Abstract
Food allergies affect an estimated 3 to 4% of adults and up to 8% of children in developed western countries. Results from in vitro simulated gastric digestion studies with purified proteins are routinely used to assess the allergenic potential of novel food proteins. The digestion of purified proteins in simulated gastric fluid typically progresses in an exponential fashion allowing persistence to be quantified using pseudo-first-order rate constants or half lives. However, the persistence of purified proteins in simulated gastric fluid is a poor predictor of the allergenic status of food proteins, potentially due to food matrix effects that can be significant in vivo. The evaluation of the persistence of novel proteins in whole, prepared food exposed to simulated gastric fluid may provide a more correlative result, but such assays should be thoroughly validated to demonstrate a predictive capacity before they are accepted to predict the allergenic potential of novel food proteins.
Similar content being viewed by others
Background
The adult human gastrointestinal tract (GI) is a tube approximately 9 meters long, running through the body from the mouth to the anus. The lumen of the GI tract is continuous with the external environment, keeping its contents outside of the rest of the body. The epithelial layer, which lines the interior of the GI tract, presents a partial barrier to invasion by ingested pathogens, parasites, toxins and antinutrients. If pathogens, toxins and food proteins breach the epithelium barrier, the immune system acts as our primary defense system. Antibodies are formed that specifically react with epitopes on certain antigenic proteins, and subsequent binding of subtypes of these antibodies to proteins can result in the mobilization of host defenses, including deleterious responses like allergy.
The GI tract helps prevent food antigen penetration through its gut epithelial barrier. Epithelial cells are joined together with their neighbors via tight junctions and mucus produced by goblet cells [1]. In the upper bowel, the bulk of antigen exposure comes from foods, while in the lower bowel, the antigenic load comes from the complex microflora living in the GI tract. In addition to serving as a barrier, the mucosal system has two robust adaptive immune mechanisms to prevent general antigen circulation: (i) antigen exclusion mediated through the secretion of IgA and IgM antibodies to modulate the colonization of microorganisms and dampen penetration of soluble luminal agents, and (ii) suppressive mechanisms to avoid hypersensitivity to substances present in the mucosal surface [2]. The latter mechanism is known as oral tolerance when it is induced by food antigens [3].
Despite these host defense mechanisms, antigens can be absorbed and distributed in the body. Intact food proteins can be detected in plasma [4–6] and gut bacteria can be detected in mesenteric lymph nodes [7]. An estimated 3 to 4% of adults and up to 8% of children suffer from food allergies in developed western countries [8, 9]. In the western world, most infectious diseases of the gut are largely under control, yet food allergies are considered to be a major health concern. Food allergy accounts for up to 50% of anaphylactic episodes resulting in hospitalizations [10, 11].
Failure of oral tolerance leading to food allergies is most often due to an IgE-mediated hypersensitivity to a small subset of proteins found in milk, eggs, peanuts, fish, shellfish, soy, wheat and tree nuts [12]. Typical diets contain tens of thousands of different proteins, and efforts to understand the unique physiochemical and molecular properties of food allergens are ongoing [13–15].
The exact site of food absorption and allergy induction is still unknown. It is believed that most food allergens are absorbed in the intestines, prior to initiating an immune response, requiring proteins to move through the stomach in an immunologically intact form. Food protein can also enter the circulation through the oral mucosa [16, 17]. Certain disease conditions, such as celiac disease, can increase the amount of intact proteins in general circulation [18].
The majority of ingested food proteins break down as they travel through the GI tract. This occurs through the processes of digestion, where the food is exposed to the denaturing environment of hydrochloric acid in the stomach, bile from the liver and digestive enzymes released by the salivary glands, chief cells in the stomach, and the pancreas. The proteases and peptidases produced and secreted by chief cells and the pancreas digest proteins into small peptides typically less than 8 amino acids in size [19]. This extensive digestion renders these peptides non-reactive for antigen recognition [20]. For this reason, resistance to proteolysis has been considered a promising indicator of allergenic potential [21]. More recently Utersmayr and Jensen-Jarolim [22] have shown that antiulcer agents increase the risk of food allergy by interfering with the digestive function and decreasing the threshold of allergens required to elicit symptoms in patients with food allergy. Therefore, when the gastric digestion of a protein is impaired or limited, protein persistence increases, potentially triggering sensitization or allergic symptoms. This phenomenon is known as allergen persistence [22].
Based on the relationship between GI digestion and food allergy, results of in vitro digestion experiments have been considered to assess the allergenic potential of new food proteins. In this paper, we review the influence of gastric digestion on the development of food allergy, and evaluate the currently applied digestion assays for testing the allergenic potential of novel food proteins. We start by defining a food allergen, and then discuss the standard simulated gastric fluid digestion (SGF) assay currently used to assess allergenic potential of food proteins. We found that results from SGF assays with pure proteins are not a good predictor of the allergenic potential of food proteins, but rather that they simply measure the resistance of purified food proteins to in vitro digestion. Moreover resistance to SGF is not a sufficient or useful criterion for evaluating food allergen sensitization or induction.
What is a food allergen?
