Abstract
Pancreatic cancer remains a challenging disease with an overall cumulative 5-year survival rate below 1%. The process of cancer initiation, progression and metastasis is still not understood well. Invasion and tumor metastasis are closely related and both occur within a tumour-host microecology, where stroma and tumour cells exchange enzymes and cytokines that modify the local extracellular matrix, stimulate cell migration, and promote cell proliferation and tumor cell survival. During the last decade considerable progress has been made in understanding genetic alterations of genes involved in local and systemic tumor growth. The most important changes occur in genes which regulate cell cycle progression, extracellular matrix homeostasis and cell migration. Furthermore, there is growing evidence that epigenetic factors including angiogenesis and lymphangiogenesis may participate in the formation of tumor metastasis. In this review we highlight the most important genetic alterations involved in tumor invasion and metastasis and further outline the role of tumor angiogenesis and lymphangiogenesis in systemic tumor dissemination.
Similar content being viewed by others
Review
Pancreatic cancer remains an unfortunate disease with a 5-year survival rate below 1%. Thus it represents one of the leading causes of cancer related death in industrialized countries despite advances in medical therapy and surgical techniques [1]. One of the major hallmarks of pancreatic cancer is its early systemic dissemination and its extraordinary local tumor progression [2]. These features may contribute to more than 3/4 of patients diagnosed with this disease can not be offered curative treatment and, therefore, may determine the high mortality rate among patients with pancreatic cancer [1].
One standing problem in the therapy of pancreatic cancer is metastatic disease. How metastatic progression develops is unknown in as much as little is known on how malignant cells detach from the primary tumor site and grow in distant organs [3]. Invasion and metastasis occur within a tumour-host microecology, where stroma and tumour cells exchange signals that modify the local extracellular matrix, stimulate migration, and promote proliferation and survival [4]. In general the genetic variability of cancer cells leads to the manifestation of six essential alterations that collectively dictate malignant, and most likely also metastatic and invasive tumor growth: self-sufficiency in growth signals, insensitivity to growth-inhibitory (antigrowth) signals, evasion of programmed cell death (apoptosis), limitless replicative potential, sustained angiogenesis, and tissue invasion and metastasis [4].
In the present review we will focus on the impact of molecular alterations including metalloproteinases, the plasminogen activator/plasmin system and tumor metastasis suppressor genes and we will highlight the role of angiogenesis and lymphangiogenesis in pancreatic cancer progression.
Genetic instability and tumor progression
The understanding of the molecular mechanisms of tumor growth and metastasis is one of the most important issues in cancer research. It is necessary to identify genetic but also epigenetic determinants which govern systemic tumor dissemination. Since cancer is attributed to genetic alterations it is indispensable to identify those genes whose alterations accumulate during tumor progression. Over the past two decades, a number of these genes have been identified. In 1980, identification of oncogenes opened the way to specifically search for genetic alterations in human cancers [5]. In the late 1980s and 1990s, isolation of tumor suppressor genes further accelerated the understanding of the genetic network. In the early period restriction fragment length polymorphism analysis (RFLP) of tumor suppressor genes [6] identified that loss of heterozygosity (LOH) – a hallmark of gene inactivation – occurs frequently at multiple chromosomal loci in a variety of human cancers including pancreatic cancer [7]
The presence of multiple genetic alterations in human cancers strongly indicated that alterations accumulate during tumor progression. Comparative analysis of these genetic alterations in early and late stage tumors led to the hypothesis of a multistage carcinogenesis in colorectal cancer progression which now is a widely accepted genetic tumor progression model [8]. A similar progression model has recently been postulated for pancreatic cancer, where an adenoma-carcinoma sequence is proposed [9]. Based on the concept of multistage carcinogenesis, the metastatic activity of cancer cells should be defined by those genes whose alterations accumulate predominantly in late stage cancer cells.
What makes pancreatic cancer invasive and metastatic
Sooner or later during the development of pancreatic cancer the primary tumor mass spawns pioneer cells that move out, invade adjacent tissues, and circulate to distant organs where they may form new colonies. These processes are responsible for ~90% of pancreatic cancer deaths in patients [2]. Once metastatic cells settled in distant organs nutrients and space are no longer limited because newly formed metastases arise as islets of cancer cells surrounded by normal cells of the host tissue. Invasion and metastasis are complex processes, and their genetic and biochemical determinants are still largely unknown. Mechanistically they are closely related since both utilize similar strategies, involving changes in the physical coupling of cells to their microenvironment and activation of extracellular proteases. It is known that the movement of neoplastic cells is not a random process, even so the mechanisms governing their movement, survival in foreign tissue environments, and choice of residence at a final destination have remained uncertain [4].
