Abstract
Background
Previous studies showed that mesothelin (MSLN) plays important roles in survival of pancreatic cancer (PC) cells under anchorage dependent/independent conditions as well as resistance to chemotherapy. The recent success of intratumorally-injected adeno-encoded, chemo/radiation-inducible-promoter driven hTNF-α, (TNFerade) + gemcitabine in pre-clinical models of PC have renewed interest in use of TNF-α as a therapeutic component. To help find additional factors which might affect the therapy, we examined the resistance of MSLN-overexpressing pancreatic cancer cell lines to TNF-α-induced growth inhibition/apoptosis.
Methods
Stable MSLN overexpressing MIA PaCa-2 cells (MIA-MSLN), stable MSLN-silenced AsPC-1 cells (AsPC-shMSLN) and other pancreatic cells (MIA-PaCa2, Panc 28, Capan-1, BxPC3, PL 45, Hs 766T, AsPC-1, Capan-2, Panc 48) were used. NF-κB activation was examined by western blots and luciferase reporter assay. TNF-α induced growth inhibition/apoptosis was measured by MTT, TUNEL assay and caspase activation. IL-6 was measured using luminex based assay.
Results
Compared to low endogenous MSLN-expressing MIA PaCa-2 and Panc 28 cells, high endogenous MSLN-expressing Capan-1, BxPC3, PL 45, Hs 766T, AsPC-1, Capan-2, Panc 48 cells were resistant to TNF-α induced growth inhibition. Stable MSLN overexpressing MIA-PaCa2 cells (MIA-MSLN) were resistant to TNF-α-induced apoptosis while stable MSLN-silenced AsPC1 cells (AsPC-shMSLN) were sensitive. Interestingly, TNF-α-treated MIA-MSLN cells showed increased cell cycle progression and cyclin A induction, both of which were reversed by caspase inhibition. We further found that MIA-MSLN cells showed increased expression of anti-apoptotic Bcl-XL and Mcl-1; deactivated (p-Ser75) BAD, and activated (p-Ser70) Bcl-2. Constitutively activated NF-κB and Akt were evident in MIA-MSLN cells that could be suppressed by MSLN siRNA with a resultant increase in sensitivity of TNF-α induced apoptosis. Blocking NF-κB using IKK inhibitor wedelolactone also increased sensitivity to TNF-α-mediated cytotoxicity with concomitant decrease in Mcl-1. Blocking Akt using PI3K inhibitor also had a likewise effect presumably affecting cell cycle. MIA-MSLN cells produced increased IL-6 and were increased furthermore by TNF-α treatment. SiRNA-silencing of IL-6 increased TNF-α sensitivity of MIA-MSLN cells.
Conclusions
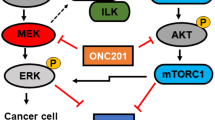
Our study delineates a MSLN-Akt-NF-κB-IL-6-Mcl-1 survival axis that may be operative in PC cells, and might help cancer cells' survival in the highly inflammatory milieu evident in PC. Further, for the success of TNFerade + gemcitabine to be successful, we feel the simultaneous inhibition of components of this axis is also essential.
Similar content being viewed by others
Background
The importance of mesothelin (MSLN) as a biomarker and preferred immunotherapeutic target is steadily growing for many cancers, including pancreatic cancer (PC) [1–3]. The functional consequence of MSLN overexpression in various neoplasms has only recently begun to emerge. Evidence suggests that MSLN confers resistance to anoikis in breast cancer [4] and chemotherapy (platinum + cyclophosphamide/paclitaxel) in ovarian cancer [5]. In pancreatic cancer, it was suggested that MSLN is up-regulated following K-RAS, p53, p16 mutations [6], denoting its advantage in surviving early genotoxic insult. Our previous data [1] showed that MSLN-induced Stat3/cyclin E promotes survival/proliferation of pancreatic cancer cells under reduced serum conditions. Studies to ascertain role of MSLN in resisting other kinds of stress/apoptotic stimuli are thus warranted.
Tumor necrosis factor-α (TNF-α) is a vital member of the TNF-α super family, and plays roles in immunity, cellular remodeling, apoptosis and cell survival [7]. It acts primarily through tumor necrosis factor receptor-1 (TNFR1) (55 kD) to induce apoptosis by activating caspases through both mitochondria-dependent and independent pathways. A second receptor, TNFR2 (75 kD), signals primarily in immune cells [8]. TNF-α was identified as a cytokine that induces tumor necrosis/regression in animals [9]. Early studies suggesting an increased TNF-α sensitivity in oncogene/chemically transformed cells [10, 11] aroused huge hopes but eventually subsided because of the issue of systemic toxicity. Recently, intratumorally-injected adeno-encoded, chemo/radiation-inducible-promoter driven hTNF-α, (TNFerade) in conjunction with conventional chemotherapy (e.g. gemcitabine in pre-clinical models of PC without metastasis at diagnosis) is largely devoid of the toxicity issue and has generated renewed interest in TNF- α treatment [12, 13]. However, a large percentage of patients and/or cell lines are resistant to TNF-α treatment [14, 15]. TNF-α also plays a significant role in the inflammatory etiology of pancreatic cancer [16, 17]. Macrophages and other immune cells invading the tumor space, and tumor cells themselves, secrete TNF-α [17, 18]. TNF-α was found to support pancreatic cancer cell growth through epidermal growth factor receptor (EGFR) and transforming growth factor (TGF-α) expression [19]. Thus factors determining cell fate in presence of TNF-α need to be studied. Therefore, there is a need to: 1) Identify TNF-α-responsive cells to select patients potentially responsive to TNF-α; and 2) ascertain factors responsible for resistance in an effort to improve therapeutic approaches.
NF-κB proteins are transcription factors induced in response to inflammatory and other stress stimuli [17]. A majority of cancer cells become resistant to TNF-α as a result of the activation of NF-κB [17] and consequent induction of anti-apoptotic molecules (e.g. IAPs/Bcl-XL), as the pro-survival effects of TNF-α out-perform the pro-apoptotic effects. Literature shows that blocking NF-κB activation can overcome TNF-α resistance [17], although a constitutive NF-κB activation, rather than the inducible one, has been suggested to be more important [20].
Here, we aimed at deciphering how MSLN overexpression in pancreatic cancer cells affects sensitivity to TNF-α-induced apoptosis. A panel of stable MSLN-overexpressing and MSLN-shRNA silenced cells were treated with TNF- α and examined for the changes of relevant signaling pathways, pro- and anti-apoptotic molecules and cytokine production. Our results demonstrate that MSLN overexpression leads to constitutive NF-κB/Akt activation resulting in resistance to TNF-α mediated cytotoxicity, presumably through de-activation of BAD, activation of Bcl-2 and upregulation of Mcl-1, in an IL-6 dependent manner. Our study may indicate a very important survival axis of MSLN-expressing pancreatic cancer cells in midst of inflammatory cytokines abundant in this cancer.
Methods
Cell culture, chemicals, and antibodies
Human pancreatic cancer cell lines MIA PaCa-2, Panc 28, Capan-1, BxPC3, PL 45, Hs 766T, AsPC-1, Capan-2, Panc 48 were purchased from the American Type Culture Collection (ATCC, Rockville, MD). Puromycin, anti-β-actin antibody were purchased from Sigma (St. Louis, MO). Recombinant human TNF-α was from R&D Systems. Antibodies for p-IκB-α/IκB-α/Bcl-XL/Bcl-2/Mcl-1/BAX/BAD/phospho-BAD/IKK-α/goat anti-rabbit IgG-HRP/goat anti-mouse IgG-HRP are from Cell Signaling Technology Laboratories Inc (Beverly, MA); p65 antibody was from Santa Cruz Biotechnology (Santa Cruz, CA); and Lamin A antibody from Abcam (Cambridge, MA). MSLN overexpressing stable cells were selected in PC cells using retroviral cloning as described previously [3].
