Abstract
Background
Infertile women might get pregnant sometime after fertility treatment, but today, there is no prediction model on who will eventually have children. The objective of the present study was to characterize hormone levels in an arbitrary menstrual cycle in women with unexplained infertility and male infertility, and to determine the predictive value for long-term possibility of live birth.
Methods
In this cross-sectional study, with 71 infertile women with diagnosis unexplained infertility and male infertility, blood samples were obtained during the proliferative and secretory phases of an arbitrary menstrual cycle. Serum concentrations of FSH, LH, AMH, inhibin B, estradiol, progesterone, PRL and TSH were determined. The predictive value of ovulation and hormonal analysis was determined by identifying the proportion of women with at least one live birth. Mann Whitney U test, chi2 test and Spearman’s correlation were used for statistical analysis. A value of p < 0.05 was considered statistically significant.
Results
There were no differences in hormone values and live birth rates between women with unexplained infertility and male infertility. The best sole predictors of live birth were age of the women, followed by ovulatory cycle, defined as serum progesterone concentration of greater than or equal to 32 nmol/L, and a serum TSH concentration of less than or equal to 2.5 mIU/L. Combining the age with the ovulatory cycle and serum TSH less than or equal to 2.5 mIU/L or serum AMH greater than or equal to 10 pmol/L the predictive value was close to 90%.
Conclusions
Age in combination with the presence of an ovulatory cycle and serum TSH or serum AMH is predictive for long-term live birth. The advantage of serum AMH compared with serum TSH is the very little variation throughout the menstrual cycle, which makes it a useful tool in infertility diagnosis.
Similar content being viewed by others
Background
The menstrual cycle reflects a complex combination of synchronized endocrine events in which the hypothalamus, the anterior pituitary and the ovaries are involved [1]. These events are necessary for successful oocyte development, ovulation, fertilization and implantation.
Gonadotrophin-Releasing Hormone (GnRH), Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH) control ovarian function through a sensitive feedback system. A high level of serum FSH in the early follicular phase, a consequence of reduced ovarian function, is predictive of impaired pregnancy outcome after infertility treatment [2] and it has been shown that a combination of low FSH levels and high LH levels can predict pregnancy outcome after infertility treatment [3].
Anti-Müllerian hormone (AMH) is a dimeric glycoprotein produced by granulosa cells from pre-antral and antral follicles. The main role of AMH is to inhibit follicular development from primordial to primary follicular stages. During the menstrual cycle, serum AMH levels are relatively stable [4]. AMH seems also to be a better predictor of pregnancy outcome after IVF treatment than other hormonal parameters [5, 6].
Inhibin B, produced by granulosa cells in antral follicles, has been suggested as a marker of follicular growth. Low serum inhibin B levels have been related to elevated levels of FSH, which have been shown to have an association with decreased oocyte quality and fertility [4]. The levels of inhibin B vary more than AMH throughout the menstrual cycle. However, the combination of concentrations of AMH and inhibin B is predictive for pregnancy after infertility treatments [7].
Oestrogen plays important roles in oocyte maturation, embryo quality and fertilization [8, 9]. The most important oestrogen is estradiol (E) [8], the serum level of which in combination with that of FSH, and age is predictive of pregnancy outcome after IVF treatment [10].
Progesterone (P) is the most important hormone for endometrial development, implantation and maintenance of pregnancy [11]. Progesterone support during the luteal phase has been shown to result in significantly better pregnancy rates as well as live birth rates after infertility treatment [12, 13].
Thyroid hormones influence ovarian function directly and indirectly through elevated prolactin (PRL) and altered GnRH secretion. In women with thyroid dysfunctions, ovarian insufficiencies are common [14]. Elevated levels of serum PRL have been associated with menstrual disorders as a result of its restraining effect on pulsatile GnRH secretion as well as inhibition of FSH and LH release [15]. Furthermore, hyperprolactinaemia has been shown to be associated with ovulatory dysfunction [16] and both hypothyroidism and hyperprolactinaemia have been implicated in infertility. However, the association between pregnancy outcome and serum TSH levels is controversial. It has been shown that infertile women with elevated levels of serum TSH have lower pregnancy rates than women with normal TSH levels [16].
Approximately 10% of all couples worldwide are infertile [17]. In the western world, women tend to have their first child at an older age, which decreases overall fertility. Therefore, we believe that women with tendency of early ovarian failure will be the most vulnerable group of women in this respect. The most successful treatment of infertility is in vitro fertilization (IVF) [18] with pregnancy rates between 13–43% per single IVF cycle [18–20]. However, some couples experience repeated failures of pregnancy after treatment [21].
