Abstract
Chemokines are small molecular weight peptides responsible for adhesion, activation, and recruitment of leukocytes into tissues. Leukocytes are thought to influence follicular atresia, ovulation, and luteal function. Many studies in recent years have focused attention on the characterization of leukocyte populations within the ovary, the importance of leukocyte-ovarian cell interactions, and more recently, the mechanisms of ovarian leukocyte recruitment. Information about the role of chemokines and leukocyte trafficking (chemotaxis) during ovarian function is important to understanding paracrine-autocrine relationships shared between reproductive and immune systems. Recent advances regarding chemokine expression and leukocyte accumulation within the ovulatory follicle and the corpus luteum are the subject of this mini-review.
Similar content being viewed by others
Introduction
Leukocyte recruitment and activation within the ovary are thought to play important roles in follicular atresia, ovulation, and luteal function [1–6]. Consequently, many studies concerning ovarian function within the past several years have focused on characterizing leukocyte populations within the ovary, understanding further the importance of leukocyte-ovarian cell interactions, and more recently, discerning the mechanisms of ovarian leukocyte recruitment. The existence of specific subsets of leukocytes (e.g., monocytes-macrophages, T-lymphocytes, eosinophils, etc.) and their fluctuation in number within the ovary during select stages of ovarian function are currently well-documented [7–15]. Leukocytes and their secretory products are thought to influence ovarian function by acting as local mediators of follicular atresia, ovulation, and luteolysis [16–20]. The observation that leukocytes accumulate only within certain structures of the ovary, suggests that these cells migrate from the bloodstream in response to specific, unidirectional chemoattractant cues. The discovery and characterization of an ever-expanding family of molecules specialized to attract leukocytes, called chemokines, has led to a renewed interest among reproductive biologists concerning the importance of leukocyte trafficking within the ovary. This mini-review focuses primarily on recent advances relative to chemokine expression and leukocyte recruitment during the periovulatory period, luteinization, and during regression of the corpus luteum.
Classification of chemokines
Chemokines are small molecular weight peptides responsible for adhesion, activation, and chemotaxis of leukocytes [21]. Chemokines are structurally related, possessing a pattern of conserved cysteine residues near the amino-terminal domain. It is the position of these cysteine residues that is the basis for the classification of chemokines into four families (see Table 1). The -CXC-, or alpha chemokine family, has one amino acid (X) separating two of four conserved cysteine residues. A well-characterized chemokine of this family is interleukin-8 (IL-8), which is often expressed by endothelial cells to attract neutrophils. Conversely, the -CC-, or beta family of chemokines has two adjacent cysteine residues. A representative chemokine of this family is monocyte chemoattractant protein-1 (MCP-1), a potent chemotactic molecule that elicits monocyte and T-lymphocyte recruitment [22].
Two relatively new chemokine families have been identified, the -C- family and -CX3C-family. Lymphotactin, a member of the -C-chemokine family, has only one conserved cysteine residue and predominantly attracts lymphocytes. The -CX3C-chemokine, fractalkine, has three amino acids separating two of four cysteines and attracts natural killer cells. Interestingly, fractalkine is a membrane-bound protein that may be cleaved, leaving a functional adhesion molecule and releasing the soluble chemokine [23].
Chemokines activate G protein-mediated signal transduction cascades by signaling through seven-transmembrane receptors [24, 25]. Chemokine receptor families are generally categorized according to their corresponding ligand family (i.e., CXCR, CCR, XCR and CX3CR receptors correspond with -CXC-, -CC-, -C-, and -CX3C-chemokines, respectively; see Table 1). Although chemokine-receptor interactions are specific within families, many chemokines bind to more than one type of receptor, and most receptors bind several different chemokines (see Table 1). Thus, leukocytes may exhibit varying patterns of chemokine receptors. For example, neutrophils express receptors from the CXCR family, while T-lymphocytes express receptors from both CXCR and CCR families (Table 1). Moreover, resting T-lymphocytes express only a couple of chemokine receptors, whereas activated T-lymphocytes display many. All chemokines have two key regions within their structure that are necessary for interaction with their corresponding receptors (Figure 1). The first is a loop within the peptide backbone stretching between the second and third cysteine residues. This loop region initiates binding to the receptor, allowing then for proper presentation of the second key region, a domain within the amino-terminus (Figure 1). Together, these regions of the chemokine molecule trigger receptor activation [24].
Schematic representation of the four chemokine families. Chemokine families are structurally related peptides possessing a pattern of conserved cysteine residues near the amino-terminal (-NH2) domain. The position of the cysteine residues is the basis for the classification into four families. The -CXC-, or alpha chemokine family, has one amino acid (X) separating two of four conserved cysteine residues. The -CC-, or beta family of chemokines has two adjacent cysteine residues. The -C-chemokine, lymphotactin, has only one conserved cysteine residue. The -CX3C-chemokine, fractalkine, has three amino acids separating two of four cysteines. Regions of chemokine-receptor interaction are also depicted.
