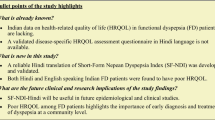
Abstract
Background
Symptoms of heartburn has an impact on health-related quality of life (HRQL). When a questionnaire is translated into a new language, a linguistic validation is necessary but not sufficient unless the psychometric characteristics have been verified. The aim is to document the psychometric characteristics of the German translation of the Gastrointestinal Symptom Rating Scale (GSRS) and Quality of Life in Reflux and Dyspepsia (QOLRAD) questionnaire.
Methods
142 patients with symptoms of heartburn (Age: M = 47.5, ± 14.6; Males = 44.4%) completed the German translation of GSRS, the QOLRAD, the Short-Form-36 (SF-36) and the Hospital Anxiety and Depression (HAD) scale.
Results
The internal consistency reliability of GSRS ranged from 0.53–0.91 and of QOLRAD from 0.90–0.94, respectively. The test-retest reliability of GSRS ranged from 0.49–0.73 and of QOLRAD from 0.70–0.84. The relevant domains of the GSRS and QOLRAD domain scores significantly correlated. GSRS domains of Abdominal Pain and Constipation correlated (negatively) with most of the domains of the SF-36. The relevant QOLRAD domains significantly correlated with all SF-36 domains.
Conclusions
The psychometric characteristics of the German translation of GSRS and QOLRAD were found to be good, with satisfactory reliability and validity. The reliability of the GSRS Abdominal Pain domain was moderate.
Similar content being viewed by others
Background
Heartburn is the primary symptom of gastro-esophageal reflux disease (GERD). The diagnosis relies solely on patients' subjective symptom evaluation unless an endoscopy is performed [1]. Heartburn affects several aspects of patients' lives [2, 3], such as their ability to have a good night sleep and to eat and drink whatever they want [4]. Hence, the assessment of how upper gastrointestinal symptoms impact patients' health-related quality of life provides important information about the patient's health status and how patients perceive the treatment regime [5]. This information is of interest to clinicians, enabling them to better understand how to tailor treatment to the individual patient's needs. However, in order to be a viable measure of treatment outcome in clinical trials, Patient-Reported Outcomes (PRO) instruments must be extensively documented to both meet scientific standards [6] and to satisfy regulatory criteria, particularly from the perspective of claims for labeling and promotion [7]. The regulatory criterion is twofold: linguistic, cross-cultural adaptation and psychometric documentation. The translation and the cross-cultural adaptation of the German translation of the QOLRAD were done according to the latest guidelines [8]. Its psychometric properties remain to be documented. Thus, the aim of this study was to document the reliability and validity of the German translation of the GSRS and QOLRAD in patients with GERD.
Methods
Patients
Consecutive patients with current or previously verified (there was no definite time frame given) predominant symptoms of heartburn were screened in both general practices and gastroenterology clinics. Heartburn was defined as a 'burning feeling rising from the stomach or lower part of the chest up towards the neck'. Patients were excluded if they had: concurrent diagnosis of Irritable Bowel Syndrome (IBS) or peptic ulcer disease; other significant medical or surgical disease; major psychiatric illness or dementia. Patients treated for peptic ulcer with anti-secretory or anti-Helicobacter pylori therapy and referred for follow-up endoscopy or those using of acetyl salicylic acid (ASA) or other nonsteroidal anti-inflammatory drugs (NSAIDs) daily were also excluded. Patients had to be able to complete the PRO instruments themselves, i.e. no proxy assessment or interpreter was allowed. The study was conducted between December 2000 and November 2001 in five centers. Written informed consent was obtained from all patients prior to inclusion in the trial. The study protocol and consent form were approved by independent local ethics committee in accordance with the revised Declaration of Helsinki. The patient was free to discontinue participation in the study at any time.
Demographic and clinical variables
Clinicians reported: patient demographics (age, sex, race, family and employment status); medical history; history of gastrointestinal disease; and frequency and severity of heartburn symptoms. Investigators also assessed the patients' symptoms using a four-graded scale: 0 = none: no symptoms; 1 = mild: awareness of sign or symptom, but easily tolerated; 2 = moderate: discomfort sufficient to cause interference with normal activities; 3 = severe: incapacitating with inability to perform normal activities. All data were reported in a paper case report form.
