Abstract
Background
Previous studies demonstrate that tolterodine extended release (ER) significantly improves urgency urinary incontinence (UUI) episodes. Instruments that measure patient-reported outcomes (PROs) provide additional information that is valuable for assessing whether clinical improvements are meaningful to the patient. This study determined the correlation of changes in bladder diary variables and other PROs in subjects with overactive bladder (OAB).
Methods
Subjects with OAB, urinary frequency, and UUI were treated with 4 mg once-daily tolterodine ER or placebo for 12 weeks. Subjects completed 7-day bladder diaries, the Patient Perception of Bladder Condition (PPBC), and the King's Health Questionnaire (KHQ) at baseline and week 12. Only subjects who reported at least some minor bladder-related problems at baseline (PPBC score ≥ 3) were included in this analysis.
Results
Reductions in UUI episodes per week were significantly greater in the tolterodine ER group (n = 500) compared with the placebo group (n = 487) at week 12 (-71% vs -33%, P < 0.0001). A significantly greater percentage of subjects in the tolterodine ER group reported improvement on the PPBC versus placebo (58% vs 45%, P < 0.0001), and 7 of 10 KHQ domains were significantly improved versus placebo (all P < 0.05). Significant correlations were found for median percentage changes in UUI episodes with changes in PPBC scores (r = 0.35,P < 0.0001) and the 7 improved KHQ domains (r = 0.16–0.32, P ≤ 0.0011). Changes in PPBC scores and all KHQ domains were significantly correlated (r = 0.13–0.38, P ≤ 0.009) in the tolterodine ER group. Correlations among endpoints in the placebo group were similar to those observed in the tolterodine ER group.
Conclusion
Improvement in UUI episodes after 12 weeks of treatment with tolterodine ER or placebo was correlated with improvements in patients' perception of their bladder-related problems and health-related quality of life. Correlations were moderate in magnitude but statistically significant, suggesting that PROs are important and relevant measures for evaluating OAB treatment.
Similar content being viewed by others
Background
Overactive bladder (OAB) is defined by the International Continence Society (ICS) as urgency, with or without urgency urinary incontinence (UUI), usually with increased daytime frequency and nocturia [1, 2]. OAB affects approximately 17% of adults in the United States [3] and Europe [4]. A recent study using current ICS definitions of OAB found the prevalence of OAB to be 11% in men and 13% in women [5]. It was also demonstrated that the prevalence of OAB increases with advancing age, occurring in 20% of subjects who are ≥ 60 years of age. Antimuscarinics, such as tolterodine, are first-line treatments for OAB and have proven efficacy and tolerability [6].
Bladder diaries are traditionally used to quantify OAB symptoms and provide information about treatment effects on the frequency and severity of symptoms, but they do not provide information regarding the patient's perspective on his or her symptoms or the impact of treatment. Instruments that measure patient-reported outcomes (PROs) provide valuable additional information for assessing whether clinical improvements are meaningful to the patient [7]. Several questionnaires, measuring a broad array of concepts, have been validated for use in subjects with OAB, including the King's Health Questionnaire (KHQ) [8] and Patient Perception of Bladder Condition (PPBC) [9].
Numerous studies have used questionnaires to demonstrate that OAB symptoms have a negative impact on the subjects' health-related quality of life (HRQL) [3, 10–13]. OAB adversely affects social and professional activities, social and sexual relationships, and travel [14, 15]. Treatment with antimuscarinics is associated with significant improvement in HRQL, symptom bother, and perception of treatment benefit, as well as improvement in bladder diary variables [16–19]. Evidence suggests that treatment effects on the number and/or severity of OAB symptoms and urodynamic variables may not be fully predictive of treatment effects on HRQL and other PROs that are not based on changes in bladder diary variables, leading some authors to advocate that the use of these PROs become standard in clinical studies of OAB [20].
We evaluated the relationships between treatment-related changes in UUI episodes as recorded in bladder diaries and 2 validated questionnaires using data from a large placebo-controlled trial of tolterodine [21].
