Abstract
Background
Lipoprotein associated phospholipase A2 (Lp-PLA2) is a novel biomarker for cardiovascular risk prediction. Whether increased Lp-PLA2 level is associated with re-stenosis after stent-placement is unclear.
Methods
Totally 326 participants eligible for stent-placement were enrolled and divided into two groups according to baseline Lp-PLA2 levels (named normal and elevated groups). Baseline characteristics and clinical outcomes were compared between normal and elevated groups. The relationships between Lp-PLA2 and other risk factors with re-stenosis were evaluated.
Results
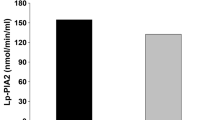
Only the between-group difference of Lp-PLA2 was significant (123.2 ± 33.6 ng/mL vs 336.8 ± 85.4 ng/mL, P < 0.001) while other demographic and clinical characteristics between these two groups were comparable. Approximately 55.1% and 58.5% of participants in normal and elevated groups presented with acute coronary syndrome, and the percentage of tri-vessels stenoses was significantly higher in elevated group (40.8% vs 32.1%, P = 0.016). Nearly 96.0% and 94.0% of participants in normal and elevated Lp-PLA2 groups were placed with drug-eluting stents, and the others were with bare-metal stents. After 1 year’s follow-up, the incidence of clinical end-points was comparable (13.3% vs 15.4%, P = 0.172). Nevertheless, the incidence of re-stenosis was marginally higher in elevated Lp-PLA2 group (8.5% versus 4.6%, P = 0.047). With multivariate analysis, after adjustment for other risk factors, Lp-PLA2 remained an independent predictor for re-stenosis with a hazard ratio of 1.140. No synergistic effect between Lp-PLA2 and other risk factors for re-stenosis was found.
Conclusion
Increased Lp-PLA2 level is associated with an increased risk of re-stenosis. Lp-PLA2 assessment may be useful in predicting subjects who are at increased risk for re-stenosis.
Similar content being viewed by others
Introduction
Atherosclerotic cardiovascular diseases (CAD), in terms of coronary heart disease (CHD), ischemic stroke and peripheral vascular disease, are still the leading causes of morbidity and mortality worldwide [1, 2]. Currently, it has been well documented that inflammatory reaction plays critical roles on the initiation and progression of atherosclerosis and CHD [3, 4]. Lipoprotein associated phospholipase A2 (Lp-PLA2), an enzyme excreted by inflammatory cells such as macrophages, nowadays has raised many concerns owing to its highly sensitive and specific features for vascular inflammation [5, 6]. Previously, some basic research show that Lp-PLA2 plays casual role on atherosclerosis and inhibiting Lp-PLA2 ameliorates vascular inflammation and deters atherosclerosis progression [7, 8]. Furthermore, some epidemiological studies and meta-analyses also consistently show that increased plasma level of Lp-PLA2 is associated with increased risk of cardiovascular events [9–12]. In light of these findings, Lp-PLA2 has been recognized as a novel and important predictor for cardiovascular risk assessment [13, 14].
Currently, percutaneous coronary intervention (PCI) is the preferred choice for patients with acute myocardial infarction or with significant coronary artery stenoses. Nevertheless, despite dual anti-platelet and intensive statins therapy, the incidence of re-stenosis after stent placement is still high [15, 16]. Therefore, identifying a specific and sensitive biomarker for predicting re-stenosis is of paramount importance. Owing to the significant and unequivocal implications of Lp-PLA2 on the initiation and progression of atherosclerosis and CAD, we speculated that increased plasma level of Lp-PLA2 at baseline might contribute to re-stenosis in patients with stent placement. If finally corroborated, we believed that in the future lowering Lp-PLA2 level with its specific antagonist would definitely reduce the risk of re-stenosis and doubtless improve the outcomes of patient with CAD.
Method
Study population and protocol
Current study was started in September of 2011 and ended in September of 2012. All participants were without previous history of atherosclerotic cardiovascular diseases. After angiographic evaluation, patients diagnosed as significant CHD and eligible for stent-placement were enrolled after written informed consent was obtained. Baseline demographic and clinical characteristics including traditional risk factors and laboratory results were collected. All participants were followed-up for 1 year via outpatient visit or telephone contact for detecting the first episode of pre-specified clinical outcomes.