Women with unexplained infertility are often considered to be subfertile, and will eventually become pregnant spontaneously sometime after fertility treatment [22]. The possibility of successful pregnancy in the long term depends on the presence of ovulatory menstrual cycles. The long-term probability of live birth in women with unexplained infertility and women with male infertility has to our knowledge not previously been investigated. Therefore, we studied serum hormone levels in an arbitrary menstrual cycle and determined the predictive value for long-term possibility of live birth in women with unexplained infertility and male infertility.
Methods
Study design and subjects
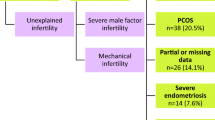
Seventy-one infertile women, referred to the Fertility Unit at Karolinska University Hospital Huddinge between 1999 and 2008 participated in the study. Recruitment of the women was focused on unexplained infertility and male infertility, as these two groups of patients have normal menstrual cycles. All women were referred from an outpatient gynaecological clinic to the Fertility Unit for further examination and treatment of infertility. The women were healthy except for their infertility and did not use any hormonal medication.
Infertility was determined by way of a standard set of tests that included hormone analyses and at least two semen analyses. Tubal passage was demonstrated by Hysterosalpingo Contrast Sonography (HyCoSy), or, if needed, laparoscopy was performed to exclude factors such as endometriosis. Semen analyses were based on WHO criteria of normality. The final diagnosis was established after these examinations. The diagnosis of unexplained infertility was chosen when no explanation for infertility was found, and the diagnosis of male infertility was set for women whose partner had abnormal semen analyses.
Most of the women were contacted by telephone five years after inclusion in the study and asked about pregnancy outcome, or the data of live birth was determined from patient records. Informed consent was obtained from all participating women and the study was approved by the Ethics Committee of Karolinska Institutet.
Collection of blood samples
Blood samples were obtained at regular intervals during one arbitrary normal menstrual cycle. In most women blood was collected three times during the follicular phase and four times during the luteal phase for assay of serum FSH, LH, AMH, inhibin B, E, P, PRL and TSH. All hormones except E and P were analysed in blood obtained at cycle day 2 to 5. Serum E levels were determined on three occasions; before the LH surge (LH -6 to LH -1), the early secretory phase (LH 0 to LH +5) and the mid-luteal phase (LH +6 to LH +9). Progesterone was assayed in four different samples during the luteal phase for determination of area under the curve (AUC), measured as concentration of progesterone/day. Additionally, the value determined during the mid-luteal phase (LH +6 to LH +8) is also shown.
Hormone analyses
All blood samples were analysed at the same time using routine methods at the central clinical laboratory (FSH, LH, E, P and PRL) at Karolinska University Hospital Huddinge or at the research laboratory, Department of Obstetrics and Gynaecology, Uppsala University Hospital, Uppsala, Sweden (TSH, AMH and inhibin B).
Serum concentrations of FSH and LH were measured using AutoDELFIA hFSH and hLH respectively (Perkin Elmer, Waltham, Massachusetts, USA). An enzyme-linked immunosorbent assay (ELISA) (Immunotech, A Beckman Coulter Company, Marseille, France) was used to determine serum AMH levels. The intra-assay CV of the ELISA was 12.3% and the inter-assay CV was 14.2%. The active Inhibin B Gen II enzyme-linked immunosorbent assay (Diagnostic Systems Laboratories, Inc., A Beckman Coulter Company, Webster, USA) was used to measure serum inhibin B levels. The intra-assay CV of the ELISA was 2.40% and the inter-assay CV was 3.68%. Two values of inhibin B were determined to be < 7 pg/mL. These were set to 7.0 pg/mL in the statistical analysis. Serum E and P were assayed by using Modular Analytics E170 equipment (Roche, Basel, Switzerland). Levels of TSH and PRL were measured by using a Roche Cobas e601 system (Roche, Basel, Switzerland).
Definition of ovulation, cut-off values and live birth
Ovulation was established according to Landgren et al. [23], using a serum P concentration of ≥ 32 nmol/L (anovulation < 32 nmol/L). For FSH < 7.0 IU/L, for the FSH:LH ratio ≤ 2.0 [24] and for AMH ≥ 10 pmol/L were used as cut-off values. The cut-off value for TSH was set to 2.5 mIU/L according to Baker et al. [25]. Serum concentrations of inhibin B and PRL varied considerably; therefore these hormones were not used for prediction of live birth. Live birth was defined as delivery of a healthy child. All live births were considered regardless of time in relation to the arbitrary cycle and regardless of whether or not it was spontaneously conceived or conceived after infertility treatment.
