Abstract
Background
The nature of the relationship between Helicobacter pylori and reflux esophagitis (RE) is not fully understood. In addition, the effect of H. pylori eradication on RE and gastroesophageal reflux disease (GERD) is unclear. This study was designed to investigate the relationship between H. pylori infection and the grade of GERD in patients with reflux symptoms.
Methods
Between January 2010 and July 2013, 184 consecutive patients with daily reflux symptoms for at least one year were evaluated at the ambulatory for functional esophageal disease, Tor Vergata University Hospital, Rome, Italy. All patients underwent a pretreatment evaluation, which included anamnesis, clinical examination, Esophagogastroduodenoscopy (EGDS) with biopsy, esophageal manometry and 24-hour pH-metry. All statistical elaborations were obtained using Statigraphies 5 plus for Window XP.
Results
There was no statistical difference regarding Lower Esophageal Sphincter (LES) pressure between patients who were H. pylori-positive and H. Pylori-negative (19.2 ± 9.5 (range: 3.7 to 46.2) and 19.7 ± 11.0 (range: 2.6 to 61), respectively). Further, no significant difference was evidenced in esophageal wave length (mean value: 3.1 seconds in H. pylori-negative patients versus 3.2 seconds in H. pylori-positive patients) or in esophageal wave height (mean value: 72.2 ± 39.3 in H. pylori-negative patients versus 67.7 ± 28.4 in H. pylori-positive patients). We observed that hiatal hernia (P = 0.01), LES opening (P = 0.05), esophageal wave length (P = 0.01) and pathological reflux number (P = 0.05) were significantly related to the presence of esophagitis. However, H. pylori infection was not significantly related to the presence of reflux esophagitis.
Conclusions
Our clinical, endoscopic, manometric and pH-metric data shows no significant role of H. pylori infection in the development of GERD or in the pathogenesis of reflux esophagitis. However, current data do not provide sufficient evidence to define this relationship and further prospective large studies are needed.
Similar content being viewed by others
Background
Helicobacter pylori (HP) infection plays a major role in the pathogenesis of peptic ulcer disease, chronic gastritis, gastric mucosa-associated lymphoid tissue lymphoma (MALToma) and the development of gastric cancer. However, its role in reflux-induced esophageal injury (reflux esophagitis (RE)) and gastroesophageal reflux disease without esophagitis (GERD) is not fully understood. In addition, the effect of H. pylori eradication on RE or GERD is unclear. Several reports have shown an association of H. pylori eradication with the development of RE or GERD symptoms [1–3]. However, contradictory results have been reported, and sometimes a beneficial effect of H. pylori eradication on GERD has been observed [4–6].
Despite the results of these studies, it is conceivable that H. pylori could contribute to esophagitis in GERD through any of at least three potential mechanisms: 1) H. pylori infection might cause a predisposition to GERD by increasing gastric acid secretion, 2) H. pylori might cause esophageal damage by directly infecting the gastric-type columnar epithelium that can line the distal esophagus normally or as part of Barrett's esophagus or 3) H. pylori might cause esophageal damage indirectly through the action of noxious substances that are secreted by the organism into the refluxed gastric juice [7].
Colonization of gastric mucosa by H. pylori may result in hypochlorhydria in patients with diffuse gastritis and gastric atrophy and who seem to be at less risk of developing GERD [8]. Therefore, association between H. pylori infection and development of either hypochlorhydria or hyperacid secretion depends on the inflammatory response of the gastric mucosa. Thus, the effect of H. pylori infection on the development of GERD is contradictory and is an intricate relationship [8]. This study was designed to investigate the relationship between H. pylori infection and the grade of GERD in patients with reflux symptoms.
Methods
Between January 2010 and July 2013, 184 consecutive patients with daily reflux symptoms for at least one year were evaluated at the ambulatory for functional esophageal disease, Tor Vergata University Hospital, Rome, Italy, and were included in this prospective study. The study had been approved by the Institutional Committee of the Tor Vergata University of Rome.
We classified the symptoms of the patients as did Patti et al. [9]; a patient-estimated scale ranging from 0 (no symptom) to 4 (disabling symptom). Swallowing status was graded as follows: excellent (no dysphagia), good (occasional dysphagia), fair (frequent dysphagia requiring dietary adjustments) or poor (severe dysphagia preventing the ingestion of solid food).