Before we discuss the use of digestion experiments for predicting the allergenic potential of food proteins, we must define a "food allergen". This term is general and ambiguous. Food allergens have at least three potential attributes:
-
(1)
Induction of allergic sensitization.
-
(2)
Reaction with IgE antibodies
-
(3)
Induction of allergic reactions.
The food proteins which do all three of the above are known as complete food allergens [23], while the others are called incomplete food allergens. Incomplete food allergens are divided into two categories [24]: (i) non-elicitors, which do (2), but not (1) or (3), and (ii) non-sensitizing elicitors, which do (2) and (3), but not (1). Bannon [25] suggests that complete allergens are resistant to digestion in the GI tract, while incomplete allergens are potentially susceptible to digestion in the GI tract [26, 27].
The standard digestion assay to assess allergenic potential of food proteins
Digestion assays in simulated gastric fluid (SGF) are commonly employed to predict the allergenic potential of food proteins [28–31], and are currently required as part of the allergenicity assessment of transgenic proteins expressed in food crops [32, 33]. Astwood et al. [34] used the SGF assays to investigate the stability of 25 food proteins to pepsin. The hypothesis was that food allergens would survive the acidic gastric environment and resist digestion by pepsin in the stomach to reach the intestinal mucosa and be absorbed, while non-allergens would not [35]. Astwood et al. [34] found that the stability to digestion is significant in the selected food allergens, and concluded that digestion is a valid parameter that distinguishes food allergens from non-allergens.
The simulated gastric fluid assay
As a result of the Astwood et al. [34] report, the SGF assay has been incorporated in the decision tree or weight-of-evidence approach to evaluate the allergenic potential of novel food proteins that may be present in food crops [32, 33]. The SGF assay has been standardized to facilitate comparisons among substrates [36]. This recipe specifies 0.32% pepsin in hydrochloric acid at a pH of 1.2. SGF was developed to provide a model system for mammalian monogastric digestion and has been used to evaluate the relative nutritional value of different protein sources, and the dissolution of pharmaceuticals [37, 38]. It is widely understood that the SGF assay does not actually replicate the gastric environment but only represents a standardized model system for proteolysis under acidic conditions. The SGF assay was first used to systematically evaluate the gastric stability of allergenic food proteins by Astwood et al. [34]. In this study, 0.017% protein substrate was incubated in SGF (0.32% pepsin, pH 1.2) at 37°C.
Pepsin is an aspartic protease generated from the auto-cleavage of pepsinogen under the acidic conditions in the stomach. Pepsin has broad substrate specificity, preferentially cleaving proteins at leucine, phenylalanine and tyrosine [39]. Pepsinolysis is generally very rapid unless hindered by the secondary or tertiary structure of the protein substrate [40–42]. The optimum pH for pepsinolysis is between 1.8 and 3.2, and pepsin is irreversibly denatured at pH 6 to 7 [39, 43]. This latter property of pepsin allows the SGF reaction to be stopped by neutralizing aliquots of the solution after different incubation periods. These aliquots can then be analyzed to track the digestion of substrate proteins.
The analytical tool generally used to track the digestion of substrate protein in SGF is sodium dodecyl polyacrylimide gel electrophoresis (SDS-PAGE). SDS-PAGE separates denatured proteins on polyacrylamide gels based primarily on molecular mass, and thus does not distinguish enzyme-bound from non-bound substrate. Proteins are visualized by staining with various dyes such as colloidal Coomassie brilliant blue. While the density of stained bands is generally directly proportional to the protein concentration for any given protein [31, 44, 45], different proteins have different propensities to bind stain [46]. Thus, the relative concentration of any given protein can be tracked through time, but comparisons of concentration across different proteins are not accurate based solely on band densities. It also follows that the minimum concentration that can be visualized on SDS-PAGE gels differs among different proteins. An example of the dramatic difference in protein staining between two proteins can be seen in Figure 3 in Thomas et al. [38]. In panel B of this figure, the pepsin to ovalbumin ratio is 3:1 w/w, however the ovalbumin band at time zero, prior to digestion, is much darker than the pepsin band.
In some cases, discrete smaller-molecular-weight protein fragments appear, and sometimes disappear, as digestion progresses [38, 47]. These digestion fragments may be capable of eliciting an allergic reaction if they have at least two IgE binding sites (epitopes) and are of sufficient size (> 3 kDa) such that the antibody-protein complex can cross-link two receptors on the surface of mast cells causing the cascade of effects leading to an allergic reaction [48]. It is noteworthy that when fragments are seen, they universally appear as discrete bands rather than as smears of many different molecular-weight peptides, indicating that specific fragments likely retain some level of secondary and/or tertiary structure that hinders pepsinolysis.
Patterns of digestion in the simulated gastric fluid assays
The SGF assays can produce complex patterns of digestions in SDS-PAGE gels. These patterns revolve around the multiple cleavage sites on the protein substrate rather than from the presence of multiple enzymes or compartments. However, the digestion of the substrate protein generally follows an exponential decline.
