Abstract
Background
Several studies have shown that common carotid intima-media thickness (IMT) is increased after radiotherapy (RT) to the head and neck. However, further studies are needed to define the exact mechanism of radiation-induced injury in large vessels, investigate the relationship between radiation dose and large vessel injury and evaluate the rate of progress of atherosclerosis in irradiated vessels.
Objectives
To investigate whether external irradiation to the carotid area has any effect on IMT of the common carotid artery in a group of patients who received RT vs control group matched for age, gender and race.
Methods
We studied 19 patients (10 male; 47.8 ± 17.4 years) during a 5-month period (January 2009-July 2009); they had completed RT with a mean of 2.9 years before (range: 1 month-6 years) The mean radiation dose to the neck in the irradiated patients was 41.2 ± 15.6 Gy (range: 25-70 Gy). Common carotid IMT was measured with echo-color Doppler. Nineteen healthy adult patients (10 male; 47.8 ± 17.6) were recruited as a control group.
Results
IMT was not significantly higher in patients when compared to the control group (0.59 ± 0.16 vs 0.56 ± 0.16 mm, p = 0.4). There was no significant difference between the two groups in relation to the absence (p = 0.7) or presence (p = 0.6) of vascular risk factors. Although the difference did not reach statistical significance (p = 0.1), the irradiated young patients (age ≤ 52 years) had IMT measurements higher (0.54 ± 0.08 mm) than the non-irradiated young patients (0.49 ± 0.14 mm). The mean carotid IMT increased with increasing doses of radiation to the neck (p = 0.04).
Conclusion
This study shows that increased IMT of the common carotid artery after RT is radiation-dose-related. Therefore it is important to monitor IMT, which can be used as an imaging biomarker for early diagnosis of cerebrovascular disease in patients who have had radiotherapy for treatment of cancer of the head and neck and who are at increased risk for accelerated atherosclerosis in carotid arteries.
Similar content being viewed by others
Introduction
Radiotherapy (RT) as a single modality or in combination with surgery has been widely used in the treatment of head and neck tumours for many years, and this has resulted in a marked improvement in survival of patients with these tumours, who previously had a dismal prognosis. Successful treatment increases survival but also puts the patient at risk of radiation-related side effects. Of these, vascular side effects are serious and may be life-threatening.
RT involving the head and neck or supraclavicular (SC) region necessarily include segments of the carotid artery. It has traditionally been accepted that the carotid is fairly resistant to the fibrosis and narrowing that are evident in smaller vessels undergoing comparable radiation exposure [1, 2]. However, several papers have described increasing frequency of stroke or transient ischemic attack after RT [3–8]. Increased common carotid intima-media thickness assessed by high frequency ultrasound is an early marker of atherosclerosis and a predictor of subsequent death from myocardial infarction and stroke [9].
Indeed, recent studies have shown that common carotid IMT is increased after RT to the head and neck [10–12]. However, the clinical relevance of these observations remains unknown, and further studies are essential to define the role of IMT as a non-invasive diagnostic tool for identifying subclinical vascular disease and estimating risk of future cardiovascular disease in long-term cancer survivors. Therefore, the aim of this study was to examine IMT in patients who received irradiation to the carotid arteries during radiotherapy vs. control group matched for age, gender and race, by using B-mode ultrasonography.
Patients and Methods
Patient population
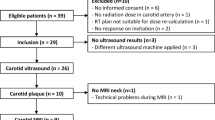
Over a 5-month period (January 2009-July 2009), we studied nineteen asymptomatic patients (47.8 ± 17.4 years) who had completed RT. Only patients who received radiation doses to the neck were selected. They were recruited from the follow-up activity of the Radiotherapy Division of "Perrino" Hospital, Brindisi, and were sent to the ultrasound laboratory at the Division of Cardiology of the same hospital. All the patients were studied for the common risk factors for atherosclerosis.
Ten patients were males (42.3 ± 15.9 years) and nine patients were women (54 ± 17.8 years). More than half of the patients (58%) were < 52 years old. Nine patients received RT symmetrically, on the left and right carotid.
Nineteen healthy adult patients (10 male; 47.8 ± 17.6) were recruited for the control group. They had no history of irradiation to the head and neck. Age, sex and race of the control group matched those of the irradiated group, while risk factors not were matched individually, but for frequency.