Cell proliferation measurement by cell viability assay (MTT)
Two thousand cells were plated and serum starved for 24 h. Various treatments were added to the media and the culture was continued for 2/4/6 days. Proliferating capacity was measured by dividing the OD (590 nm) at a time point by OD at 0 day (day after plating cells). Percent viability was measured by dividing OD value of the treated cells by that for untreated cells multiplied by 100.
TUNEL assay
Apoptosis was evaluated by measuring DNA fragmentation using the Apo-Direct assay kit (Pharmingen, San Diego, CA) for TUNEL (terminal deoxynucleotidyltransferase dUTP nick end labeling). Briefly, cells were serum starved for 24 h (with or without pre-treatments) followed by treatment with 0/10/20/50 ng/ml of TNF-α, for 24/48/72 h. At each time-point, cells were harvested, fixed in 1% Paraformaldehyde, stained in 300 μL of propidium iodine/RNase solution and analyzed by flow cytometry.
Real-Time RT-PCR
MSLN, TNFR1, TNFR2, and GAPDH mRNA levels were analyzed by real-time RT-PCR using the SYBR Green supermix kit (Bio-Rad) using 40 cycles at 95°C for 20 sec and 60°C for 1 min. Target gene mRNA was normalized to GAPDH mRNA level. Relative mRNA level was presented as unit values of 2^[Ct(GAPDH) - Ct(gene of interest)], Ct = threshold cycle. Primer sequences for the genes are as follows; hMSLN sense: 5'-CTCAACCCAGATGCGTTCTCG-3', hMSLN antisense: 5'-AGGTCCACATTGGCCTTCGT-3', hTNFR1 sense: 5'CCTGGTCATTTTCTTTGGTC TTTG-3', hTNFR1 antisense: 5'-GGGTGAAGCCTGGAGTGG-3', hTNFR2 sense: CCAAGCACCTCCTTCCTG, hTNFR2 antisense: CACCACTCCTATTATTAGTAGA CC, hGAPDH sense: 5'-TGCACCACCAACTGCTTA GC-3', hGAPDH antisense: 5'-GGCATGGACTGTGGTCATGAG-3'.
Immunoblot analysis
Cells were lysed with lysis buffer (Cell Signaling Technology, Beverly, MA) with phosphatase and protease inhibitors. Proteins were then resolved by SDS-PAGE, transferred to nitrocellulose membrane (Bio-Rad Laboratories, Hercules, CA) and detected using specific primary antibodies, appropriate HRP-conjugated secondary antibodies and ECL detection system (Amersham Biosciences, UK). The nuclear/cytoplasmic extracts were prepared using the N-PER nuclear and cytoplasmic extraction reagents (Pierce Biotechnology, Rockford, IL, U. S. A).
Treatment with Wedelolactone
MIA-MSLN and MIA-V were treated with 0, 12.5 or 25 μM of the IKK inhibitor Wedelolactone (Calbiochem La Jolla, CA). Cells were collected after 24 h and whole cell and cytoplasmic/nuclear extracts were prepared similarly as previously described [1] and used for western blot to detect various proteins. For functional assays following 12 h Wedelolactone treatment, cells were washed thoroughly, and then treated with various concentrations of TNF-α and outcomes measured.
NF-κB Reporter Assay
One day after plating, cells were co-transfected with 10 μg of pGL3-NF-κB-Firefly luciferase reporter plasmid and 0.1 μg of pGL3-β-Actin-Renilla luciferase as an internal control. 24 h post-transfection, cells were harvested in reporter lysis buffer and lysates were assayed for luciferase activities using a dual luciferase assay kit (Promega, Madison, WI). Luciferase activities were normalized by the ratio of firefly and Renilla luciferase activities. All experiments were carried out in duplicates.
MSLN and IL-6 shRNA/siRNA transfections
For MSLN shRNA transfection experiments, plasmid encoding MSLN shRNA (TR311377, Origene, Rockville, MD) and 29-mer shRNA encoding non-effective expression plasmid against GFP (TR30003) were used. MIA-MSLN and MIA-V cells were transfected with MSLN/IL-6 specific siRNA using Lipofectamine 2000 (Invitrogen, CA, USA). Cells treated with transfection reagent alone (mock) or a control scrambled siRNA (for MSLN siRNA experiments) were used as negative controls. Cells/supernatants were collected 48 h post transfection for mRNA/proteins extraction for real time-PCR/protein detection and 72 h for apoptosis assays.
Statistical Analysis
A two tailed student's t-test was used to compare the statistical difference between two groups. The results were expressed as the mean with SD. The differences were considered statistically significant when the p value was ≤ 0.05, although various levels were represented in the figures with appropriate symbols in the legends.
Results
High MSLN expressing pancreatic cancer cells are resistant to TNF-α-induced growth inhibition/apoptosis
To determine the role of MSLN in PC cells' sensitivity to TNF-α-induced growth-inhibition/apoptosis, cell lines with differential MSLN expression levels (Figure 1A) were used, including MSLN-low MIA PaCa-2 (MIA) [3] and Panc 28, and MSLN-high Capan-1, BxPC3, PL 45, Hs 766T, AsPC-1, Capan-2 and Panc 48 cells. Following serum starvation, cells were treated with 0/20/50 ng/ml of recombinant human TNF-α in serum free medium and the viability determined by MTT. As shown in Figure 1B, MSLN-high cells Capan-1, BxPC3, Hs 766T, AsPC-1, Capan-2 and Panc 48 were relatively resistant to growth inhibition by TNF-α, showing only about 8-17% reduction and in most cases these decreases were not significant. PL 45 was the only cell line which showed around 30% reduction in viability upon TNF-α treatment. At least three cell lines (BxPC3, Capan-2 and Panc 48) actually showed an increase in viability under identical conditions. In contrast, MSLN-low cells MIA PaCa-2 and Panc 28 had viability drastically reduced to 50-60% (*p < 0.05) upon TNF-α treatment. These data indicated a positive correlation between high MSLN expression and increased resistance against TNF-α. To test if serum level affects viability, two MSLN-high cells, BxPC-3/AsPC-1, were serum-starved and treated with 20 ng/ml of TNF-α in 0/0.2/2/10% FBS-containing media. As shown in Additional File 1, Fig. S1, TNF-α treatment did not affect viability in either BxPC-3 or AsPC-1 at any of these FBS concentrations. Given these results, we used serum free media for TNF-α treatment in subsequent experiments.
MSLN expression level positively correlates with protection of pancreatic cancer cell lines from TNF-α induced apoptosis. (A). Evaluation of MSLN mRNA expression in PC cell lines. Relative MSLN mRNA levels in pancreatic cancer cell lines MIA PaCa-2, Panc28, Capan-1, BxPC3, PL 45, Hs 766T, AsPC-1, Capan-2 and Panc 48 cells. Total mRNA from the cell lines were reverse transcribed and tested for MSLN expression by Real Time PCR. The results depicted denote MSLN mRNA levels in each cell line normalized to the GAPDH mRNA level. Relative mRNA level is presented as 2^[Ct(GAPDH)-Ct(MSLN)]. The bars denote SD of duplicate data. (B). A panel of PC cells' viability with or without TNF-α treatment. Cells were seeded in 96-well plates, serum-starved for 24 h, and then cultured in serum free medium ± 20/50 ng/ml of TNF-α for 72 h. Viable cells were quantitated by using MTT assay. Relative fold increase in viability is plotted along Y axis. Data plotted show means of triplicate wells.