Routine laboratory parameters and Lp-PLA2 measurements
Fasting blood samples were drawn by veni-puncture in the morning. Measurements of routine laboratory parameters in current study were consistent to previous study report unless otherwise mentioned [17]. Plasma level of Lp-PLA2 was detected with commercial Lp-PLA2-ELISA kit (PLAC test; supplied by dia Dexus Inc, South San Francisco, California). All the procedures were performed according to the manufactures’ instructions. Based on previous recommendation [18], plasma Lp-PLA2 level less than 200 ng/mL is defined as within normal range, while equal or higher than 200 ng/mL is recognized as elevation. All participants were divided into two groups on the basis of the plasma level of Lp-PLA2.
Clinical outcomes assessments post-stent placement
Clinical outcomes were defined as cardiovascular related death, nonfatal myocardial infarction, nonfatal ischemic stroke, and re-stenosis (> 50% stenosis of target lesion) by angiographic examination. Comparisons of clinical outcomes were conducted between groups with normal or elevated plasma levels of Lp-PLA2 during the 1 year’s follow-up. Risk factors for re-stenosis after 1 year’s follow-up were also evaluated.
Statistical analysis
Continuous variable was presented as mean ± SD or median appropriately, and compared by the Student’s t-test when data was normally distributed, otherwise compared by Wilcoxon rank-sum test. Categorical data was showed as percentage and compared by χ2 test. Univariate and multivariate Cox proportional hazard regression were used to evaluate the associations between baseline demographic and clinical characteristics and incidence of re-stenosis after 1 year’s follow-up. Variables with p values < 0.10 were entered into multivariable model and variables with p values < 0.10 were stayed in the model. Synergistic effects between other risk factors and Lp-PLA2 for re-stenosis were also evaluated. Statistical analyses were performed by using SPSS software version 16.0 (SPSS, Inc., Chicago, Illinois). A value of p <0.05 was considered significant.
Results
Baseline demographic and clinical characteristics of participants
A total of 326 participants were enrolled in our current study, and accordingly, were divided into two groups on the basis of baseline plasma levels of Lp-PLA2. As presented in Table 1, only the difference of plasma Lp-PLA2 level between the normal and elevated groups achieved statistical significance. Male patients were predominant and accounted for 66.3% and 65.4% in each group, respectively. More than 50.0% of patients in each group have a history of hypertension. Each group had nearly 20% of patients with diabetes mellitus, and 29 (85.3%) patients in normal Lp-PLA2 group and 20 (83.3%) patients in elevated Lp-PLA2 group were treated with insulin and the rest (14.7% vs 16.7%, P = 0.283) were treated with sulfonylureas. More than 40.0% of participants in both groups have a family history of atherosclerotic cardiovascular diseases. Notably, in both groups, baseline levels of Hs-CRP were increased, and no significant differences were found across other risk factors such as total cholesterol, LDL-C, HDL-C and Lp(a) levels in both groups.
Angiographic characteristics and clinical presentations of participants
As shown in Table 2, participants in Lp-PLA2 elevated group more frequently presented with emergency conditions such as unstable angina and acute myocardial infarction than the normal Lp-PLA2 group (58.5% vs 55.1%). Moreover, the percentage of three vessels stenoses was higher in elevated Lp-PLA2 group than normal Lp-PLA2 group (40.8% vs 32.1%).
Clinical outcome evaluation after 1 year’s follow-up
Approximately 96.0% (188) and 94.0% of participants (122) in normal and elevated Lp-PLA2 groups were placed with drug-eluting stents (DES), and the others were with bare-metal stents (BMS). During 1 year’s follow-up, all participants were adherent to dual anti-platelet (aspirin plus clopidogrel) and statins (atorvastatin or rosuvastatin) therapies. Other medications such as beta-receptor blockers, angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker, and medications for hypertension or glucose control were prescribed accordingly, and no between-group differences were found. The incidence of clinical outcomes was comparable between normal and elevated Lp-PLA2 groups (13.3% versus 15.4%, P = 0.172, see Table 3). Moreover, each pre-specified outcome was further evaluated and only the incidence of re-stenosis was slightly but significantly higher in elevated Lp-PLA2 group than that of normal Lp-PLA2 group (8.5% vs 4.6%, P = 0.047).