Methods
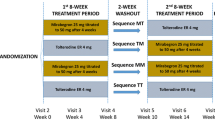
Details of the study design have been previously published [21]. Briefly, this 12-week, double-blind, placebo-controlled trial included subjects with urinary frequency (≥ 8 micturitions per 24 h) and UUI (≥ 5 episodes per wk) who had OAB symptoms for ≥ 6 months. This study was conducted in 167 centers in Australasia (n = 4), Europe (n = 89), and North America (n = 74). The study was conducted in accordance with the Good Clinical Practice Guidelines and the Declaration of Helsinki. The appropriate International Ethics Committees/Institutional Review Boards approved the study protocol, and all patients gave written informed consent before the start of the study. Subjects were randomized to once-daily treatment with 4 mg tolterodine extended release (ER) or placebo for 12 weeks. For this analysis, only subjects who reported at least some minor bladder-related problems at baseline (PPBC score ≥ 3) were included.
Symptom assessment using bladder diaries and questionnaires
Subjects completed 7-day bladder diaries in which they recorded every incontinence episode, urgency episode, and micturition at the times at which they occurred during 7 consecutive days prior to the baseline and week 12 visits. Subjects also completed the KHQ and the PPBC at baseline and week 12. The KHQ is a measure of HRQL that includes 2 single-item domains (General Health Perceptions and Incontinence Impact), 7 multi-item domains (Role Limitations, Physical Limitations, Social Limitations, Personal Relationships, Emotions, Sleep/Energy, Severity/Coping), and a multi-item Symptom Severity scale [22]. The 2 single-item domains and the 7 multi-item domains of the KHQ are scored on a scale from 0 (best) to 100 (worst). The Symptom Severity scale is scored from 0 (best) to 30 (worst). Decreases in KHQ domain scores indicate an improvement in HRQL. The minimally important difference (MID) – the smallest change in score that subjects perceive as beneficial – is 3 points for the Symptom Severity scale and 5 points for all other KHQ domains [23].
The PPBC is a validated single-item measure of the subjects' perception of the extent of their bladder-related problems [9, 24]. Subjects select 1 of 6 statements ranging from "my bladder condition does not cause me any problems at all" to "my bladder condition causes me many severe problems" [9, 24]. A decrease in score indicates improvement.
Statistical analysis
Median percentage changes in UUI episodes per week were analyzed using a rank analysis of covariance (ANCOVA) with baseline value as a covariate; mean changes in UUI episodes per week were analyzed using ANCOVA with baseline value as a covariate. Mean changes in KHQ scores from baseline to week 12 were analyzed for the current study using ANCOVA with baseline value as a covariate. Categorical changes in PPBC scores were analyzed using chi-square tests. A ≥ 2-point reduction in PPBC score was considered a major improvement, a 1-point reduction was considered a minor improvement, and no change or an increase was considered no improvement in the extent of bladder-related problems. The relationships between changes in UUI episodes, PPBC scores, and KHQ scores were evaluated using Spearman correlation coefficients. Changes in UUI episodes were used for this analysis because they were a defining symptom for this population. Correlations were considered to be small in size for |r| < 0.30 and moderate in size for |r| = 0.30 to 0.49 [25].
Results
Baseline demographics and clinical characteristics for 987 subjects (placebo, n = 487; tolterodine ER, n = 500) are presented in Table 1. Most subjects were women (82%) and white (95%).
Subjects treated with tolterodine ER showed a significantly greater median percentage (-71% vs -33%, P < 0.0001) and mean (-11.8 vs -6.9, P < 0.0001) reduction in UUI episodes per week than did subjects treated with placebo. A significantly greater percentage of subjects treated with tolterodine ER showed improvement in PPBC scores (58%; 30% with ≥ 2-point improvement) than did subjects treated with placebo (45%; 21% with ≥ 2-point improvement; P < 0.0001). Subjects treated with tolterodine ER also achieved significantly larger improvements on 7 KHQ domains, including Incontinence Impact, Role Limitations, Physical Limitations, Social Limitations, Sleep/Energy, Severity/Coping, and Symptom Severity compared with subjects receiving placebo (Table 2). Among subjects treated with tolterodine ER, the change in every KHQ domain score except Symptom Severity and General Health Perceptions exceeded MID criteria for improvement [23]. The MID criteria were met for the Emotions domain in the tolterodine ER group; however, the improvement from baseline was not statistically significant (P = 0.0746) compared with the placebo group.