Patient-Reported Outcomes (PRO) instruments
Generic instruments are comprehensive, designed to be applicable across diseases, treatments and populations. Both general population norm values and values of populations with a number of chronic diseases are available. Disease-specific instruments, on the other hand, capture details about the disease activity and symptom patterns and are likely to be more responsive to change than generic instruments [9, 10]. Taking into consideration the complementary nature of these different kinds of instruments, disease-specific and generic instruments are in practice often used in tandem.
Patients completed four PRO instruments: Gastrointestinal Symptom Rating Scale (GSRS) [11]; the heartburn version of Quality of Life in Reflux and Dyspepsia (QOLRAD) [12] questionnaire; the Short-Form Health 36 (SF-36) [13]; and the Hospital Anxiety and Depression scale (HAD) [14]. All PRO instruments have been tested in terms of validity and reliability (see below).
Gastrointestinal Symptom Rating Scale (GSRS)
The Gastrointestinal Symptom Rating Scale is a disease-specific instrument that includes 15 items combined into five-symptom clusters addressing different gastrointestinal symptoms. The five-symptom clusters depict reflux, abdominal pain, indigestion, diarrhea and constipation. The GSRS has a seven-graded Likert type scale where 1 represents absence of bothersome symptoms and 7 very bothersome symptoms. The GSRS is well documented to be reliable and valid [15] and norm values for a general population are available [16].
Quality of Life in Reflux and Dyspepsia (QOLRAD)
The heartburn version of the QOLRAD is a disease-specific instrument, including twenty-five items combined into five dimensions: Emotional distress, Sleep disturbance, Vitality, Food/drink problems and Physical/social functioning. The questions are rated on a seven-graded Likert-type scale; the lower the value the more severe the impact on the daily functioning. The QOLRAD has been extensively documented in international studies in patients with heartburn with regard to reliability, validity [12] and responsiveness [4], assessing the impact of GERD on patients' HRQL. Previous studies have also revealed that a change of approximately 0.5 represents a clinically relevant change in the QOLRAD [17]. Its factor structure was also replicated in several translations [18].
Short-Form Health 36 (SF-36)
The SF-36 is an extensively used generic questionnaire containing 36 items clustered in eight dimensions. Item scores for each dimension are coded, summed and transformed to a scale from 0 (worst possible health state measured by the questionnaire) to 100 (best possible health state). The higher value indicates a better evaluation of health. The SF-36 is well documented in terms of reliability and validity in all available language versions [19, 20]. This study used the acute version of the SF-36, i.e. a one week recall period.
Hospital Anxiety and Depression scale (HAD)
The HAD consists of 14 items divided into two sub-scales for anxiety (7 items) and depression (7 items), in which the patient rates each item on a four-point scale. The higher scores indicate the presence of problems. A cut off of ≥ 11 implies definite cases, a cut off of 8–10 probable cases and ≤ 7 no cases. The validity and reliability of the HAD have been reported in several studies [21, 22].
All the above instruments have been translated and linguistically validated according to international guidelines [8]. The linguistic validation of a questionnaire is not a literal translation of the original questionnaire, but the production of a translation, which is conceptually equivalent to the original and culturally acceptable in the country in which the translation will be used. This translation process includes forward and backward translations by independent translators.
Administration of PRO instruments
All questionnaires were completed in an electronic data capture device (Apple Newton Pad). The method of using Electronic Data Capture (EDC) for HRQL studies has previously been shown to improve the quality of the data and to be well received by patients [23]. All study personal were trained to use the EDC and to instruct the patients in a standardized way for minimizing bias and enhancing compliance.
Psychometric evaluation of the instruments
Reliability
Internal consistency refers to the extent to which the items are interrelated. Cronbach's coefficient is one method of assessing internal consistency and is the method most widely used for this purpose. Cronbach's alpha was calculated [24] in each dimension of the instruments to assess the internal consistency reliability. A high alpha coefficient (≥ 0.70) suggests that the items within a dimension measure the same construct and supports the construct validity.
Test-retest reliability refers to the stability of a score derived from serial administrations of a measure by the same rater. Repeated measurements are made in the same individuals, presumably with a time interval long enough to ensure independence. Here, patients in the stable phase (between visits one and two) and in whom the treatment – not study mandated – remained unchanged were assessed. A reliability coefficient above 0.70 [10] is considered to be acceptable.