Exclusion criteria were: previous therapy to eradicate H. pylori, concomitant assumption of aspirin and non-steroidal antiinflammatory drugs or previous surgical procedures on the digestive tract. All patients underwent pretreatment evaluation, which included anamnesis, clinical examination, EGDS with biopsy, esophageal manometry and 24 hours pH-metry. Symptoms (heartburn, pain and regurgitation) were assessed by patients' visits. Outpatient manometry and pH studies were performed using a conventional protocol.
The study has not evaluated the degree of GERD as we are only interested in the correlation between RE and GERD. Kusano et al. [10] have shown that the Frequency Scale for Symptoms of GERD (FSSG) is useful only to evaluate therapeutic efficacy in GERD patients during the follow-up period without repeated endoscopy.
Esophageal manometry
All subjects presented for a manometry after fasting for a minimum of eight hours. Medications known to inhibit or affect esophageal motility (nitrates, metoclopramide hydrochloride or calcium channel-blocking agents) were discontinued five days before manometry or 24-hour pH monitoring. A six-way perfusion water catheter (three radial and three spaced at 1-cm intervals) was used for all studies. The catheter was calibrated from 0 to 50 mmHg immediately before use (Medtronic Polygram Net™ version 4.01. Tonsbakken, Denmark).
An esophageal manometry was performed in order to define the position, extension, pressure of Lower Esophageal Sphincter (LES) (resting pressure and relaxation), amplitude, duration and velocity of esophageal peristaltic. Esophageal motility and gastroesophageal junction coordination were evaluated using 5 ml of room temperature water in a sequence of 10 swallows. Double swallows and swallows including pressure artefacts associated with coughing or belching were not counted in the 10 swallows.
24-hour esophageal pH monitoring
During the study the patients consumed an unrestricted diet and took no medications that could interfere with the results. Esophageal pH monitoring was conducted using an antimony pH catheter with external or internal reference (AccuView pH, Sierra Scientific Instruments. Yoqneam, Israel). The sensor was positioned 5 cm above the LES. Continuous pH recording was performed for 24 hours.
The DeMeester score [11] was used to calculate the following distal pH variables: percentage of total time that pH was less than 4, percentage of supine time that pH was less than 4, percentage of upright time that pH was less than 4, longest reflux event, number of reflux events longer than five minutes, and number of reflux episodes in 24 hours. A DeMeester score of greater than 14.72 was considered abnormal.
In patients with an abnormal reflux score (reference reflux score: 14.7), tracings were analyzed to distinguish between false reflux (due to stasis and fermentation) and true reflux [8]. When the clinical picture was ambiguous (a patient with good response to Proton Pump Inhibitors (PPIs) and esophagitis, or a normal but borderline reflux score), the pH monitoring study was repeated after three weeks.
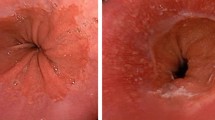
Endoscopic procedure
All study subjects underwent upper gastrointestinal endoscopic examinations. The endoscopic findings of RE in the lower esophagus were classified according to the Savary-Miller classification [12], based on the longest length of the mucosal break and confluence of erosions. Esophagitis was graded by endoscopy: grade 0, no lesions; grade 1, esophagitis was defined as the presence of single or isolated erosion on one mucosal fold; grade 2, non-circumferential erosions on more than one mucosal fold with or without confluence; grade 3, circumferential erosions that may be confluent; grade 4, ulcer, stricture, or esophageal shortening and Barrett's epithelium.
A hiatal hernia was endoscopically defined as a distance from the esophagogastric junction to the diaphragmatic impingement of more than 1 cm. The esophagogastric junction was defined as the proximal margin of the gastric mucosal fold [3]. Barrett's esophagus has been defined as the presence of squamo-columnar metaplasia localized at least 3 cm above the esophagus-gastric junction; two to three samples of the lower esophagus (last 3 cm) were obtained [12]. An endoscopic biopsy both of the gastric body and the antrum was performed in order to diagnose H. pylori infection and to obtain histological evaluation of the mucosa. H. pylori infection was diagnosed by the color-coded biopsy test (CCBT); we did not choose the stool antigen test (SAT) because CCBT is more feasible, faster to perform and executable at the time of the endoscopic procedure. The specimens were preserved in formaldehyde solution (10%) for histopathologic evaluation.