Among subjects receiving tolterodine ER, the present analysis revealed a moderately sized but statistically significant correlation between week 12 median percentage reductions in UUI episodes and changes in PPBC score (|r| ≥ 0.35, P ≤ 0.001). Small to moderately sized but statistically significant correlations were also observed between median percentage reductions in UUI episodes from baseline and improvements in 8 of 10 KHQ domains (|r| = 0.16–0.35, all P ≤ 0.01) in tolterodine ER-treated subjects (Table 3). Similar correlations were observed between mean reductions in UUI episodes and improvements in PPBC and KHQ scores.
Treatment-related changes in PPBC scores were correlated with changes in all 10 KHQ domains (Table 4). Similar relationships were observed in the placebo group. Moderate but statistically significant correlations (|r| ≥ 0.30, all P < 0.001) were observed between PPBC scores and Incontinence Impact, Role Limitations, Physical Limitations, Emotions, Severity/Coping, and Symptom Severity in the tolterodine ER group; the placebo group showed similar correlations except for Emotions and Symptom Severity, which were poorly correlated. Categorical improvement on the PPBC was correlated with improvements in KHQ domain scores in the tolterodine ER group (Figure 1). Changes in KHQ scores were 2 to 3 times larger in subjects who showed a ≥ 2-point improvement on the PPBC than in those who showed a 1-point improvement.
There were improvements from baseline in UUI episodes, PPBC, and KHQ in the placebo group that were statistically significantly smaller than those in the tolterodine ER group (Table 2). However, correlations among these endpoints in the placebo group were similar to those observed in the tolterodine ER group (Tables 3 and 4).
Discussion
In this analysis, the tolterodine ER group showed statistically significant and clinically meaningful improvements in UUI episodes, subjects' perceptions of the extent of their bladder-related problems, and HRQL compared with placebo. These results are consistent with previous reports demonstrating that tolterodine ER significantly improved UUI episodes [26, 27], PPBC scores [18, 26], and KHQ scores [16, 17] in subjects with OAB. However, correlational analyses showed that improvement in UUI episodes was significantly correlated with improvements in PPBC scores and most domains of the KHQ in subjects receiving either tolterodine ER or placebo. The results were similar regardless of whether median percentage or mean changes in UUI episodes were used in the analyses. Changes in PPBC scores were also correlated with changes in scores on each domain of the KHQ, and categorical improvements in PPBC scores were positively associated with the magnitude of improvement on each KHQ domain. These data suggest that the PPBC and KHQ are relevant measures of OAB treatment efficacy.
Although the correlations among improvements in UUI episodes, PPBC scores, and KHQ scores after treatment with tolterodine ER were small to moderate, they were statistically significant. Similarly, a study that used data from primary care patients collected during an open-label trial of tolterodine ER found that improvements in bladder diary variables were significantly correlated with improvements on the PPBC, the Overactive Bladder Questionnaire (OAB-q) Symptom Bother scale, and all HRQL domains of the OAB-q [28]. As in the present study, the correlations were small to moderate but statistically significant. Collectively, these findings suggest that PROs provide information about OAB treatment efficacy that is related to, but not redundant with, bladder diaries. This interpretation is consistent with a study by Abrams et al [20] in which symptom-based outcomes (ie, bladder diaries, urodynamics) were compared with questionnaire outcomes from 27 clinical trials of antimuscarinics. The results showed that, although there were often parallel improvements in these 2 outcomes, there were cases in which improvements in symptom-based measures were not accompanied by corresponding changes in PRO measures.