Several controversial theories exist to explain the metastatic specificity. Among them, the homing theory suggests that organs distant to sites of primary malignancy actively attract malignant cells via expression of adhesion receptors or by secretion of soluble chemotactic factors [10]. Identification of molecular addresses or adhesion receptors on endothelial cells in vascular beds of distal organs that specifically trap circulating malignant cells supports the active arrest view of the homing theory [11]. In contrast, the fertile soil theory proposes that different organ environments provide variable growth conditions for specific circulating cell types. It seems likely that distinct mechanisms/molecules might govern a malignant cell's journey to an ectopic tissue, separate from those regulating its growth and/or survival once its destination has been achieved [4]. Tumor invasion encompasses the process of tumor cell penetration or infiltration into adjacent tissue. This event is also central and related to the development of metastasis. Loss of junctional contact between adjacent epithelial cells and cell-extracellular matrix association are essential prerequisites for tumor cell detachment from the primary tumor site [12]. It is postulated that migration and invasion of cancer cells into surrounding stroma are prevented by cell-cell and cell-matrix adhesion molecules. Disruption of these adhesive connections leads to increased motility of tumor cells, which detach from the primary lesion. Therefore, adhesion molecules on the cell surface play an important role in tumor cell migration and regulate the potential for epithelial cells to metastasize.
Cell adhesion molecules and their role in metastasis
Several classes of proteins are participating when cells exhibit an invasive or metastatic phenotype. This includes cell-cell adhesion molecules (CAMs) like members of the immunoglobulin and calcium-dependent cadherin families and integrins [13]. Notably, all of these "adherence" interactions convey regulatory signals to the cell [14]. One widely observed alteration in cell-to-environment interaction in pancreatic cancer involves E-cadherin, which couples adjacent cells by E-cadherin bridges. As a result the transmission of antigrowth signals is mediated via cytoplasmic contacts with catenin to intracellular signaling circuits that include the Lef/Tcf transcription factor [15]. E-cadherin function is lost in a majority of pancreatic tumors [16]. Currently, the presence of E-cadherin is considered as an important suppressor of invasion and metastasis and its functional elimination may represent a key step in the acquisition of this phenotype.
Alterations of cell adhesion molecule expression in the immunoglobulin superfamily also appear to play critical role in invasion and metastasis [17, 18]. Clearly N-CAM undergoes a switch in expression from a highly adhesive isoform to poorly adhesive forms and its down regulation leads to invasive pancreatic cancer [19]. Furthermore, differential expression of the cell adhesion molecules ICAM-1 (intercellular adhesion molecule-1), VCAM-1 (vascular cell adhesion molecule-1), and ELAM-1 (endothelial leukocyte adhesion molecule-1) in human pancreatic cancer has recently been studied [20]. Northern blot analysis revealed a 5.4-fold increase of ICAM-1 and a 3.7-fold increase in VCAM-1 mRNA expression in cancer samples in comparison with normal controls. In contrast, ELAM-1 mRNA levels did not show significant differences between cancer and normal tissues. Therefore, it is likely that enhanced ICAM-1 and VCAM-1 expression plays a role in human pancreatic cancer pathogenesis, where they likely contribute to cancer cell migration and the spread of cancer cells to distant organs, or both [20].
Changes in integrin expression are also evident in invasive and metastatic pancreatic cancer cells. The importance of integrins in tumor cell dissemination is their role in cellular adaptation to changing tissue microenvironments as found in metastatic organs. This is achieved through various permutations in the spectrum of the more than 22 integrin subtypes. Experimental changes in expression of integrin subunits in cultured cells induces or inhibits invasive and metastatic growth, which confers their role as central determinants of these processes [21].
The second class of players in transforming pancreatic cancer into an invasive and metastatic phenotype are extracellular proteases [22]. Several studies in pancreatic cancer indicate that proteases are upregulated, protease inhibitors are downregulated, and inactive zymogen forms of proteases are converted into active enzymes [23]. One imagines that docking of active proteases on the cell surface can facilitate invasion by cancer cells into nearby stroma, across blood vessel walls, and through normal epithelial cell layers. However, this theory is getting even more complex due to multiple cell types involved in protease expression and display. In many types of carcinomas, matrix-degrading proteases are produced by conscripted stromal and inflammatory cells but not by the epithelial cancer cells [24]. For example, in the case of pancreatic cancer there is evidence that certain cancer cells induce urokinase (uPA) expression in stromal cells, which then bind to the urokinase receptor (uPAR) expressed on the cancer cells [25].