Construct validity
Construct validity is concerned with whether the indicator actually measures the underlying attribute. The construct validity of the GSRS and QOLRAD was examined by convergent, discriminant and known-groups validity.
Convergent validity consists of showing that a postulated dimension of the instrument correlates appreciably with all other dimensions that theory suggests should be related to it. Here, it was was examined by: a) correlating the QOLRAD and the GSRS; b) correlating the QOLRAD and the GSRS with the dimensions of SF-36; and c) correlating the QOLRAD and GSRS with the HAD and the clinician-assessed patient heartburn symptoms. Using Pearson's product moment correlation, similar dimensions in these instruments were expected to have high correlations with each other. A strong correlation was considered to be over 0.60, a moderate between 0.30 and 0.60 and a low (very low) correlation below 0.30 [25]. Low correlation was expected between those dimensions that are theoretically unrelated constructs, thereby testing the discriminant validity of the instruments. Correlating the QOLRAD and the GSRS with severity and frequency of heartburn symptoms also tested the discriminant validity of the instruments. Finally, known-groups validity [26] was also tested since a PRO instrument should be able to differentiate between groups of patients whose health status differs according to the characteristics of patients' disease, in this case heartburn severity and frequency [27]. Physician-assessed overall severity of symptoms and its relation to the QOLRAD dimensions were also evaluated.
In addition, the SF-36 summary scores were calculated for the physical component summary scale (PCS) and the mental component summary scale (MCS) based on German data (algorithm) [20] from the IQOLA project [28].
Finally, the HAD was used to evaluate the extent to which anxiety or depression correlates with the QOLRAD and the GSRS scores.
Statistical methods
Statistical analyses were performed utilizing the Statistical Analysis System (SAS, version 8.02) [29]. Test results are reported as significant for P < 0.0003, adjusted for multiplicity (Bonferroni's correction [30], 0.05/165). In the case of missing data in the PRO instruments, the mean of the completed items in one dimension was imputed to substitute the missing item provided that more than 50% of the items in one dimension were completed [31].
Results
Study population
A total of 142 patients (79 females) were included in the study. The diagnosis was verified at the discretion of the investigator when the patient fulfilled a history of episodes of heartburn for six months or longer with episodes of heartburn for one day or more during the last seven days prior to inclusion.
Patients' ages ranged from 19 to 79 with a mean of 47.5 years ± 14.6 (Table 1). For patients scheduled for the second visit (consecutive patients) there was no change in the treatment between visits 1 and 2 and the patients were in a stable phase. All participants were Caucasian, and 66 % were married. 62 % of patients was employed full-time. Further demographics and clinical characteristics of the patient population are shown in Table 1.
Patients were recruited with diverse severity of symptoms. The majority (70%) had moderate symptoms and 15 percent had either severe or mild heartburn symptoms. The frequency of symptoms was evenly distributed among those experiencing symptoms one to four days per week. Forty-six percent of the patients had symptoms more than five days a week.
The Gastrointestinal Symptom Rating Scale and the Quality of Life in Reflux and Dyspepsia questionnaire
Patients were bothered most by symptoms of 'Reflux' (Mean = 3.9), 'Indigestion' (Mean = 3.3) and 'Abdominal pain' (Mean = 3.0). The consequences of GI symptoms were reflected in the following dimensions of the QOLRAD: 'Food and Drink Problems' (Mean = 4.4); 'Vitality' (Mean = 4.6); 'Emotional Distress' (Mean = 5.0); and 'Sleep Disturbance' (Mean = 5.1), in that order. Hence, patients reported that, because of their symptoms, they could not eat and drink whatever they liked; their vitality was impaired; they were emotionally distressed; and they could not have a good night sleep.
Internal consistency reliability and test-retest reliability
Cronbach's alpha ranged from 0.53 (Abdominal Pain) to 0.91 (Diarrhea) in GSRS. In QOLRAD, the intercorrelations ranged from 0.90 (Vitality) to 0.94 (Emotional Distress) (Table 2), respectively.
The test-retest reliability in GSRS ranged from 0.49 (Abdominal Pain) to 0.72 (Constipation), in QOLRAD from 0.70 (Vitality domain), to 0.84, respectively (Emotional Distress and Food/Drink Problems domain) (Table 2).