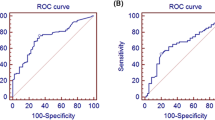
Univariate and multivariate analysis for incidence of re-stenosis after 1 year’s follow-up and evaluation of synergistic effect
For further evaluating the value of each parameter for the prediction of re-stenosis after 1 year’s stent-placement, univariate and multivariate analyses were conducted. As showed in Table 4, several variables were found associated with re-stenosis after 1 year’s stent-placement with univariate analysis. However, with multivariate analysis, after adjustment for variables such as age, smoking, hypertension, total cholesterol, Lp(a), Hs-CRP, anti-platelet and medications for hypertension, only diabetes mellitus, LDL-C and Lp-PLA2 were found increasing hazard ratio for re-stenosis, whereas statins and medications for diabetes mellitus were found beneficial for reducing the incidence of re-stenosis (See Table 5). Synergistic effects between Lp-PLA2 and other risk factors for re-stenosis were evaluated by Cox proportional hazard regression and all values of P were higher than 0.05.
Discussion
Importantly, our current study shows that increased plasma level of Lp-PLA2 at baseline is associated with an increased risk for re-stenosis after 1 year’s stent placement. Moreover, patients with increased Lp-PLA2 level more frequently present with urgent situations such as unstable angina and acute myocardial infarction, which is consistent with previous findings that higher Lp-PLA2 level is strongly associated with a higher incidence of plaque rupture and major adverse events [19, 20]. Additionally, our study also reveals that although a vast majority of patients present with Hs-CRP elevation, increased Hs-CRP level at baseline is not associated with re-stenosis after adjustment for other risk factors, and no synergistic effects between Lp-PLA2 and other risk factors for re-stenosis is found in current study.
Notably, in the past decades, the outcomes of patients with acute coronary syndrome have been significantly improved by stent placement, and with its excellent features of less invasive and highly efficient, PCI has become the principal therapy for patients with significant CHD [21–23]. However, the incidence of re-stenosis after PCI is still high in spite of prolongation of dual anti-platelet therapy and intensive statin treatment [15, 24]. Many mechanisms have been identified responsible for this phenomenon. For example, endothelial dysfunction and activation, smooth muscle cells migration and proliferation, as well as continuous vascular inflammation have been demonstrated that individually and/or simultaneously contribute to in-stent re-stenosis [25, 26].
Accordingly, Lp-PLA2 is an enzyme predominantly produced by leukocytes within atherosclerotic plaques and then excretes into circulation system [27, 28]. It has now been well documented that plasma level of Lp-PLA2 is highly correlated with the concentration of Lp-PLA2 within the plaques [29]. Therefore, evaluating plasma level of Lp-PLA2 could accurately and promptly reflect the severity of vascular inflammation. Owning to its value of adding prognostic information to traditional risk evaluation algorithm, measurement of Lp-PLA2 has been recommended to patients with moderate or high cardiovascular risk [18, 30]. However, whether increased plasma level of Lp-PLA2 is associated with an increased risk of re-stenosis after stent-placement is still unclear. For example, the study conducted by Moldoveanu and colleagues showed that there was no significant difference of baseline level of Lp-PLA2 in patients with and without re-stenosis after PCI [31]. Nevertheless, the result in our current study indicated that increased baseline level of Lp-PLA2 portended an increased risk of re-stenosis after 1 year’s follow-up. To our best knowledge, there might be some mechanisms contributing to this discrepancy. In the first place, the protocols of these two studies are quite different. In the study conducted by Moldoveanu et al., they divided patients into two groups according to the end-point in terms of with or without in-stent re-stenosis. While in our study, patients were assigned into normal and elevated Lp-PLA2 groups according to their baseline levels. Secondary, the duration of follow-up in the former study was only 6 months, while the patients in our study were followed-up for 1 year. Thirdly, the smaller sample size of Moldoveanu’s study might also be a potential reason for the negative finding. In light of the mechanisms associated with re-stenosis as mentioned above, we believed that the complex roles Lp-PLA2 plays on vessel walls might in part explain our findings. Pathophysiologically, after engulfed by macrophages, oxidative-LDL would be degraded into two major substrates, named lyso-phosphotidylcholine (Lyso-PC) and oxidized non-esterified fatty acids (oxNEFAs), by Lp-PLA2. Accordingly, Lyso-PC and oxNEFAs have potent effects in recruiting inflammatory cells, promoting platelets activation and aggregation, impairing endothelial functions as well as enhancing smooth muscle cells proliferation and migration which subsequently lead