To further confirm if MSLN overexpression in PC cells is responsible for resistance to TNF-α-induced apoptosis, we selected at least three different clones of MSLN stably overexpressed MIA PaCa-2 cell lines (MIA-MSLN) to study the role of MSLN in TNF-α-induced apoptosis. As shown in Figure 2A, the untransfected MIA PaCa-2 cells, the vector control cells (MIA-V), and the GFP expressing control cells (MIA-GFP) showed significant viability reduction (**p < 0.01) upon TNF-α treatment, but only MIA-MSLN cells were resistant to this effect (p > 0.05).
MSLN overexpression protects PC cells from TNF-α induced cell viability decrease and apoptosis. (A). MIA-MSLN and control cells viability assay with or without TNF-α treatment. About 3000 cells were plated in 96 well plates, serum starved for 24 h and treated with TNF-α at 20 ng/ml for 96 h after which viability was measured by MTT. Relative increase in viability was measured by dividing viability at a time point by viability of same cells at day 0 (day after plating) and is plotted along Y axis. Data plotted show mean of triplicate wells. Bars denote s.d. of triplicate data. *, # denote p < 0.05, **, ## denote p < 0.01, compared with controls by using student t test. (B). MIA-MSLN cells are resistant to TNF-α induced apoptosis using TUNEL assay. Cells were treated ± 20 ng/ml of TNF-α for 72 h and apoptosis was measured by TUNEL assay. Representative flow histograms show percentage of dUTP-FITC-positive apoptotic cells. Lower panel shows mean number of TUNEL positive cells (duplicate wells). (C). siRNA-silencing MSLN renders MIA-MSLN cells become TNF-α-sensitive measured by TUNEL assay. MIA-V/MIA-MSLN ells were plated in 6 well plates, transfected with siRNA, 24 h after transfection media was replaced by growth media, cells were serum starved and treated with TNF-α at 20 ng/ml for 72 h after which cells were collected, fixed and tested for DNA strand breaks by TUNEL assay. Bars denote s.d. of duplicate data. *, # denote p < 0.05, **, ## denote p < 0.01, compared with controls by using student t test.
We then examined whether reduction in viability of control cells by TNF-α was due to decreased proliferation and/or increased apoptosis. As shown in Figure 2B about 50% of MIA-V cells underwent apoptosis after TNF-α treatment. Under similar conditions, only about 6% of MIA-MSLN cells underwent apoptosis. Bar chart (Figure 2B lower panel) from duplicate treatment wells showed minimal apoptosis in MIA-MSLN cells upon TNF-α treatment, compared to significant apoptosis in MIA-V cells (**p < 0.01)). The extent of apoptosis in MIA-V cells was time and TNF-α concentration-dependent (data not shown). To ascertain whether this protection against TNF-α was a direct effect of MSLN overexpression, we used specific siRNA against MSLN to knock down MSLN expression in MIA-MSLN cells and examine whether this could reverse the protective effect. As shown in Figure 2C, treatment with 10 ng/ml of TNF-α resulted in about 16% and 6% of MIA-V/mock-transfected MIA-MSLN cells undergoing apoptosis, respectively. However, significantly increased apoptosis (37%) was observed in MSLN-siRNA transfected cells. Additional File 2, Fig. S2 confirms that MSLN-specific siRNA significantly (p < 0.005) knocked down MSLN mRNA in MIA-MSLN cells. Furthermore, an examination of 7 high-MSLN-expressing cells Capan1, BxPC3, PL 45, AsPC-1, Capan-2, Panc 48 revealed that all of them were more resistant to TNF-α (20 ng/ml, 72 h) induced apoptosis (Table 1). When the base line TUNEL positivity (without TNF-α treatment) varied around 5%, TNF-α increased the percentages of TUNEL positivity to around 8.5% for most of them. AsPC-1 cells in fact showed a decrease in percentage of apoptotic cells from 4.7% to 1.8%. In comparison, MIA cells, with negligible MSLN expression were very sensitive and showed around 30% apoptosis (Table 1). These data suggest that MSLN overexpression has a direct effect on sensitivity/resistance of PC cells to TNF-α.
MSLN confers resistance to TNF-α-induced apoptosis through caspase-3 activation
To obtain further insight into the mechanism of TNF-α resistance in MIA-MSLN, we compared caspase-3 cleavage ± TNF-α treatment in MIA-V/MIA-MSLN cells. In accordance with our viability/TUNEL assay data, we found decreased caspase-3 cleavage in MIA-MSLN cells compared to MIA-V cells upon TNF-α treatment (Figure 3A). This result was confirmed in another PC cell line, AsPC-1. Shown in Figure 3B, silencing MSLN using MSLN specific shRNA, correlated with increased caspase-3 cleavage with TNF-α treatment. Furthermore, as shown in Figure 3C, when MIA-V cells were pre-treated with pan-caspase inhibitor zVAD-fmk, a reduced percentage of apoptosis (from 87% to about 33%) was observed, indicating that MIA-V cells undergo caspase-dependent apoptosis upon treatment with TNF-α, while MIA-MSLN cells are resistant.
MSLN overexpression makes PC cells resistant to TNF-α induced apoptosis through reduced Caspase 3 cleavage and up regulated anti-apoptotic proteins. (A). Reduced Caspase 3 cleavage in MIA-MSLN cells by 20 ng/ml of TNF-α treatment for 72 h. (B). Silencing endogenous MSLN in AsPC-3 cells renders it sensitive to TNF-α induced apoptosis through increased Caspase 3 cleavage. Panel (i) shows the reduction of MSLN expression level in AsPC-shMSLN stable cell line. Panel (ii) shows the increased caspase 3 cleavage upon TNF-α treatment. (C). Pre-treatment with pan-caspase inhibitor zVAD-fmk renders MIA-V cells resistant to TNF-α-induced apoptosis. Cells were treated with 20 ng/ml of TNF-α for 72 h and then stained with TUNEL assay. (D). Pro and anti-apoptotic molecules expression in MIA-V/MIA-MSLN cells with or without treatment of 20 ng/ml TNF-α assayed by Western blot. (E). Effect of different TNF-α doses on selected pro/anti-apoptotic molecules expression in MIA-V/MIA-MSLN cells. (F). Effect of zVAD-fmk pre-treatment on various pro and anti-apoptotic molecules expression in MIA-V/MIA-MSLN cells after treatment with 50 ng/ml of TNF-α for 72 h.
Upregulated anti-apoptotic proteins and downregulated pro-apoptotic proteins in MIA-MSLN cells
To further delineate the mechanism of TNF-α-resistance in MIA-MSLN cells, we examined expression of key anti/pro-apoptotic molecules ± TNF-α treatment. As shown in Figure 3D, two anti-apoptotic Bcl-2 family members, Bcl-XL/Mcl-1, were upregulated in MIA-MSLN cells. Importantly, Mcl-1 levels remained high even after TNF-α treatment. In MIA-V cells, on the other hand, Mcl-1 level increased slightly upon TNF-α treatment, but still remained lower than in MIA-MSLN cells. Another significant aspect is increased phosphorylation of anti-apoptotic molecule Bcl-2 at Ser70 position in its positive regulatory loop enhancing its anti-apoptotic action [21]. MIA-MSLN cells had increased p-Ser70; which could be a major factor behind the observed TNF-α resistance. In a dose-dependence study, we found that even with 50 ng/ml TNF-α treatment, Bcl-XL/Mcl-1 expression were still high in MIA-MSLN cells compared with control cells (Figure 3E). TNF-α treatment slightly decreased expression of two pro-apoptotic molecules, BAX and BAD (Figure 3D) in MIA-MSLN cells compared with a slight increase of BAX in control cells. Dephosphorylated BAD promotes apoptosis by binding and sequestering Bcl-2 and/or Bcl-XL away from pro-apoptotic Bax/Bak proteins [22, 23]. Phosphorylated BAD, conversely, is bound and sequestered in cytosol by the chaperone protein 14-3-3. Phosphorylations at Ser75/Ser99/Ser118 are thus inhibitory for the pro-apoptotic function of BAD [24, 25] as these affect interactions with 14-3-3 and/or Bcl-2 family members. The p-BAD (Ser75) level was consistently high in MIA-MSLN ± TNF-α treatment (Figure 3D, E) and thus might make BAD ineffective in inducing apoptosis in MIA-MSLN cells. Further, MIA-V pre-treatment with zVAD-fmk reversed the pattern of expression of the above pro- and anti-apoptotic molecules in the TNF-α treated MIA-V (Figure 3F), concomitant with the apoptosis reversal as shown in Figure 3C.
