Abstract
Introduction
PGE-2 is constitutively produced by many non-small cell lung cancers (NSCLC) and its immunosuppressive effects have been linked to altered immune responses in lung cancer. We asked whether elevated levels of plasma PGE-2 correlated with monocyte IL10 production in the NSCLC environment. Looking for correlation in NSCLC patient blood we assayed plasma from NSCLC patients for PGE2 and IL10; we further evaluated production of IL10 by adherent mononuclear cells from a subset of these patients looking for an altered cytokine profile.
Results
Our initial in vitro experiments show that monocyte IL10 induction correlates with tumor cell PGE-2 production, confirming similar reports in the literature. Data show plasma PGE-2 levels in 38 NSCLC patients are elevated compared to normal controls. Plasma IL10 levels were not significantly elevated; however, adherent monocytes derived from NSCLC patient blood did produce significantly more IL10 in 24 hr primary culture than those from normal controls (p < 0.01). The association of elevated plasma PGE-2 and monocyte derived IL-10 was not significant.
Conclusions
Elevated plasma PGE-2 and monocyte IL10 production are associated with NSCLC. The biological significance to elevated PGE-2 levels in NSCLC are unclear. Further investigation of each as a nonspecific marker for NSCLC tumor is warranted.
Similar content being viewed by others
Background
One mechanism by which tumors evade immune destruction is through cytokine production or induction [1]. Prostaglandin E-2 (PGE-2), constitutively produced by many NSCLC has been identified as one factor that has direct immunosuppressive properties and is known to induce IL10 in mononuclear cells [2–7]. IL10 is a dominant immunosuppressive cytokine found in the NSCLC environment known to directly affect T cell-mediated immunity [2–12]. Both PGE-2 and IL10 have been shown to suppress antigen presentation, to suppress cytotoxic T cell (CTL) responses, and to inhibit cytokine production by T cells and antigen presenting cells, perhaps most importantly IL12, that plays a central role in initiation and potentiation of cellular immune responses [2–7], [11–19]. We asked whether PGE-2 levels and/or IL10 levels were elevated in plasma of NSCLC patients, whether monocytes from NSCLC patients produce more IL10 than normals, and whether there was correlation within our findings. As an additional in vitro correlate, we evaluated differences in IL10 production by normal adherent peripheral blood mononuclear cells cultured in conditioned media from cell lines that produce variable amounts of PGE-2.
Results
PGE-2 produced by tumor cell lines correlated with IL10 production by normal donor adherent PBMC
To confirm observations from the literature, supernatants from 6 different NSCLC cell lines producing variable amounts of PGE-2 (ranging from 100 pg/ml/5 × 105 cells to >50,000 pg/ml/5 × 105 cells) were compared directly for their ability to induce IL10 in adherent mononuclear cells. Each cell line induced IL10 in adherent mononuclear cells that was greater than control. This relative increase in IL10 correlated with PGE-2 produced by each cell line (p < 0.05).(Figure 1).
Production of PGE-2 and induction of IL10 by NSCLC tumor cell lines. Supernatants from 6 established cell lines and control cell line 293 (5 × 105/ml) were assayed for PGE-2 over 24 hr by ELISA. Data are presented as mean of triplicate samples and are expressed as pg/ml/5 × 105 cells. Supernatants were transferred to adherent mononuclear cells from healthy volunteers (106/ml) and IL10 was assayed in supernatants at 24 hr. Data are expressed as mean +/- SEM.
PGE-2 levels in plasma of individuals with NSCLC
Two separate assays yielded similar elevations in plasma levels of PGE2 above normals. Each assay used different sets of normals for comparison. Significant differences were seen when comparing measurements from 38 NSCLC samples to 9 normals (234+/-40 vs.519+/-54; p = 0.0167) and 27 NSCLC patient samples to 16 normals (846+/-62 vs. 1838 +/-213; p = 0.0011) (Figure 2). Absolute measures of PGE-2 differed between assays that prevented the pooling of results; relative values may reflect differences in sample handling or assay conditions, or differences in ELISA kits themselves. Plasma IL10 levels measured in 29 patient samples were not significantly elevated above controls (6.6 ± 4.6 vs. 3.9 ± 3.6; p > 0.1; not shown). PGE-2 levels did not correlate with stage or histology (p > 0.1 all comparisons).
Plasma levels of prostaglandin E-2 (PGE-2) in individuals with NSCLC. Two separate assays measuring PGE-2 levels in NSCLC patients and normal controls. One assay measured 38 NSCLC plasma samples and 9 normal controls, the other, 27 NSCLC patient samples compared to a separate set of 16 normals; both assays show similar results. The data are presented as mean ± standard error of the mean.