Chemokines of the periovulatory period
Leukocyte chemoattractant activity within the ovary was discovered initially in follicular fluid of ovulatory follicles [26–29]. Murdoch and McCormick [3, 30] reported that periovulatory follicles secrete low molecular weight factors, 15–16 amino acids in length, capable of stimulating leukocyte migration in vitro. Of particular interest in these studies was the finding that subsets of leukocytes migrated in a temporal manner. That is, neutrophils and eosinophils were attracted to conditioned medium from follicular tissue obtained 24 and 36 hours after the LH surge; whereas monocytes migrated only in response to tissues from the 36-hour time point (approximately 12 hours after the occurrence of ovulation). Basophils and lymphocytes did not exhibit chemotaxis. A similar pattern of neutrophilic and/or eosinophilic chemotaxis at ovulation, followed by monocyte-macrophage chemotaxis during luteinization, occurs in other mammalian species, including humans [8, 10, 31–34]. Neutrophilic chemokines, interleukin-8 (IL-8) and growth related oncogene (GRO), and eosinophilic chemokines, eotaxin and RANTES (regulated upon activation, normal T-cell expressed and secreted) are all expressed by ovulatory follicles [35–44]. Similarly, monocyte chemoattractant protein-1 (MCP-1), a chemokine specific for monocytes and T-lymphocytes, is expressed during ovulation and the formation of the corpus luteum [42, 45]. Collectively, these observations are consistent with the concept that specific leukocyte subsets are recruited to play a role in the process of ovulation and luteinization.
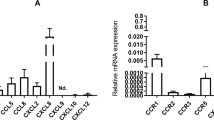
At present, there is limited information available about the hormonal regulation and temporal expression of chemokines during the periovulatory period. Chemokines from all four families are transcribed within follicles of rats following treatment with eCG and hCG [42]. However, this gonadotropin effect on chemokine expression is possibly due to the actions of hCG alone. Ushigoe and co-workers [41] determined that GRO expression in the rat ovary is stimulated by hCG, but not eCG. Similar findings of hCG-stimulated, chemokine expression have been reported in follicles of human and rabbit ovaries [35, 37, 39, 45]. Neutrophilic chemokine expression occurs initially within the thecal layer of the follicle, and then progresses to the granulosal-lutein layer as ovulation becomes imminent [35, 37, 39, 45]. Chemokine expression within follicles probably results from an indirect effect of hCG. Gonadotropins induce the expression of interleukin-1β (IL-1β) and tumor necrosis factor-α (TNFα) in preovulatory follicles [46]. Chemokine expression by thecal and granulosal-lutein cells in culture is stimulated directly by IL-1β and TNFα [35, 37, 39, 45]. Hence, gonadotropin-stimulated chemokine expression within follicles is likely mediated by IL-1β and TNFα effects. Similar actions of gonadotropins and cytokines would be expected to establish the recruitment of eosinophils and monocytes as described in other species [3, 13, 33, 34, 43–45], but the regulatory aspects have not been fully elucidated. Importantly, neutrophilic and eosinophilic chemotaxis into the follicle occurs prior to extravasation of red blood cells and vascular damage [47]. As a consequence of recruitment and activation, neutrophils and eosinophils release proteolytic enzymes, cytokines, and other mediators that may be involved in aspects of ovulation and luteinization. Monocytes most likely engage in similar activities, including the possible expression of IL-8 to attract additional neutrophils [35, 45].
The influence of ovarian steroids on chemokine expression during the periovulatory period is controversial. In two recent studies it was determined that estradiol and progesterone do not affect chemokine (IL-8 & GRO) expression in ovarian tissue [40, 41]. These results are in contrast to work by Arici and co-workers [35], who concluded that progesterone suppresses both basal and IL-1α-stimulated IL-8 expression in cultures of ovarian stromal and granulosal-lutein cells. Considering that many of the chemokines are regulated through the common pathway of NF-kappa B activation [48], it is plausible that ovarian steroids influence chemokine expression through transcriptional regulation. Further work is needed to define the temporal and hormonal regulation of chemokine expression during the periovulatory period, especially the effects of cytokines and ovarian steroids. Moreover, there have been no studies to our knowledge that have investigated whether or not steroidogenic cells of the ovary respond to chemokines directly, or for that matter, possess chemokine receptors. In contrast, there is evidence that Leydig cells of the testis express the -CXC-chemokine, interferon-gamma-inducible protein 10 (IP-10), and that IP-10 inhibits basal and hCG-induced testosterone production [49].