The SGF assay is similar to other dissipation experiments, which are conducted to track the disappearance of substrates in complex systems. One example is the tracking of pest-control substances in soil. Microbial digestion of compounds, via many enzymes, in soil often predominates in such systems, and in spite of the complexity of the processes, dissipation of substrate often closely follows a negative exponential pattern [49, 50]. Similarly, the clearance of pharmaceuticals from blood also is the result of complex processes often including enzyme catalyzed cleavage, but still generally follows an exponential decline pattern [51]. This same pattern has been observed in a number of in vitro protein-protease systems [52], particularly in proteolysis assays under acid-denaturing conditions [53] and pepsinolysis [42, 54]. The exponential decay pattern is sometimes biphasic but the final phase of digestion most often follows pseudo-first order kinetics [55]. The progress of the digestion seems to be quite insensitive to variation in both the pepsin concentration and the substrate protein concentration as long as the pepsin concentration is close to that specified in the USP (0.32%), and the substrate protein concentration is relatively low [31, 47, 56, 57].
There are four possible explanations for the biphasic and pseudo-first order decay pattern observed in proteolysis experiments: (i) Protein digestion is dominated by a first-order rate-limiting step. A possible rate-limiting step can be the acid-induced unfolding of the protein under the low pH (1.2) of SGF [42, 58]. Unfolding rates have often been found to be critical in proteolysis, and once unfolding occurs, pepsinolysis can proceed very quickly. This would result in apparent exponential disappearance of protein substrate in SGF. (ii) Protein digestion follows pseudo-first-order kinetics [59] under the excess of the digestive enzyme. This is the theory generally used to explain the first-order behavior of protein digestion in SGF [45, 52, 56, 57, 60, 61]. (iii) In protein digestion assays there is an exponential decay, which is only applicable to the slow transient of the digestion reaction at high enzyme concentrations. Schnell and Maini [62] and Tzafriri [63] have shown that enzyme catalyzed reactions can be described by a first-order kinetics after the initial transient of the reaction at high enzyme concentrations. (iv) The aggregate behavior of complex reactions, such as protein digestion, produces a behavior indistinguishable from the first-order kinetics [64]. Recent computational models have shown that the later theory (iv) provides a compelling explanation for the exponential decay in protein digestion assays [55].
Is it appropriate to assess the allergenic potential using digestion assays?
While the predictive power of the SGF assay has been promulgated in a number of papers [28–31], and is required as part of the allergenicity assessment of transgenic proteins expressed in food crops [32, 33], the predictive power of the assay remains uncertain [47, 54, 65, 66]. Using simulated SGF assays [36], Astwood et al. [34] originally found a good correlation between allergenic status and susceptibility to pepsin under acidic conditions. It was this work that initially prompted the use of the SGF assay to predict the allergenic potential of novel food proteins. However, Fu et al. [65] noticed a confounding factor in the Atwood et al. study. The cellular functions of the proteins evaluated in this investigation were correlated with the allergenic status of the proteins. When a group of allergens and non-allergens were chosen by the latter researchers that controlled for cellular function, the correlation was absent. More recently, Herman et al. [47] found no correlation between the digestibility and allergenic status of seven allergens and eight non-allergens.
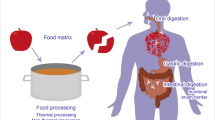
Likely reasons for the poor predictive capability of this assay include a lack of consideration of the prevalence of the allergen in food, effects of food processing, and food-matrix interactions [67–73]. The latter factor may be very important since components of food may sequester certain proteins away from the acid and pepsin in gastric fluid. For example, Polovic et al. [73] found that the purified kiwi allergen, Act c 2, was digested quickly in SGF, but was protected from digestion by fruit pectin both in vitro and in vivo. Similarly, Chikwamba et al. [67] found that transgenic corn expressing the Escherichia coli heat-labile enterotoxin facilitated the association of this protein with starch granules that protected it against digestion in SGF. Thus the evaluation of purified proteins in the SGF assay may be misleading.
Also there are a number of complete or potent allergens which are not stable in SGF assays [65, 66, 74], but their peptide fragments are recognizable by allergen-specific T cells [75]. Digestion outcomes can be influenced by the concentration of substrate protein or pepsin, pH and other factors [76]. Protein allergens of food sources like milk [77], fish [17, 78] and hazelnut [75] can be digested in vitro, unless the digestion process is inhibited by antacid medication [22]. In the later case, there is an increased risk of food allergy. The sudden increase of food allergy by inhibiting digestion suggests that the concentration of allergens reaching the intestinal mucosa is important in triggering an allergic reaction [79]. A similar phenomenon is observed with gastro-intestinal inflammation diseases, which can increase gut-permeability prior to food allergen contact [7]. This does not imply that allergens are more likely to be stable to digestion in simulated gastric fluid compared with non-allergens, but rather it suggests that if the concentration of a food allergen increases, then the chance of protein absorption is also higher. Once food allergens permeate the GI tract, they will stimulate the immune system to produce IgE antibodies, and degranulate mast cells upon subsequent contact leading to an allergic reaction.