to neointima formation and re-stenosis [32–34]. Taken together, it was reasonable to speculate that increased plasma level of Lp-PLA2 was associated with higher risk of re-stenosis. Nevertheless, the study conducted by Turunen and colleagues showed that local adenovirus-mediated Lp-PLA2 gene transfer resulted in a significant reduction in neointima formation in balloon-denuded rabbit aorta [35]. However, the pathophysiology of aorta denudation by balloon was somewhat, if not completely, different from that of vascular inflammation inducing by hyperlipidemia and endothelial dysfunction and activation. Furthermore, a large number of clinical studies have consistently demonstrated the positive relationship between increased plasma level of Lp-PLA2 and adverse clinical outcomes [8, 9, 11, 20]. Additionally, as stent placement may stimulate local inflammatory reaction and up-regulate inflammatory cytokines such as tumor necrosis factor-alpha expression, which in turn leads to platelet activating factor and Lp-PLA2 correspondingly increase. However, since only baseline Lp-PLA2 level has been measured, our study was impossible to make any conclusion that whether the change of platelet activating factor and Lp-PLA2 after stent-placement would also have significant effects on re-stenosis. Furthermore, since the percentages of drug-eluting stent and bare-metal stent placement in the normal and elevated groups were comparable, any bias related to stent-placement might also be excluded. In the future, conducting a prospective research to investigate whether reducing Lp-PLA2 level could decrease the risk of re-stenosis would definitely be a milestone with regard to the new era of CAD therapy.
On the other hand, at the very beginning, Lp-PLA2 was considered as a cardio-protective factor due to its effects on degrading platelet activating factor, a potent substrate in enhancing vascular inflammation and impairing cardiac function [36]. Nevertheless, since the positive relationship between Lp-PLA2 level and increased CVD risk has been firstly reported in WOSCOPS study in 2000 [37], many studies thereafter have consistently corroborated the detrimental effects of Lp-PLA2 on cardiovascular system [8, 38, 39]. Currently, the results from our study also indicated that patient with increased Lp-PLA2 level appeared to present more severe and urgent condition than that with normal Lp-PLA2 level, which might be partially explained by the adverse effects (expanding necrotic lipid core and thinning fibrous cap) Lp-PLA2 imposes on vessel walls [8, 40]. The higher percentage of patients with three vessels stenoses in elevated Lp-PLA2 group might also partially reflect the adverse effects Lp-PLA2 exerts on atherogenesis and progression.
Thirdly, due to the production of inflammatory cytokines such as interleukin-6 tumor necrosis factor-alpha and platelet activating factor from adipose tissues, obesity is considered as one of the major risk factor for cardiovascular events such as in-stent re-stenosis [41, 42]. Interestingly, previous one study showed that increased Lp-PLA2 might compensate for the adiposity-associated increases in inflammatory and oxidative burden [43]. Therefore, it might be reasonable to speculate that in patients with obesity, the incidence of re-stenosis in higher Lp-PLA2 level group might be lower than the lower Lp-PLA2 group. However, in our current study, no significant difference of incidence of re-stenosis was found in obese patients with normal and increased Lp-PLA2 level (33.3% vs 36.4%, P = 0.208).
Finally, since a vast majority of participants in current study were with increased level of Hs-CRP (>3 mg/L), we therefore further evaluated the relationship between Hs-CRP level and re-stenosis. With univariate analysis, Hs-CRP appeared to be a potential predictor for re-stenosis. Nevertheless, after adjustment for other risk factors, Hs-CRP did not remain independently associated with re-stenosis, which was consistent with previous studies [44, 45], in which increased Hs-CRP level before PCI were not associated with in-stent re-stenosis. We believed that this negative finding might be partially due to the unspecific characteristic of Hs-CRP, with respect to Hs-CRP elevation could be confounded by other diseases such as latent and modest infection [46, 47]. Contrary to Hs-CRP, Lp-PLA2 still remained an independent predictor for re-stenosis after adjustment for other risk factors (hazard ratio: 1.140, 95% confidence interval: 1.068-1.195), which we believed was predominantly due to its high specificity for vascular inflammation in the setting of atherosclerotic cardiovascular diseases [6, 14]. In order to explore any synergistic effect between Lp-PLA2 and other risk factors for re-stenosis, Cox proportional hazard regression were performed and no significant synergism was found which we considered might be partially ascribed to the relatively small sample size of current study and future study is warranted to further investigate whether any synergistic effect exists between traditional risk factor and Lp-PLA2 for re-stenosis after stent-placement.