Cytokine profiles of adherent mononuclear cells from NSCLC patients
Adherent cells, predominantly mononuclear phagocytes, from 13 individuals were evaluated for IL10 production. Data show adherent mononuclear cells from NSCLC patients produced baseline levels of IL10 significantly greater than those of normal volunteers (40 ± 25 vs. 574 ± 127; p < 0.01; Figure 3). IL10 production did not correlate with stage or histology (not shown).
IL10 production by adherent mononuclear cells from individuals with NSCLC and normals. 106 adherent cells/ml from 13 individuals with various stage NSCLC and 8 healthy volunteers were incubated in serum containing culture medium for 24 hr and assayed for IL10 and by ELISA. Data are presented as mean ± standard error of the mean.
Correlation of PGE-2 levels and IL10 production from adherent mononuclear cells
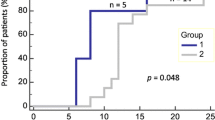
Paired comparisons of plasma PGE-2 levels and mononuclear cell IL10 was possible in 11 patient samples. Paired comparisons in patient sample did not reach statistical significance (p > 0.1), although in a subset of 9 patients, excluding 2 samples with the highest PGE-2 levels, a positive correlation of PGE-2 levels and IL10 production was apparent (p < 0.05; Figure 4). There was no simple explanation for these outliers, nor rationale for excluding these samples. There was a significant correlation between PGE-2 levels and IL10 production in normal samples (p < 0.05), but combining normals and patient data did not strengthen the statistical observations.
PGE-2 levels and IL10 production by adherent peripheral blood mononuclear cells in NSCLC. Shown is a regression analysis of PGE-2 levels and IL10 production by mononuclear phagocytes from 11 individuals with NSCLC. Two separate regression lines indicate significance of the correlation including two outliers (dashed line; p > 0.1) and excluding two outliers (solid line; p < 0.05). Outliers are filled circles inside the box as indicated.
Discussion
COX-2 is an inducible enzyme upregulated in inflammatory states [20, 21]. Notably, many NSCLC and what have been characterized as "premalignant" lung lesions have been shown to constitutively express the COX-2 enzyme and produce prostaglandin E-2 (PGE-2), the primary product of the COX-2 pathway [22–26]. Importantly, PGE-2 production by tumor cells has been linked to tumor-induced immunosuppression in NSCLC [2–5]. PGE-2 has been shown to directly suppress T cell mediated immunity, the primary effector against tumor cells, at a variety of levels [2–7]. Further, PGE-2 has been shown to induce the IL10 in mononuclear cells [4, 5]. IL10 is a prominent immunosuppressive cytokine that may have a dominant role in preventing innate antitumor responses in the NSCLC environment [2–5], [8–19]. Among myriad suppressive effects on T cells and antigen presenting cells, IL10 is known to inhibit IL12 production [14–18]. IL12 plays a key role in the initiation and potentiation of cellular immune responses and alteration of the IL12 producing function in circulating mononuclear phagocytes may be a critical factor in suppressed T cell immunity to NSCLC [27, 28].
We evaluated both PGE-2 and IL10 in plasma of NSCLC patients finding only PGE-2 to be significantly elevated above controls. Elevations were independent of stage of disease or tumor histology. Data also show mononuclear phagocytes from NSCLC patients produce significantly more IL10 over 24 hr in primary culture than controls, consistent with reports of altered cytokine profiles of adherent mononuclear cells from breast cancer patients [29]. Although in vitro experiments suggest there could be a direct link between elevated plasma PGE-2 levels and increased IL10 production by adherent mononuclear cells in NSCLC, the measurements of patient samples do not support a simple causal relationship. The correlation seen in a subset of 9/11 patient samples may reflect only the presence of underlying malignancy, however, it is tempting to speculate on the physiologic relationship between the two.
PGE-2 can be induced by a number of inflammatory conditions, however no single factor, other than cancer, is likely to account for the significant differences seen in this series. Absolute values of PGE-2, that may vary with different assays, are likely less important than the observed differences between NSCLC and normals. The lack of association with disease stage or histology, and the nonspecific production of PGE-2 by multiple cell types, may limit the usefulness of PGE-2 as a specific, independent marker for NSCLC.