Statistical analysis
All statistical elaborations were obtained by using Statigraphies 5 plus for Window XP (Statsoft; Tulsa, Oklahoma, United States). Results are expressed as mean values and standard deviation (SD). Quantitative variables between the two groups (H. pylori-positive and H. pylori-negative patients) were compared using the Student's t-test; qualitative parameters were compared between the two groups using chi-squared test. Results were considered statistically significant at P <0.05.
Results
The present study included 184 patients (73 males and 111 females) with a mean age of 51.5 ± 15.2 years (range: 23 to 89). The baseline characteristics of the two groups are shown in Table 1.
All patients suffered from daily reflux symptoms for at least one year, there was no statistical difference regarding the severity of symptoms and symptoms score as given by the patients between the two groups (Table 2).
H. pylori infection was diagnosed in 85 patients (46.2%; 32 males and 53 females), while 99 patients (53.8%; 41 males and 58 females) were H. pylori-negative. Patients with and without H. pylori infection were statistically compared. There were no significant differences between the two groups regarding age, gender and presentation of symptoms. Hiatal hernia was found in 122 out of 184 patients (66.3%); 31 of which were H. pylori-positive (25.4%) and 91 were H. pylori-negative (74.6%), this data was statistically significant (P <0.0001). Out of these 122 patients with hiatal hernia, 40 (32.8%) suffered from RE, and in this group H. pylori-infection was diagnosed in 10 patients (25%), therefore in 82 patients (67.2%) with GERD and no RE, H. pylori-infection was present in 21 cases (25.6%). The incidence of hiatal hernia between the group with RE (40 patients) and the group without RE (82 patients) was significant (P <0.0001).
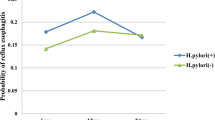
According to the Savary-Miller classification [9], 132 patients (71.7%) were graded 0 and had GERD only, and in 52 out of 184 patients (28.3%) reflux esophagitis was evidenced, of which 18 patients were graded 1 to 3 (four H. pylori-positive patients and 14 H. pylori-negative) and 34 patients were graded 4 (11 H. pylori-positive patients and 23 H. pylori-negative); two of these cases were found to have Barrett’s esophagus, and both were H. pylori-negative. Impairment of esophageal motility and presence of waves dropped and not forwarded was detected at manometry in 140 patients out of 184 (76%). H. pylori was present in 33 of these (23.6%), while 107 were H. pylori-negative (76.4%).
There was no statistical difference regarding LES pressure between patients who were H. pylori-positive and H. pylori-negative (19.2 ± 9.5 (range: 3.7 to 46.2) and 19.7 ± 11.0 (range: 2.6 to 61), respectively). Further, significant difference was not evidenced in either esophageal wave length (mean value: 3.1 seconds in H. pylori-negative patients versus 3.2 seconds in H. pylori-positive) nor in esophageal wave height (mean value: 72.2 ± 39.3 in H. pylori-negative patients versus 67.7 ± 28.4 in H. pylori-positive), (Table 3).
The pH-metric parameters, that is, reflux episodes, pathological reflux episodes (refluxes with pH <4 that last over five minutes) and extent of esophageal acid exposure, were similar in both groups (Table 4).
Out of 146 patients, 95 (51.6%) had pathological values on the DeMeester scale; 22 patients were H. pylori-positive (23.1%) and 73 were H. pylori-negative (76.8%). The mean value of the DeMeester score was 35.9 ± 56.7 in H. pylori-positive patients versus 33.3 ± 48 in H. pylori-negative, and this difference was not significant.
In addition, to investigate the influence of the mentioned clinical, endoscopic and functional variables on reflux esophagitis, a univariate analysis of clinical, endoscopic and functional parameters was performed, considering the presence of esophagitis as independent variable. We observed that hiatal hernia (P = 0.01), LES opening (P = 0.05), esophageal wave length (P = 0.01) and pathological reflux number (P = 0.05) were significantly related to the presence of esophagitis. However, H. pylori infection was not significantly related to the presence of reflux esophagitis.