Abrams et al [20] concluded that statistically significant changes in the frequency of symptoms may not always reflect subjects' assessments of treatment success, and that both symptom-based measures and patient-centric measures of treatment impact should be used in studies of OAB pharmacotherapy [20]. The findings reported here support the conclusion that symptom-based measures and patient-centric measures are complementary and should be used together in clinical trials. The KHQ, PPBC, and other instruments, such as the OAB-q, Overactive Bladder Symptom Score (OABSS) and Urgency Perception Scale (UPS), have been validated among patients with OAB and are reliable and responsive to treatment [9, 10, 24, 29–32].
In the current study, correlations between improvements in PPBC and KHQ scores were also of small to moderate strength, suggesting that these instruments may reflect different aspects of OAB treatment efficacy. The PPBC, a single-item measure that is easy to use and interpret, provides a global integrated measure of the subjects' perception of the extent of their bladder-related problems. Other validated instruments, such as the KHQ or OAB-q, provide detailed and multidimensional information concerning patient outcome or condition that is not captured by a single-item measure. The choice of questionnaires administered in clinical trials should reflect the research objectives of the trial [9].
Notably, these instruments are patient-friendly and may help clinicians diagnose OAB and assess treatment efficacy in the clinic without the inconvenience of a bladder diary. The importance of measuring patients' assessment of treatment impact has been demonstrated by evidence of disparity between the opinions of clinicians and patients regarding the level of bother and the impact of urinary symptoms on HRQL [33].
Although changes from baseline for each endpoint were significantly smaller among placebo- versus tolterodine ER-treated subjects, relationships among endpoints were generally similar in the active and placebo groups. This is not unexpected because the correlations should be similar for changes from baseline that are in the same direction, whether they occur in the treatment or placebo group.
The current analysis suggests that PROs are relevant and complementary to changes in UUI episodes in the assessment of OAB treatment; however, the study has some limitations. Inclusion criteria for this study required subjects to have UUI; therefore, the analysis is limited to only patients with UUI. However, a large proportion of patients with OAB are not incontinent [3–5]. Because UUI was the only variable used to assess these relationships, we cannot extrapolate these results to other OAB symptoms.
Conclusion
Changes in UUI episodes were correlated with changes in PPBC and HRQL scores in subjects with OAB treated with either tolterodine ER or placebo. These findings indicate that data obtained from PROs provide a distinct source of information about treatment efficacy in the evaluation of OAB treatments.
Abbreviations
- ER:
-
extended release
- HRQL:
-
health-related quality of life
- ICS:
-
International Continence Society
- KHQ:
-
King's Health Questionnaire
- MID:
-
minimally important difference
- OAB:
-
overactive bladder
- PPBC:
-
Patient Perception of Bladder Condition
- PRO:
-
patient-reported outcome
- TER:
-
tolterodine extended release
- UUI:
-
urgency urinary incontinence.
References
Abrams P, Artibani W, Cardozo L, Dmochowski R, van Kerrebroeck P, Sand P: Reviewing the ICS 2002 Terminology Report: The Ongoing Debate. Neurourol Urodyn 2006, 25: 293. 10.1002/nau.20251
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A: The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 2003,61(1):37–49. 10.1016/S0090-4295(02)02243-4
Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, Hunt TL, Wein AJ: Prevalence and burden of overactive bladder in the United States. World J Urol 2003,20(6):327–336.