The role of matrix metalloproteases in pancreatic cancer dissemination
Recent studies of the activity of matrix metalloproteases (MMPs) and their tissue inhibitors (TIMPS) in invasive neoplasms have indicated that these enzymes play an important role in the degradation of connective tissue which is associated with the development of tumor metastases [26]. The matrix metalloproteases comprise a family of secreted or transmembrane proteins. Currently at least 15 structurally related members with a broad spectrum of proteolytic activities against components of the extracellular matrix have been identified. Based on their substrate specificities, MMPs have been categorized into five groups: collagenases, gelatinases, stromelysins, metalloelastases and the newly identified membrane-type MMP. In particular, MMP-2 and MMP-9 (gelatinase A and gelatinase B) are involved in the systemic dissemination of tumors. The importance of MMPs during tumor metastasis may be related to their proteolytic activity against type IV collagen, which is a major component of epithelial basement membranes [26]. The proteolytic acitivity of MMPs is regulated at different levels, including regulation of mRNA transcription by biologically active agents such as growth factors, hormones and oncogens, as well as regulation at the level of mRNA stability and translation. Most of the MMPs are produced in the form of biologically inactive proenzymes and need to become activated. For example, activation of MMP-2 involves the action of a membrane-type 1 matrix metalloproteinase (MT-1-MMP) which cleaves a portion of the carboxy terminus of pro-MMP-2 [27]. Once MMP-2 is active, it is susceptible for inhibition by a family of so called specific tissue inhibitors of metalloproteinases (TIMPS). Nowadays, there is strong experimental evidence that MMPs play a major role in local and systemic growth of pancreatic cancer [28]. Furthermore, high expression of MT1-MMP and MT2-MMP, MMP-2, and MMP-9, as well as TIMP-1 and TIMP-2 was found in pancreatic cancer [29]. Recent studies suggested that members of the MMPs also enhance tumor angiogenesis by triggering the angiogenic switch [24].
The plasminogen activator /plasmin system
In addition to the MMP family, the plasminogen activator/plasmin system has been implicated in tumor invasion and metastasis. Plasmin participates in tissue degradation and is activated from the inactive precursor plasminogen by two types of plasminogen activators – uPA (urokinase plasminogen activator) and tPA (tissue plasminogen activator) [30]. The proteolytic activity of uPA plays a dominant role in cell migration, angiogenesis, and tumor metastases and is tightly regulated by proteolytic cleavage. It is released from various cell types as an inactive proenzyme (pro-uPA) which upon cleavage by proteinases becomes enzymatically active [31]. uPA binds to a specific cell surface receptor the Urokinase Plasminogen Activator Receptor (uPAR). Upon binding, uPA converts the zymogen plasminogen to plasmin, an enzyme which degrades fibrin and numerous other components of the extracellular matrix, such as type IV collagen, fibronectin and laminin [32]. This likely enables tumor cells to migrate through tissue barriers [32, 33]. Several studies provided evidence that the expression of active uPA by malignant cells correlates with their invasive potential [34]. Elevated levels of uPA/uPAR have been reported in numerous tumors, including pancreatic cancer [25]. In patients with pancreatic cancer concomitant overexpression of uPA and uPAR was found to be associated with a shorter post-operative survival compared with those patients in whom only uPA or its receptor were overexpressed [25]. In a recent study, the u-PA/u-PA receptor proteolytic system has been reported to be involved in the hepatocyte growth factor (HGF)-stimulated motility of pancreas cancer cells [35]. HGF-induced cell motility is significantly reduced by inhibitors of u-PA proteolytic activity, such as antibodies neutralizing u-PA activity, plasminogen activator inhibitor 1 and amiloride [35]. Additionally, anti-uPA antibodies injected into mice together with tumor cells caused a significant inhibition of metastasis formation, providing strong evidence for the involvement of this enzymatic system in tumor invasion and metastases.