Convergent and discriminant validity of Gastrointestinal Symptom Rating Scale and Quality of Life in Reflux and Dyspepsia
Pearson correlation coefficients were used to assess the convergent and discriminant validity (Table 3). There was a negative correlation between the Gastrointestinal Symptom Rating Scale and SF-36 in all domains. GSRS domains of 'Reflux' and SF-36 'Vitality' and 'Bodily Pain' were significantly correlated. The GSRS domains of 'Abdominal Pain' and 'Constipation' were significantly correlated with nearly all SF-36 domains in a negative direction. The relevant GSRS domains, 'Reflux', 'Abdominal Pain', and 'Indigestion', correlated significantly with all QOLRAD domains.
HAD scores yielded positive correlations between GSRS and anxiety, with significant correlations between anxiety and 'Abdominal pain' and 'Indigestion'. In addition, physician-assessed frequency of symptoms and the GSRS domain of 'Reflux' were significantly correlated.
QOLRAD correlated positively with all domains of the SF-36. The strongest correlations (>0.50) were found between QOLRAD 'Emotional Distress', 'Physical/Social functioning', and 'Vitality' and all SF-36 domains except for 'General health' and 'Bodily pain'. Furthermore, significant correlations were found between QOLRAD and anxiety and depression in a negative direction. Finally, QOLRAD and physician-assessed frequency of the symptoms significantly correlated in the expected (negative) direction (Table 3).
Known-groups validity of Gastrointestinal Symptom Rating Scale and Quality of Life in Reflux and Dyspepsia
All domains of the GSRS and QOLRAD questionnaires were able to differentiate between groups of patients whose health status differed according to the physician-assessed overall frequency and severity of heartburn, thereby confirming the known-groups validity of the instruments (Figures 1 and 2).
Discussion
Clear and consistent associations were found between the symptoms of heartburn and their impact on patients' HRQL. In agreement with these results, a recent German study reported that GERD patients with at least moderately severe reflux symptoms had reduced HRQL [32]. The relevance of the sample of patients was confirmed when patients reported that the most bothersome symptoms they had were heartburn and acid regurgitation (reflux), indigestion and abdominal pain, in that order. This finding is in accordance with previous descriptions of symptom patterns [2, 4, 33] in patient with GERD.
One of the most established, validated, reliable and responsive instruments available in this area is the QOLRAD [12], which has been proven to have excellent psychometric characteristics when tested in clinical trials [34, 35].
The primary goal of this study of documenting the psychometric characteristics of the German translation of the GSRS and QOLRAD was achieved. The reliability of the most relevant GSRS domain (Reflux) was satisfactory, but the 'Abdominal Pain' domain was not optimal. The low reliability of 'Abdominal Pain' may suggest that pain can be perceived differently from time to time and/or that pain intensity may vary considerably even during a shorter period of time. More research is needed to explore this issue. All domains of QOLRAD had excellent internal consistency and test-retest reliability.
The construct validity of GSRS and QOLRAD has also been documented. The relevant domain scores of the GSRS and QOLRAD significantly correlated. The GSRS domains of Abdominal Pain and Indigestion significantly (negatively) correlated with most of the domains of the SF-36. All QOLRAD domains correlated significantly with the domains of SF-36, thereby confirming the construct validity of QOLRAD. Known-groups validity was also proven; GSRS and QOLRAD did differentiate between patients with different frequency and severity of symptoms, which is comparable to previous findings [12, 36].
The moderate or low correlation between patient-reported and physician-assessed symptom frequency and severity indicates that symptom assessment should be balanced between clinician examination and patient report [12, 37].
In conclusion, the German translations of GSRS and QOLRAD are reliable and valid.
References
Velanovich V, Vallance SR, Gusz JR, Tapia FV, Harkabus MA: Quality of life scale for gastroesophageal reflux disease. J Am Coll Surg 1996, 183: 217–224.