Milsom I, Abrams P, Cardozo L, Roberts RG, Thuroff J, Wein AJ: How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int 2001,87(9):760–766. 10.1046/j.1464-410x.2001.02228.x
Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, Coyne KS, Kelleher C, Hampel C, Artibani W, et al.: Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: Results of the EPIC study. Eur Urol 2006, 50: 1306–1315. 10.1016/j.eururo.2006.09.019
Andersson KE: Antimuscarinics for the treatment of overactive bladder. Lancet Neurol 2004,3(1):46–53. 10.1016/S1474-4422(03)00622-7
Leidy NK, Revicki DA, Geneste B: Recommendations for evaluating the validity of quality of life claims for labeling and promotion. Value Health 1999, 2: 113–127. 10.1046/j.1524-4733.1999.02210.x
Reese PR, Pleil AM, Okano GJ, Kelleher CJ: Multinational study of reliability and validity of the King's Health Questionnaire in patients with overactive bladder. Qual Life Res 2003,12(4):427–442. 10.1023/A:1023422208910
Coyne KS, Matza LS, Kopp Z, Abrams P: The validation of the patient perception of bladder condition (PPBC): a single-item global measure for patients with overactive bladder. Eur Urol 2006,49(6):1079–1086. 10.1016/j.eururo.2006.01.007
Coyne K, Revicki D, Hunt T, Corey R, Stewart W, Bentkover J, Kurth H, Abrams P: Psychometric validation of an overactive bladder symptom and health-related quality of life questionnaire: the OAB-q. Qual Life Res 2002,11(6):563–574. 10.1023/A:1016370925601
Liberman JN, Hunt TL, Stewart WF, Wein A, Zhou Z, Herzog AR, Lipton RB, Diokno AC: Health-related quality of life among adults with symptoms of overactive bladder: results from a U.S. community-based survey. Urology 2001,57(6):1044–1050. 10.1016/S0090-4295(01)00986-4
Coyne KS, Payne C, Bhattacharyya SK, Revicki DA, Thompson C, Corey R, Hunt TL: The impact of urinary urgency and frequency on health-related quality of life in overactive bladder: results from a national community survey. Value Health 2004,7(4):455–463. 10.1111/j.1524-4733.2004.74008.x
Coyne KS, Zhou Z, Thompson C, Versi E: The impact on health-related quality of life of stress, urge and mixed urinary incontinence. BJU Int 2003,92(7):731–735. 10.1046/j.1464-410X.2003.04463.x
Abrams P, Kelleher C, Lerr L, Rogers R: Overactive bladder significantly affects quality of life. Am J Manag Care 2000, 6: S580–590.
Irwin DE, Milsom I, Kopp Z, Abrams P, Cardozo L: Impact of overactive bladder symptoms on employment, social interactions and emotional well-being in six European countries. BJU Int 2006,97(1):96–100. 10.1111/j.1464-410X.2005.05889.x
Kelleher CJ, Reese PR, Pleil AM, Okano GJ: Health-related quality of life of patients receiving extended-release tolterodine for overactive bladder. Am J Manag Care 2002,8(19 Suppl):S608-S615.
Homma Y, Kawabe K: Health-related quality of life of Japanese patients with overactive bladder treated with extended-release tolterodine or immediate-release oxybutynin: a randomized, placebo-controlled trial. World J Urol 2004,22(4):251–256. 10.1007/s00345-004-0455-3
Freeman R, Hill S, Millard R, Slack M, Sutherst J: Reduced perception of urgency in treatment of overactive bladder with extended-release tolterodine. Obstet Gynecol 2003,102(3):605–611. 10.1016/S0029-7844(03)00623-9
Roberts R, Bavendam T, Glasser DB, Carlsson M, Eyland N, Elinoff V: Tolterodine extended release improves patient-reported outcomes in overactive bladder: results from the IMPACT trial. Int J Clin Pract 2006, 60: 752–758. 10.1111/j.1742-1241.2006.00987.x
Abrams P, Artibani W, Gajewski JB, Hussain I: Assessment of treatment outcomes in patients with overactive bladder: importance of objective and subjective measures. Urology 2006,68(suppl 2A):17–28. 10.1016/j.urology.2006.05.044
van Kerrebroeck P, Kreder K, Jonas U, Zinner N, Wein A: Tolterodine once-daily: superior efficacy and tolerability in the treatment of the overactive bladder. Urology 2001,57(3):414–421. 10.1016/S0090-4295(00)01113-4
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S: A new questionnaire to assess the quality of life of urinary incontinent women. Br J Obstet Gynaecol 1997,104(12):1374–1379.