The KAI1 gene – A potential suppressor gene of metastasis lost in pancreatic cancer
Despite the number of genes which putatively regulate tumor metastasis remains low, differential analysis identified some genes which may be involved in tumor metastasis. Among the genes are p9Ka/mtal, KAI1, KiSS-1, Tiam-1 and nm23-H1 [36, 37]. Among the most interesting genes involved in metastatic disease progression in pancreatic cancer is the putative metastasis suppressor gene, called KAI1, which was originally identified as metastasis suppressor gene for prostate cancer [38]. The KAI1 protein is a member of the transmembrane-4 superfamily (TM4SF) [39]. Additional studies revealed that decreased KAI1 expression could be a useful marker for metastatic/invasive potential in a series of human tumor types, including cancers of the bladder, colon, breast and skin [40–43]. In the case of pancreatic cancer KAI1 appears to be crucial for the development of distant organ metastasis since loss of KAI1 expression was found in lymph node and distant metastasis [43, 44]. For example, Northern blot analysis showed increased steady-state levels of KAI1 mRNA in 89% of pancreatic cancer samples. These findings were confirmed by in situ hybridization, by which enhanced KAI1 mRNA levels could be localized in pancreatic cancer cells. In contrast, the stroma surrounding the cancer mass and normal pancreatic tissue adjacent to the cancer cells exhibited very low levels of KAI1 mRNA. Correlation of mRNA levels obtained by Northern blot analysis with clinical parameters of the patients revealed that KAI1 mRNA levels were significantly higher in earlier tumor stages than in advanced tumor stages, in which lymph node or distant metastases were present. These studies indicated that KAI1 mRNA expression is reduced in patients with advanced tumor stages and additionally revealed that pancreatic cancer cells of distant metastases were devoid of KAI1 mRNA in comparison with those of primary pancreatic cancers [44]. In addition, KAI1 mRNA expression was shown to be associated with poor prognosis in patients with pancreatic cancers but also in patients with lung and breast cancers [44]. Those studies suggest that down-regulation of KAI1 expression may be an important step in metastatic progression of many types of human cancers.
The role of Angiogenesis in local and systemic tumor growth
Oxygen and nutrients supplied by the vasculature are crucial for cell function and survival. Thus, the formation of new blood vessels (angiogenesis) is permissive for local and systemic expansion of the tumor mass and can be induced by multiple molecules that are released by both cancer cells and stromal cells [45]. Angiogenesis itself encompasses a cascade of sequential processes emanating from microvascular endothelial cells, which are stimulated to proliferate and degrade the endothelial basement membrane of parental vessels, migrate, and penetrate into host stroma and initiate a capillary sprout [46]. The recruitment of endothelial cells during angiogenesis and the formation of vascular tumors depends on the breakdown of basement membranes, which occurs under control of numerous activating factors that were shown to be overexpressed in pancreatic cancer, including vascular endothelial growth factor (VEGF), bFGF, angiogenin, members of the TGF and FGF gene families, and interleukin-8 (IL-8) [47]. For instance, some of the pro-angiogenic cytokines are overexpressed in pancreatic cancer tissues, and even correlate with cancer aggressiveness and the patient's prognosis [48]. In addition to neovascularization and disruption of cell-cell and cell-matrix adhesion, active proteolytic degradation of the extracellular matrix is required when detached malignant cells start migrating through the stroma surrounding the tumor [3]. A similar process may be necessary when cells exit blood vessels to colonize distant metastatic sites [3].
In order to progress to a larger size, incipient neoplasias must develop an angiogenic ability [49]. The angiogenesis-initiating signals are exemplified by vascular endothelial growth factor (VEGF) and acidic and basic fibroblast growth factors (FGF1, FGF2). Each binds to transmembrane tyrosine kinase receptors displayed by endothelial cells and in the case of pancreatic cancer even on cancer cells themselves thus creating autocrine growth stimulation [50].
Integrin signaling also contributes to tumor neoangiogenesis. Quiescent vessels express one class of integrins, whereas sprouting capillaries express another. Interference with signaling from the latter class of integrins can inhibit angiogenesis underscoring the important contribution of cell adhesion to the angiogenic program which has also been shown for pancreatic cancer [21]. Furthermore, extracellular proteases are physically and functionally connected with proangiogenic integrins, and both help to dictate the invasive capability of angiogenic endothelial cells [51].
Experimental evidence for the importance of inducing and sustaining angiogenesis in tumors has been studied extensively during the last couple of years [52]. Molecular proof of principle came, for example, when VEGF as well the VEGF receptors were therapeutically targeted and proved able to impair neovascularization and growth of tumors in mice [53, 54].