Chemokine expression within the ovulatory follicle could have important physiological implications. Diminished ovulation rates have been reported in animals depleted of neutrophils [39, 50]; whereas the addition of peripheral blood leukocytes to in vitro-perfused rat ovaries increases the number of LH-induced ovulations [6]. In other studies, ovulation rate is unaffected by depletion of leukocytes [51, 52], but development and function of the corpus luteum is impaired [53–55]. Thus, whether chemokines, leukocyte chemotaxis, and leukocytes are indispensable to ovulation remains controversial, but these factors may contribute to aspects of luteinization and the early development of the corpus luteum.
The influence of chemokines on luteinization has not been studied extensively, but may be related to promoting neovascularization, similar to the effects of vascular endothelial growth factor (VEGF) [56–58]. Several -CXC-chemokines, including IL-8 and GRO, have potent angiogenic properties distinct from their ability to attract leukocytes and promote inflammation [59]. Of the -CC-chemokines, MCP-1 has been characterized as a potent angiogenic molecule in corneal angiogenesis and collateral vessel formation [60, 61], but initial evidence indicates that MCP-1 does not promote vascularization of the corpus luteum [61]. In addition to the potential angiogenic effects of chemokines, eosinophils have been recently implicated as a source of VEGF in the developing corpus luteum [54]. Thus, the combined actions of chemokines and leukocytes might encourage neovascularization during luteal development.
The consequences of genetic deletion of chemokines or of similar chemotactic molecules during the folliculo-luteal transition have been examined directly in only a few studies [55, 62–64]. Experiments with genetic knock-out mice have not resolved whether or not the absence of a single chemokine impairs ovulation and luteal function [55, 62–64]. The inherent redundancy of chemokine expression in tissues might be a confounding issue in these studies. Multiple chemokines are often expressed in response to a single stimulus (e.g., the induction of IL-8, GRO, and MCP-1 in follicles by hCG), and might provide for overlapping influences. Such redundant pathways serve to optimize error-free information transmission. However, within this redundancy are elements of specificity, including the hormonal microenvironment (e.g., chemokine concentration) and the temporal pattern and cellular source(s) of chemokine/receptor expression. An emerging view of chemokine action is that distinct networks of cells interact through production of specific chemokines and/or the expression of a highly unique pattern of chemokine receptors [21]. Thus, future work determining the role and physiological implications of chemokines during ovulation and luteinization should consider these emerging concepts.
Chemokines of the regressing corpus luteum
The accumulation of leukocytes, particularly monocytes-macrophages, within the regressing corpus luteum is well-documented, but only recently have investigators considered that this accumulation might result from chemokine expression. Monocyte chemoattractant protein-1 (MCP-1), a potent and monocyte-specific peptide, was the first identified and is currently the most studied chemokine involved in the process of luteal regression. Hosang and co-workers determined that porcine luteal tissue contains mRNA for MCP-1 and -2 [65, 66]. This initial discovery was followed quickly by studies documenting that MCP-1 expression occurs prior to and during luteal regression [67], is induced by luteolytic hormones [68–70], and is accompanied by an accumulation of monocytes-macrophages within the corpus luteum [67]. Similar increases in MCP-1 expression and monocyte-macrophage accumulation during luteal regression have been observed in a variety of mammalian species [15, 71, 72] such that increased MCP-1 expression is now viewed as an indicator of the luteolytic process [19, 20, 73, 74].
Identifying the cellular sources and regulation of MCP-1 within the corpus luteum has been the focus of recent investigations. Endothelial cells of the corpus luteum are clearly a source of MCP-1 [15, 61, 71, 75] and as expected, proinflammatory cytokines such as TNFα and interferon-gamma directly stimulate MCP-1 production [75]. However, progesterone and prostaglandin F2α (PGF) do not affect endothelial cell secretion of MCP-1 [75]. How then does PGF-induced luteal regression in the cow and ewe result in an increase in MCP-1 expression [70, 76]? One possibility is that other cell types within the corpus luteum (e.g., T-lymphocytes, monocytes-macrophages, steroidogenic cells, fibroblasts) respond to PGF and secrete MCP-1. T-lymphocytes are a potential source of MCP-1 within the corpus luteum [77], but the responsiveness of T-lymphocytes to PGF has not been determined. Large steroidogenic luteal cells possess PGF receptors, but their capacity to synthesize MCP-1 is controversial [69, 70, 78]. Another possibility is that endothelial cells of the corpus luteum express MCP-1 in response to factors produced by other PGF-sensitive cells (e.g., steroidogenic cells, immune cells). In addition to cytokines, other factors that provoke MCP-1 expression include oxygen-derived free radicals, Fas-ligand [79, 80], and metabolites of apoptosis. In a very recent study, the onset of luteal cell apoptosis was proposed to activate MCP-1 gene expression in adjacent, non-apoptotic cells of the corpus luteum [78]. Specifically, the process is thought to be Fas-ligand/Fas mediated, in which luteal cells undergoing Fas-ligand induced apoptosis stimulate MCP-1 expression in non-apoptotic cells: MCP-1 then attracts monocytes-macrophages to the corpora lutea containing apoptotic cells, and the apoptotic cells are selectively removed by phagocytosis. These concepts are intriguing, and are completely consistent with the recently hypothesized 'nurturing role' of immune cells in luteal regression (i.e., to diminish an inflammatory condition resulting from dead and dying cells) proposed by Pate and Keyes [19]. Hence, future research should focus on the importance of cell-cell interactions during luteal regression, and the relationships among PGF, Fas, chemokines (especially MCP-1), and apoptosis within the corpus luteum.