TNF-α induced cyclin A and concomitant cell cycle progression in MIA-MSLN cells
Loss of cyclin A and G1-cell cycle arrest was found to precede cell-killing by TNF-α in endothelial cells [26]. TNF-α promoted cell cycle progression and cyclin A synthesis in serum starved HeLa cells to rescue them from pro-apoptotic effects [27]. To determine whether TNF-α treatment promotes cell cycle progression or arrest in MIA-MSLN cells, cell cycle analysis was used. Shown in Figure 4A, we found an induction of serum-starved MIA-MSLN cells into S phase (from 27.8% to 50%) by 10/20 ng/ml of TNF-α in presence of 0.2% serum with concomitant decrease of cells in G0/G1 phase. In contrast, the number of MIA-V cells going to S phase was much lower (from 29% to 33%). This indicates that TNF-a promotes growth of MSLN overexpressing cells. We further examined S-phase promoting cyclins A/E [28] and cdk2. Consistent with our previous report [1], cyclin E/cdk2 were slightly elevated in MIA-MSLN cells but remained unaffected by TNF-a treatment (Figure 4B). However, there was a clear induction of cyclin A in MIA-MSLN cells but not in MIA-V cells by TNF-α treatment.
TNF-α induces S phase progression and induction of cyclin A in MIA-MSLN cells. (A). Cell cycle analysis of MIA-V/MIA-MSLN cells treated with 10/20 ng/ml of TNF-α for 24 h. (B). Cell cycle related molecules detection by western blot using the lysates from cells treated as in (A). (C). Cell cycle analysis of MIA-V/MIA-MSLN cells after pre-treatment with zVAD-fmk and then treated with 50 ng/ml of TNF-α for 72 h. (D). Cyclin A detection by western blot using the cell lysates from cells treated as in (C).
Since we found previously that caspase inhibitor z-VAD-fmk rescued MIA-V cell from TNF-a-induced apoptosis, we examined its effect on both S phase progression and cyclin A induction. Interestingly, z-VAD-fmk pre-treatment not only decreased the apoptotic sub-G0 fraction (from 8% to 2.9%), it also increased MIA-V cells in S phase (from 15.4% to 26.9%) by TNF-α treatment (Figure 4C). This indicates that a failure to go into DNA synthesis is linked to MIA-V cells' induction to apoptosis by TNF-a treatment. In agreement with this observation, cyclin A expression also increased in z-VAD-fmk treated MIA-V cells (Figure 4D). Together, our data shows that TNF-a induces MSLN overexpressing PC cells progress to S phase through upregulation of cyclin A which makes the cells resistant its cytotoxic effects.
The level of TNF receptor-1 expression is unchanged upon MSLN overexpression
To further dissect MIA-MSLN cells' resistance to TNF-α-induced apoptosis, we examined the expression of TNF receptors one (TNFR1) and two (TNFR2). Real-time PCR data showed there was high expression of TNFR1 (Additional File 3, Fig. S3A) and low expression of TNFR2 (data not shown) in both MIA-V and MIA-MSLN cells. TNFR1 was slightly decreased in MIA-MSLN cells (statistically insignificant). Western blot analysis showed that there was no significant difference of TNFR1 protein (~55 kD) expression between MIA-V and MIA-MSLN cells (Additional File 3, Fig. S3B). This data indicate that resistance of MSLN high expressing cells to TNF-α may not be caused by a differential receptor expression on these cells.
MSLN overexpression induces NF-κB activation and nuclear translocation of its subunits in pancreatic cancer cell MIA PaCa-2
To identify signals activated by MSLN, we examined various transcription factors, kinases, and related intermediates in MIA-MSLN cells. One of our major findings is that MIA-MSLN cells had significantly higher constitutive NF-κB activity than control cells. As represented in Figure 5A, relative NF-κB luciferase activity was increased 26-fold in MIA-MSLN cells compared to control cells. Figure 5B-(i) shows an increased nuclear translocation of p65/p50 subunits in MIA-MSLN cells. MSLN shRNA reduced nuclear translocation of p65 (Figure 5B, ii), indicating a causal relationship between MSLN overexpression and NF-κB activation.
MSLN overexpression is associated with activation of NF-κB and Akt activity in PC cells. (A). Enhanced NF-κB reporter gene activity in MIA-MSLN cells. Data plotted was measured as ratio of co-transfected firefly-NF-κB reporter normalized to Actin-Renilla. ** denote p < 0.01, compared with controls, t test. (B). Nuclear protein from MIA-MSLN and control cells were subjected to western blot to detect nuclear-translocated p65, p50 and nuclear envelop protein Lamin A (panel i). Panel ii showed inhibited nuclear protein translocation when MIA-MSLN cells were transfected with MSLN specific shRNA encoding plasmid or control plasmids. (C). Whole cell extract (WCE) or nuclear protein from MIA-V and two pools of MIA-MSLN cells were probed for various IκB-α degradation pathway proteins in western blot. (D). Whole protein from MIA-V/MIA-MSLN (panel i) and from the AsPC-1 shMSLN and control cells (panel ii) were probed for various PI3k-Akt pathway proteins. Note: (panel i) data has individual lanes combined from a single electrophoresis gel.
Nuclear translocation of p65 was observed in two different MSLN overexpressing cell populations selected at different times (Figure 5C). We also observed an increased phosphorylation of NF-κB cytoplasm-sequestering inhibitor IκB-α (Figure 5C). Not surprisingly, we found an increased expression of IκB-α, a NF-κB regulated gene, in both MSLN overexpressing cells. An increased phosphorylation of NF-κB subunit p65 was also seen. All these data indicate that the IKK-IκB-α pathway may be operative in MSLN overexpressing cells.
MSLN overexpression activates Akt activity in pancreatic cancer cells
To delineate MSLN-induced signaling, we also examined Akt pathway in MSLN overexpression or silencing stable cells. Shown in Figure 5D, we found activation of Akt (increased p-Thr473 and total Akt), the Akt kinase PDK1 (p-Ser241), and a deactivation of Akt inhibitor PTEN (p-Ser380) in MIA-MSLN cells. Correspondingly, the MSLN-silenced AsPC-1 cells (AsPC-shMSLN) had decreased p-Akt, p-GSK-3β (p-Ser9), PDK1 (p-Ser241) and PTEN (p-Ser380). Together, this data indicate that MSLN expression leads to Akt activation in PC cells.