Conclusion
The results of our study indicate that increased plasma level of Lp-PLA2 at baseline is associated with increased risk of re-stenosis after 1 year’s stent-placement, and measurement of Lp-PLA2 may be helpful and useful for identifying subjects who are at an increased risk for re-stenosis. Future study is warranted to investigate whether decreasing plasma level of Lp-PLA2 with specific antagonist will reduce the incidence of re-stenosis.
Authors’ information
Dongdan Zheng, FanFang Zeng, Anping Cai: co-first authors.
References
Lloyd-Jones DM: Cardiovascular risk prediction: basic concepts, current status, and future directions. Circulation. 2010, 121: 1768-1777. 10.1161/CIRCULATIONAHA.109.849166
Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ: Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011, 123: 933-944. 10.1161/CIR.0b013e31820a55f5
Ross R: Atherosclerosis–an inflammatory disease. N Engl J Med. 1999, 340: 115-126. 10.1056/NEJM199901143400207
Madjid M, Willerson JT: Inflammatory markers in coronary heart disease. Br Med Bull. 2011, 100: 23-38. 10.1093/bmb/ldr043
Ikonomidis I, Michalakeas CA, Lekakis J, Parissis J, Anastasiou-Nana M: The role of lipoprotein-associated phospholipase A2 (Lp-PLA(2)) in cardiovascular disease. Rev Recent Clin Trials. 2011, 6: 108-113. 10.2174/157488711795177903
Cai A, Zheng D, Qiu R, Mai W, Zhou Y: Lipoprotein-associated phospholipase A2 (Lp-PLA(2)): a novel and promising biomarker for cardiovascular risks assessment. Dis Markers. 2013, 34: 323-331. 10.1155/2013/432136
Theilmeier G, De Geest B, Van Veldhoven PP, Stengel D, Michiels C, Lox M, Landeloos M, Chapman MJ, Ninio E, Collen D, Himpens B, Holvoet P: HDL-associated PAF-AH reduces endothelial adhesiveness in apoE-/-mice. FASEB J. 2000, 14: 2032-2039. 10.1096/fj.99-1029com
Wilensky RL, Shi Y, Mohler ER, Hamamdzic D, Burgert ME, Li J, Postle A, Fenning RS, Bollinger JG, Hoffman BE, Pelchovitz DJ, Yang J, Mirabile RC, Webb CL, Zhang L, Zhang P, Gelb MH, Walker MC, Zalewski A, Macphee CH: Inhibition of lipoprotein-associated phospholipase A2 reduces complex coronary atherosclerotic plaque development. Nat Med. 2008, 14: 1059-1066. 10.1038/nm.1870
May HT, Horne BD, Anderson JL, Wolfert RL, Muhlestein JB, Renlund DG, Clarke JL, Kolek MJ, Bair TL, Pearson RR, Sudhir K, Carlquist JF: Lipoprotein-associated phospholipase A2 independently predicts the angiographic diagnosis of coronary artery disease and coronary death. Am Heart J. 2006, 152: 997-1003. 10.1016/j.ahj.2006.01.011
Jenny NS, Solomon C, Cushman M, Tracy RP, Nelson JJ, Psaty BM, Furberg CD: Lipoprotein-associated phospholipase A(2) (Lp-PLA(2)) and risk of cardiovascular disease in older adults: results from the Cardiovascular Health Study. Atherosclerosis. 2010, 209: 528-532. 10.1016/j.atherosclerosis.2009.09.021
Thompson A, Gao P, Orfei L, Watson S, Di AE, Kaptoge S, Ballantyne C, Cannon CP, Criqui M, Cushman M, Hofman A, Packard C, Thompson SG, Collins R, Danesh J: Lipoprotein-associated phospholipase A(2) and risk of coronary disease, stroke, and mortality: collaborative analysis of 32 prospective studies. Lancet. 2010, 375: 1536-1544.