Aside from MCP-1, there is very little information available about other chemokines expressed during luteal regression. Endothelial cells of the bovine corpus luteum express RANTES, and this expression is elevated in response to TNFα [81]. The ovine corpus luteum produces chemoattractant(s) for eosinophils following treatment of ewes with PGF [2], but a specific chemokine has not been identified. Eosinophils accumulate within the corpus luteum prior to functional and structural manifestations of regression [2], but are not considered essential to luteolysis despite their capacity to affect tissue structure and inflammatory events [51]. The equine corpus luteum also secretes chemoattractant(s) for leukocytes in late diestrus (before a decline in progesterone secretion), and throughout spontaneous and PGF-induced luteal regression [82]. Recent evidence of chemokine expression and leukocyte accumulation within the corpus luteum prior to regression in these and other studies [15, 67, 77] infers that chemokines might be a contributing cause rather than effect of luteolysis. Moreover, the observation that rescue of the corpus luteum during simulated early pregnancy is associated with a diminished accumulation of luteal macrophages [83] indicates that leukocyte-ovarian cell interactions may be of fundamental importance to a variety of reproductive states. Further examination of chemokine expression and leukocyte accumulation within the corpus luteum during luteal regression and during early pregnancy is warranted.
Conclusion
The discovery and characterization of an ever-growing family of chemokines over the past two decades has prompted renewed interest in leukocyte trafficking during ovarian function. Chemokines are expressed within ovulatory follicles and within the corpus luteum, predominantly during luteal regression. Chemokine expression in these ovarian structures is regulated in part by hormones of reproductive function (e.g., gonadotropins, PGF) and immune response (e.g., TNFα, IL-1β), and is associated with the accumulation of select subsets of leukocytes (e.g., neutrophils, eosinophils, monocytes). Future work should focus further on the physiological implications of chemokines and leukocytes in ovarian function, especially the role of these elements in ovulation, luteal regression, and other aspects of ovarian function that have not received as much attention (i.e., follicular atresia and maternal rescue of the corpus luteum). This will provide important and new insight about relationships shared between reproductive and immune systems.
References
Bukovsky A, Presl J, Krabec Z, Bednarik T: Ovarian function in adult rats treated with antithymocyte serum. Experientia. 1977, 33: 280-281.
Murdoch WJ: Treatment of sheep with prostaglandin F2 alpha enhances production of a luteal chemoattractant for eosinophils. Am J Reprod Immunol Microbiol. 1987, 15: 52-56.
Murdoch WJ, McCormick RJ: Production of low molecular weight chemoattractants for leukocytes by periovulatory ovine follicles. Biol Reprod. 1989, 41: 86-90.
Adashi EY: The potential relevance of cytokines to ovarian physiology: the emerging role of resident ovarian cells of the white blood cell series. Endocr Rev. 1990, 11: 454-464.
Mori T: Immuno-endocrinology of cyclic ovarian function. Am J Reprod Immunol. 1990, 24: 80-89.
Hellberg P, Thomsen P, Janson PO, Brannstrom M: Leukocyte supplementation increases the luteinizing hormone-induced ovulation rate in the in vitro-perfused rat ovary. Biol Reprod. 1991, 44: 791-797.
Lobel BL, Levy E: Enzymic correlates of development, secretory function and regression of follicles and corpora lutea in the bovine ovary. II. Formation, development and involution of corpora lutea. Acta Endocrinologica. 1968, 59: 35-51.
Standaert FE, Zamora CS, Chew BP: Quantitative and qualitative changes in blood leukocytes in the porcine ovary. Am J Reprod Immunol. 1991, 25: 163-168.