Abrogating the PI3K and NF-κB activity sensitizes MIA-MSLN cells to TNF-α-induced apoptosis
Aberrant NF-κB activity in cancer cells is implicated in apoptosis resistance to various stimuli, including inflammatory cytokines like TNF-α [17]. Activated Akt was implicated in proliferation/survival of PC cells and/or resistance to TNF-α mediated cell death in various cancers [29, 30]. Here, we found that MSLN-induced NF-κB rescues cells from TNF-α-induced apoptosis. Pre-treatment with the pharmacological IKK inhibitor wedelolactone or the PI3K inhibitor Ly2940002 rendered MIA-MSLN cells sensitive to TNF-α-mediated viability reduction (Figure 6A, B) and apoptosis (Figure 6C). While the MIA-V cells had a 45% reduction in cell viability following TNF-α treatment, 100% of MIA-MSLN cells remained viable after 3 days of treatment. Twelve hours pre-treatment with Wedelactone, however, made MIA-MSLN cells extremely sensitive to TNF-α-induced apoptosis, with 83% and 93% reduction in viability respectively with 12.5 μg/ml and 25 μg/ml of Wedelolactone (Figure 6A). Pretreatment with Ly294002 also reduced viability to similar levels (Figure 6B). The TUNEL-positive apoptotic fraction of MIA-MSLN cells after TNF-α treatment (20 ng/ml, 72 h) increased from 5% to 80% (Figure 6C) upon pre-treatment with 25 μg/ml of Wedelolactone and 44% upon pretreatment with Ly294002. These data clearly indicate a role of constitutive NF-κB as well as activated Akt in MIA-MSLN cells' protection from TNF-α-induced apoptosis.
Inhibiting NF-κB/Akt pathway or endogenous IL-6 abrogates MIA-MSLN cells resistance to TNF-α-induced apoptosis. (A). MIA-MSLN cell viability was reduced upon pre-treatment with IKK inhibitor wedelolactone and then 20 ng/ml of TNF-α for 72 h. (B). MIA-MSLN cell viability was reduced upon pre-treatment with PI3K inhibitor Ly 2940002 and then 20 ng/ml of TNF-α for 72 h. (C). Cell apoptosis was determined by TUNEL assay in samples treated as in (A) and (B). (D). Proteins from similarly treated cells were subjected to western blot to detect caspase 3 cleavage and key pro/anti-apoptotic molecules.
Inhibiting PI3K and NF-κB activity increases Caspase activity and decreases anti-apoptotic protein expression in MIA-MSLN cells
We further found that both Ly294002 & Wedelolactone pre-treatment increased caspase-3 activation in MIA-MSLN cells after TNF-α treatment compared with controls (Figure 6D). In addition, the levels of Mcl-1/Bcl-XL were also reduced in Wedelolactone/TNF-α-treated MIA-MSLN (Figure 6D). Interestingly, we did not find a reduction in Mcl-1 by Ly294002 pre-treated cells. We then did a cell cycle analysis (Additional File 4, Fig. S4) with similar treatments and found that Ly2940002/TNF-α caused a G1 arrest (from 54.6%G1/26.6%S to 73.6%G1/12.4%S) of MIA-MSLN. In contrast, Wedelolactone/TNF-α treatment decreased S phase cells (to 17.4%) but increased G2 (23.9%) and partly increased sub G0 cells thus denoting a G2 arrest and apoptosis. Our data strongly implicate Mcl-1 may act as a major molecule that protecting MSLN overexpressing cells from TNF-α-mediated cytotoxicity.
Silencing the endogenous production of IL-6 in MIA-MSLN cells increases the sensitivity of the cells to TNF-α-mediated cytotoxicity
We previously showed that cells overexpressing MSLN either naturally (e.g. BxPC3) or artificially (e.g. MIA-MSLN) express increased IL-6 at both mRNA/protein levels [31]. We also found this IL-6 was NF-κB-regulated. Previous studies showed IL-6 as protective against cytokine-induced apoptosis in various cells [32, 33]. We asked whether protective effect of MSLN against TNF-α is due to increased IL-6. We examined IL-6 production by MIA-V/MIA-MSLN cells ± TNF-α treatment. As demonstrated in Figure 7A, a significantly higher production of IL-6 was observed in MIA-MSLN cells, and this was further increased by TNF-α treatment. We then blocked IL-6 production using IL-6 specific siRNA pool and examined the effect of TNF-α treatment on apoptosis by TUNEL. Shown in Figure 7B, IL-6-silenced MIA-MSLN cells had increased apoptotic (28% TUNEL positive) fraction after TNF-α treatment compared to only 9% in non-targeting siRNA transfected cells, indicating the protective role of IL-6.
High levels of IL-6 in MIA-MSLN cells plays important role in resistance to TNF-α-mediated cytotoxicity. (A). Elevated constitutive and TNF-α induced IL-6 expression in MIA-MSLN cells using Luminex-based IL-6 assay kit. Y-axis represents fluorescence corresponding to IL-6-levels. Bars denote SD of duplicate data. (B). Inhibiting endogenous IL-6 by siRNA sensitizes MIA-MSLN cells to TNF-α-induced apoptosis. MIA-MSLN cells were either mock-transfected (control) or transfected with non-targeting (siNT) or IL-6 specific siRNA pools (siIL-6) and treated with 20 ng/ml of TNF-α for 72 h and analyzed for TUNEL positivity. Flow histograms show percentage of dUTP-FITC-positive apoptotic cells. Plots are representatives of three independent experiments.
Discussion
In our previous publications, we have reported that MSLN overexpression is associated with increased migration [3], and increased colony forming ability under both anchorage independence as well as in matrigel [31]. These characteristics all pointing towards a tumorigenic role and metastasis related phenotypes of mesothelin. The current study is a significant step forward in understanding the role of MSLN in PC pathogenesis, especially with regards to cancer cell survival in a highly inflammatory milieu, a hallmark of this deadly cancer. There is a clear correlation between MSLN level and resistance to TNF-α induced apoptosis in various PC cells lines. We also convincingly show that forced overexpression of MSLN in the PC cell line MIA PaCa-2 made these cells resistant to TNF-α-induced growth inhibition/apoptosis, and that silencing endogenous MSLN in AsPC-1 cells renders these cells sensitive. TNF-α also induced S-phase promoting effects in MIA-MSLN cells with concomitant induction of cyclin A. Furthermore, an increased constitutive activation of NF-κB in MIA-MSLN cells seemed to be responsible for its apparent TNF-α resistance, as blocking this activation using the IKK inhibitor wedelolactone significantly increased the sensitivity to TNF-α-mediated cytotoxicity. Similarly, an activated Akt pathway also contributes towards resistance to growth inhibition by TNF-α. Furthermore, high endogenous production of NF-κB-regulated IL-6 and increased Mcl-1 seem to be direct players in this protection. Our results describe a novel function for MSLN, inducing an NF-κB/Akt-dependent, anti-apoptotic pathway which can protect PC cells from TNF-α-induced apoptosis, and describe a probable mechanism of PC cell survival in midst of inflammation and inflammatory mediators.
Previous data [14, 34] and ours presented here show that PC cell lines Capan-1, BxPC3, PL 45, Hs 766T, AsPC-1, Capan-2, Panc 48 cells are resistant to TNF-α. Interestingly, all these cells have high MSLN expression [35], while TNF-α sensitive cells such as MIA PaCa-2 and Panc 28 expresses low MSLN [35]. In addition, silencing MSLN expression in AsPc-1/MIA-MSLN cells reversed the TNF-α resistance, indicating a direct role of MSLN. The ability of normal mesothelial and mesothelioma cells [36–38] to survive/proliferate in presence of TNF-α is intriguing. Another interesting observation is that TNF-α induces MIA-MSLN cells to go into cell cycle rather than stalling the process, similar to previous reports of auto/paracrine growth stimulation by TNF-α [17]. PC cells are prone to proliferation by TNF-α through up-regulation of PDGF [39] and/or EGFR/TGF-α [19]. Given our data it's a strong proposition that MSLN contribute towards this. Further, our PI3 kinase inhibition data indicates that the cells' ability to evade growth inhibition might be due to activated Akt found in these cells.