Dohi T, Miyauchi K, Okazaki S, Yokoyama T, Ohkawa R, Nakamura K, Yanagisawa N, Tsuboi S, Ogita M, Yokoyama K, Kurata T, Yatomi Y, Daida H: Decreased circulating lipoprotein-associated phospholipase A2 levels are associated with coronary plaque regression in patients with acute coronary syndrome. Atherosclerosis. 2011, 219: 907-912. 10.1016/j.atherosclerosis.2011.09.019
Anderson JL: Lipoprotein-associated phospholipase A2: an independent predictor of coronary artery disease events in primary and secondary prevention. Am J Cardiol. 2008, 101: 23F-33F. 10.1016/j.amjcard.2008.04.015
Corson MA, Jones PH, Davidson MH: Review of the evidence for the clinical utility of lipoprotein-associated phospholipase A2 as a cardiovascular risk marker. Am J Cardiol. 2008, 101: 41F-50F. 10.1016/j.amjcard.2008.04.018
Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, Joyal SV, Hill KA, Pfeffer MA, Skene AM: Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004, 350: 1495-1504. 10.1056/NEJMoa040583
Pedersen TR, Faergeman O, Kastelein JJ, Olsson AG, Tikkanen MJ, Holme I, Larsen ML, Bendiksen FS, Lindahl C, Szarek M, Tsai J: High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA. 2005, 294: 2437-2445. 10.1001/jama.294.19.2437
Kamstrup PR, Benn M, Tybjaerg-Hansen A, Nordestgaard BG: Extreme lipoprotein(a) levels and risk of myocardial infarction in the general population: the Copenhagen City Heart Study. Circulation. 2008, 117: 176-184. 10.1161/CIRCULATIONAHA.107.715698
Davidson MH, Corson MA, Alberts MJ, Anderson JL, Gorelick PB, Jones PH, Lerman A, McConnell JP, Weintraub HS: Consensus panel recommendation for incorporating lipoprotein-associated phospholipase A2 testing into cardiovascular disease risk assessment guidelines. Am J Cardiol. 2008, 101: 51F-57F. 10.1016/j.amjcard.2008.04.019
Brilakis ES, McConnell JP, Lennon RJ, Elesber AA, Meyer JG, Berger PB: Association of lipoprotein-associated phospholipase A2 levels with coronary artery disease risk factors, angiographic coronary artery disease, and major adverse events at follow-up. Eur Heart J. 2005, 26: 137-144.
Kiechl S, Willeit J, Mayr M, Viehweider B, Oberhollenzer M, Kronenberg F, Wiedermann CJ, Oberthaler S, Xu Q, Witztum JL, Tsimikas S: Oxidized phospholipids, lipoprotein(a), lipoprotein-associated phospholipase A2 activity, and 10-year cardiovascular outcomes: prospective results from the Bruneck study. Arterioscler Thromb Vasc Biol. 2007, 27: 1788-1795. 10.1161/ATVBAHA.107.145805
Tanaka A, Imanishi T, Kitabata H, Kubo T, Takarada S, Tanimoto T, Kuroi A, Tsujioka H, Ikejima H, Komukai K, Kataiwa H, Okouchi K, Kashiwaghi M, Ishibashi K, Matsumoto H, Takemoto K, Nakamura N, Hirata K, Mizukoshi M, Akasaka T: Lipid-rich plaque and myocardial perfusion after successful stenting in patients with non-ST-segment elevation acute coronary syndrome: an optical coherence tomography study. Eur Heart J. 2009, 30: 1348-1355. 10.1093/eurheartj/ehp122
Mega JL, Simon T, Collet JP, Anderson JL, Antman EM, Bliden K, Cannon CP, Danchin N, Giusti B, Gurbel P, Horne BD, Hulot JS, Kastrati A, Montalescot G, Neumann FJ, Shen L, Sibbing D, Steg PG, Trenk D, Wiviott SD, Sabatine MS: Reduced-function CYP2C19 genotype and risk of adverse clinical outcomes among patients treated with clopidogrel predominantly for PCI: a meta-analysis. JAMA. 2010, 304: 1821-1830. 10.1001/jama.2010.1543