Wiklund I: Quality of life in patients with gastroesophageal reflux disease. American Journal of Gastroenterology 2001, 96: S46–53. 10.1016/S0002-9270(01)02591-6
Moyer CA, Fendrick AM: Measuring health-related quality of life in patients with upper gastrointestinal disease. Dig Dis 1998, 16: 315–324. 10.1159/000016881
Talley NJ, Fullerton S, Junghard O, Wiklund I: Quality of life in patients with endoscopy-negative heartburn: reliability and sensitivity of disease-specific instruments. Am J Gastroenterol 2001, 96: 1998–2004. 10.1016/S0002-9270(01)02495-9
Symonds T, Berzon R, Marquis P, Rummans TA, Aaronson N, Barofsky I, Bonomi A, Bullinger M, Cappelleri JC, Cella D, Fairclough DL, Ferrans CE, Frost MH, Guyatt GH, Hays RD, Moinpour CM, Moynihan T, Norman G, Osoba D, Patrick D, Revicki D, Scott C, Sloan JA, Sprangers M, Varricchio C, Wong G, Wu A, Wyrwich K: The clinical significance of quality-of-life results: Practical considerations for specific audiences. Mayo Clinic Proceedings 2002, 77: 572–583.
Lohr K: Assessing health status and quality-of-life instruments: attributes and review criteria. Quality of Life Research 2002, 11: 193–205. 10.1023/A:1015291021312
Leidy NK, Revicki DA, Genesté B: Recommendations for evaluating the validity of quality of life claims for labeling and promoting. Value in Health 1999, 2: 113–127. 10.1046/j.1524-4733.1999.02210.x
Chassany O, Sagnier P, Marquis P, Fullerton S, Aaronson N: Patient-reported outcomes: The example of health-related quality of life - A European guidance document for the improved integration of health-related quality of life assessment in the drug regulatory process. Drug Information Journal 2002, 36: 209–238.
Guyatt GH, Feeny DH, Patrick DL: Measuring health-related quality of life. Ann Intern Med 1993, 118: 622–629.
Fitzpatrick R, Davey C, Buxton MJ, Jones DR: Evaluating patient-based outcome measures for use in clinical trials. Health Technology Assessment (Winchester, England) 1998, 2: i-74.
Svedlund J, Sjodin I, Dotevall G: GSRS--a clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Digestive Diseases & Sciences 1988, 33: 129–134.
Wiklund IK, Junghard O, Grace E, Talley NJ, Kamm M, Veldhuyzen van Zanten S, Pare P, Chiba N, Leddin DS, Bigard MA, Colin R, Schoenfeld P: Quality of Life in Reflux and Dyspepsia patients. Psychometric documentation of a new disease-specific questionnaire (QOLRAD). Eur J Surg Suppl 1998, 583: 41–49.
Ware J. E., Jr., Sherbourne CD: The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992, 30: 473–483.
Zigmond AS, Snaith RP: The hospital anxiety and depression scale. Acta Psychiatr Scand 1983, 67: 361–370.
Dimenas E, Glise H, Hallerback B, Hernqvist H, Svedlund J, Wiklund I: Well-being and gastrointestinal symptoms among patients referred to endoscopy owing to suspected duodenal ulcer. Scand J Gastroenterol 1995, 30: 1046–1052.
Dimenas E, Carlsson G, Glise H, Israelsson B, Wiklund I: Relevance of norm values as part of the documentation of quality of life instruments for use in upper gastrointestinal disease. Scand J Gastroenterol Suppl 1996, 221: 8–13.
Wiklund IK, Fullerton S, Junghard O, Talley NJ: Interpretability and meaningfulness of quality of life changes in patients with heartburn. Annual Meeting at Digestive Disease Week, the American Gastroenterological Association (AGA) San Diego, California 2000.
Kulich KR, Wiklund I, Junghard O: Factor structure of the quality of life in reflux and dyspepsia (QOLRAD) questionnaire evaluated in patients with heartburn predominant reflux disease. Quality of Life Research 2003, 6: 699–708. 10.1023/A:1025192100450
Ware JE, Kosinski M, Gandek B, Aaronson NK, Apolone G, Bech P, Brazier J, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M: The factor structure of the SF-36 Health Survey in 10 countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 1998, 51: 1159–1165. 10.1016/S0895-4356(98)00107-3
Ware JE, Gandek B, Kosinski M, Aaronson NK, Apolone G, Brazier J, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M, Thunedborg K: The equivalence of SF-36 summary health scores estimated using standard and country-specific algorithms in 10 countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 1998, 51: 1167–1170. 10.1016/S0895-4356(98)00108-5
Moorey S, Greer S, Watson M, Gorman C, Rowden L, Tunmore R, Robertson B, Bliss J: The factor structure and factor stability of the hospital anxiety and depression scale in patients with cancer. Br J Psychiatry 1991, 158: 255–259.