Mesothelin promotes both survival and proliferation under anchorage dependence [1, 3] and independence [4, 31] in low serum conditions [31]. Furthermore, loss of cyclin A and G1-cell cycle seemed to proceed cell-killing by TNF-α in endothelial cells & TNF-α promoted cell cycle progression and cyclin A synthesis [26, 27]. Based on these facts, we raised a question whether a lack of cell cycle promotion by TNF-α is essential for its pro-apoptotic role in MSLN-low cells. In addition, caspase inhibition not only decreased the apoptotic sub-G0 fraction (from 8% to 2.9%), but also increased MIA-V cells in S phase (from 15.4% to 26.9%) by TNF-α treatment (Figure 4C). This indicates that a failure to go into DNA synthesis is linked to MIA-V cells' induction to apoptosis by TNF-a treatment.
Bcl-2 regulates apoptosis by heterodimerization with its pro-apoptotic partner, Bax, to maintain mitochondrial integrity [40]. Phosphorylation of Bcl-2 at Ser70 is necessary for its anti-apoptotic function [41]. Although we have not identified the responsible kinase, nevertheless an increased p-Ser70 in MIA-MSLN cells is a significant observation with respect to its anti-apoptotic role. BAD is a pro-apoptotic Bcl-2 family member coordinating survival and mitochondrial cell death signals [42]. BAD phosphorylation is essential to block apoptosis [24]. An increased Ser75 phosphorylation of BAD in MIA-MSLN cells could be thus critical for its anti-apoptotic functions. PI3K activity supports EGF/serum induced survival of cancer cells, through phosphorylation-mediated inactivation of BAD [43] although other kinases could also control Ser75 phosphorylation [25]. Given that inhibiting PI3K activity rendered MIA-MSLN cells sensitive to TNF-α, the pathway could be involved in BAD-inactivation and hence protection from TNF-α. Another interesting finding is that Mcl-1 is a major player in MSLN-induced resistance to TNF-α. Although primarily a Stat3 regulated gene, NF-κB regulated Mcl-1 is responsible for TRAIL resistance in various tumors [44, 45] including the MSLN-high PC cell line BxPC-3 [46]. The fact that MIA-MSLN cells have activated Stat3 [1] indicates a probable role of the factor in TNF-α resistance as well. MSLN-induced Mcl-1 upregulation has been reported in taxol resistant ovarian cancer cells [47] indicating its importance in MSLN induced protection from various apoptotic stimuli.
TNF-α induces NF-κB activation in most cells [17, 18] but this is not always sufficient to avoid the pro-apoptotic effects of TNF-α; rather, a constitutive activation of NF-κB seems to be necessary [20]. Similarly, we found that constitutively activated NF-κB is responsible for resistance to TNF-α-induced apoptosis. Autocrine IL-6-induced Mcl-1 could protect prostate cancer cells from apoptosis [33]. IL-6 also protects pancreatic islet beta cells from TNF-α-induced cell death [32]. Incidentally, MSLN is highly expressed in the islet beta cells of developing rat pancreas [48] leading one to speculate its role in IL-6 production and subsequent TNF-α protection. We found that MIA-MSLN cells produce increased IL-6 in a NF-κB regulated manner [31] and IL-6 production increased significantly upon TNF-α treatment. In fact, studies reveal that co-operative action of IL-6 and TNF-α induces proliferation during liver regeneration after multiple partial hepatectomy [49]. Thus it could be the co-operativity between the two that results in S-phase induction by TNF-α under reduced serum conditions. The elevated IL-6 may be responsible for increased Mcl-1 expression and partially contribute to Stat3 activation in these cells. More precisely, we hypothesize that a MSLN-NF-κB-IL-6-Stat3-Mcl-1 axis may be a major survival axis operating in these cells. Our data clearly show that silencing endogenous IL-6 increased sensitivity of MIA-MSLN cells to TNF-α-induced cell death. Although Mcl-1 is not a direct target for Akt, NF-kappa B and Akt signaling pathways can converge. Therefore, an indirect relationship could be established between Akt and Mcl-1 through NF-κB. MSLN-Akt-NF-kB-IL-6-Mcl-1 survival axis could be unique for PC cells.
The recent success of intratumorally-injected adeno-encoded, radiation-inducible-promoter driven hTNF-α, AdEgr.TNF.11D (TNFerade)+gemcitabine [12] proves TNF-α could still be useful as anti-tumor agent. The balance between cytotoxicity and stimulation of growth factor synthesis determines which biological effects will finally result from TNF-α. This critical balance eventually decides which PC cells might escape the anti-proliferative effects of TNF-α, and the effects that these properties will have on patient tumors. Deciphering the mechanism of TNF-α resistance in MSLN-expressing tumors would thus help provide rationale for designing combined chemotherapy with TNF-α ± MSLN inhibition to efficiently target these tumors.
Conclusions
In summary, we found that MSLN overexpressing cells are generally resistant to TNF-α induced cytotoxicity and cell inhibition, which helps the cells thrive in an inflammatory milieu which is a hallmark of PC. There is a renewed interest in intratumorally-injected TNFerade in conjunction with conventional chemotherapy in PC without metastasis at diagnosis. Because MSLN is expressed in about 90% of PC patients, a simultaneous blocking of its action is warranted for the success of a therapeutic regimen.
Abbreviations
- MSLN:
-
mesothelin
- PC:
-
pancreatic cancer
- TNF-α:
-
Tumor necrosis factor-α
- TNFR:
-
tumor necrosis factor receptor
- TNFerade:
-
adeno-encoded, chemo/radiation-inducible-promoter driven hTNF-α
- MIA-MSLN:
-
a MIA PaCa2 cell line that stably overexpressing MSLN
- MIA-V:
-
a MIA PaCa2 cell line with vector control
- MIA-GFP:
-
a MIA PaCa2 cell line that stably overexpressing GFP
- HPDE:
-
Human pancreatic ductal epithelial cell
References
Bharadwaj U, Li M, Chen C, Yao Q: Mesothelin-induced pancreatic cancer cell proliferation involves alteration of cyclin E via activation of signal transducer and activator of transcription protein 3. Mol Cancer Res. 2008, 6: 1755-1765. 10.1158/1541-7786.MCR-08-0095
Hassan R, Ho M: Mesothelin targeted cancer immunotherapy. Eur J Cancer. 2008, 44: 46-53. 10.1016/j.ejca.2007.08.028
Li M, Bharadwaj U, Zhang R, Zhang S, Mu H, Fisher WE, Brunicardi FC, Chen C, Yao Q: Mesothelin is a malignant factor and therapeutic vaccine target for pancreatic cancer. Mol Cancer Ther. 2008, 7: 286-296. 10.1158/1535-7163.MCT-07-0483
Uehara N, Matsuoka Y, Tsubura A: Mesothelin promotes anchorage-independent growth and prevents anoikis via extracellular signal-regulated kinase signaling pathway in human breast cancer cells. Mol Cancer Res. 2008, 6: 186-193. 10.1158/1541-7786.MCR-07-0254
Cheng WF, Huang CY, Chang MC, Hu YH, Chiang YC, Chen YL, Hsieh CY, Chen CA: High mesothelin correlates with chemoresistance and poor survival in epithelial ovarian carcinoma. Br J Cancer. 2009, 100: 1144-1153. 10.1038/sj.bjc.6604964
Koorstra JB, Hustinx SR, Offerhaus GJ, Maitra A: Pancreatic carcinogenesis. Pancreatology. 2008, 8: 110-125. 10.1159/000123838
Szlosarek P, Charles KA, Balkwill FR: Tumour necrosis factor-alpha as a tumour promoter. Eur J Cancer. 2006, 42: 745-750. 10.1016/j.ejca.2006.01.012
Balkwill F: TNF-alpha in promotion and progression of cancer. Cancer Metastasis Rev. 2006, 25: 409-416. 10.1007/s10555-006-9005-3
Carswell EA, Old LJ, Kassel RL, Green S, Fiore N, Williamson B: An endotoxin-induced serum factor that causes necrosis of tumors. Proc Natl Acad Sci USA. 1975, 72: 3666-3670. 10.1073/pnas.72.9.3666
Fernandez A, Marin MC, McDonnell T, Ananthaswamy HN: Differential sensitivity of normal and Ha-ras-transformed C3H mouse embryo fibroblasts to tumor necrosis factor: induction of bcl-2, c-myc, and manganese superoxide dismutase in resistant cells. Oncogene. 1994, 9: 2009-2017.