Sorajja P, Gersh BJ, Cox DA, McLaughlin MG, Zimetbaum P, Costantini C, Stuckey T, Tcheng JE, Mehran R, Lansky AJ, Grines CL, Stone GW: Impact of delay to angioplasty in patients with acute coronary syndromes undergoing invasive management: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage strategY) trial. J Am Coll Cardiol. 2010, 55: 1416-1424. 10.1016/j.jacc.2009.11.063
LaRosa JC, Grundy SM, Waters DD, Shear C, Barter P, Fruchart JC, Gotto AM, Greten H, Kastelein JJ, Shepherd J, Wenger NK: Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005, 352: 1425-1435. 10.1056/NEJMoa050461
Breen DM, Dolinsky VW, Zhang H, Ghanim H, Guo J, Mroziewicz M, Tsiani EL, Bendeck MP, Dandona P, Dyck JR, Heximer SP, Giacca A: Resveratrol inhibits neointimal formation after arterial injury through an endothelial nitric oxide synthase-dependent mechanism. Atherosclerosis. 2012, 222: 375-381. 10.1016/j.atherosclerosis.2012.03.021
Park SJ, Kang SJ, Virmani R, Nakano M, Ueda Y: In-stent neoatherosclerosis: a final common pathway of late stent failure. J Am Coll Cardiol. 2012, 59: 2051-2057. 10.1016/j.jacc.2011.10.909
Packard CJ: Lipoprotein-associated phospholipase A2 as a biomarker of coronary heart disease and a therapeutic target. Curr Opin Cardiol. 2009, 24: 358-363. 10.1097/HCO.0b013e32832bcb22
Rosenson RS: Phospholipase A2 inhibition and atherosclerotic vascular disease: prospects for targeting secretory and lipoprotein-associated phospholipase A2 enzymes. Curr Opin Lipidol. 2010, 21: 473-480. 10.1097/MOL.0b013e32833eb581
Colley KJ, Wolfert RL, Cobble ME: Lipoprotein associated phospholipase A(2): role in atherosclerosis and utility as a biomarker for cardiovascular risk. EPMA J. 2011, 2: 27-38. 10.1007/s13167-011-0063-4
Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002, 106: 3143-3421.
Moldoveanu E, Mut-Vitcu B, Tanaseanu GR, Marta DS, Manea G, Kosaka T, Vidulescu C, Tanaseanu C: Low basal levels of circulating adiponectin in patients undergoing coronary stenting predict in-stent restenosis, independently of basal levels of inflammatory markers: lipoprotein associated phospholipase A2, and myeloperoxidase. Clin Biochem. 2008, 41: 1429-1433. 10.1016/j.clinbiochem.2008.09.109
Boffa MB, Marcovina SM, Koschinsky ML: Lipoprotein(a) as a risk factor for atherosclerosis and thrombosis: mechanistic insights from animal models. Clin Biochem. 2004, 37: 333-343. 10.1016/j.clinbiochem.2003.12.007
Tsimikas S, Tsironis LD, Tselepis AD: New insights into the role of lipoprotein(a)-associated lipoprotein-associated phospholipase A2 in atherosclerosis and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2007, 27: 2094-2099. 10.1161/01.ATV.0000280571.28102.d4
Garg PK, McClelland RL, Jenny NS, Criqui M, Liu K, Polak JF, Jorgensen NW, Cushman M: Association of lipoprotein-associated phospholipase A(2) and endothelial function in the Multi-Ethnic Study of Atherosclerosis (MESA). Vasc Med. 2011, 16: 247-252. 10.1177/1358863X11411360
Turunen P, Puhakka H, Rutanen J, Hiltunen MO, Heikura T, Gruchala M, Yla-Herttuala S: Intravascular adenovirus-mediated lipoprotein-associated phospholipase A2 gene transfer reduces neointima formation in balloon-denuded rabbit aorta. Atherosclerosis. 2005, 179: 27-33. 10.1016/j.atherosclerosis.2004.10.025
Detopoulou P, Nomikos T, Fragopoulou E, Chrysohoou C, Antonopoulou S: Platelet Activating Factor in Heart Failure: Potential Role in Disease Progression and Novel Target for Therapy. Curr Heart Fail Rep. 2013, 10: 122-129. 10.1007/s11897-013-0131-2