Herrmann C: International experiences with the Hospital Anxiety and Depression Scale-a review of validation data and clinical results. J Psychosom Res 1997, 42: 17–41. 10.1016/S0022-3999(96)00216-4
Drummond HE, Ghosh S, Ferguson A, Brackenridge D, Tiplady B: Electronic quality of life questionnaires: a comparison of pen-based electronic questionnaires with conventional paper in a gastrointestinal study. Qual Life Res 1995, 4: 21–26.
Cronbach LJ: Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16: 297–334.
Hinkle DE, Jurs SG, Wiersma W: Applied statistics for the behavioral sciences. 2nd -- Edition Boston, Houghton Mifflin 1988, xix, 682.
Kerlinger Fred N., Lee Howard B.: Foundations of behavioral research. 4th Edition Fort Worth, TX, Harcourt College Publishers 2000, xxv, 890, [82].
Fayers Peter M., Machin David: Quality of life: assessment, analysis and interpretation. Chichester, Wiley 2000, xii, 404.
Ware J. E., Jr., Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A: Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Medical Care 1995, 33: AS264–79.
SAS Institute Inc 8.02 Cary, NC, USA 2001.
Curtin F, Schulz P: Multiple correlations and Bonferroni's correction. Biological Psychiatry 1998, 44: 775–777. 10.1016/S0006-3223(98)00043-2
Halling K, Långström G, Wiklund I: Handling missing data in quality of life questionnaires: Experience from clinical trials. 6th Annual Conference of the International Society for Quality of Life Research, Barcelona, Spain 1999.
Hollenz M, Stolte M, Labenz J: Pravalenz der Refluxkrankheit in einer Allgemeinpraxis. Deutsche Medizinische Wochenschrift 2002, 127: 1007–1012. 10.1055/s-2002-28325
Havelund T, Lind T, Wiklund I, Glise H, Hernqvist H, Lauritsen K, Lundell L, Pedersen SA, Carlsson R, Junghard O, Stubberod A, Anker-Hansen O: Quality of life in patients with heartburn but without esophagitis: effects of treatment with omeprazole. Am J Gastroenterol 1999, 94: 1782–1789. 10.1016/S0002-9270(99)00262-2
Crawley J, Frank L, Joshua-Gotlib S, Flynn J, Frank S, Wiklund I: Measuring change in quality of life in response to Helicobacter pylori eradication in peptic ulcer disease: the QOLRAD. Dig Dis Sci 2001, 46: 571–580. 10.1023/A:1005655317121
Wahlqvist P, Carlsson J, Stalhammar NO, Wiklund I: Validity of a Work Productivity and Activity Impairment questionnaire for patients with symptoms of gastro-esophageal reflux disease (WPAI-GERD)-results from a cross-sectional study. Value in Health 2002, 5: 106–113. 10.1046/j.1524-4733.2002.52101.x
Glise H, Wiklund I: Health-related quality of life and gastrointestinal disease. Journal of Gastroenterology & Hepatology 2002, 17 Suppl: S72–84. 10.1046/j.1440-1746.17.s1.6.x
Slevin ML, Plant H, Lynch D, Drinkwater J, Gregory WM: Who should measure quality of life, the doctor or the patient? British Journal of Cancer 1988, 57: 109–112.
Acknowledgement
We owe special thanks to Uwe Schöning and Werner Marquardt, AstraZeneca Germany, for their support and assistance in this study.
This study was funded by AstraZeneca R&D, Mölndal, Sweden.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
IW conceived the study and KRK managed its design and coordination. JC was responsible for the statistical analysis. IW co-participated in the overall process.
PM, AM, JL, EB, SM, were the best recruiters of patients in the study and made comments to the draft manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kulich, K.R., Malfertheiner, P., Madisch, A. et al. Psychometric validation of the German translation of the Gastrointestinal Symptom Rating Scale (GSRS) and Quality of Life in Reflux and Dyspepsia (QOLRAD) questionnaire in patients with reflux disease. Health Qual Life Outcomes 1, 62 (2003). https://doi.org/10.1186/1477-7525-1-62
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7525-1-62