The risk factors were studied individually or by using a synthetic indicator, which analyzes the frequency of any risk factor or at least one risk factor in irradiated patients and in the control group.
None of the patients had a history of previous stroke or transient ischemic attack. Furthermore, patients with carotid plaques were excluded from the study for both groups. The maximum time elapsed between radiotherapy and ultrasound examination was 6 years, and the minimum time was 1 month. A complete history, including cardiovascular risk factors such as hypertension, diabetes, and dyslipidemia, was collected from all patients. Diabetes mellitus [13], arterial hypertension [14], hypertriglyceridemia and hypercholesterolemia [15]http://www.nhlbi.nih.gov/guidelines/cholestrol/index.htm.were defined according to standard definitions.
Current smokers were defined as patients with moderate or heavy cigarette use (at least 3 cigarettes per day) at the time of entry into the study. Former smokers were defined as the participants who had smoked regularly, at least 3 cigarettes/day, and who had quit smoking for at least 6 months at the time of enrolment. Non-smokers were defined as patients who had never smoked before admission. Smoker patients were the combined group of the past and current smokers. Accordingly, each risk factor was coded as either present or absent.
Carotid measurements
Carotid IMT of the arterial wall was determined using a Philips IE33 Ultrasound at high resolution, with 5-12 MHz linear array transducer. Patients were placed comfortably in the supine position with the head directed away from the side of interest and the neck extended slightly. Both common carotid arteries were examined along their full visible length. All measurements of IMT were made in the longitudinal plane at the point of maximum thickness on the far wall of the common carotid artery.
The carotid IMT assessment was supplemented by a thorough scan of the extracranial carotid arteries for the eventual presence of carotid plaques, to increase sensitivity for identifying subclinical vascular disease. The mean intima-media thickness was calculated using the semiautomated edge-detection software package (QLAB) 1 cm distant from the carotid arterial bifurcation. This is a program incorporated in the software package of the ultrasound equipment.
Statistical analysis
Data are expressed as means ± standard deviation. Differences in non-continuous variables were tested by χ2 analysis. Differences between the means of the two continuous variables were evaluated by Student's t-test. Regression analysis with Pearson's test was also used to evaluate the relationship between the two continuous variables. Multiple regression analyses were carried out with IMT values as dependent variables, and relevant parameters (radiation dose, age, vascular risk factors) as independent variables. The level of significance set at p < 0.05 was considered for all statistical analyses. Statistical analysis was performed using SAS statistical software (SAS Institute Inc, Cary, NC) versions 8.2 per Microsoft Windows.
Results
The demographic and clinical characteristics of the study population are reported in Table 1. Six patients in the control group did not present any risk factor (31.6%) and 13 patients had at least one risk factor (68.4%); five irradiated patients (26.3%) did not present any risk factor and fourteen patients (73.7%) had at least one risk factor.
Hypercholesterolemia was not significantly higher (21.1%) in irradiated patients than in control patients (10.5%, p = 0.37). Family history of cardiovascular or cerebrovascular diseases was higher in control patients (42.1%, p = 0.31) than in irradiated patients (26.3%), and diabetes was more frequent in control patients (15.5%) than in irradiated patients (5.3%, p = 0.29).
Over 70% of patients the control group and irradiated receiving no therapy and more than 20% of patients in both groups taking antihypertensive drugs.
Tumor type and RT dose are summarized in Table 2. All the patients received radiation doses to the neck in the range 25-70 Gy. The mean radiation dose to the neck in the irradiated patients was 41.2 ± 15.6 Gy. The median post-RT time was 1046 days (range 29-2492 days).
We also observed a higher IMT in males (0.61 ± 0.19 mm) compared to females (0.57 ± 0.13 mm) for irradiated carotid (p = 0.56). However, non-irradiated carotid IMT was higher in females (0.61 ± 0.16 mm) than in males (0.51 ± 0.15 mm) (p = 0.06). We did not find a significant association between carotid IMT and age in patient groups (p = 0.06); while the association was statistically significant in the control group (p < 0.0001).
IMT measurements of the irradiated carotid were not significantly higher in patients compared to control group (Table 3). There was no significant difference between the two groups in relation to the absence (p = 0.7) or presence (p = 0.6) of vascular risk factors. The irradiated young patients (age = 52 years) had IMT measurements higher (0.54 ± 0.08 mm) than the non-irradiated young patients (0.49 ± 0.14 mm). The difference was not statistically significant (p = 0.1), but suggested the existence of a relationship (Table 3). The mean carotid IMT increases with increasing radiation dose to the neck (p = 0.04) (Fig. 1). There was no linear correlation between the IMT and the post-RT time.
