referred to our tertiary care center by their gynecologist for a distinct reason (e.g., multiple pregnancy, advanced maternal age, desire for first-trimester screening, wish for a second opinion concerning the mode of delivery), and women who undergo an ICSI procedure, typically performed for male subfertility, might be younger and more healthy, and therefore, less often referred to a tertiary care unit. However, age, BMI, and pre-existing diseases, such as hypertension, did not differ between the two groups in our study.
We have to admit, however, that the disproportionate underrepresentation of ICSI is an obvious limitation of our study.
Moreover, the “origin” of sperm for ICSI (ejaculated/frozen/after testicular sperm extraction/after epididymal sperm aspiration) was unfortunately not systemically noted in our data. A recent cohort study revealed, however, that the above-mentioned methods of operative sperm collection seem to be as safe as conventional ICSI, IVF, and natural conception with regard to neonatal outcome, including congenital malformations [20].
Another possible limitation of our study is the lack of an age-matched control group.
We decided, however, against creating a control group from our high-risk collective at the University clinic (only a few uncomplicated pregnancies are treated at our center) in order to avoid comparing one high-risk collective (e.g., women after preterm delivery or premature rupture of membranes in a past pregnancy), with another (St. p. ART) and preferred to use data concerning uncomplicated pregnancy outcomes from low-risk collectives reported in the literature.
Conclusions
We systematically investigated a pre-defined group of Austrian women after conception via IVF/ICSI. We found that the course of pregnancies was more complicated after conventional IVF, whereas the primary fetal outcome seems to be better in this group, compared to ICSI treatment. Of course, our results must be interpreted with caution, as the study had a very skewed population, with underrepresentation of ICSI cases, and because the data were drawn exclusively from a tertiary care center. Further research that includes a larger cohort of ART pregnancies is required to confirm our hypothesis.
Abbreviations
- ART:
-
Assisted reproductive techniques
- i.e.:
-
Id est
- ICSI:
-
Intra cytoplasmatic sperm injection
- IVF:
-
In vitro fertilization.
References
Woldringh GH, Frunt MHA, Kremer JAM, Spaanderman MEA: Decreased ovarian reserve related to pre-eclampsia in IVF/ICSI pregnancies. Hum Reprod. 2006, 21: 2948-2954. 10.1093/humrep/del155.
Shevel T, Malone FD, Vidaver J, Porter TF, Luthy DA, Comstock CH, Hankins GD, Eddleman K, Dolan S, Dugoff L, et al: Assisted reproductive technology and pregnancy outcome. Obstet Gynecol. 2005, 106: 1039-1045. 10.1097/01.AOG.0000183593.24583.7c.
Cooper AR, O’Neill KE, Allsworth JE, Jungheim ES, Odibo AO, Gray D, Ratts VSL, Moley KH, Odem RR: Smaller fetal size in singletons after infertility therapies: the influence of technology and the underlying infertility. Fertil Steril. 2011, 96: 1100-1106. 10.1016/j.fertnstert.2011.08.038.
Källén B, Finnström O, Lindam A, Nilsson E, Nygren KG, Olausson PO: Selected neonatal outcomes in dizygotic twins after IVF versus non-IVF pregnancies. BJOG. 2010, 117: 676-682. 10.1111/j.1471-0528.2010.02517.x.
Tomic V, Tomic J: Neonatal outcome of IVF singletons versus naturally conceived in women aged 35 years and over. Arch Gynecol Obstet. 2011, 285: 1411-1416.
Buckett WM, Chian RC, Holzer H, Dean N, Usher R, Tan SL: Obstetric outcomes and congenital abnormalities after in vitro maturation, in vitro fertilization, and intrazytoplasmatic sperm injection. Obstet Gynecol. 2007, 110: 885-891. 10.1097/01.AOG.0000284627.38540.80.
Wisborg K, Ingerslev HJ, Henriksen TB: In vitro fertilization and preterm delivery, low birth weight, and admission to the neonatal intensive care unit: a prospective follow-up study. Fertil Steril. 2010, 94: 2102-2106. 10.1016/j.fertnstert.2010.01.014.
Helmerhorst FM, Perquin DA, Donker D, Keirse MJ: Perinatal outcome of singletons and twins after assistend conception: a systemic review of controlled studies. BMJ. 2004, 328: 261-10.1136/bmj.37957.560278.EE.