Kelleher CJ, Pleil AM, Reese PR, Burgess SM, Brodish PH: How much is enough and who says so? The case of the King's Health Questionnaire and overactive bladder. BJOG 2004,111(6):605–612. 10.1111/j.1471-0528.2004.00129.x
Matza LS, Thompson CL, Krasnow J, Brewster-Jordan J, Zycyzynski T, Coyne KS: Test-retest reliability of four questionnaires for patients with overactive bladder: the Overactive Bladder Questionnaire (OAB-q), Patient Perception of Bladder Condition (PPBC), Urgency Questionnaire (UQ), and the Primary OAB Symptom Questionnaire (POSQ). Neurourol Urodyn 2005, 24: 215–225. 10.1002/nau.20110
Cohen J: Statistical Power Analysis for the Behavioral Sciences. 2nd edition. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988.
Homma Y, Paick JS, Lee JG, Kawabe K: Clinical efficacy and tolerability of extended-release tolterodine and immediate-release oxybutynin in Japanese and Korean patients with an overactive bladder: a randomized, placebo-controlled trial. BJU Int 2003,92(7):741–747. 10.1046/j.1464-410X.2003.04468.x
Michel MC, de la Rosette JJ, Piro M, Schneider T: Comparison of symptom severity and treatment response in patients with incontinent and continent overactive bladder. Eur Urol 2005,48(1):110–115. 10.1016/j.eururo.2004.11.012
Coyne KS, Elinoff V, Gordon DA, Deng DY, Brodsky M, Glasser DB, Jumadilova Z, Carlsson M: Relationships between improvements in symptoms and patient assessments of bladder condition, symptom bother and health-related quality of life in patients with overactive bladder treated with tolterodine. Int J Clin Pract 2008,62(6):925–931. 10.1111/j.1742-1241.2008.01778.x
Coyne KS, Matza LS, Thompson CL: The responsiveness of the Overactive Bladder Questionnaire (OAB-q). Qual Life Res 2005, 14: 849–855. 10.1007/s11136-004-0706-1
Coyne K, Tubaro A, Brubaker L, Bavendam T: Development and validation of patient-reported outcomes measures for overactive bladder. Urology 2006,68(suppl 2A):9–16. 10.1016/j.urology.2006.05.042
Homma Y, Yoshida M, Seki N, Yokoyama O, Kakizaki H, Gotoh M, Yamanishi T, Yamaguchi O, Takeda M, Nishizawa O: Symptom assessment tool for overactive bladder syndrome – overactive bladder symptom score. Urology 2006,68(2):318–323. 10.1016/j.urology.2006.02.042
Cardozo L, Coyne KS, Versi E: Validation of the Urgency Perception Scale. BJU Int 2005, 95: 591–596. 10.1111/j.1464-410X.2005.05345.x
Marschall-Kehrel D, Roberts RG, Brubaker L: Patient-reported outcomes in overactive bladder: the influence of perception of condition and expectation for treatment benefit. Urology 2006,68(suppl 2A):29–37. 10.1016/j.urology.2006.02.046
Acknowledgements
This study was funded by Pfizer Inc. Editorial support was provided by Colin P. Mitchell, PhD, and Donald G. Buerk, PhD, from Complete Healthcare Communications, Inc., and was funded by Pfizer Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
PVK has been an investigator and lecturer for Astellas, Eli-Lilly, Ferring, Pfizer Inc, and Novartis; CK has been a consultant, investigator, and lecturer for Astellas, GlaxoSmithKline, Novartis, Pfizer Inc, Tanabe, Union Chimique Belge, and Watson; KSC has been a consultant for Pfizer Inc; ZK, MB, and JTW are employees of Pfizer Inc.
Authors' contributions
PvK, CK, KC, ZK, MB, and JTW participated in the concept and design, interpretation of data, and the drafting and revising of the manuscript. PvK was involved in collecting the data. JTW conducted the data analysis. All authors have read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Van Kerrebroeck, P.E., Kelleher, C.J., Coyne, K.S. et al. Correlations among improvements in urgency urinary incontinence, health-related quality of life, and perception of bladder-related problems in incontinent subjects with overactive bladder treated with tolterodine or placebo. Health Qual Life Outcomes 7, 13 (2009). https://doi.org/10.1186/1477-7525-7-13
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7525-7-13