Discussion
This study shows that the IMT of the common carotid artery increases with increasing doses of radiation to the neck. Moreover, it is noteworthy that in our study a significant association with age was found only in healthy adult controls and not in cancer survivors. Interestingly, the irradiated young patients showed higher IMT measurements than the non-irradiated young patients.
Our findings are in agreement with previous observations. In a previous study, the median low cervical radiation dose was 38 Gy (range, 30-57 Gy) for those who developed carotid artery disease [16]. The minimal dose for RT damage of the cervical arteries was assumed to be 41 Gy [17]. A recent study has shown that there were two distinct subgroups of Hodgkin lymphoma survivors who developed non-coronary atherosclerotic vascular disease. The first group is an older population with probable pre-existing disease either unaffected or only accelerated by radiation. These patients experienced strokes and TIAs, were older at RT exposure (median age, 51 years), and had a relatively short time interval (median, 5.6 years) from RT to development of vascular disease. The second group differs in that the patients were younger (median, 20 years) at RT exposure, and had a longer latency period before diagnosis (median, 20.8 years) [16].
Radiotherapy to the neck is believed to predispose to atherosclerosis. Recently, irradiation of the neck has been associated with subsequent vascular wall thickening [18], accelerated atherosclerotic plaque formation [19], decreased flow on ultrasound [20], and coronary artery stenosis [21]. A recent study found that irradiation of the neck of Hodgkin (H) and non-Hodgkin (NH) patients determines a greater IMT of the arterial wall than in controls matched for the classic atherosclerosis risk factors, so authors concluded that radiotherapy can influence the atherosclerotic process [22, 23].
On the other hand, some researchers have documented no increase in clinical cerebrovascular events (CVEs) after SC RT [24, 25], in breast cancer patients.
The exact mechanism of radiation injury remains uncertain. Injury to the vasa vasorum and consequent ischemic lesions of the arterial wall were thought to be morphological features distinguishing radiation-induced arterial injury from spontaneous atherosclerosis [26–29].
Many factors have been associated with increased risk of developing atherosclerosis--for example, increasing age, diabetes mellitus, hypertension, hypercholesterolemia, smoking and irradiation to the affected vessels [30].
It has been assumed that the carotid lesion in an irradiated artery arises from an accelerated atherosclerotic process, and the patient's subsequent risk of stroke would be similar to those who did not receive radiation but with an equivalent degree of luminal stenosis [31, 32].
The potential for stroke is well-recognized in patients with head and neck cancer and is generally considered a risk related to pre-existing atherosclerotic disease. Since the IMT of the common carotid artery is a good predictor of stroke [33], data from other reports should heighten awareness that patients who have had radiotherapy for treatment of head and neck malignancy are at increased risk of accelerated atherosclerosis in carotid arteries, which in turn can lead to cerebrovascular accidents. As most patients with early changes in post-radiation carotid injury remain asymptomatic, early detection and monitoring are possible by routine ultrasound examination and measurement of the IMT of common carotid arteries.
Hypertension, diabetes mellitus, hypercholesterolemia and obesity are known to exacerbate the severity and speed of atherosclerosis. Effective management of these modifiable factors with appropriate changes in lifestyle may halt or slow the development of severe atherosclerosis leading to carotid stenosis or cerebrovascular events. Meanwhile, we recommend a higher level of alert and routine surveillance with ultrasonography in all patients with carotid artery stenosis induced by radiation therapy. However, recommendation of a routine exam certainly does not derive from our small number of patients, but is based on several previously-mentioned studies.
The study limitations were the small number of patients, the variable time interval from RT to vascular ultrasound, and lack of pre-RT baseline. Another restriction is the lack of follow-up in one patient. Additional studies are needed on a larger number of patients for early detection of the IMT changes as a predictive sign of atherosclerotic risk in irradiated patients.
The most important clinical implication is establishing appropriateness of indications for radiotherapy to the neck, especially in younger patients.
References
Levinson SA, Close MB, Ehrenfeld AX, et al.: Carotid artery occlusive disease following external cervical irradiation. Arch Surg. 1973, 107: 395-7.