Apart from standardized measurement of PGE-2 as a marker for disease, a biologically relevant aspect of elevated PGE-2 would be in the association with altered immune profile of mononuclear phagocytes, specifically IL10 induction. Importantly, serum IL10 levels were established as an independent marker for disease and response to therapy by De Vita et al [10]. The source of the IL10 in that series was thought to be from mononuclear cells. Based on the observations and conclusions of these investigators, and the measurable increases in IL10 production by mononuclear phagocytes derived from NSCLC patients compared to controls, plasma levels of IL10 from these patients might be expected to also be elevated. In the current series, however, there was no difference between patient and control plasma IL10 levels. The reasons for this discrepancy are unclear, and may be related to differences in handling/processing samples or differences in the sensitivity of the ELISAs used in the studies. Further, there was no significant correlation between IL10 production by mononuclear cells and disease stage, as might be inferred from the previously mentioned studies. There was no correlation with histologic type of lung cancer.
Conclusions
Plasma PGE-2 levels may be a nonspecific marker for NSCLC and warrants further investigation. In contrast, plasma IL10 levels did not appear to be sensitive markers in our studies; IL10 production by circulating mononuclear cells, however appears to be associated with disease. The reasons for IL10 production by mononuclear cells in NSCLC are speculative and may be varied. Plasma PGE-2 may contribute but cannot be simply and directly linked.
Methods
Cell lines
Six established NSCLC cell lines (UKY-104, NCI-460, NCI-820, NCI-1155, NCI-1355, and A549) were evaluated. Cell line UKY-104 is an adenocarcinoma established in primary culture from a malignant pleural effusion. Cell lines NCI-460 and NCI-1155 are large cell carcinomas, NCI-820 is a bronchoalveolar type NSCLC, NCI-1355 is an adenocarcinoma, all established at the National Cancer Institute (gift of H. Oie, NCI, National Institutes of Health, Bethesda, MD). A549 is an undifferentiated lung carcinoma and was purchased from American Type Culture Collection (ATCC, Rockville, MD). All cells were maintained in RPMI complete media (10 % fetal bovine serum, 50 units/ml penicillin G and 50 mg/ml streptomycin; Gibco BRL Grand Island, NY). 293, a human embryonic kidney cell line was used as a control.
IL10 production by adherent PBMC from normal donors
Adherent monocytes, derived from whole blood of normal donors were purified from peripheral blood by lysing red blood cells using Red Blood Cell Lysis Solution (Sigma, St Louis, MO) and Ficoll Hypaque density separation technique. Adherent mononuclear cells were separated from granulocytes and nonadherent mononuclear cells (T cells, B cells Natural Killer cells) by 4 hour adherence step. 106 cells/ml were plated in a 24 well culture dish for 24 hr in tumor cell or control cell conditioned media then supernatants were assayed for IL10 by ELISA (R&D).
Human subjects
Following informed consent, peripheral blood was obtained from individuals with histologically confirmed NSCLC. None of the subjects had concomitant illness such as infection and none of the subjects in this series were taking anti-inflammatory medications.
Plasma cytokines in individuals with NSCLC
Plasma was separated from cells by centrifugation and cryopreserved at -80° until use. PGE-2 and IL10 levels were measured in 38 NSCLC patients and compared to that from healthy volunteers by ELISA (R&D, Minneapolis, MN). PGE-2 levels were measured in two separate assays: the first compared 38 NSCLC patient samples to 9 normals; the second compared 27 patient samples to a different set of 16 normals. Stage distribution included 11 stage I or II, 15 stage IIIa/b, and 13 stage IV. Four of 10 stage 4 patients donated blood samples during follow-up appointments in between cycles of chemotherapy. One individual was seen for local recurrence of primary disease (stage IV), all other samples were drawn at the time of initial diagnosis. Histologies included 13 squamous cell, 12 adenocarcinoma, one adeno/squamous cell, and 12 unspecified NSCLC (undifferentiated or poorly differentiated non-small cell carcinoma) because specific cell type was not discernable from available biopsies.
Cytokine profile of adherent PBMC from individuals with NSCLC
In 13 individual samples adequate numbers of peripheral blood mononuclear cells were available for processing (stage I-II n = 3; stage IIIa/b n = 6; stage IV n = 4). Adherent PBMC were purified from peripheral blood as above. 106 adherent mononuclear cells/ml were incubated in a 24 well culture plate in complete RPMI and supernatant was evaluated at 24 hr for basal production of IL10 by ELISA (R&D). Plasma and mononuclear cells were available for evaluation in 11 of 29 patient plasma samples.