Food allergies are complex, and can be the result of complex interactions. There are also food allergens which can only cause symptoms under cross-reactivity conditions. For example, pollen-allergic patients frequently present food allergies after the ingestion of several plant foods [24]. On the other hand, the mechanisms of how some patients with IgE to ovalbumin tolerate eggs, while others do not, remains unclear [23]. Digestion assays can neither predict the effects of cross-reactivity between food allergens and other antigens, nor the allergic response of a patient to food protein [80].
Conclusion
Although the value of comparing the stability of proteins in SGF for the purpose of evaluating the allergenic potential of novel food proteins is dubious, such comparisons are routinely used for this purpose. The nature of allergy to food proteins is still unknown. At the moment, we know that the resistance to in vivo digestion of an allergenic food protein increases its potential for causing an allergic reaction in susceptible individuals. We also know that some peptide fragments of digested proteins can be recognizable by allergen-specific T cells. However, the amount of food protein and the condition under which can trigger the allergic reaction are largely unknown [81].
Re-evaluating the application of simulated gastric fluid assay to test food proteins
The limitations of the SGF assays for predicting the allergenic potential are becoming apparent to the food allergy community [47, 54, 65, 66, 74]. In light of the limitations of the SGF assays, Utersmayr and Jensen-Jarolim [22] suggested the introduction of a new concept in the food allergen community: allergen persistence. Slow or impaired digestion of food proteins which are potential allergens increases the risk for food allergy induction in sensitized individuals. Although SGF assays with purified proteins cannot predict allergenic potential, they can quantitatively estimate the food protein persistence in the GI tract if food-matrix effects are not significant. If a novel food protein is an allergen, then a dose increase in the GI tract can exceed the threshold for triggering an allergic reaction in sensitized individuals. The typical protein absorption time correlates with gastric transit time determined for pharmaceutical compounds [82].
A kinetic approach to measuring SGF digestion is currently the most reasonable method to quantitatively compare the persistence of purified food proteins during in vitro digestion [42, 45, 47, 54, 56]. The digestion of proteins in SGF typically conforms to a negative-exponential model allowing first-order rate constants or half lives to characterize the disappearance of substrates over their dissipation profile. This approach provides an in vitro measure of the persistence of food proteins.
Apart from the quantitative estimates of protein persistence, other aspects of the SGF assay protocol can also be improved. The evaluation of the persistence of novel proteins in whole, prepared food exposed to SGF [83] may provide better estimates of in vivo persistence of food proteins. The proteolysis of food proteins can be affected as a result of processing and interaction with food ingredients. For example, β-lactoglobulin proteolysis by trypsin and chymotrypsin is reduced in the presence of polysaccharides such as gum arabic, low methylated pectin or xylan [84]. Peanut protein digestibility is also reduced in the presence of gum Arabic and xylan [85]. Finally new assays have been proposed to model more realistically the multi-phase nature of the digestive processes [75, 84, 86]. These digestion assays mimic the passage of the food into the stomach and then into the gut. The development of these digestion assays has demonstrated the importance of using physiologically relevant conditions to investigate the digestion of food proteins in vitro [69]. Some of these models have been recently reviewed in [76].
We emphasize that the persistence to SGF in vitro provides little value in the absence of evidence that a particular protein can induce IgE antibodies or elicit an allergic response. The allergenic potential of a food can only be diagnosed through sensitive analytical methods which recognize the presence of allergenic antigens in food. For novel food proteins, where populations of allergic individuals are absent or limited, results from SGF assays with pure proteins are of little value in predicting allergenicity. Continued work on new animal models of sensitization for food proteins will be of critical importance for accurately predicting the allergenicity of novel food proteins [87]. SGF assays should be employed for estimating protein persistence in vitro and isolating peptide fragments with potential allergenic epitopes. Therefore the assessment of food allergen requires the use of both digestion and immunology assays as a means to ensure consumer safety to food proteins.
References
Deplancke B, Gaskins HR: Microbial modulation of innate defense: goblet cells and the intestinal mucus layer. American Journal of Clinical Nutrition. 2001, 73: 1131S-1141S.
Brandtzaeg P: Current understanding of gastrointestinal immunoregulation and its relation to food allergy. Ann N Y Acad Sci. 2002, 964: 13-45.
Faria AMC, Weiner HL: Oral tolerance. Immunological Reviews. 2005, 206: 232-259. 10.1111/j.0105-2896.2005.00280.x
Brunner M, Walzer M: Absorption of undigested proteins in human beings: the absorption of unaltered fish proteins in adults. Arch Intern Med. 1928, 42: 173-179.
Husby S, Jensenius JC, Svehag SE: Passage of undegraded dietary antigen into the blood of healthy adults. Quantification, estimation of size distribution, and relation of uptake to levels of specific antibodies. Scandinavian Journal of Immunology. 1985, 22: 83-92. 10.1111/j.1365-3083.1985.tb01862.x
Husby S, Jensenius JC, Svehag SE: Passage of undegraded dietary antigen into the blood of healthy adults. Further characterization of the kinetics of uptake and the size distribution of the antigen. Scandinavian Journal of Immunology. 1986, 24: 447-455. 10.1111/j.1365-3083.1986.tb02133.x
MacDonald TT, Monteleone G: Immunity, inflammation, and allergy in the gut. Science. 2005, 307: 1920-1925. 10.1126/science.1106442
Kanny G, Moneret-Vautrin DA, Flabbee J, Beaudouin E, Morisset M, Thevenin F: Population study of food allergy in France. Journal of Allergy and Clinical Immunology. 2001, 108: 133-140. 10.1067/mai.2001.116427.