Lymph-angiogenesis and lymphangio-invasion and its role in metastasis of pancreatic cancer
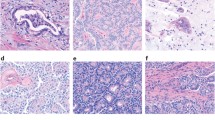
Tumor cells spread via the lymphatic system to regional lymph nodes and finally into larger lymphatic vessels which re-enter into the blood vascular system. In view of its function, it is not surprising that deficiencies in the lymphatic system are implicated in tumor growth [55]. Like in normal tissues, both vascular and lymphatic vessels are present in malignant tissues, but some remarkable differences from normal vessels have been observed. Unraveling alterations in lymphangiogenesis in tumors is of major importance for understanding tumor spread. Both vascular systems in a growing tumor share many common features. Tumor blood vessels are highly disorganized, tortous and dilated. They may display uneven diameter, excessive branching, shunts, and incomplete or absent muscular coverage [56]. Consequently, tumor vessels are leaky and blood flow is sluggish [57]. Lymphatic vessels in pancreatic cancer have not been studied well, most likely due to a lack of appropriate molecular markers, however, lymphangiogenesis appears important in metastasis of pancreatic cancer [58]. Morphological studies clearly indicated alterations of lymphatic vessels in the periphery of the tumors, where enlarged and well perfused lymphatic vessels can be detected, whereas compressed and non-functional vessels in the inside of the tumor can be seen [59]. One explanation may be that neoplastic cells grown in a confined space generate mechanical stress, compressing the newly formed lymphatic channels inside the tumor, while at the periphery, excess VEGF-C causes lymphatics to enlarge. It is noteworthy that overexpression of the lymphangiogenic factor VEGF-C and expression of its receptor flt-4 has been reported recently for pancreatic cancer where more than 2 fold higher levels for VEGF-C can be detected in cancer tissue than in normal pancreatic tissue [60]. The presence of VEGF-C in these cells was associated with increased lymphatic vessels invasion and lymph node metastasis, but not with decreased patient survival. These findings suggest that VEGF-C and its receptor are commonly overexpressed in human pancreatic cancers and may contribute to the lymphangiogenic process and metastasis in this disease.
Conclusion
The most devastating aspect of cancer is the emergence of metastases in organs distant from the primary tumor and most deaths from cancer are related to metastases. Thus, the understanding of the molecular mechanisms by which metastases are generated is one of the most important issues in cancer research. Recent advances in molecular biology have made it possible to identify genetic and epigenetic determinants for tumor progression and metastases. In fact, various genes including cell-cell adhesion molecules (CAMs), members of the cadherin families and integrins have been identified as modulators of metastatic growth. Furthermore, metalloproteinases, the uPA/uPAR system as well as the metastasis suppressor gene KAI1 appear to be crucial for the development of distant organ metastasis. Last but not least the emerging role of angiogenesis and lymphangiogenesis in invasion and metastasis appeared to be critically important for tumor cell dissemination. Based on this novel insights in mechanism of tumor invasion and metastasis, novel therapies are currently in the final clinical stages to become available for therapy of patients with pancreatic cancer.
Authors contribution
SK; PB; RL; MWB; and HF contributed to the writing and critical review of the manuscript. All authors read and approved the final manuscript.
References
Neoptolemos JP, Dunn JA, Stocken DD, Almond J, Link K, Beger HG: Adjuvant chemoradiotherapy and chemotherapy in resectable pancreatic cancer: a randomised controlled trial. Lancet. 2001, 358: 1576-1585. 10.1016/S0140-6736(01)06651-X.
DiMagno EP, Reber HA, Tempero MA: AGA technical review on the epidemiology, diagnosis, and treatment of pancreatic ductal adenocarcinoma. Gastroenterolgy. 1999, 117: 1464-1484.
Kim J, Yu W, Kovalski K, Ossowski L: Requirement for specific proteases in cancer cell intravasation as revealed by a novel semiquantitative PCR-based assay. Cell. 1998, 94: 353-362.
Hanahan D, Weinberg RA: The hallmarks of cancer. Cell. 2000, 100: 57-70.
Bishop JM: Molecular themes in oncogenesis. Cell. 1991, 64: 235-248.
Cavenee WK, Dryja TP, Phillips RA, Benedict WF, Godbout R, Gallie BL: Expression of recessive alleles by chromosomal mechanisms in retinoblastoma. Nature. 1983, 305: 779-784.
Ponder B: Cancer. Gene losses in human tumours. Nature. 1988, 335: 400-402. 10.1038/335400a0.