Discussion
The incidence of H. pylori infection in patients with GERD varies widely in literature from 30 to 90%, and is approximately of 35% in most series [12]. This heterogeneity between the studies may be due to the geographical location of the studies due to the difference in the prevalence of H. pylori in the Far East, North America and Western Europe [8]. It was suggested that H. pylori could contribute to GERD through different mechanisms: the development of antral gastritis which increases acid production, a decrease of LES pressure and impairment of gastric filling [10]. Nevertheless, the decreasing prevalence of H. pylori infection and related diseases (ulcer disease and gastric cancer) in Western countries has been paralleled by an increased incidence of gastroesophageal reflux and related complications. These epidemiological data do not support a causative role of H. pylori for reflux disease, but suggest a negative association [11].
Esophageal H. pylori infection is uncommon in patients with Barrett’s IM, dysplasia, or adenocarcinoma, and may be restricted to the non-intestinalized columnar epithelium. Gastric H. pylori infection may have a protective effect for the development of Barrett’s esophagus [13]; this data was also found in our study, although the small sample size should be emphasized. Other authors have even found a lower prevalence of H. pylori infection in patients with reflux symptoms and have suggested a 'protective' role of H. pylori infection against the development of esophageal diseases [14, 15]. Smout believed that pre-existing LES dysfunction and gastritis, and susceptibility to reflux, increased by a latent reflux, are probably causative factors contributing to esophageal diseases, rather than H. pylori infection [14]. Another possible explanation for the heterogeneous results regarding the relationship between GERD and H. pylori may be related to the variable effect of H. pylori on gastric acid.
According to Gisbert et al. [16], who found no influence of H. pylori infection either on pH-metric data or on endoscopic findings, in our trial out of 184 GERD patients, 46% were H. pylori-infected while 54% were H. pylori-negative; in addition we found no statistical difference regarding presence and severity of reflux esophagitis between patients with and without H. pylori infection. Contrary to our study, most trials base the correlation between H. pylori infection and GERD only on endoscopic observations; the endoscopic pattern of GERD patients is often normal, and 24-hour pH-monitoring revealed a high diagnostic accuracy for GERD [17, 18]. Actually, even if the role of acid secretion in esophageal lesions is undeniable, it does not seem increased in GERD patients [19, 20]. In the present study, we found no correlation between H. pylori infection and pH-metric data, and the mean value of the DeMeester score was similar in H. pylori-positive and -negative patients as found by Oberg et al. [21]. Further, the total time of acidification was similar in both groups as outlined by Oberg et al. [21], who did not find any correlation between H. pylori infection and esophageal exposure to acid, detected by 24 hours pH-metry, in patients with erosive esophagitis or Barrett's esophagus. Schwizer et al. [22] studied 70 patients with GERD treated with lansoprazole associated with clarithromycin and amoxicillin in patients with H. pylori infection. There was no difference in 24-hour pH values before and after H. pylori eradication, suggesting that H. pylori eradication did not affect distal esophageal acid exposure.
In our study, we found an unusual prevalence of hiatal hernia in contrast with some authors [23, 24]. We are not able to explain this data, however one theory is that it may be due to the excessive attention with which this condition was searched for. The incidence of patients with hiatal hernia and no H. pylori infection was higher than patients with H. pylori infection and hiatal hernia (91 versus 31; P <0.0001). Moreover, according to a past study [23] and this present one, the incidence of hiatal hernia did not associate with RE (P <0.0001). We found significant correlation between H. pylori infection and hiatal hernia, considered by some authors as a supporting element of GERD, and significantly associated with the development of esophagitis [23, 24].
Virulent strains of H. pylori, including those with a cytotoxin-associated gene named cagA+, have been reported to be associated with significant gastric inflammation [11]. H. pylori gastritis is accompanied by the release of nitric oxide, cytokines and prostaglandins that may impair afferent nerve function, reduce LES pressure and damage esophageal mucosa [25, 26]. However, in contrast to other authors [27, 28], in our trial LES pressure was similar in patients with and without H. pylori infection. Further, out of 184 GERD patients only 26% had LES pressure <14 mmHg, and LES opening (P = 0.05) and esophageal wave length (P = 0.01) were significantly related to esophagitis.