Sicherer SH, Munoz-Furlong A, Sampson HA: Prevalence of seafood allergy in the United States determined by a random telephone survey. Journal of Allergy and Clinical Immunology. 2004, 114: 159-165. 10.1016/j.jaci.2004.04.018.
Brown AFT, McKinnon D: Emergency department anaphylaxis: A review of 142 patients in a single year. Journal of Allergy and Clinical Immunology. 2001, 108: 861-866. 10.1067/mai.2001.119028.
Sampson HA: Food anaphylaxis. British Medical Bulletin. 2000, 56: 925-935. 10.1258/0007142001903607
Sampson HA: Food allergy. Part 1: Immunopathogenesis and clinical disorders. Journal of Allergy and Clinical Immunology. 1999, 103: 717-728. 10.1016/S0091-6749(99)70411-2.
Breiteneder H, Mills ENC: Molecular properties of food allergens. Journal of Allergy and Clinical Immunology. 2005, 115: 14-23. 10.1016/j.jaci.2004.10.022.
Hauser M, M E, Wallner M, Wopfner N, Schmidt G, Ferreira F: Molecular Properties of Plant Food Allergens: A Current Classification into Protein Families. The Open Immunology Journal. 2008, 1: 1-12.
Lehrer SB, Bannon GA: Risks of allergic reactions to biotech proteins in foods: perception and reality. Allergy. 2005, 60: 559-564. 10.1111/j.1398-9995.2005.00704.x
Dirks CG, Pedersen MH, Platzer MH, Bindsley-Jensen C, Skov PS, Poulsen LK: Does absorption across the buccal mucosa explain early onset of food-induced allergic systemic reactions?. Journal of Allergy and Clinical Immunology. 2005, 115: 1321-1323. 10.1016/j.jaci.2005.03.027.
Untersmayr E, Vestergaard H, Malling HJ, Jensen LB, Platzer MH, Boltz-Nitulescu G, Scheiner O, Skov PS, Jensen-Jarolim E, Poulsen LK: Incomplete digestion of codfish represents a risk factor for anaphylaxis in patients with allergy. Journal of Allergy and Clinical Immunology. 2007, 119: 711-717. 10.1016/j.jaci.2006.10.039.
Husby S, Foged N, Host A, Svehag SE: Passage of dietary antigens into the blood of children with celiac disease. Quantification and size distribution of absorbed antigens. Gut. 1987, 28: 1062-1072. 10.1136/gut.28.9.1062
Erickson RH, Kim YS: Digestion and absorption of dietary protein. Annual Review of Medicine. 1990, 41: 133-139. 10.1146/annurev.me.41.020190.001025
York IA, Goldberg AL, Mo XY, Rock KL: Proteolysis and class I major histocompatibility complex antigen presentation. Immunological Reviews. 1999, 172: 49-66. 10.1111/j.1600-065X.1999.tb01355.x
Berrens L: Digestion of atopic allergens with trypsin, α-chymotrypsin and pancreatic kallikrein, and influence of allergens upon the proteolytic and esterolytic activity of these enzymes. Immunochemistry. 1968, 5: 585. 10.1016/0019-2791(68)90094-3
Untersmayr E, Jensen-Jarolim E: The role of protein digestibility and antacids on food allergy outcomes. Journal of Allergy and Clinical Immunology. 2008, 121: 1301-1308. 10.1016/j.jaci.2008.04.025.
Aalberse RC: Food allergens. Environmental Toxicology and Pharmacology. 1997, 4: 55-60. 10.1016/S1382-6689(97)10042-4.
Vieths S: Allergenic cross-reactivity, food allergy and pollen. Environmental Toxicology and Pharmacology. 1997, 4: 61-70. 10.1016/S1382-6689(97)10043-6.
Bannon GA: What makes a food protein an allergen?. Current Allergy and Asthma Reports. 2004, 4: 43-46. 10.1007/s11882-004-0042-0.
Jensen-Jarolim E, Wiedermann U, Ganglberger E, Zurcher A, Stadler BM, Boltz-Nitulescu G, Scheiner O, Breiteneder H: Allergen mimotopes in food enhance type I allergic reactions in mice. Faseb Journal. 1999, 13: 1586-1592.
Vieths S, Scheurer S, Ballmer-Weber B: Current understanding of cross-reactivity of food allergens and pollen. Ann N Y Acad Sci. 2002, 964: 47-68.
Bannon G, Fu TJ, Kimber I, Hinton DM: Protein digestibility and relevance to allergenicity. Environmental Health Perspectives. 2003, 111: 1122-1124.