Brannstrom M, Giesecke L., Moore IC, Van Den Heuvel CJ, Robertson SA: Leukocyte subpopulations in the rat corpus luteum during pregnancy and pseudopregnancy. Biol Reprod. 1994, 50: 1161-1167.
Brannstrom M, Pascoe V, Norman RJ, McClure N: Localization of leukocyte subsets in the follicle wall and in the corpus luteum throughout the human menstrual cycle. Fertil Steril. 1994, 61: 488-495.
Suzuki T, Sasano H, Takaya R, Fukaya T, Yajima A, Date F, Nagura H: Leukocytes in normal-cycling human ovaries: immunohistochemical distribution and characterization. Hum Reprod. 1998, 13: 2186-2191. 10.1093/humrep/13.8.2186.
Lawler DF, Hopkins J, Watson ED: Immune cell populations in the equine corpus luteum throughout the oestrous cycle and early pregnancy: an immunohistochemical and flow cytometric study. J Reprod Fertil. 1999, 117: 281-290.
Reibiger I, Spanel-Borowski K: Difference in localization of eosinophils and mast cells in the bovine ovary. J Reprod Fertil. 2000, 118: 243-249. 10.1530/reprod/118.2.243.
Ramadan AA, Selim SA, Hassan HM, Wahba MA: Immune regulation of ovarian function in buffaloes (Bubalus bubalus). Theriogenology. 2001, 55: 661-669. 10.1016/S0093-691X(01)00434-4.
Townson DH, O'Connor CL, Pru JK: Expression of monocyte chemoattractant protein-1 and distribution of immune cell populations in the bovine corpus luteum throughout the estrous cycle. Biol Reprod. 2002, 66: 361-366.
Chun SY, Hsueh AJ: Paracrine mechanisms of ovarian follicle apoptosis. J Reprod Immunol. 1998, 39: 63-75. 10.1016/S0165-0378(98)00013-8.
Meidan R, Milvae RA, Weiss S, Levy N, Friedman A: Intraovarian regulation of luteolysis. J Reprod Fertil Suppl. 1999, 54: 217-228.
Asselin E, Xiao CW, Wang YF, Tsang BK: Mammalian follicular development and atresia: role of apoptosis. Biol Signals Recept. 2000, 9: 87-95. 10.1159/000014627.
Pate JL, Landis Keyes P: Immune cells in the corpus luteum: friends or foes?. Reproduction. 2001, 122: 665-676. 10.1530/reprod/122.5.665.
Webb R, Woad KJ, Armstrong DG: Corpus luteum (CL) function: local control mechanisms. Domest Anim Endocrinol. 2002, 23: 277-285. 10.1016/S0739-7240(02)00163-7.
Rossi D, Zlotnik A: The biology of chemokines and their receptors. Annu Rev Immunol. 2000, 18: 217-242. 10.1146/annurev.immunol.18.1.217.
Garcia-Velasco JA, Arici A: Chemokines and human reproduction. Fertil Steril. 1999, 71: 983-993. 10.1016/S0015-0282(99)00120-X.
Ludwig A, Berkhout T, Moores K, Groot P, Chapman G: Fractalkine is expressed by smooth muscle cells in response to IFN-gamma and TNF-alpha and is modulated by metalloproteinase activity. J Immunol. 2002, 168: 604-612.
Baggiolini M: Chemokines and leukocyte traffic. Nature. 1998, 392: 565-568. 10.1038/33340.
Nelson PJ, Krensky AM: Chemokines, lymphocytes and viruses: what goes around, comes around. Curr Opin Immunol. 1998, 10: 265-270. 10.1016/S0952-7915(98)80164-7.
Herriot DM, Warnes GM, Kerin JF: Pregnancy-related chemotactic activity of human follicular fluid. Fertil Steril. 1986, 45: 196-201.
Seow WK, Thong YH, Waters MJ, Walters M, Cummins JM: Isolation of a chemotactic protein for neutrophils from human ovarian follicular fluid. Int Arch Allergy Appl Immunol. 1988, 86: 331-336.
Harkin DG, Bignold LP, Herriot-Warnes DM, Kirby CA: Chemotaxis of polymorphonuclear leukocytes towards human pre-ovulatory follicular fluid and serum using a 'sparse-pore' polycarbonate filtration membrane. J Reprod Immunol. 1994, 27: 151-155. 10.1016/0165-0378(94)90030-2.
Sirotkin AV, Luck MR: Potential leukocyte attractants in the bovine peri-ovulatory ovary. Reprod Nutr Dev. 1995, 35: 675-683.
Murdoch WJ, McCormick RJ: Sequence analysis of leukocyte chemoattractant peptides secreted by periovulatory ovine follicles. Biochem Biophys Res Commun. 1992, 184: 848-852.