Statistical analysis
Statistical analyses were performed using SPSS (Statistical Package for the Social Sciences) software (SPSS 15.0 for Windows; SPSS Inc. Chicago, IL). Data is given as median (range). We used the Mann Whitney U test for comparisons between two groups. For comparisons including categorical variables the χ2 test was applied. Spearman’s correlation was used for correlation analysis. A value of p < 0.05 was considered statistically significant.
The predictive value of ovulation and hormonal analysis was determined by identifying the proportion of women with at least one live birth 5 years or more after inclusion in the study. The calculation of the predictive value was performed as previously described [26].
Results
Patient characteristics
Patient characteristics are shown in Table 1. The groups consisted of 42 women with unexplained infertility and 29 women with male infertility.
Hormone profile and pregnancy outcome in relation to diagnosis
There were no significant differences in hormone values or pregnancy outcome in relation to diagnosis when comparing the women with unexplained infertility and women with male infertility. Hormone concentrations and pregnancy outcome in relation to infertility diagnosis are shown in Table 2.
Ovulation
Lack of ovulation could be a sign of premature menopause. The occurrence of ovulation did not affect any of the other hormones or the possibility of a live birth after 5 years or more. The numbers of women that ovulated in both groups are shown in Table 2.
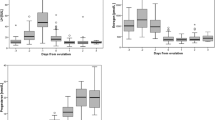
Correlations
Serum levels of AMH were associated with the FSH:LH ratio (p < 0.001) (Figure 1), but not with those of FSH, (p = 0.11). Serum levels of inhibin B were associated with those of AMH (p = 0.013), but not with those of FSH, or the FSH:LH ratio (p = 0.266 and 0.112 respectively).
Prediction of pregnancy outcome
None of the studied hormones were good predictors of long-term pregnancy outcome (Table 3). The best hormonal predictor, with a predictive value of 56%, sensitivity of 78% and specificity of 30% was the presence of ovulatory menstrual cycles (Table 3). However, and not surprisingly, age was the best predictor of successful future pregnancies – predictive value 77%, sensitivity 54% and specificity 82% (Table 3). Combined prediction using the three best predictive values: age, presence of ovulatory cycles as determined by P ≥ 32 nmol/L and TSH ≤ 2.5 mIU/L increased the probability of predicting live birth to 88%, with a sensitivity of 100% and specificity of 33%. Since AMH has increased in popularity in infertility evaluation, we also calculated a combined predictive value of age, presence of ovulatory cycle and AMH ≥ 10 pmol/L. This calculation resulted in the predictive value of 83%, sensitivity of 83% and specificity of 25%. Menstrual cycle length, and serum inhibin B and PRL concentrations did not predict the later possibility of a live birth (data not shown).
Discussion
Serum hormone concentrations in 71 women, with diagnoses unexplained infertility and male infertility, were studied during one arbitrary natural menstrual cycle to investigate the possibility of predicting live birth. There were no significant differences in hormone levels or pregnancy outcome between women with unexplained infertility and women with male infertility.
One reason for increased infertility problems in Sweden is that women tend to delay their pregnancies, which results in a reduced fertility rate [27]. This is also seen in the present study where it is shown that women at the age of 32 or less have the highest chance of a future live birth. Age of the women had the best predictive value of live birth, which is also known from previous studies [28, 29]. The increasing age has also been associated with a shortening length of the menstrual cycle, and the women with cycle length < 26 days has been shown to have significantly lower pregnancy rates after infertility treatment compared with the women with cycle length >34 days [30]. However, this could not been shown in our study, where the menstrual cycle length was not related to the pregnancy outcome.
The presence of one progesterone value ≥ 32 nmol/L was indicative of ovulation [23]. In the present study, an ovulatory cycle as assessed by assay of serum P was a better predictor of a future live birth than levels of any of the other hormones. It has previously been suggested that women with unexplained infertility have diminished ovarian reserve [31], but this was not noticed in our study.
The use of AMH for determination of ovarian function instead of FSH and/or FSH:LH ratio has increased, and therefore we studied the correlations between these parameters. Serum concentrations of AMH correlated with the FSH:LH ratio, and also with inhibin B levels, which leads to the conclusion that AMH could replace these markers in assessment of ovulatory function. The advantage of AMH is its capacity to maintain relative stable levels during the menstrual cycle [32] although circadian variations have been observed [33]. The disadvantage of AMH is that there are still no international standard assays for AMH measurement, which makes comparison between different laboratories complicated [34].