Shariat M, Alias NA, Biswal BM: Radiation effects on the intima-media thickness of the common carotid artery in post-radioterapy patients with head and neck malignancy. Med J. 2008, 84: 609-612.
Smith GL, Smith BD, Buchholz TA, Giordano SH, Garden AS, Woodward WA, et al.: Cerebrovascular disease risk in older head and neck cancer patients after radiotherapy. J Clin Oncol. 2008, 26: 30-
Nilsson G, Holmberg L, Garmo H, Terent A, Blomqvist C: Increased incidence of stroke in women with breast cancer. Eur J Cancer. 2005, 41: 423-9. 10.1016/j.ejca.2004.11.013.
Bowers DC, McNeil DE, Liu Y, Yasui Y, Stovall M, Gurney JG, et al.: Stroke as a late treatment effect of Hodgkin's Disease: a report from the childhood cancer survivor study. J Clin Oncol. 2005, 23: 6508-15. 10.1200/JCO.2005.15.107.
Moser EC, Noordijk EM, van Leeuwen FE, le Cessie S, Baars JW, Thomas J, et al.: Long-term risk of cardiovascular disease after treatment for aggressive non-Hodgkin lymphoma. Blood. 2006, 107: 2912-9. 10.1182/blood-2005-08-3392.
Dorresteijn LD, Kappelle AC, Boogerd W, Klokman WJ, Balm AJ, Keus RB, et al.: Increased risk of ischemic stroke after radiotherapy on the neck in patients younger than 60 years. J Clin Oncol. 2002, 20: 282-8. 10.1200/JCO.20.1.282.
Jagsi R, Griffith KA, Koelling T, Roberts R, Pierce LJ: Stroke rates and risk factors in patients treated with radiation therapy for early-stage breast cancer. J Clin Oncol. 2006, 24: 2779-85. 10.1200/JCO.2005.04.0014.
O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK: Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999, 340: 14-22. 10.1056/NEJM199901073400103.
Sidhu PS, Naoumova RP, Maher VMG, et al.: The extracranial carotid artery in familial hypercholesterolaemia: relationship of intimal-medial thickness and plaque morphology with plasma lipids and coronary heart disease. J Cardiovasc Risk. 1996, 3: 61-7. 10.1097/00043798-199602000-00009.
Shariat M, Alias NAA, Biswal BM: Radiation effects on the intima-media thickness of the common carotid artery in post-radiotherapy patients with head and neck malignancy. Postgrad Med J. 2008, 84: 609-612. 10.1136/pgmj.2008.068569.
Cheng Stephen, FRCS MS, Ting Albert: Carotid Stenosis After Radiotherapy for Nasopharyngeal Carcinoma. Arch Otolaryngol Head Neck Surg. 2000, 126: 517-521.
World Health Organization, Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications:: Report of a WHO Consultation. Part I: Diagnosis and Classification of Diabetes Mellitus WHO/NCD/NCS/99.2. World Health Organisation, Geneva. 1999
European Society of Hypertension-European Society of Cardiology: Guidelines for the management of arterial hypertension. J Hypertens. 2003, 21: 1011-1053. 10.1097/00004872-200306000-00001.
National Cholesterol Education Program Expert Panel, Third Report of the Expert Panel on Detection: Evaluation and Treatment of High Blood Cholesterol in Adults. (Adult Treatment Panel III).http://www.nhlbi.nih.gov/guidelines/cholestrol/index.htm
Hull Matthew, Morris Christopher, Pepine Carl, et al.: Valvular Dysfunction and Carotid, Subclavian, and Coronary Artery Disease in Survivor of Hodgkin Lymphoma Treated with Radiation Therapy. JAMA. 2003, 290: 2831-2837. 10.1001/jama.290.21.2831.
Graus F, Rogers LR, Posner JB: Cerebrovascular complications in patients with cancer. Medicine. 1985, 64: 16-35. 10.1097/00005792-198501000-00002.
Dorresteijn LD, Kappelle AC, Scholz NMJ, Munneke M, Scholma JT, Balm AJM, et al.: Increased carotid wall thickening after radiotherapy on the neck. Eur J Cancer. 2004, 41: 1026-30. 10.1016/j.ejca.2005.01.020.
Fonkalsrud EW, Sanchez M, Zerubavel R: Serial changes in arterial structure following radiation therapy. Surg Gynecol Obstet. 1977, 145: 395-400.