Gerdes U, Gafvels M, Bergh A, Cajander S: Localized increases in ovarian vascular permeability and leucocyte accumulation after induced ovulation in rabbits. J Reprod Fertil. 1992, 95: 539-550.
Brannstrom M, Mayrhofer G, Robertson SA: Localization of leukocyte subsets in the rat ovary during the periovulatory period. Biol Reprod. 1993, 48: 277-286.
Kerban A, Dore M, Sirois J: Characterization of cellular and vascular changes in equine follicles during hCG-induced ovulation. J Reprod Fertil. 1999, 117: 115-123.
Rohm F, Spanel-Borowski K, Eichler W, Aust G: Correlation between expression of selectins and migration of eosinophils into the bovine ovary during the periovulatory period. Cell Tissue Res. 2002, 309: 313-322. 10.1007/s00441-002-0602-3.
Arici A, Oral E, Bukulmez O, Buradagunta S, Engin O, Olive DL: Interleukin-8 expression and modulation in human preovulatory follicles and ovarian cells. Endocrinology. 1996, 137: 3762-3769. 10.1210/en.137.9.3762.
Runesson E, Bostrom EK, Janson PO, Brannstrom M: The human preovulatory follicle is a source of the chemotactic cytokine interleukin-8. Mol Hum Reprod. 1996, 2: 245-250.
Oral E, Seli E, Bahtiyar MO, Jones EE, Arici A: Growth-regulated alpha expression in human preovulatory follicles and ovarian cells. Am J Reprod Immunol. 1997, 38: 19-25.
Karstrom-Encrantz L, Runesson E, Bostrom EK, Brannstrom M: Selective presence of the chemokine growth-regulated oncogene alpha (GROalpha) in the human follicle and secretion from cultured granulosa-lutein cells at ovulation. Mol Hum Reprod. 1998, 4: 1077-1083. 10.1093/molehr/4.11.1077.
Ujioka T, Matsukawa A, Tanaka N, Matsuura K, Yoshinaga M, Okamura H: Interleukin-8 as an essential factor in the human chorionic gonadotropin-induced rabbit ovulatory process: interleukin-8 induces neutrophil accumulation and activation in ovulation. Biol Reprod. 1998, 58: 526-530.
Runesson E, Ivarsson K, Janson PO, Brannstrom M: Gonadotropin- and cytokine-regulated expression of the chemokine interleukin 8 in the human preovulatory follicle of the menstrual cycle. J Clin Endocrinol Metab. 2000, 85: 4387-4395. 10.1210/jc.85.11.4387.
Ushigoe K, Irahara M, Fukumochi M, Kamada M, Aono T: Production and regulation of cytokine-induced neutrophil chemoattractant in rat ovulation. Biol Reprod. 2000, 63: 121-126.
Wong KH, Negishi H, Adashi EY: Expression, hormonal regulation, and cyclic variation of chemokines in the rat ovary: key determinants of the intraovarian residence of representatives of the white blood cell series. Endocrinology. 2002, 143: 784-791. 10.1210/en.143.3.784.
Aust G, Brylla E, Lehmann I, Kiessling S, Spanel-Borowski K: Cloning of bovine RANTES mRNA and its expression and regulation in ovaries in the periovulatory period. FEBS Lett. 1999, 463: 160-164. 10.1016/S0014-5793(99)01599-9.
Aust G, Simchen C, Heider U, Hmeidan FA, Blumenauer V, Spanel-Borowski K: Eosinophils in the human corpus luteum: the role of RANTES and eotaxin in eosinophil attraction into periovulatory structures. Mol Hum Reprod. 2000, 6: 1085-1091. 10.1093/molehr/6.12.1085.
Arici A, Oral E, Bukulmez O, Buradagunta S, Bahtiyar O, Jones EE: Monocyte chemotactic protein-1 expression in human preovulatory follicles and ovarian cells. J Reprod Immunol. 1997, 32: 201-219. 10.1016/S0165-0378(97)82476-X.
Terranova PF, Rice VM: Review: cytokine involvement in ovarian processes. Am J Reprod Immunol. 1997, 37: 50-63.
Cavender JL, Murdoch WJ: Morphological studies of the microcirculatory system of periovulatory ovine follicles. Biol Reprod. 1988, 39: 989-997.
Barnes PJ, Karin M: Nuclear factor-kappaB: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med. 1997, 336: 1066-1071. 10.1056/NEJM199704103361506.
Hu J, You S, Li W, Wang D, Nagpal ML, Mi Y, Liang P, Lin T: Expression and regulation of interferon-gamma-inducible protein 10 gene in rat Leydig cells. Endocrinology. 1998, 139: 3637-3645. 10.1210/en.139.8.3637.