McDonald SD, Han Z, Mulla S, Murphy KE, Beyene J, Ohlsson A: Preterm birth and low birth weight among in vitro fertilization singletons: a systemic review and meta-analyses. Eur J Obstet Gynecol Reprod Biol. 2009, 146: 138-148. 10.1016/j.ejogrb.2009.05.035.
Finnström O, Källén B, Lindam A, Nilsson E, Nygren KG, Otterblad Olausson P: Maternal and child outcome after in vitro fertilization – a review of 25 years of population-based data from Sweden. Acta Obstet Gynecol Scan. 2011, 90: 494-500. 10.1111/j.1600-0412.2011.01088.x.
Al-Fifi S, Al-Binali A, Al-Shahrani M, Shafiq H, Bahar M, Almushait M, Sobandi L, Eskandar M: Congenital anomalies and other perinatal outcomes in ICSI vs. naturally conceived pregnancies: a comparative study. J Assist Reprod Genet. 2009, 26: 377-381. 10.1007/s10815-009-9329-3.
Wen J, Jiang J, Ding C, Dai J, Liu Y, Xia Y, Liu J, Hu Z: Birth defects in children conceived by in vitro fertilization and intracytoplasmatic sperm injection: a meta-analysis. Fertil Steril. 2012, 97 (6): 1331-1337. 10.1016/j.fertnstert.2012.02.053.
Morken NH: Preterm delivery in IVF versus ICSI singleton pregnancies: a national population-based cohort. Eur J Obstet Gynecol Reprod Biol. 2011, 154: 62-66. 10.1016/j.ejogrb.2010.08.025.
Bonduelle M, Liebaers I, Deketelaere V, Derde MP, Camus M, Devroey P, Van-Steirteghem A: Neonatal data on a cohort of 2889 infants born after ICSI (1991–1999) and 2995 infants born after IVF (1983–1999). Hum Reprod. 2002, 17: 671-694. 10.1093/humrep/17.3.671.
Stuebe AG, Mcelrath M: Tubal factor infertility is associated with an increased risk of preterm birth compared with male factor infertility. Am J Obstet Gynecol. 2006, 195: S75-
Belva F, De-Schrijver F, Tournaye H, Liebaers I, Devroey P, Haentjens P, Bonduelle M: Noenatal outcome of 724 children born after ICSI using non-ejaculated sperm. Hum Reprod. 2011, 26: 1752-1758. 10.1093/humrep/der121.
Pandey S, Shetty A, Hamilton M, Bhattacharya S, Maheshwari A: Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systemic review and meta-analysis. Hum Reprod Update. 2012, 18: 485-503. 10.1093/humupd/dms018.
Pinborg A, Wennerholm UB, Romundstad LB, Loft A, Aittomaki K, Söderström-Anttila V, Nygren KG, Hazekamp J, Bergh C: Why do singleton conveived after assisted reproductive technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum Reprod Update. 2013, 19: 87-104. 10.1093/humupd/dms044.
Yan J, Huang G, Sun Y, Zhao X, Chen S, Zou S, Hao C, Quan S, Chen ZJ: Birth defects after assisted reproduuctive technologies in China: analysis of 15,405 offspring in seven centers (2004–2008). Fertil Steril. 2011, 95: 458-460. 10.1016/j.fertnstert.2010.08.024.
Fedder J, Loft A, Parner ET, Rasmussen S, Pinborg A: Neonatal outcome and congenital malformations in children born after ICSI with testicular or epididymal sperm: a controlled national cohort study. Hum Reprod. 2013, 28: 230-240. 10.1093/humrep/des377.
Acknowledgments
The authors want to thank Bernd Otzelberger for precious statistical support and Mary McAllister for careful proofreading of the manuscript and language corrections.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interest
The authors declare that they have no competing interest.
Authors’ contributions
KN designed, analyzed, and reported the study. JO and DP analyzed the data. LS acquired the data presented in Tables 1, 2, 3, 4, 5 and 6. SF performed the statistical analysis. KW analysed, reported, and revised the study. All authors contributed to the study protocol, and read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Nouri, K., Ott, J., Stoegbauer, L. et al. Obstetric and perinatal outcomes in IVF versus ICSI-conceived pregnancies at a tertiary care center - a pilot study. Reprod Biol Endocrinol 11, 84 (2013). https://doi.org/10.1186/1477-7827-11-84
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7827-11-84