The relationship between H. pylori infection and gastric adenocarcinoma is also controversial. Some authors suggest an increased risk of gastric atrophy in H. pylori-positive patients treated with long-term proton pump inhibitor therapy. In a small subset of H. pylori-infected patients, chronic gastritis may lead to gastric atrophy and intestinal metaplasia, a potential precursor for gastric adenocarcinoma [29].
In a recent randomized controlled trial by Kuipers et al. [30], none of the H. pylori-positive GERD patients treated with anti-reflux surgery developed gastric atrophy, compared to 31% of patients treated with proton pump inhibitor therapy for an average of five years. Differently, in a long-term trial of GERD patients treated for years with omeprazole, there was an increase both in the severity of corpus gastritis and in gastric atrophy in H. pylori-positive patients [31]. Amongst the H. pylori-infected patients, atrophy was detected in 12% at baseline and 39% on follow-up.
Contrarily, it has been suggested that H. pylori cagA+ may potentially protect against complications of GERD, such as Barrett's esophagus and dysplasia and adenocarcinoma [32, 33]. The H. pylori infection in patients with Barrett's esophagus has been reported in 12 to 60% cases [34–37]. A recent meta-analysis presented at Digestive Disease Week 2002 reported a negative association between the prevalence of H. pylori and cagA + H. pylori and reflux disease, Barrett's esophagus and esophageal adenocarcinoma [38].
Conclusions
The exact association between H. pylori and reflux disease continues to be debated. Our clinical, endoscopic manometric and pH-metric data show a significant role of H. pylori infection neither in the development of GERD nor in the pathogenesis of reflux esophagitis. However, there are the works in the literature that analyze all the variables we considered. Nevertheless, current data do not provide sufficient evidence to define the relationship between H. pylori and GERD. We are fully in agreement with Wu et al. [19] in stating that a comparative study of H. pylori gastritis patterns between GERD patients and non-reflux controls is therefore mandatory.
References
Rokkas T, Ladas SD, Triantafyllou K, Liatsos C, Petridou E, Papatheodorou G, Karameris A, Raptis SA: The association between CagA status and the development of esophagitis after the eradication of Helicobacter pylori. Am J Med. 2001, 110: 703-707. 10.1016/S0002-9343(01)00723-9.
Take S, Mizuno M, Ishiki K, Nagahara Y, Yoshida T, Yokota K, Oguma K, Okada H, Yamamoto K: Helicobacter pylori eradication may induce de novo, but transient and mild, reflux esophagitis: prospective endoscopic evaluation. J Gastroenterol Hepatol. 2009, 24: 107-113. 10.1111/j.1440-1746.2008.05606.x.
Cremonini F, Di Caro S, Delgado-Aros S, Sepulveda A, Gasbarrini G, Gasbarrini A, Camilleri M: Meta-analysis: the relationship between Helicobacter pylori infection and gastrooesophageal reflux disease. Aliment Pharmacol Ther. 2003, 18: 279-289. 10.1046/j.1365-2036.2003.01665.x.
Fallone CA, Barkun AN, Friedman G, Mayrand S, Loo V, Beech R, Best L, Joseph L: Is Helicobacter pylori eradication associated with gastroesophageal reflux disease?. Am J Gastroenterol. 2000, 95: 914-920. 10.1111/j.1572-0241.2000.01929.x.
Schwizer W, Thumshirn M, Dent J, Guldenschuh I, Menne D, Cathomas G, Fried M: Helicobacter pylori and symptomatic relapse of gastro-esophageal reflux disease: a randomised controlled trial. Lancet. 2001, 357: 1738-1742. 10.1016/S0140-6736(00)04894-7.
McColl KE, Dickson A, El-Nujumi A, El-Omar E, Kelman A: Symptomatic benefit 1-3 years after H. pylori eradication in ulcer patients: impact of gastroesophageal reflux disease. Am J Gastroenterol. 2000, 95: 101-105.
Spechler SJ: Does Helicobacter pylori infection contribute to gastroesophageal reflux disease?. Yale J Biol Med. 1998, 71: 143-148.
Mahdi BM: The relationship between helicobacter pylori infection and gastro-esophageal reflux disease. N Am J Med Sci. 2011, 3: 142-145.
Patti MG, Gorodner MV, Galvani C, Tedesco P, Fisichella PM, Ostroff JW, Bagatelos KC, Way LW: Spectrum of esophageal motility disorders. Arch Surg. 2005, 140: 442-449. 10.1001/archsurg.140.5.442.