Bannon GA, Goodman RE, Leach JN, Rice E, Fuchs RL, Astwood JD: Digestive Stability in the Context of Assessing the Potential Allergenicity of Food Proteins. Comments on Toxicology. 2002, 8: 271-285. 10.1080/08865140214384.
Goodman RE, Vieths S, Sampson HA, Hill D, Ebisawa M, Taylor SL, van Ree R: Allergenicity assessment of genetically modified crops – what makes sense?. Nature Biotechnology. 2008, 26: 73-81. 10.1038/nbt1343
Ofori-Anti AO, Ariyarathna H, Chen L, Lee HL, Pramod SN, Goodman RE: Establishing objective detection limits for the pepsin digestion assay used in the assessment of genetically modified foods. Reg Toxicol Pharmacol. 2008, 52: 94-103. 10.1016/j.yrtph.2008.06.006.
EFSA, : Updated guidance document for the risk assessment of genetically modified plants and derived food and feed. The EFSA Journal. 2008, 727: 1-135.
Joint FAO/WHO Food Standard Programme, Twenty-Fifth Session. Rome, Italy: CODEX Alimentarius Commission; 2003.
Astwood JD, Leach JN, Fuchs RL: Stability of food allergens to digestion in vitro. Nature Biotechnology. 1996, 14: 1269-1273. 10.1038/nbt1096-1269
Lehrer SB, Horner WE, Reese G: Why are some proteins allergenic? Implications for biotechnology. Critical Reviews in Food Science and Nutrition. 1996, 36: 553-564.
USP: The United States Pharmacopeia 24. Simulated gastric fluid, TS. In The National Formulary Volume 19. Edited by: Trustees Bo. Rockville, MD: United States Pharmacopeial Convention, Inc; 2000:2235.
Azarmi S, Roa W, Lobenberg R: Current perspectives in dissolution testing of conventional and novel dosage forms. International Journal of Pharmaceutics. 2007, 328: 12-21. 10.1016/j.ijpharm.2006.10.001
Thomas K, Aalbers M, Bannon GA, Bartels M, Dearman RJ, Esdaile DJ, Fu TJ, Glatt CM, Hadfield N, Hatzos C, et al.: A multi-laboratory evaluation of a common in vitro pepsin digestion assay protocol used in assessing the safety of novel proteins. Regulatory Toxicology and Pharmacology. 2004, 39: 87-98. 10.1016/j.yrtph.2003.11.003.
Oka T, Morihara K: Specificity of pepsin: Size and property of the active site. FEBS Letters. 1970, 10: 222-224. 10.1016/0014-5793(70)80633-0
Fontana A, de Laureto PP, Spolaore B, Frare E, Picotti P, Zambonin M: Probing protein structure by limited proteolysis. Acta Biochimica Polonica. 2004, 51: 299-321.
Park C, Marqusee S: Probing the high energy states in proteins by proteolysis. Journal of Molecular Biology. 2004, 343: 1467-1476. 10.1016/j.jmb.2004.08.085
Herman R, Gao Y, Storer N: Acid-induced unfolding kinetics in simulated gastric digestion of proteins. Regulatory Toxicology and Pharmacology. 2006, 46: 93-99. 10.1016/j.yrtph.2006.05.010.
Kamatari YO, Dobson CM, Konno T: Structural dissection of alkaline-denatured pepsin. Protein Science. 2003, 12: 717-724. 10.1110/ps.0219903
Brussock SM, Currier TC: Use of sodium dodecyl-sulfate polyacrylamide gel electrophoresis to quantify Bacillus thuringiensis delta-endotoxins. ACS Symposium Series. 1990, 432: 78-87.
Herman RA, Schafer BW, Korjagin VA, Ernest AD: Rapid digestion of Cry34Ab1 and Cry35Ab1 in simulated gastric fluid. Journal of Agricultural and Food Chemistry. 2003, 51: 6823-6827. 10.1021/jf034290p.
Tal M, Silberstein A, Nusser E: Why does Coomassie Brilliant Blue R interact differently with different proteins? A partial answer. Journal of Biological Chemistry. 1985, 260: 9976-9980.
Herman RA, Woolhiser MM, Ladics GS, Korjagin VA, Schafer BW, Storer NP, Green SB, Kan L: Stability of a set of allergens and non-allergens in simulated gastric fluid. International Journal of Food Sciences and Nutrition. 2007, 58: 125-141. 10.1080/09637480601149640.
Huby RDJ, Dearman RJ, Kimber I: Why are some proteins allergens?. Toxicological Sciences. 2000, 55: 235-246. 10.1093/toxsci/55.2.235
Scow KM, Schmidt SK, Alexander M: Kinetics of biodegradation of mixtures of substrates in soil. Soil Biology & Biochemistry. 1989, 21: 703-708. 10.1016/0038-0717(89)90067-9.
Herman RA, Scherer PN: Comparison of linear and nonlinear regression for modeling the first-order degradation of pest-control substances in soil. Journal of Agricultural and Food Chemistry. 2003, 51: 4722-4726. 10.1021/jf034135a.
Dvorchik BH, Vesell ES: Pharmacokinetic interpretation of data gathered during therapeutic drug monitoring. Clinical Chemistry. 1976, 22: 868-878.