It has previously been shown that FSH:LH ratio can be used as predictor of pregnancy outcome in infertile women [35], but this was not confirmed in the present study. It has also been demonstrated that AMH is a better marker than age, FSH on cycle day 3 or inhibin B for prediction of IVF pregnancy success [36], which could neither be shown in the present study. However, our data showed that AMH combined with age and an ovulatory menstrual cycle was predictive for future live birth.
There are only limited data on inhibin B and AMH, and we are not aware of any studies in which groups of infertile women have been compared. However, there was considerable individual variation in serum levels of inhibin B and PRL, which shows that these hormones are not useful in diagnosis and prediction of live birth in women with unexplained and male infertility.
We found no differences in TSH levels between women in the studied groups. Previously, Cramer et al. [16] demonstrated relatively high TSH levels and relatively low PRL levels in women with male infertility. Conversely, Arojoki et al. [37] found the lowest TSH levels in women with male infertility, and the highest levels of TSH in women with unexplained infertility, and ovulatory dysfunction. However, menstrual disorders in women with hypothyroidism are more rare than previously reported [38]. In our study TSH as a single variable was not predictive for future live birth, but the combination with age of 32 or less, ovulatory cycle and TSH ≤ 2.5 mIU/L resulted in a predictive value of 88%.
The strength of the present study is the number of hormones measured. Eight different hormones were measured at various occasions during the menstrual cycle and the patients needed to come to the clinic several times during one natural cycle, which may have been challenging for women undergoing in vitro fertilisation. Additionally, our study group was well-defined in two selected groups; unexplained infertile and male infertility, while many previous studies have included patients regardless of cause of infertility. To our knowledge, the long-term probability of live birth in women with unexplained infertility and women with male infertility has not previously been studied.
A weakness of our study is the long recruitment period, which resulted in a prolonged follow-up time. Possible factors (e.g. stress) influencing the serum hormone levels were not taken into account, which may be considered a drawback.
Conclusions
It can be concluded from the present results that there are no perfect markers for prediction of pregnancy outcome on a long-term basis; the best is still the age of the woman. Age in combination with the presence of an ovulatory cycle and a serum TSH concentration of ≤ 2.5 mIU/L or AMH concentration of ≥ 10 pmol/L is predictive of live birth in the long term. The advantage of serum AMH is its only slight variation in concentration throughout the menstrual cycle, which makes it a more useful tool in infertility diagnosis than TSH.
References
Hawkins SM, Matzuk MM: The menstrual cycle: basic biology. Ann N Y Acad Sci. 2008, 1135: 10-18. 10.1196/annals.1429.018.
Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB: A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update. 2006, 12: 685-718. 10.1093/humupd/dml034.
Brodin T, Bergh T, Berglund L, Hadziosmanovic N, Holte J: High basal LH levels in combination with low basal FSH levels are associated with high success rates at assisted reproduction. Hum Reprod. 2009, 24: 2755-2759. 10.1093/humrep/dep254.
Broekmans FJ, Soules MR, Fauser BC: Ovarian aging: mechanisms and clinical consequences. Endocr Rev. 2009, 30: 465-493. 10.1210/er.2009-0006.
Wu CH, Chen YC, Wu HH, Yang JG, Chang YJ, Tsai HD: Serum anti-Mullerian hormone predicts ovarian response and cycle outcome in IVF patients. J Assist Reprod Genet. 2009, 26: 383-389. 10.1007/s10815-009-9332-8.
Brodin T, Hadziosmanovic N, Berglund L, Olovsson M, Holte J: Antimullerian hormone levels are strongly associated with live-birth rates after assisted reproduction. J Clin Endocrinol Metab. 2013, 98: 1107-1114. 10.1210/jc.2012-3676.
Wunder DM, Guibourdenche J, Birkhauser MH, Bersinger NA: Anti-Mullerian hormone and inhibin B as predictors of pregnancy after treatment by in vitro fertilization/intracytoplasmic sperm injection. Fertil Steril. 2008, 90: 2203-2210. 10.1016/j.fertnstert.2007.10.078.
Sundarrajan C, Liao W, Roy AC, Ng SC: Association of oestrogen receptor gene polymorphisms with outcome of ovarian stimulation in patients undergoing IVF. Mol Hum Reprod. 1999, 5: 797-802. 10.1093/molehr/5.9.797.