Kusano M, Shimoyama Y, Sugimoto S, Kawamura O, Maeda M, Minashi K, Kuribayashi S, Higuchi T, Zai H, Ino K, Horikoshi T, Sugiyama T, Toki M, Ohwada T, Mori M: Development and evaluation of FSSG: frequency scale for the symptoms of GERD. J Gastroenterol. 2004, 39: 888-891. 10.1007/s00535-004-1417-7.
Johnson LF, DeMeester TR: Development of the 24-hour intraesophageal pH monitoring composite scoring system. J Clin Gastroenterol. 1986, 8 (Suppl 1): 52-58.
Savary M, Miller G: The Esophagus. Handbook and Atlas of Endoscopy. 1978, Solothurn, Switzerland: Verlag Grassmann, 135-142.
Lord RV, Frommer DJ, Inder S, Tran D, Ward RL: Prevalence of Helicobacter pylori infection in 160 patients with Barrett's esophagus or Barrett's adenocarcinoma. Aust N Z J Surg. 2000, 70: 26-33. 10.1046/j.1440-1622.2000.01737.x.
Smout AJPM: Endoscopy-negative acid reflux disease. Aliment Pharmacol Ther. 1997, 11 (S2): 81-85.
Gisbert JP, Pajares JM, Losa C: Helicobacter pylori and gastroesophageal reflux disease: friends or foes?. Hepatogastroenterology. 1999, 46: 1023-1029.
Gisbert JP, de Pedro A, Losa C, Barreiro A, Pajares JM: Helicobacter pylori and gastroesophageal reflux disease: lack of influence of infection on twenty-four-hour esophageal ph monitoring and endoscopic findings. J Clin Gastroenterol. 2001, 32: 210-221. 10.1097/00004836-200103000-00005.
Galmiche JP, Barthelemy P, Hamelin B: Treating the symptoms of gastroesophageal reflux disease: a double-blind comparison of omeproazole and cisapride. Aliment Pharmacol Ther. 1997, 11: 765-773. 10.1046/j.1365-2036.1997.00185.x.
Güliter S, Kandilci U: The effect of Helicobacter pylori eradication on gastroesophageal reflux disease. J Clin Gastroenterol. 2004, 38: 750-755. 10.1097/01.mcg.0000139071.30956.30.
Wu JC, Chan FK, Wong SK, Lee YT, Leung WK, Sung JJ: Effect of Helicobacter pylori eradication on esophageal acid exposure in patients with reflux oesophagitis. Aliment Pharmacol Ther. 2002, 16: 545-552. 10.1046/j.1365-2036.2002.01189.x.
Zhu H, Pace F, Sangaletti O, Bianchi Pocco G: Gastric acid secretion and pattern of gastroesophageal reflux in patients with esophagitis and concomitant duodenal ulcer. A multivariate analysis of pathogenetic factors. Scand J Gastroenterol. 1993, 28: 387-392. 10.3109/00365529309098237.
Oberg S, Peters JH, Nigro JJ, Theisen J, Hagen JA, DeMeester SR, Bremner CG, DeMeester TR: Helicobacter pylori is not associated with the manifestations of gastroesophageal reflux disease. Arch Surg. 1999, 134: 722-726. 10.1001/archsurg.134.7.722.
Calleja JL, Suarez M, De Tejada AH, Navarro A, Pantogerd Group: Helicobacter pylori infection in patients with erosive esophagitis is associated with rapid heartburn relief and lack of relapse after treatment with pantoprazole. Dig Dis Sci. 2005, 50 (3): 432-9. 10.1007/s10620-005-2453-8.
Grande M, Sileri P, Attinà GM, De Luca B, Ciano P, Ciangola CI, Cadeddu F: Nonerosive gastroesophageal reflux disease and mild degree of esophagitis: comparison of symptoms endoscopic, manometric and pH-metric patterns. World J Surg Oncol. 2012, 10: 84-10.1186/1477-7819-10-84.
Thor PJ, Blaut U: Helicobacter pylori infection in pathogenesis of gastroesophageal reflux disease. J Phisiol Pharmacol. 2006, 57 (S3): 81-90.