Vaintraub IA: Kinetics of the co-operative proteolysis. Nahrung-Food. 1998, 42: 59-60. 10.1002/(SICI)1521-3803(199804)42:02<59::AID-FOOD59>3.3.CO;2-N.
Vaintraub IA, Morari D: Applying the increase in rate constants of cooperative proteolysis to the determination of transition curves of protein denaturation. Journal of Biochemical and Biophysical Methods. 2003, 57: 191-201. 10.1016/S0165-022X(03)00106-4.
Herman RA, Storer NA, Gao Y: Digestion assays in allergenicity assessment of transgenic proteins. Environmental Health Perspectives. 2006, 114: 1154-1157.
Srividhya J, Schnell S: Why substrate depletion has apparent first-order kinetics in enzymatic digestion. Computational Biology and Chemistry. 2006, 30: 209-214. 10.1016/j.compbiolchem.2006.03.003.
Herman RA, Korjagin VA, Schafer BW: Quantitative measurement of protein digestion in simulated gastric fluid. Regulatory Toxicology and Pharmacology. 2005, 41: 175-184. 10.1016/j.yrtph.2004.12.004.
Imoto T, Yamada H, Ueda T: Unfolding rates of globular proteins determined by kinetics of proteolysis. Journal of Molecular Biology. 1986, 190: 647-649. 10.1016/0022-2836(86)90250-0
Noda Y, Fujiwara K, Yamamoto K, Fukuno T, Segawa S: Specificity of typsin digestion and conformational flexibility at different sites of unfolded lysozyme. Biopolymers. 1994, 34: 217-226. 10.1002/bip.360340208
Schnell S, Mendoza C: The condition for pseudo-first-order kinetics in enzymatic reactions is independent of the initial enzyme concentration. Biophysical Chemistry. 2004, 107: 165-174. 10.1016/j.bpc.2003.09.003
Terada S, Kato T, Izumiya N: Synthesis and hydrolysis by pepsin and trypsin of a cyclic hexapeptide containing lysine and phenylalanine. European Journal of Biochemistry. 1975, 52: 273-282. 10.1111/j.1432-1033.1975.tb03995.x
Irvine GB, Blumsom NL, Elmore DT: The kinetics of hydrolysis of some synthetic substrates containing neutral hydrophilic groups by pig pepsin and chicken liver cathepsin-D. Biochemical Journal. 1983, 211: 237-242.
Schnell S, Maini PK: Enzyme kinetics at high enzyme concentration. Bulletin of Mathematical Biology. 2000, 62: 483-499. 10.1006/bulm.1999.0163
Tzafriri AR: Michaelis-Menten kinetics at high enzyme concentrations. Bulletin of Mathematical Biology. 2003, 65: 1111-1129. 10.1016/S0092-8240(03)00059-4
Bandstra JZ, Tratnyek PG: Central limit theorem for chemical kinetics in complex systems. Journal of Mathematical Chemistry. 2005, 37: 409-422. 10.1007/s10910-004-1107-y.
Fu TJ: Digestion stability as a criterion for protein allergenicity assessment. Ann N Y Acad Sci. 2002, 964: 99-110.
Fu TT, Abbott UR, Hatzos C: Digestibility of food allergens and nonallergenic proteins in simulated gastric fluid and simulated intestinal fluid – A comparative study. Journal of Agricultural and Food Chemistry. 2002, 50: 7154-7160. 10.1021/jf020599h.
Chikwamba RK, Scott MP, Mejia LB, Mason HS, Wang K: Localization of a bacterial protein in starch granules of transgenic maize kernels. Proceedings of the National Academy of Sciences of the United States of America. 2003, 100: 11127-11132. 10.1073/pnas.1836901100
Takagi K, Teshima R, Okunuki H, Sawada J: Comparative study of in vitro digestibility of food proteins and effect of preheating on the digestion. Biological & Pharmaceutical Bulletin. 2003, 26: 969-973. 10.1248/bpb.26.969
Moreno FJ, Mackie AR, Mills ENC: Phospholipid interactions protect the milk allergen alpha-lactalbumin from proteolysis during in vitro digestion. Journal of Agricultural and Food Chemistry. 2005, 53: 9810-9816. 10.1021/jf0515227.
Tagliazucchi D, Verzelloni E, Conte A: Effect of some phenolic compounds and beverages on pepsin activity during simulated gastric digestion. Journal of Agricultural and Food Chemistry. 2005, 53: 8706-8713. 10.1021/jf058074n.
Weangsripanaval T, Moriyama T, Kageura T, Ogawa T, Kawada T: Dietary fat and an exogenous emulsifier increase the gastrointestinal absorption of a major soybean allergen, Gly m Bd 30K, in mice. Journal of Nutrition. 2005, 135: 1738-1744.
Peyron S, Mouecoucou J, Fremont S, Sanchez C, Gontard N: Effects of heat treatment and pectin addition on beta-lactoglobulin allergenicity. Journal of Agricultural and Food Chemistry. 2006, 54: 5643-5650. 10.1021/jf053178j.