Sundarrajan C, Liao WX, Roy AC, Ng SC: Association between estrogen receptor-beta gene polymorphisms and ovulatory dysfunctions in patients with menstrual disorders. J Clin Endocrinol Metab. 2001, 86: 135-139. 10.1210/jc.86.1.135.
Srouji SS, Mark A, Levine Z, Betensky RA, Hornstein MD, Ginsburg ES: Predicting in vitro fertilization live birth using stimulation day 6 estradiol, age, and follicle-stimulating hormone. Fertil Steril. 2005, 84: 795-797. 10.1016/j.fertnstert.2005.02.042.
Graham JD, Clarke CL: Physiological action of progesterone in target tissues. Endocr Rev. 1997, 18: 502-519. 10.1210/er.18.4.502.
Bjuresten K, Landgren BM, Hovatta O, Stavreus-Evers A: Luteal phase progesterone increases live birth rate after frozen embryo transfer. Fertil Steril. 2011, 95: 534-537. 10.1016/j.fertnstert.2010.05.019.
Erdem A, Erdem M, Atmaca S, Guler I: Impact of luteal phase support on pregnancy rates in intrauterine insemination cycles: a prospective randomized study. Fertil Steril. 2009, 91: 2508-2513. 10.1016/j.fertnstert.2008.04.029.
Poppe K, Velkeniers B, Glinoer D: Thyroid disease and female reproduction. Clin Endocrinol (Oxf). 2007, 66: 309-321. 10.1111/j.1365-2265.2007.02752.x.
Kostrzak A, Warenik-Szymankiewicz A, Meczekalski B: The role of serum PRL bioactivity evaluation in hyperprolactinaemic women with different menstrual disorders. Gynecol Endocrinol. 2009, 25: 799-806. 10.3109/09513590903209329.
Cramer DW, Sluss PM, Powers RD, McShane P, Ginsburgs ES, Hornstein MD, Vitonis AF, Barbieri RL: Serum prolactin and TSH in an in vitro fertilization population: is there a link between fertilization and thyroid function?. J Assist Reprod Genet. 2003, 20: 210-215. 10.1023/A:1024151210536.
Boivin J, Bunting L, Collins JA, Nygren KG: International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod. 2007, 22: 1506-1512. 10.1093/humrep/dem046.
Smith S, Pfeifer SM, Collins JA: Diagnosis and management of female infertility. JAMA. 2003, 290: 1767-1770. 10.1001/jama.290.13.1767.
Ola B, Li TC: Implantation failure following in-vitro fertilization. Curr Opin Obstet Gynecol. 2006, 18: 440-445. 10.1097/01.gco.0000233940.82296.49.
Isaksson R, Tiitinen A: Present concept of unexplained infertility. Gynecol Endocrinol. 2004, 18: 278-290. 10.1080/0951359042000199878.
Margalioth EJ, Ben-Chetrit A, Gal M, Eldar-Geva T: Investigation and treatment of repeated implantation failure following IVF-ET. Hum Reprod. 2006, 21: 3036-3043. 10.1093/humrep/del305.
Evers JL: Female subfertility. Lancet. 2002, 360: 151-159. 10.1016/S0140-6736(02)09417-5.
Landgren BM, Unden AL, Diczfalusy E: Hormonal profile of the cycle in 68 normally menstruating women. Acta Endocrinol (Copenh). 1980, 94: 89-98.
Liu KE, Greenblatt EM: Elevated day 3 follicle-stimulating hormone/luteinizing hormone ratio >or= 2 is associated with higher rates of cancellation in in vitro fertilization-embryo transfer cycles. Fertil Steril. 2008, 90: 297-301. 10.1016/j.fertnstert.2007.06.038.
Baker VL, Rone HM, Pasta DJ, Nelson HP, Gvakharia M, Adamson GD: Correlation of thyroid stimulating hormone (TSH) level with pregnancy outcome in women undergoing in vitro fertilization. Am J Obstet Gynecol. 2006, 194: 1668-1674. 10.1016/j.ajog.2006.03.040. discussion 1674–1665
Csemiczky G, Wramsby H, Landgren BM: Luteal phase oestradiol and progesterone levels are stronger predictors than follicular phase follicle stimulating hormone for the outcome of in-vitro fertilization treatment in women with tubal infertility. Hum Reprod. 1996, 11: 2396-2399. 10.1093/oxfordjournals.humrep.a019122.