Kinzler KW, Vogelstein B: Life (and death) in a malignant tumour. Nature. 1996, 379: 19-20. 10.1038/379019a0.
Brat DJ, Lillemoe KD, Yeo CJ, Warfield PB, Hruban RH: Progression of pancreatic intraductal neoplasias to infiltrating adenocarcinoma of the pancreas. Am J Surg Pathol. 1998, 22: 163-169. 10.1097/00000478-199802000-00003.
Muller A, Homey B, Soto H, Ge N, Catron D, Buchanan ME: Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001, 410: 50-56. 10.1038/35065016.
Borsig L, Wong R, Hynes RO, Varki NM, Varki A: Synergistic effects of L- and P-selectin in facilitating tumor metastasis can involve non-mucin ligands and implicate leukocytes as enhancers of metastasis. Proc Natl Acad Sci U S A. 2002, 99: 2193-2198. 10.1073/pnas.261704098.
Tawil NJ, Gowri V, Djoneidi M, Nip J, Carbonetto S, Brodt P: Integrin alpha3beta1 can promote adhesion and spreading of metastatic breast carcinoma cells on the lymph node stroma. Int J Cancer. 1996, 66: 703-710. 10.1002/(SICI)1097-0215(19960529)66:5<703::AID-IJC20>3.0.CO;2-3.
Hanahan D, Bergers G, Bergsland E: Less is more, regularly: metronomic dosing of cytotoxic drugs can target tumor angiogenesis in mice. J Clin Invest. 2000, 105: 1045-1047.
Aplin AE, Howe A, Alahari SK, Juliano RL: Signal transduction and signal modulation by cell adhesion receptors: the role of integrins, cadherins, immunoglobulin-cell adhesion molecules, and selectins. Pharmacol Rev. 1998, 50: 197-263.
Christofori G, Semb H: The role of the cell-adhesion molecule E-cadherin as a tumour-suppressor gene. Trends Biochem Sci. 1999, 24: 73-76. 10.1016/S0968-0004(98)01343-7.
Karayiannakis AJ, Syrigos KN, Polychronidis A, Simopoulos C: Expression patterns of alpha-, beta- and gamma-catenin in pancreatic cancer: correlation with E-cadherin expression, pathological features and prognosis. Anticancer Res. 2001, 21: 4127-4134.
Skubitz AP: Adhesion molecules. Cancer Treat Res. 2002, 107: 305-329.
Maurer CA, Friess H, Kretschmann B, Wildi S, Muller CC, Graber H: Over-expression of ICAM-1, VCAM-1 and ELAM-1 might influence tumor progression in colorectal cancer. Int J Cancer. 1998, 79: 76-81. 10.1002/(SICI)1097-0215(19980220)79:1<76::AID-IJC15>3.0.CO;2-F.
Fogar P, Basso D, Pasquali C, De Paoli M, Sperti C, Roveroni G: Neural cell adhesion molecule (N-CAM) in gastrointestinal neoplasias. Anticancer Res. 1997, 17: 1227-1230.
Tempia-Caliera AA, Horvath LZ, Zimmermann A, Tihanyi TT, Korc M, Friess H: Adhesion molecules in human pancreatic cancer. J Surg Oncol. 2002, 79: 93-100. 10.1002/jso.10053.
Varner JA, Cheresh DA: Integrins and cancer. Curr Opin Cell Biol. 1996, 8: 724-730. 10.1016/S0955-0674(96)80115-3.
Coussens LM, Werb Z: Matrix metalloproteinases and the development of cancer. Chem Biol. 1996, 3: 895-904.
Bloomston M, Zervos EE, Rosemurgy AS: Matrix metalloproteinases and their role in pancreatic cancer: a review of preclinical studies and clinical trials. Ann Surg Oncol. 2002, 9: 668-674. 10.1245/aso.2002.9.7.668.
Bergers G, Brekken R, McMahon G, Vu TH, Itoh T, Tamaki K: Matrix metalloproteinase-9 triggers the angiogenic switch during carcinogenesis. Nat Cell Biol. 2000, 2: 737-744. 10.1038/35036374.
Cantero D, Friess H, Deflorin J, Zimmermann A, Brundler MA, Riesle E: Enhanced expression of urokinase plasminogen activator and its receptor in pancreatic carcinoma. Br J Cancer. 1997, 75: 388-395.