PGE-2 production by established cell lines in vitro and generation of tumor cell conditioned media
Tumor cell lines or control cell line 293 were plated in a 24 well culture dish (5 × 105/ml) in complete media × 24 hr. Supernatants were assayed for PGE-2 by ELISA (R&D). Tumor cell conditioned media (CM) was supernatant of cells cultured × 24 hr in RPMI complete media at a density of 5 × 105/ml. All conditioned media was filtered through a 0.22 um filter prior to use.
Statistical analysis
Comparisons among individual patient samples were made using paired t-test and all other comparisons were made by ANOVA.
Abbreviations
- NSCLC:
-
Non-small cell lung cancer
- PGE-2:
-
Prostaglandin E-2
- IL10:
-
Interleukin 10
- CTL:
-
cytotoxic T cell
References
Sulitzeanu D: Immunosuppressive factors in human cancer. Adv Cancer Res. 1993, 60: 247-67.
Stolina M, Sharma S, Lin Y, Dohadwala M, Gardner B, Luo J, Zhu L, Kronenberg M, Miller PW, Portanova J, Lee JC, Dubinett SM: Specific inhibition of cyclooxygenase 2 restores antitumor reactivity by altering the balance of IL-10 and IL-12 synthesis. J Immunol. 2000, 164: 361-70.
Huang M, Wang J, Lee P, Sharma S, Mao JT, Meissner H, Uyemura K, Modlin R, Wollman J, Dubinett SM: Human non-small cell lung cancer cells express a type 2 cytokine pattern. Cancer Res. 1995, 55: 3847-53.
Huang M, Sharma S, Mao JT, Dubinett SM: Non-small cell lung cancer-derived soluble mediators and prostaglandin E2 enhance peripheral blood lymphocyte IL-10 transcription and protein production. J Immunol. 1996, 157: 5512-20.
Huang M, Stolina M, Sharma S, Mao JT, Zhu L, Miller PW, Wollman J, Herschman H, Dubinett SM: Non-small cell lung cancer cyclooxygenase-2-dependent regulation of cytokine balance in lymphocytes and macrophages: up-regulation of interleukin 10 and down-regulation of interleukin 12 production. Cancer Res. 1998, 58: 1208-16.
Snijdewint FG, Kalinski P, Wierenga EA, Bos JD, Kapsenberg ML: Prostaglandin E2 differentially modulates cytokine secretion profiles of human T helper lymphocytes. J Immunol. 1993, 150: 5321-9.
van der Pouw Kraan TC, Boeije LC, Smeenk RJ, Wijdenes J, Aarden LA: Prostaglandin-E2 is a potent inhibitor of human interleukin 12 production. J Exp Med. 1995, 181: 775-9.
Wojciechowska-Lacka A, Matecka-Nowak M, Adamiak E, Lacki JK, Cerkaska-Gluszak B: Serum levels of interleukin-10 and interleukin-6 in patients with lung cancer. Neoplasma. 1996, 43: 155-8.
Yanagawa H, Takeuchi E, Suzuki Y, Ohmoto Y, Bando H, Sone S: Presence and potent immuno-suppressive role of interleukin-10 in malignant pleural effusion due to lung cancer. Cancer Lett. 1999, 136: 27-32. 10.1016/S0304-3835(98)00299-7
De Vita F, Orditura M, Galizia G, Romano C, Roscigno A, Lieto E, Catalano G: Serum interleukin-10 levels as a prognostic factor in advanced non-small cell lung cancer patients. Chest. 2000, 117: 365-73. 10.1378/chest.117.2.365
de Waal Malefyt R, Yssel H, Roncarolo MG, Spits H, de Vries JE: Interleukin-10. Curr Opin Immunol. 1992, 4: 314-20. 10.1016/0952-7915(92)90082-P
Moore KW, O'Garra A, de Waal Malefyt R, Vieira P, Mosmann TR: Interleukin-10. Annu Rev Immunol. 1993, 11: 165-90. 10.1146/annurev.immunol.11.1.165
Beissert S, Hosoi J, Grabbe S, Asahina A, Granstein RD: IL-10 inhibits tumor antigen presentation by epidermal antigen-presenting cells. J Immunol. 1995, 154: 1280-
Fiorentino DF, Zlotnik A, Vieira P, Mosmann TR, Howard M, Moore KW, O'Garra A: IL-10 acts on the antigen-presenting cell to inhibit cytokine production by Th1 cells. J Immunol. 1991, 146: 3444-51.
Fiorentino DF, Zlotnik A, Mosmann TR, Howard M, O'Garra A: IL-10 inhibits cytokine production by activated macrophages. J Immunol. 1991, 147: 3815-22.