Brannstrom M, Bonello N, Norman RJ, Robertson SA: Reduction of ovulation rate in the rat by administration of a neutrophil-depleting monoclonal antibody. J Reprod Immunol. 1995, 29: 265-270. 10.1016/0165-0378(95)00941-D.
Murdoch WJ, Steadman LE: Investigations concerning the relationship of ovarian eosinophilia to ovulation and luteal function in the sheep. Am J Reprod Immunol. 1991, 25: 81-87.
Chun SY, Daphna-Iken D, Calman D, Tsafriri A: Severe leukocyte depletion does not affect follicular rupture in the rat. Biol Reprod. 1993, 48: 905-909.
Murdoch WJ, McCormick RJ: Mechanisms and physiological implications of leucocyte chemoattraction into periovulatory ovine follicles. J Reprod Fertil. 1993, 97: 375-380.
Murdoch WJ, Van Kirk EA: Aetiology of attenuated luteal development in prednisolone-induced eosinopenic ewes. Reprod Fertil Dev. 2000, 12: 127-132.
Jasper MJ, Robertson SA, Van der Hoek KH, Bonello N, Brannstrom M, Norman RJ: Characterization of ovarian function in granulocyte-macrophage colony-stimulating factor-deficient mice. Biol Reprod. 2000, 62: 704-713.
Ferrara N, Chen H, Davis-Smyth T, Gerber HP, Nguyen TN, Peers D, Chisholm V, Hillan KJ, Schwall RH: Vascular endothelial growth factor is essential for corpus luteum angiogenesis. Nat Med. 1998, 4: 336-340.
Goede V, Schmidt T, Kimmina S, Kozian D, Augustin HG: Analysis of blood vessel maturation processes during cyclic ovarian angiogenesis. Lab Invest. 1998, 78: 1385-1394.
Reynolds LP, Grazul-Bilska AT, Redmer DA: Angiogenesis in the corpus luteum. Endocrine. 2000, 12: 1-9. 10.1385/ENDO:12:1:1.
Belperio JA, Keane MP, Arenberg DA, Addison CL, Ehlert JE, Burdick MD, Strieter RM: CXC chemokines in angiogenesis. J Leukoc Biol. 2000, 68: 1-8.
Ito WD, Arras M, Winkler B, Scholz D, Schaper J, Schaper W: Monocyte chemotactic protein-1 increases collateral and peripheral conductance after femoral artery occlusion. Circ Res. 1997, 80: 829-37.
Goede V, Brogelli L, Ziche M, Augustin HG: Induction of inflammatory angiogenesis by monocyte chemoattractant protein-1. Int J Cancer. 1999, 82: 765-770. 10.1002/(SICI)1097-0215(19990827)82:5<765::AID-IJC23>3.0.CO;2-F.
Cohen PE, Zhu L, Pollard JW: Absence of colony stimulating factor-1 in osteopetrotic (csfmop/csfmop) mice disrupts estrous cycles and ovulation. Biol Reprod. 1997, 56: 110-118.
Robertson SA, Mau VJ, Young IG, Matthaei KI: Uterine eosinophils and reproductive performance in interleukin 5-deficient mice. J Reprod Fertil. 2000, 120: 423-432. 10.1530/reprod/120.2.423.
Gouon-Evans V, Pollard JW: Eotaxin is required for eosinophil homing into the stroma of the pubertal and cycling uterus. Endocrinology. 2001, 142: 4515-4521. 10.1210/en.142.10.4515.
Hosang K, Knoke I, Klaudiny J, Wempe F, Wuttke W, Scheit KH: Porcine luteal cells express monocyte chemoattractant protein-2 (MCP-2): analysis by cDNA cloning and northern analysis. Biochem Biophys Res Commun. 1994, 205: 148-153. 10.1006/bbrc.1994.2642.
Hosang K, Knoke I, Klaudiny J, Wempe F, Wuttke W, Scheit KH: Porcine luteal cells express monocyte chemoattractant protein-1 (MCP-1): analysis by polymerase chain reaction and cDNA cloning. Biochem Biophys Res Commun. 1994, 199: 962-968. 10.1006/bbrc.1994.1323.
Townson DH, Warren JS, Flory CM, Naftalin DM, Keyes PL: Expression of monocyte chemoattractant protein-1 in the corpus luteum of the rat. Biol Reprod. 1996, 54: 513-520.
Bowen JM, Keyes PL, Warren JS, Townson DH: Prolactin-induced regression of the rat corpus luteum: expression of monocyte chemoattractant protein-1 and invasion of macrophages. Biol Reprod. 1996, 54: 1120-1127.