Kleiner DE, Stetler-Stevenson WG: Matrix metalloproteinases and metastasis. Cancer Chemother Pharmacol. 1999, 43 (Suppl): S42-S51. 10.1007/s002800051097.
Cornelius LA, Nehring LC, Harding E, Bolanowski M, Welgus HG, Kobayashi DK: Matrix metalloproteinases generate angiostatin: effects on neovascularization. J Immunol. 1998, 161: 6845-6852.
Matsuyama Y, Takao S, Aikou T: Comparison of matrix metalloproteinase expression between primary tumors with or without liver metastasis in pancreatic and colorectal carcinomas. J Surg Oncol. 2002, 80: 105-110. 10.1002/jso.10106.
Gress TM, Muller-Pillasch F, Lerch MM, Friess H, Buchler MW, Adler G: Expression and in-situ localization of genes coding for extracellular matrix proteins and extracellular matrix degrading proteases in pancreatic cancer. Int J Cancer. 1995, 62: 407-413.
Wang Y: The role and regulation of urokinase-type plasminogen activator receptor gene expression in cancer invasion and metastasis. Med Res Rev. 2001, 21: 146-170. 10.1002/1098-1128(200103)21:2<146::AID-MED1004>3.0.CO;2-B.
Schmitt M, Janicke F, Moniwa N, Chucholowski N, Pache L, Graeff H: Tumor-associated urokinase-type plasminogen activator: biological and clinical significance. Biol Chem Hoppe Seyler. 1992, 373: 611-622.
Dano K, Andreasen PA, Grondahl-Hansen J, Kristensen P, Nielsen LS, Skriver L: Plasminogen activators, tissue degradation, and cancer. Adv Cancer Res. 1985, 44: 139-266.
Friess H, Cantero D, Graber H, Tang WH, Guo X, Kashiwagi M: Enhanced urokinase plasminogen activation in chronic pancreatitis suggests a role in its pathogenesis. Gastroenterology. 1997, 113: 904-913.
Bramhall SR, Neoptolemos JP, Stamp GW, Lemoine NR: Imbalance of expression of matrix metalloproteinases (MMPs) and tissue inhibitors of the matrix metalloproteinases (TIMPs) in human pancreatic carcinoma. J Pathol. 1997, 182: 347-355. 10.1002/(SICI)1096-9896(199707)182:3<347::AID-PATH848>3.0.CO;2-J.
Paciucci R, Vila MR, Adell T, Diaz VM, Tora M, Nakamura T: Activation of the urokinase plasminogen activator/urokinase plasminogen activator receptor system and redistribution of E-cadherin are associated with hepatocyte growth factor-induced motility of pancreas tumor cells overexpressing Met. Am J Pathol. 1998, 153: 201-212.
Leone A, Flatow U, King CR, Sandeen MA, Margulies IM, Liotta LA: Reduced tumor incidence, metastatic potential, and cytokine responsiveness of nm23-transfected melanoma cells. Cell. 1991, 65: 25-35.
Friess H, Guo XZ, Tempia-Caliera AA, Fukuda A, Martignoni ME, Zimmermann A: Differential expression of metastasis-associated genes in papilla of vater and pancreatic cancer correlates with disease stage. J Clin Oncol. 2001, 19: 2422-2432.
Dong JT, Lamb PW, Rinker-Schaeffer CW, Vukanovic J, Ichikawa T, Isaacs JT: KAI1, a metastasis suppressor gene for prostate cancer on human chromosome 11p11.2. Science. 1995, 268: 884-886.
Dong JT, Isaacs WB, Barrett JC, Isaacs JT: Genomic organization of the human KAI1 metastasis-suppressor gene. Genomics. 1997, 41: 25-32. 10.1006/geno.1997.4618.
Jackson P, Kingsley EA, Russell PJ: Inverse correlation between KAI1 mRNA levels and invasive behaviour in bladder cancer cell lines. Cancer Lett. 2000, 156: 9-17. 10.1016/S0304-3835(00)00427-4.
Guo XZ, Friess H, Di Mola FF, Heinicke JM, Abou-Shady M, Graber HU: KAI1, a new metastasis suppressor gene, is reduced in metastatic hepatocellular carcinoma. Hepatology. 1998, 28: 1481-1488.
Guo XZ, Friess H, Maurer C, Berberat P, Tang WH, Zimmermann A: KAI1 is unchanged in metastatic and nonmetastatic esophageal and gastric cancers. Cancer Res. 1998, 58: 753-758.