Woodward WA, Durand JB, Tucker SL, Strom EA, Perkins GH, Oh J, et al.: Prospective analysis of carotid artery flow in breast cancer patients treated with supraclavicular irradiation 8 or more years previously. Cancer. 2008, 112: 268-73. 10.1002/cncr.23172.
Woodward WA, Woodward Wendy, Durand Jean, Tucker Susan, Strom Eric, Perkins George, Oh Julia, Arriaga Lisa, Domain Delora, Buchholz Thomas: Prospective Analysis of Carotid Artery Flow in Breast Cancer Patients Treated With Supraclavicular Irradiation 8 or More Years Previously. Cancer. 2008, 112: 268-73. 10.1002/cncr.23172.
Bilora F, Pietrogrande F, Petrobelli F, Polato G, Pomerri F, Muzzio PC: Is radiation a risk factor for atherosclerosis? An echo-color Doppler study on Hodgkin and non Hodgkin patients. Tumori. 2006, 92: 295-8.
Bilora F, Pietrogrande F, Campagnolo E, Rossato A, Polato G, Pomerri F, Muzzio PC: Are Hodgkin and non-Hodgkin patients at a greater risk of atherosclerosis? A follow-up of 3 years. Eur J Cancer Care (Engl). 2009
Walman B, Salvian A, Hay JH: Carotid artery stenosis in asymptomatic patients who have received unilateral head-and-neck irradiation. Int J Radiat Oncol Biol Phys. 2005, 63: 1197-205.
Brown PD, Foote RL, McLaughlin MP, et al.: A historical prospective cohort study of carotid artery stenosis after radiotherapy for head and neck malignancies. Int J Radiat Oncol Biol Phys. 2005, 63: 1361-7. 10.1016/j.ijrobp.2005.05.046.
Scott Apryl, Parr Luke, Johnstone Peter: Risk of cerebrovascular events after neck and supraclavicular radiotherapy: A systematic review. Radiotherapy and Oncology. 2009, 90: 163-165. 10.1016/j.radonc.2008.12.019.
Zidar N, Ferluga D, Hvala A, et al.: Contribution to the pathogenesis of radiation induced injury to large arteries. J Laryngol Otol. 1997, 111: 988-90. 10.1017/S0022215100139167.
Cheng Stephen, Ting Albert, Wu Lisa: ltrasonic Analysis of Plaque Characteristics and Intimal-medial Thickness in Radiation-induced Atherosclerotic Carotid Arteries. Eur J Vasc Endovasc Surg. 2002, 24: 499-04. 10.1053/ejvs.2002.1752.
Jurado Javier, Bashir Riyaz, Burket Mark: Radiation-Induced Peripheral Artery Disease. Catheterization and Cardiovascular Interventions. 2008, 72: 563-568. 10.1002/ccd.21681.
Sidhu PS, Naoumova RP, Maher VMG, et al.: The extracranial carotid artery in familialhypercholesterolaemia: relationship of intimal-medial thickness and plaque morphology with plasma lipids and coronary heart disease. J Cardiovasc Risk. 1996, 3: 61-7. 10.1097/00043798-199602000-00009.
Mathiesen EB, Bonaa KH, Joakimsen O: Echolucent plaques are associated with high risk of ischemic cerebrovascular events in carotid stenosis. The Tromso Study. Circulation. 2001, 103: 2171-2175.
Cheng SW, Ting AC, Ho P, Wu L: Accelerated progression of carotid stenosis in patients with previous external neck irradiation. J Vasc Surg. 2004, 39: 409-15. 10.1016/j.jvs.2003.08.031.
Chambless LE, Folsom AR, Clegg LX, et al.: arotid wall thickness is predictive of incident clinical stroke: the Atherosclerosis Risk in Communities (ARIC) study. Am J Epidemiol. 2000, 151: C478-87.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MEG performed the carotid Doppler examinations and drafting of the manuscript; EAG participated in data collection and performed the statistical analysis; FT partecipated in patient recruitment and in data collection; MGA participated in the statistical analysis of the results and critically revised the manuscript; MP played a main role in the design and coordination of the study, and in writing of the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Gianicolo, M.E., Gianicolo, E.A.L., Tramacere, F. et al. Effects of external irradiation of the neck region on intima media thickness of the common carotid artery. Cardiovasc Ultrasound 8, 8 (2010). https://doi.org/10.1186/1476-7120-8-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-7120-8-8