Tsai SJ, Juengel JL, Wiltbank MC: Hormonal regulation of monocyte chemoattractant protein-1 messenger ribonucleic acid expression in corpora lutea. Endocrinology. 1997, 138: 4517-4520. 10.1210/en.138.10.4517.
Haworth JD, Rollyson MK, Silva P, McIntush EW, Niswender GD: Messenger ribonucleic acid encoding monocyte chemoattractant protein-1 is expressed by the ovine corpus luteum in response to prostaglandin F2alpha. Biol Reprod. 1998, 58: 169-174.
Senturk LM, Seli E, Gutierrez LS, Mor G, Zeyneloglu HB, Arici A: Monocyte chemotactic protein-1 expression in human corpus luteum. Mol Hum Reprod. 1999, 5: 697-702. 10.1093/molehr/5.8.697.
Krusche CA, Vloet TD, Herrler A, Black S, Beier HM: Functional and structural regression of the rabbit corpus luteum is associated with altered luteal immune cell phenotypes and cytokine expression patterns. Histochem Cell Biol. 2002, 118: 479-489.
Penny LA: Monocyte chemoattractant protein 1 in luteolysis. Rev Reprod. 2000, 5: 63-66. 10.1530/revreprod/5.2.63.
Davis JS, Rueda BR: The corpus luteum: an ovarian structure with maternal instincts and suicidal tendencies. Front Biosci. 2002, 7: d1949-1978.
Cavicchio VA, Pru JK, Davis BS, Davis JS, Rueda BR, Townson DH: Secretion of monocyte chemoattractant protein-1 by endothelial cells of the bovine corpus luteum: regulation by cytokines but not prostaglandin F2alpha. Endocrinology. 2002, 143: 3582-3589. 10.1210/en.2002-220388.
Tsai SJ, Kot K, Ginther OJ, Wiltbank MC: Temporal gene expression in bovine corpora lutea after treatment with PGF2alpha based on serial biopsies in vivo. Reproduction. 2001, 121: 905-913. 10.1530/reprod/121.6.905.
Penny LA, Armstrong DG, Baxter G, Hogg C, Kindahl H, Bramley T, Watson ED, Webb R: Expression of monocyte chemoattractant protein-1 in the bovine corpus luteum around the time of natural luteolysis. Biol Reprod. 1998, 59: 1464-1469.
Nagaosa K, Shiratsuchi A, Nakanishi Y: Determination of cell type specificity and estrous cycle dependency of monocyte chemoattractant protein-1 expression in corpora lutea of normally cycling rats in relation to apoptosis and monocyte/macrophage accumulation. Biol Reprod. 2002, 67: 1502-1508.
Choi C, Xu X, Oh JW, Lee SJ, Gillespie GY, Park H, Jo H, Benveniste EN: Fas-induced expression of chemokines in human glioma cells: involvement of extracellular signal-regulated kinase 1/2 and p38 mitogen-activated protein kinase. Cancer Res. 2001, 61: 3084-91.
Yamaoka-Tojo M, Yamaguchi S, Nitobe J, Abe S, Inoue S, Nozaki N, Okuyama M, Sata M, Kubota I, Nakamura H, Tomoike H: Dual response to Fas ligation in human endothelial cells: apoptosis and induction of chemokines, interleukin-8 and monocyte chemoattractant protein-1. Coron Artery Dis. 2003, 14: 89-94. 10.1097/00019501-200302000-00010.
Lehmann I, Brylla E, Sittig D, Spanel-Borowski K, Aust G: Microvascular endothelial cells differ in their basal and tumour necrosis factor-alpha-regulated expression of adhesion molecules and cytokines. J Vasc Res. 2000, 37: 408-16. 10.1159/000025757.
Lawler DF, Brazil TJ, Dagleish MP, Watson ED: Chemoattractant properties of conditioned medium from equine corpora lutea collected at various stages of the oestrous cycle. Equine Vet J. 2002, 34: 279-282.
Duncan WC, Rodger FE, Illingworth PJ: The human corpus luteum: reduction in macrophages during simulated maternal recognition of pregnancy. Hum Reprod. 1998, 13: 2435-2442. 10.1093/humrep/13.9.2435.
Acknowledgements
This manuscript is scientific contribution number 2177 from the New Hampshire Agricultural Experiment Station. The work was supported in part by USDA Grants 97-35208-4705 & 2002-35203-12257.
Author information
Authors and Affiliations
Corresponding author
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Townson, D.H., Liptak, A.R. Chemokines in the corpus luteum: Implications of leukocyte chemotaxis. Reprod Biol Endocrinol 1, 94 (2003). https://doi.org/10.1186/1477-7827-1-94
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7827-1-94