Komori A, Yatsunami J, Suganuma M, Okabe S, Abe S, Sakai A, Sasaki K, Fujiki H: Tumor necrosis factor acts as a tumor promoter in BALB/3T3 cell transformation. Cancer Res. 1993, 53: 1982-1985.
Murugesan SR, King CR, Osborn R, Fairweather WR, O'Reilly EM, Thornton MO, Wei LL: Combination of human tumor necrosis factor-alpha (hTNF-alpha) gene delivery with gemcitabine is effective in models of pancreatic cancer. Cancer Gene Ther. 2009
Weichselbaum RR, Kufe D: Translation of the radio- and chemo-inducible TNFerade vector to the treatment of human cancers. Cancer Gene Ther. 2009, 16: 609-619. 10.1038/cgt.2009.37
Lyu MA, Kurzrock R, Rosenblum MG: The immunocytokine scFv23/TNF targeting HER-2/neu induces synergistic cytotoxic effects with 5-fluorouracil in TNF-resistant pancreatic cancer cell lines. Biochem Pharmacol. 2008, 75: 836-846. 10.1016/j.bcp.2007.10.013
Wang CY, Cusack EV, Liu R, Baldwin EV: Control of inducible chemoresistance: enhanced anti-tumor therapy through increased apoptosis by inhibition of NF-kappaB. Nat Med. 1999, 5: 412-417. 10.1038/7410
Schmiegel WH, Caesar J, Kalthoff H, Greten H, Schreiber HW, Thiele HG: Antiproliferative effects exerted by recombinant human tumor necrosis factor-alpha (TNF-alpha) and interferon-gamma (IFN-gamma) on human pancreatic tumor cell lines. Pancreas. 1988, 3: 180-188. 10.1097/00006676-198804000-00012
Aggarwal BB, Shishodia S, Sandur SK, Pandey MK, Sethi G: Inflammation and cancer: how hot is the link?. Biochem Pharmacol. 2006, 72: 1605-1621. 10.1016/j.bcp.2006.06.029
Aggarwal BB: Signalling pathways of the TNF superfamily: a double-edged sword. Nat Rev Immunol. 2003, 3: 745-756. 10.1038/nri1184
Schmiegel W, Roeder C, Schmielau J, Rodeck U, Kalthoff H: Tumor necrosis factor alpha induces the expression of transforming growth factor alpha and the epidermal growth factor receptor in human pancreatic cancer cells. Proc Natl Acad Sci USA. 1993, 90: 863-867. 10.1073/pnas.90.3.863
Giri DK, Aggarwal BB: Constitutive activation of NF-kappaB causes resistance to apoptosis in human cutaneous T cell lymphoma HuT-78 cells. Autocrine role of tumor necrosis factor and reactive oxygen intermediates. J Biol Chem. 1998, 273: 14008-14014. 10.1074/jbc.273.22.14008
Deng X, Kornblau SM, Ruvolo PP, May EV: Regulation of Bcl2 phosphorylation and potential significance for leukemic cell chemoresistance. J Natl Cancer Inst Monogr. 2001, 30-37.
Cory S, Adams JM: The Bcl2 family: regulators of the cellular life-or-death switch. Nat Rev Cancer. 2002, 2: 647-656. 10.1038/nrc883
Downward J: How BAD phosphorylation is good for survival. Nat Cell Biol. 1999, 1: E33-35. 10.1038/10026
Datta SR, Ranger AM, Lin MZ, Sturgill JF, Ma YC, Cowan CW, Dikkes P, Korsmeyer SJ, Greenberg ME: Survival factor-mediated BAD phosphorylation raises the mitochondrial threshold for apoptosis. Dev Cell. 2002, 3: 631-643. 10.1016/S1534-5807(02)00326-X
Eisenmann KM, VanBrocklin MW, Staffend NA, Kitchen SM, Koo HM: Mitogen-activated protein kinase pathway-dependent tumor-specific survival signaling in melanoma cells through inactivation of the proapoptotic protein bad. Cancer Res. 2003, 63: 8330-8337.
Spyridopoulos I, Mayer P, Shook KS, Axel DI, Viebahn R, Karsch KR: Loss of cyclin A and G1-cell cycle arrest are a prerequisite of ceramide-induced toxicity in human arterial endothelial cells. Cardiovasc Res. 2001, 50: 97-107. 10.1016/S0008-6363(01)00196-1
Volland S, Amtmann E, Sauer G: TNF accelerates the S-phase of the cell cycle in tumor cells. Int J Cancer. 1994, 56: 698-705. 10.1002/ijc.2910560515
Satyanarayana A, Kaldis P: Mammalian cell-cycle regulation: several Cdks, numerous cyclins and diverse compensatory mechanisms. Oncogene. 2009, 28: 2925-2939. 10.1038/onc.2009.170
Liu CJ, Lo JF, Kuo CH, Chu CH, Chen LM, Tsai FJ, Tsai CH, Tzang BS, Kuo WW, Huang CY: Akt Mediates 17 beta-Estradiol and/or Estrogen Receptor alpha Inhibition of LPS-Induced Tumor Necrosis Factor-alpha Expression and Myocardial Cell Apoptosis by Suppressing the JNK1/2-NFkappaB Pathway. J Cell Mol Med. 2009
Qiu J, Xiao J, Han C, Li N, Shen X, Jiang H, Cao X: Potentiation of tumor necrosis factor-alpha-induced tumor cell apoptosis by a small molecule inhibitor for anti-apoptotic protein hPEBP4. J Biol Chem. 285: 12241-12247.
Bharadwaj U, Marin-Muller C, Li M, Chen C, Yao Q: Mesothelin Overexpression Promotes Autocrine IL-6/sIL-6R Trans-signaling to stimulate Pancreatic Cancer Cell Proliferation. Carcinogenesis. 2011, 32: 1013-1024. 10.1093/carcin/bgr075
Choi SE, Choi KM, Yoon IH, Shin JY, Kim JS, Park WY, Han DJ, Kim SC, Ahn C, Kim JY: IL-6 protects pancreatic islet beta cells from pro-inflammatory cytokines-induced cell death and functional impairment in vitro and in vivo. Transpl Immunol. 2004, 13: 43-53. 10.1016/j.trim.2004.04.001
Cavarretta IT, Neuwirt H, Untergasser G, Moser PL, Zaki MH, Steiner H, Rumpold H, Fuchs D, Hobisch A, Nemeth JA, Culig Z: The antiapoptotic effect of IL-6 autocrine loop in a cellular model of advanced prostate cancer is mediated by Mcl-1. Oncogene. 2007, 26: 2822-2832. 10.1038/sj.onc.1210097
Bai J, Sui J, Demirjian A, Vollmer EV, Marasco W, Callery MP: Predominant Bcl-XL knockdown disables antiapoptotic mechanisms: tumor necrosis factor-related apoptosis-inducing ligand-based triple chemotherapy overcomes chemoresistance in pancreatic cancer cells in vitro. Cancer Res. 2005, 65: 2344-2352. 10.1158/0008-5472.CAN-04-3502
Argani P, Iacobuzio-Donahue C, Ryu B, Rosty C, Goggins M, Wilentz RE, Murugesan SR, Leach SD, Jaffee E, Yeo CJ: Mesothelin is overexpressed in the vast majority of ductal adenocarcinomas of the pancreas: identification of a new pancreatic cancer marker by serial analysis of gene expression (SAGE). Clin Cancer Res. 2001, 7: 3862-3868.