Guo X, Friess H, Graber HU, Kashiwagi M, Zimmermann A, Korc M: KAI1 expression is up-regulated in early pancreatic cancer and decreased in the presence of metastases. Cancer Res. 1996, 56: 4876-4880.
Friess H, Guo XZ, Berberat P, Graber HU, Zimmermann A, Korc M: Reduced KAI1 expression in pancreatic cancer is associated with lymph node and distant metastases. Int J Cancer. 1998, 79: 349-355. 10.1002/(SICI)1097-0215(19980821)79:4<349::AID-IJC7>3.0.CO;2-V.
Bergers G, Javaherian K, Lo KM, Folkman J, Hanahan D: Effects of angiogenesis inhibitors on multistage carcinogenesis in mice. Science. 1999, 284: 808-812. 10.1126/science.284.5415.808.
Holmgren L, O'Reilly MS, Folkman J: Dormancy of micrometastases: balanced proliferation and apoptosis in the presence of angiogenesis suppression [see comments]. Nat Med. 1995, 1: 149-153.
Yamanaka Y, Friess H, Buchler M, Beger HG, Uchida E, Onda M: Overexpression of acidic and basic fibroblast growth factors in human pancreatic cancer correlates with advanced tumor stage. Cancer Res. 1993, 53: 5289-5296.
Shimoyama S, Yamasaki K, Kawahara M, Kaminishi M: Increased serum angiogenin concentration in colorectal cancer is correlated with cancer progression. Clin Cancer Res. 1999, 5: 1125-1130.
Bouck N, Stellmach V, Hsu SC: How tumors become angiogenic. Adv Cancer Res. 1996, 69: 135-174.
Veikkola T, Jussila L, Makinen T, Karpanen T, Jeltsch M, Petrova TV: Signalling via vascular endothelial growth factor receptor-3 is sufficient for lymphangiogenesis in transgenic mice. EMBO J. 2001, 20: 1223-1231. 10.1093/emboj/20.6.1223.
Stetler-Stevenson WG: Matrix metalloproteinases in angiogenesis: a moving target for therapeutic intervention. J Clin Invest. 1999, 103: 1237-1241.
Millauer B, Shawver LK, Plate KH, Risau W, Ullrich A: Glioblastoma growth inhibited in vivo by a dominant-negative Flk-1 mutant. Nature. 1994, 367 (6463): 576-579. 10.1038/367576a0.
Kim KJ, Li B, Winer J, Armanini M, Gillett N, Phillips HS: Inhibition of vascular endothelial growth factor-induced angiogenesis suppresses tumour growth in vivo. Nature. 1993, 362 (6423): 841-4. 10.1038/362841a0.
Buchler P, Reber HA, Buchler MW, Friess H, Hines OJ: VEGF-RII Influences the Prognosis of Pancreatic Cancer. Ann Surg. 2002, 236: 738-749. 10.1097/00000658-200212000-00006.
Stacker SA, Achen MG, Jussila L, Baldwin ME, Alitalo K: Lymphangiogenesis and cancer metastasis. Nat Rev Cancer. 2002, 2: 573-583. 10.1038/nrc863.
Carmeliet P, Collen D: Molecular basis of angiogenesis. Role of VEGF and VE-cadherin. Ann N Y Acad Sci. 2000, 902: 249-262.
Brown JM, Giaccia AJ: The unique physiology of solid tumors. Opportunities (and problems) for cancer therapy. Cancer Res. 1998, 58: 1408-1416.
Tarbe N, Losch S, Burtscher H, Jarsch M, Weidle UH: Identification of rat pancreatic carcinoma genes associated with lymphogenous metastasis. Anticancer Res. 2002, 22: 2015-2027.
Padera TP, Kadambi A, di Tomaso E, Carreira CM, Brown EB, Boucher Y: Lymphatic metastasis in the absence of functional intratumor lymphatics. Science. 2002, 296: 1883-1886. 10.1126/science.1071420.
Yang X, Wei LL, Tang C, Slack R, Mueller S, Lippman ME: Overexpression of KAI1 suppresses in vitro invasiveness and in vivo metastasis in breast cancer cells. Cancer Res. 2001, 61: 5284-5288.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Keleg, S., Büchler, P., Ludwig, R. et al. Invasion and metastasis in pancreatic cancer. Mol Cancer 2, 14 (2003). https://doi.org/10.1186/1476-4598-2-14
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-4598-2-14