Bogdan C, Vodovotz Y, Nathan C: Macrophage deactivation by interleukin 10. J Exp Med. 1991, 174: 1549-55.
Nabioullin R, Sone S, Mizuno K, Yano S, Nishioka Y, Haku T, Ogura T: Interleukin-10 is a potent inhibitor of tumor cytotoxicity by human monocytes and alveolar macrophages. J Leukoc Biol. 1994, 55: 437-42.
D'Andrea A, Aste-Amezaga M, Valiante NM, Ma X, Kubin M, Trinchieri G: Interleukin 10 (IL-10) inhibits human lymphocyte interferon gamma-production by suppressing natural killer cell stimulatory factor/IL-12 synthesis in accessory cells. J Exp Med. 1993, 178: 1041-8.
Sharma S, Stolina M, Lin Y, Gardner B, Miller PW, Kronenberg M, Dubinett SM: T cell-derived IL-10 promotes lung cancer growth by suppressing both T cell and APC function. J Immunol. 1999, 163: 5020-8.
Williams CS, Mann M, DuBois RN: The role of cyclooxygenases in inflammation, cancer, and development. Oncogene. 1999, 18: 7908-16. 10.1038/sj.onc.1203286
Fosslien E: Molecular pathology of cyclooxygenase-2 in neoplasia. Ann Clin Lab Sci. 2000, 30: 3-21.
Hida T, Yatabe Y, Achiwa H, Muramatsu H, Kozaki K, Nakamura S, Ogawa M, Mitsudomi T, Sugiura T, Takahashi T: Increased expression of cyclooxygenase 2 occurs frequently in human lung cancers, specifically in adenocarcinomas. Cancer Res. 1998, 58: 3761-4.
Watkins DN, Lenzo JC, Segal A, Garlepp MJ, Thompson PJ: Expression and localization of cyclo-oxygenase isoforms in non-small cell lung cancer. Eur Respir J. 1999, 14: 412-8. 10.1034/j.1399-3003.1999.14b28.x
Ochiai M, Oguri T, Isobe T, Ishioka S, Yamakido M: Cyclooxygenase-2 (COX-2) mRNA expression levels in normal lung tissues and non-small cell lung cancers. Jpn J Cancer Res. 1999, 90: 1338-43.
Achiwa H, Yatabe Y, Hida T, Kuroishi T, Kozaki K, Nakamura S, Ogawa M, Sugiura T, Mitsudomi T, Takahashi T: Prognostic significance of elevated cyclooxygenase 2 expression in primary, resected lung adenocarcinomas. Clin Cancer Res. 1999, 5: 1001-5.
Hosomi Y, Yokose T, Hirose Y, Nakajima R, Nagai K, Nishiwaki Y, Ochiai A: Increased cyclooxygenase 2 (COX-2) expression occurs frequently in precursor lesions of human adenocarcinoma of the lung. Lung Cancer. 2000, 30: 73-81. 10.1016/S0169-5002(00)00132-X
Gately MK, Wolitzky AG, Quinn PM, Chizzonite R: Regulation of human cytolytic lymphocyte responses by interleukin-12. Cell Immunol. 1992, 143: 127-42.
Trinchieri G, Scott P: Interleukin-12: a proinflammatory cytokine with immunoregulatory functions. Res Immunol. 1995, 146: 423-31. 10.1016/0923-2494(96)83011-2
Merendino RA, Gangemi S, Misefari A, Arena A, Capozza AB, Chillemi S, D'Ambrosio FP: Interleukin-12 and interleukin-10 production by mononuclear phagocytic cells from breast cancer patients. Immunol Lett. 1999, 68: 355-8. 10.1016/S0165-2478(99)00067-X
Acknowledgments
These studies were supported by the Veterans Administration Career Development Award project #596-416905007-0001 and from a generous donation from the McDowell Foundation – Papa Johns/Valvano fund for cancer research. We would also like to thank John Yannelli for his helpful discussion.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
GH performed all experiments; LZ performed data analysis and assisted in writing the manuscript; DD participated with extensive discussion and direction in experimental design; EH directed all studies including gathering all clinical samples. All authors read and approved the final manuscript
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hidalgo, G.E., Zhong, L., Doherty, D.E. et al. Plasma PGE-2 levels and altered cytokine profiles in adherent peripheral blood mononuclear cells in non-small cell lung cancer (NSCLC). Mol Cancer 1, 5 (2002). https://doi.org/10.1186/1476-4598-1-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-4598-1-5