Csendes A, Smok G, Cerda G, Burdiles P, Mazza D, Csendes P: Prevalence of Helicobacter Pylori infection in 190 control subjects and in 236 patients with gastroesophageal reflux, erosive esophagitis or Barrett’s esophagus. Dis Esophagus. 1997, 10: 38-42.
Dent J, Holloway RH, Toouli J, Dodds WJ, Dent J: Mechanism of lower esophageal sphincter incompetence in patients with symptomatic gastroesophageal reflux. Gut. 1988, 29: 1020-1028. 10.1136/gut.29.8.1020.
Mittal RK, Holloway RH, Penagini R, Blackshaw LA, Dent JT: Lower esophageal sphincter relation. Gastroenterology. 1995, 109: 601-610. 10.1016/0016-5085(95)90351-8.
Warburton-Timms VJ, Charlett A, Valori RM, Uff JS, Shepherd NA, Barr H, McNulty CA: The significance of cagA(+) Helicobacter pylori in reflux oesophagitis. Gut. 2001, 49: 341-346. 10.1136/gut.49.3.341.
Molloy RM, Sonnenberg A: Relation between gastric cancer and previous peptic ulcer disease. Gut. 1997, 40: 247-252. 10.1136/gut.40.2.247.
Kuipers EJ, Lundell L, Klinkenberg-Knol EC, Havu N, Festen HP, Liedman B, Lamers CB, Jansen JB, Dalenback J, Snel P, Nelis GF, Meuwissen SG: Atrophic gastritis and Helicobacter pylori infection in patients with reflux esophagitis treated with omerozole or fundoplication. N Engl J Med. 1996, 334: 1018-1022. 10.1056/NEJM199604183341603.
Klinkenberg-Knol EC, Nelis F, Dent J, Snel P, Mitchell B, Prichard P, Lloyd D, Havu N, Frame MH, Romàn J, Walan A, Long-Term Study Group: Long-term omeprazole treatment in resistant gastroesophageal reflux disease: efficacy, safety and influence on gastric mucosa. Gastroenterology. 2000, 118: 661-669. 10.1016/S0016-5085(00)70135-1.
Pera M, Cameron A, TrastecK VF, Carpenter HA, Zinsmeister AR: Increasing incidence of adenocarcinoma of the esophagus and esophagogastic junction. Gastroenterology. 1993, 104: 510-513.
Newton M, Bryan R, Burnhan WR, Kamm MA: Evaluation of Helicobacter pylori in reflux oesophagitis and Barrett's esophagus. Gut. 1997, 40: 9-13. 10.1136/gut.40.1.9.
O'Connor HJ, Cunnane K: Helicobacter pylori and astrooesophagel reflux disease – a prospective study. Ir J Med Sci. 1994, 163: 369-373. 10.1007/BF02942830.
Hackelsberger A, Schultze V, Gunther T, von Arnim U, Manes G, Malfertheiner P: Prevalence of helicobacter pylori gastritis in patients with reflux osophagitis: a case-control study. Eur J Gastroentero Hepatol. 1998, 10: 465-468. 10.1097/00042737-199806000-00005.
Bleser MJ: Helicobacter pylori: microbiology of a 'slow' bacterial infection. Trends Microbiol. 1993, 1: 255-260. 10.1016/0966-842X(93)90047-U.
Lee JM, O'Moain CA: Different management for helicobacter pylori positive and negative patients with gastroesophageal reflux disease?. Gut. 1998, 43 (S1): 14-20.
Sharma VK, Howden CW: Decreased prevalence of H. pylori and cagA+ H. pylori in GERD and Barrett's esophagus (BE) with or without dysplasia or adenocarcinoma (D/AC): a meta-analysis. Gastroenterology. 2002, 122: A291-
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MG: manuscript preparation, interpretation of data and critical review. GL: acquisition data and drafting the manuscript. FDS: acquisition data and literature review. SG: acquisition and processing data. AE: acquisition and processing data. MC: acquisition and processing data. VB: acquisition and processing data. GM: literature review and manuscript preparation. MV: literature review and manuscript preparation. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Grande, M., Lisi, G., De Sanctis, F. et al. Does a relationship still exist between gastroesophageal reflux and Helicobacter pylori in patients with reflux symptoms?. World J Surg Onc 12, 375 (2014). https://doi.org/10.1186/1477-7819-12-375
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7819-12-375