Mac Dougall K, Beyene Y, Nachtigall RD: ‘Inconvenient biology:’ advantages and disadvantages of first-time parenting after age 40 using in vitro fertilization. Hum Reprod. 2012, 27: 1058-1065. 10.1093/humrep/des007.
Chuang CC, Chen CD, Chao KH, Chen SU, Ho HN, Yang YS: Age is a better predictor of pregnancy potential than basal follicle-stimulating hormone levels in women undergoing in vitro fertilization. Fertil Steril. 2003, 79: 63-68. 10.1016/S0015-0282(02)04562-4.
Wang JG, Douglas NC, Nakhuda GS, Choi JM, Park SJ, Thornton MH, Guarnaccia MM, Sauer MV: The association between anti-Mullerian hormone and IVF pregnancy outcomes is influenced by age. Reprod Biomed Online. 2010, 21: 757-761. 10.1016/j.rbmo.2010.06.041.
Brodin T, Bergh T, Berglund L, Hadziosmanovic N, Holte J: Menstrual cycle length is an age-independent marker of female fertility: results from 6271 treatment cycles of in vitro fertilization. Fertil Steril. 2008, 90: 1656-1661. 10.1016/j.fertnstert.2007.09.036.
Leach RE, Moghissi KS, Randolph JF, Reame NE, Blacker CM, Ginsburg KA, Diamond MP: Intensive hormone monitoring in women with unexplained infertility: evidence for subtle abnormalities suggestive of diminished ovarian reserve. Fertil Steril. 1997, 68: 413-420. 10.1016/S0015-0282(97)00222-7.
Robertson DM, Hale GE, Fraser IS, Hughes CL, Burger HG: Changes in serum antimullerian hormone levels across the ovulatory menstrual cycle in late reproductive age. Menopause. 2011, 18: 521-524. 10.1097/gme.0b013e3181f8d9e0.
Bungum L, Jacobsson AK, Rosen F, Becker C, Yding Andersen C, Guner N, Giwercman A: Circadian variation in concentration of anti-Mullerian hormone in regularly menstruating females: relation to age, gonadotrophin and sex steroid levels. Hum Reprod. 2011, 26: 678-684. 10.1093/humrep/deq380.
Penarrubia J, Fabregues F, Manau D, Creus M, Casals G, Casamitjana R, Carmona F, Vanrell JA, Balasch J: Basal and stimulation day 5 anti-Mullerian hormone serum concentrations as predictors of ovarian response and pregnancy in assisted reproductive technology cycles stimulated with gonadotropin-releasing hormone agonist--gonadotropin treatmen. Hum Reprod. 2005, 20: 915-922.
Seckin B, Turkcapar F, Ozaksit G: Elevated day 3 FSH/LH ratio: a marker to predict IVF outcome in young and older women. J Assist Reprod Genet. 2011, 29: 231-236.
Dehghani-Firouzabadi R, Tayebi N, Asgharnia M: Serum level of anti-mullerian hormone in early follicular phase as a predictor of ovarian reserve and pregnancy outcome in assisted reproductive technology cycles. Arch Iran Med. 2008, 11: 371-376.
Arojoki M, Jokimaa V, Juuti A, Koskinen P, Irjala K, Anttila L: Hypothyroidism among infertile women in Finland. Gynecol Endocrinol. 2000, 14: 127-131. 10.3109/09513590009167671.
Krassas GE: Thyroid disease and female reproduction. Fertil Steril. 2000, 74: 1063-1070. 10.1016/S0015-0282(00)01589-2.
Acknowledgements
The authors acknowledge Elisabeth Berg, statistician at Karolinska Institutet for assistance with statistics and Nick Bolton, Oxford, UK for language revision. This work was supported by grants from the Family Planning Foundation, Uppsala, Sweden, Praktikertjänst AB, Stockholm, Sweden, Vivian Wahlberg’s Foundation, Stockholm, Sweden and Pampers, Sweden.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
TM participated in the design of the study and its coordination, and performed the statistical analysis and drafted the manuscript. KB carried out the patient recruitment and collected the blood samples, and participated in the coordination of the study. BML conceived of the study and participated in its design and coordination, and helped to draft the manuscript. ASE participated in the design of the study and its coordination, and helped to perform the statistical analysis and drafted the manuscript. All authors read approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Murto, T., Bjuresten, K., Landgren, BM. et al. Predictive value of hormonal parameters for live birth in women with unexplained infertility and male infertility. Reprod Biol Endocrinol 11, 61 (2013). https://doi.org/10.1186/1477-7827-11-61
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7827-11-61