Packard CJ, O'Reilly DS, Caslake MJ, McMahon AD, Ford I, Cooney J, Macphee CH, Suckling KE, Krishna M, Wilkinson FE, Rumley A, Lowe GD: Lipoprotein-associated phospholipase A2 as an independent predictor of coronary heart disease. West of Scotland Coronary Prevention Study Group. N Engl J Med. 2000, 343: 1148-1155. 10.1056/NEJM200010193431603
Blankenberg S, Stengel D, Rupprecht HJ, Bickel C, Meyer J, Cambien F, Tiret L, Ninio E: Plasma PAF-acetylhydrolase in patients with coronary artery disease: results of a cross-sectional analysis. J Lipid Res. 2003, 44: 1381-1386. 10.1194/jlr.M300086-JLR200
Garza CA, Montori VM, McConnell JP, Somers VK, Kullo IJ, Lopez-Jimenez F: Association between lipoprotein-associated phospholipase A2 and cardiovascular disease: a systematic review. Mayo Clin Proc. 2007, 82: 159-165. 10.1016/S0025-6196(11)60992-0
Kougias P, Chai H, Lin PH, Lumsden AB, Yao Q, Chen C: Lysophosphatidylcholine and secretory phospholipase A2 in vascular disease: mediators of endothelial dysfunction and atherosclerosis. Med Sci Monit. 2006, 12: RA5-RA16.
Takeda R, Suzuki E, Satonaka H, Oba S, Nishimatsu H, Omata M, Fujita T, Nagai R, Hirata Y: Blockade of endogenous cytokines mitigates neointimal formation in obese Zucker rats. Circulation. 2005, 111: 1398-1406. 10.1161/01.CIR.0000158482.83179.DB
Miao CY, Li ZY: The role of perivascular adipose tissue in vascular smooth muscle cell growth. Br J Pharmacol. 2012, 165: 643-658. 10.1111/j.1476-5381.2011.01404.x
Detopoulou P, Nomikos T, Fragopoulou E, Panagiotakos DB, Pitsavos C, Stefanadis C, Antonopoulou S: Lipoprotein-associated phospholipase A2 (Lp-PLA2) activity, platelet-activating factor acetylhydrolase (PAF-AH) in leukocytes and body composition in healthy adults. Lipids Health Dis. 2009, 8: 19- 10.1186/1476-511X-8-19
Segev A, Kassam S, Buller CE, Lau HK, Sparkes JD, Connelly PW, Seidelin PH, Natarajan MK, Cohen EA, Strauss BH: Pre-procedural plasma levels of C-reactive protein and interleukin-6 do not predict late coronary angiographic restenosis after elective stenting. Eur Heart J. 2004, 25: 1029-1035. 10.1016/j.ehj.2004.04.027
Delhaye C, Sudre A, Lemesle G, Marechaux S, Broucqsault D, Hennache B, Bauters C, Lablanche JM: Preprocedural high-sensitivity C-reactive protein predicts death or myocardial infarction but not target vessel revascularization or stent thrombosis after percutaneous coronary intervention. Cardiovasc Revasc Med. 2009, 10: 144-150.
Ballantyne CM, Nambi V: Markers of inflammation and their clinical significance. Atheroscler Suppl. 2005, 6: 21-29.
Elkind MS, Tai W, Coates K, Paik MC, Sacco RL: High-sensitivity C-reactive protein, lipoprotein-associated phospholipase A2, and outcome after ischemic stroke. Arch Intern Med. 2006, 166: 2073-2080. 10.1001/archinte.166.19.2073
Acknowledgement
We appreciate very much for the help of Dr. Shaoqi Rao in assisting the statistic analyses of our results.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DZ, FZ, HL and LL predominantly performed this study, RQ and RX helped to collect the demographic and clinical characteristics of all participants, HL and AC wrote this article, and CX and WM designed this study and WM helped to revise final version of current manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Zheng, D., Zeng, F., Cai, A. et al. Baseline elevated Lp-PLA2 is associated with increased risk for re-stenosis after stent placement. Lipids Health Dis 13, 41 (2014). https://doi.org/10.1186/1476-511X-13-41
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-511X-13-41