Polovic N, Blanusa M, Gavrovic-Jankulovic M, Atanaskovic-Markovic M, Burazer L, Jankov R, Velickovic TC: A matrix effect in pectin-rich fruits hampers digestion of allergen by pepsin in vivo and in vitro. Clinical and Experimental Allergy. 2007, 37: 764-771. 10.1111/j.1365-2222.2007.02703.x.
Yagami T, Haishima Y, Nakamura A, Osuna H, Ikezawa Z: Digestibility of allergens extracted from natural rubber latex and vegetable foods. Journal of Allergy and Clinical Immunology. 2000, 106: 752-762. 10.1067/mai.2000.109171.
Vieths S, Reindl J, Muller U, Hoffmann A, Haustein D: Digestibility of peanut and hazelnut allergens investigated by a simple in vitro procedure. European Food Research and Technology. 1999, 209: 379-388. 10.1007/s002170050513.
Moreno FJ: Gastrointestinal digestion of food allergens: Effect on their allergenicity. Biomedicine & Pharmacotherapy. 2007, 61: 50-60. 10.1016/j.biopha.2006.10.005.
Untersmayr E, Bakos N, Scholl I, Kundi M, Roth-Walter F, Szalai K, Riemer AB, Ankersmit HJ, Scheiner O, Boltz-Nitulescu G, Jensen-Jarolim E: Anti-ulcer drugs promote IgE formation toward dietary antigens in adult patients. Faseb Journal. 2005, 19: 656-658.
Untersmayr E, Scholl I, Swoboda I, Beil WJ, Forster-Waldl E, Walter F, Riemer A, Kraml G, Kinaciyan T, Spitzauer S, et al.: Antacid medication inhibits digestion of dietary proteins and causes food allergy: A fish allergy model in Balb/c mice. Journal of Allergy and Clinical Immunology. 2003, 112: 616-623. 10.1016/S0091-6749(03)01719-6.
Untersmayr E, Jensen-Jarolim E: The effect of gastric digestion on food allergy. Current Opinion in Allergy and Clinical Immunology. 2006, 6: 214-219. 10.1097/01.all.0000225163.06016.93.
Metcalfe DD: Genetically modified crops and allergenicity. Nature Immunology. 2005, 6: 857-860. 10.1038/ni0905-857
Crevel RWR, Briggs D, Hefle SL, Knulst AC, Taylor SL: Hazard characterisation in food allergen risk assessment: The application of statistical approaches and the use of clinical data. Food Chem Toxicol. 2007, 45: 691-701. 10.1016/j.fct.2006.09.005
Kimura T, Higaki K: Gastrointestinal transit and drug absorption. Biological & Pharmaceutical Bulletin. 2002, 25: 149-164. 10.1248/bpb.25.149
Pasini G, Simonato B, Curioni A, Vincenzi S, Cristaudo A, Santucci B, Peruffo ADB, Giannattasio M: IgE-mediated allergy to corn: A 50 kDa protein, belonging to the Reduced Soluble Proteins, is a major allergen. Allergy. 2002, 57: 98-106. 10.1034/j.1398-9995.2002.1o3413.x
Mouecoucou J, Villaume C, Sanchez C, Mejean L: beta-lactoglobulin/polysaccharide interactions during in vitro gastric and pancreatic hydrolysis assessed in dialysis bags of different molecular weight cut-offs. Biochimica Et Biophysica Acta-General Subjects. 2004, 1670: 105-112. 10.1016/j.bbagen.2003.10.017.
Mouecoucou J, Villaume C, Sanchez C, Mejean L: Effects of gum arabic, low methoxy pectin and xylan on in vitro digestibility of peanut protein. Food Research International. 2004, 37: 777-783. 10.1016/j.foodres.2004.04.002.
Moreno FJ, Mellon FA, Wickham MSJ, Bottrill AR, Mills ENC: Stability of the major allergen Brazil nut 2S albumin (Ber e 1) to physiologically relevant in vitro gastrointestinal digestion. Febs Journal. 2005, 272: 341-352. 10.1111/j.1742-4658.2004.04472.x
Dearman RJ, Skinner RA, Herouet C, Labay K, Debruyne E, Kimber I: Induction of IgE antibody responses by protein allergens: inter-laboratory comparisons. Food and Chemical Toxicology. 2003, 41: 1509-1516. 10.1016/S0278-6915(03)00167-4.
Acknowledgements
We are grateful to Michelle Wynn (University of Michigan) for her critical comments. We also appreciate editorial comments offered by Barry Schafer, Mark Krieger and Penny Hunst (Dow AgroSciences LLC).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
SS declares that he has no competing interests. RAH is employed by Dow AgroSciences LLC which develops and markets agricultural products, including transgenic crops.
Authors' contributions
SS and RH collaborated on the conceptualization and preparation of the manuscript equally.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Schnell, S., Herman, R.A. Should digestion assays be used to estimate persistence of potential allergens in tests for safety of novel food proteins?. Clin Mol Allergy 7, 1 (2009). https://doi.org/10.1186/1476-7961-7-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-7961-7-1