Catalan MP, Subira D, Reyero A, Selgas R, Ortiz-Gonzalez A, Egido J, Ortiz A: Regulation of apoptosis by lethal cytokines in human mesothelial cells. Kidney Int. 2003, 64: 321-330. 10.1046/j.1523-1755.2003.00062.x
Gordon GJ, Mani M, Mukhopadhyay L, Dong L, Yeap BY, Sugarbaker DJ, Bueno R: Inhibitor of apoptosis proteins are regulated by tumour necrosis factor-alpha in malignant pleural mesothelioma. J Pathol. 2007, 211: 439-446. 10.1002/path.2120
Yang H, Bocchetta M, Kroczynska B, Elmishad AG, Chen Y, Liu Z, Bubici C, Mossman BT, Pass HI, Testa JR: TNF-alpha inhibits asbestos-induced cytotoxicity via a NF-kappaB-dependent pathway, a possible mechanism for asbestos-induced oncogenesis. Proc Natl Acad Sci USA. 2006, 103: 10397-10402. 10.1073/pnas.0604008103
Kalthoff H, Roeder C, Humburg I, Thiele HG, Greten H, Schmiegel W: Modulation of platelet-derived growth factor A- and B-chain/c-sis mRNA by tumor necrosis factor and other agents in adenocarcinoma cells. Oncogene. 1991, 6: 1015-1021.
Yip KW, Reed JC: Bcl-2 family proteins and cancer. Oncogene. 2008, 27: 6398-6406. 10.1038/onc.2008.307
Deng X, Ruvolo P, Carr B, May EV: Survival function of ERK1/2 as IL-3-activated, staurosporine-resistant Bcl2 kinases. Proc Natl Acad Sci USA. 2000, 97: 1578-1583. 10.1073/pnas.97.4.1578
Bergmann A: Survival signaling goes BAD. Dev Cell. 2002, 3: 607-608. 10.1016/S1534-5807(02)00328-3
Chao OS, Clement MV: Epidermal growth factor and serum activate distinct pathways to inhibit the BH3 only protein BAD in prostate carcinoma LNCaP cells. Oncogene. 2006, 25: 4458-4469. 10.1038/sj.onc.1209421
Ricci MS, Kim SH, Ogi K, Plastaras JP, Ling J, Wang W, Jin Z, Liu YY, Dicker DT, Chiao PJ: Reduction of TRAIL-induced Mcl-1 and cIAP2 by c-Myc or sorafenib sensitizes resistant human cancer cells to TRAIL-induced death. Cancer Cell. 2007, 12: 66-80. 10.1016/j.ccr.2007.05.006
Wang X, Chen W, Zeng W, Bai L, Tesfaigzi Y, Belinsky SA, Lin Y: Akt-mediated eminent expression of c-FLIP and Mcl-1 confers acquired resistance to TRAIL-induced cytotoxicity to lung cancer cells. Mol Cancer Ther. 2008, 7: 1156-1163. 10.1158/1535-7163.MCT-07-2183
Huang S, Sinicrope FA: BH3 mimetic ABT-737 potentiates TRAIL-mediated apoptotic signaling by unsequestering Bim and Bak in human pancreatic cancer cells. Cancer Res. 2008, 68: 2944-2951. 10.1158/0008-5472.CAN-07-2508
Chang MC, Chen CA, Hsieh CY, Lee CN, Su YN, Hu YH, Cheng WF: Mesothelin inhibits paclitaxel-induced apoptosis through the PI3K pathway. Biochem J. 2009, 424: 449-458. 10.1042/BJ20082196
Hou LQ, Wang YH, Liu LJ, Guo J, Teng LP, Cao LH, Shi H, Yuan L, De W: Expression and localization of mesothelin in developing rat pancreas. Dev Growth Differ. 2008, 50: 531-541. 10.1111/j.1440-169X.2008.01047.x
Ledda-Columbano GM, Curto M, Piga R, Zedda AI, Menegazzi M, Sartori C, Shinozuka H, Bluethmann H, Poli V, Ciliberto G, Columbano A: In vivo hepatocyte proliferation is inducible through a TNF and IL-6-independent pathway. Oncogene. 1998, 17: 1039-1044. 10.1038/sj.onc.1202018
Acknowledgements
This work was supported in part by Dan L Duncan Cancer Center pilot grant and the National Institutes of Health Grant CA140828 for Q. Yao.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
UB planned and performed most experiments, wrote the manuscript. CMM helped in many of these experiments and helped in making the plasmid preparations as well helped in editing the manuscript. ML and CC participated in discussion. QY participated in discussion and manuscript preparation and provided grant support for this study. All authors read and approved the final version of this manuscript.
Electronic supplementary material
12943_2011_935_MOESM1_ESM.TIFF
Additional file 1: Additional Figure S1: Effect of serum on the resistance to TNF-a mediated cytotoxicity. The MSLN-high BxPC3 and AsPC-1 cells were tested for viability by MTT assay after treatment with 20 ng/ml of TNF-a for 72 h. Data plotted shown mean value from quadruplicate wells. (TIFF 97 KB)
12943_2011_935_MOESM2_ESM.TIFF
Additional file 2: Additional Figure S2: Knocking-down MSLN expression in MIA-MSLN cells by specific siRNA directed against MSLN. Y axis shows the GAPDH-normalized mRNA levels as 2^[Ct(GAPDH)-Ct(MSLN)]. Bars denote s.d. of duplicate data. *, # denote p < 0.05, **, ## denote p < 0.01, compared with controls by using t test. (TIFF 74 KB)
12943_2011_935_MOESM3_ESM.TIFF
Additional file 3: Additional Figure S3: TNFR1 expression levels in MIA-V/MIA-MSLN cells. (A). Real-time PCR analysis of TNFR1 relative mRNA levels. Results denote GAPDH-normalized mRNA levels as 2^[Ct(GAPDH)-Ct(TNFR1)]. The bars denote s.d. of duplicate data. (B). Western blot data showing TNFR1 protein expression in MIA-V/MIA-MSLN cells. (TIFF 88 KB)
12943_2011_935_MOESM4_ESM.TIFF
Additional file 4: Additional Figure S4: Sub-confluent MIA-V/MIA-MSLN cells were serum starved for 24 h and then treated with 10/20 ng/ml of TNF-α for 72 h. Cells were collected and fixed, PI-stained, and analyzed for cell cycle phase distribution (percentage of cells) with FACS. Percentage of cells in G0/G1, S, G2/M phase are shown against the respective peaks in the histograms. (TIFF 65 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Bharadwaj, U., Marin-Muller, C., Li, M. et al. Mesothelin confers pancreatic cancer cell resistance to TNF-α-induced apoptosis through Akt/PI3K/NF-κB activation and IL-6/Mcl-1 overexpression. Mol Cancer 10, 106 (2011). https://doi.org/10.1186/1476-4598-10-106
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-4598-10-106