Abstract
Background
Malaria is the leading cause of morbidity and mortality in Ethiopia, accounting for over five million cases and thousands of deaths annually. The risks of morbidity and mortality associated with malaria are characterized by spatial and temporal variation across the country. This study examines the spatial and temporal patterns of malaria transmission at the local level and implements a risk mapping tool to aid in monitoring and disease control activities.
Methods
In this study, we examine the global and local patterns of malaria distribution in 543 villages in East Shoa, central Ethiopia using individual-level morbidity data collected from six laboratory and treatment centers between September 2002 and August 2006.
Results
Statistical analysis of malaria incidence by sex, age, and village through time reveal the presence of significant spatio-temporal variations. Poisson regression analysis shows a decrease in malaria incidence with increasing age. A significant difference in the malaria incidence density ratio (IDRs) is detected in males but not in females. A significant decrease in the malaria IDRs with increasing age is captured by a quadratic model. Local spatial statistics reveals clustering or hot spots within a 5 and 10 km distance of most villages in the study area. In addition, there are temporal variations in malaria incidence.
Conclusion
Malaria incidence varies according to gender and age, with males age 5 and above showing a statistically higher incidence. Significant local clustering of malaria incidence occurs between pairs of villages within 1–10 km distance lags. Malaria incidence was higher in 2002–2003 than in other periods of observation. Malaria hot spots are displayed as risk maps that are useful for monitoring and spatial targeting of prevention and control measures against the disease.
Similar content being viewed by others
Background
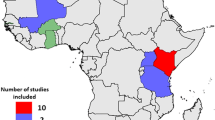
Malaria is a major public health problem in Africa with over 200 million clinical episodes and nearly one million deaths occurring annually [1, 2]. However, the risks of morbidity and mortality associated with malaria, particularly in semi-arid and highland regions, vary spatially and temporally [3–5]. In semi-arid and highland regions of Africa, malaria is unstable and epidemic malaria is a common problem, causing an estimated 12.74 million clinical episodes and 155,000–330,000 deaths annually [4–6]. In Ethiopia, malaria is the leading cause of morbidity and mortality. About 70% of the population (Approximately 52 million people) is estimated to be at risk for malaria infection each year. Health facilities in the country [7] report over five million malaria cases and thousands of deaths across all age groups. Rates of morbidity and mortality dramatically increase (5–6 fold) during epidemic years that recur at irregular intervals of 5–7 years [4, 7, 8]. Transmission usually occurs in about three-quarters of the country, below 2000 m altitude (but sometimes up to 2500 m). However, the levels of malaria risk and transmission intensity exhibit significant spatial and temporal variability related to variations in climate, altitude, topography, and human settlement pattern [9–13]. The spatial and temporal patterns of malaria transmission at the local level (fixed spatial scale) in semi-arid and highland regions in Africa, and particularly in Ethiopia, have not been well investigated or accurately defined. Such research is needed in developing dynamic and area-specific risk maps to identify locations and populations at highest risk for appropriate planning and implementation of targeted and epidemiologically sound preventive and control measures against the disease.
The existing malaria risk maps have limited operational use to support programmatic activities since they were produced at coarse spatial scales, (at continental and country levels). They are largely based on expert opinion [14], on climate based models [15, 16], and specific geo-referenced point prevalence data [17–20]. Other attempts to produce similar risk maps are based on entomological parameters [21, 22] that are not fully validated. In addition, researchers have investigated the spatial pattern of malaria distribution at household and community levels in specific sites in relation to proximity of mosquito breeding habitats [23–28]. Households located within 2–3 km of breeding habitats exhibit higher clustering of malaria cases than others [23]. These studies have focused on entomological parameters and population prevalence surveys, which demand skilled personnel and financial resources that may not be readily available.
In this context, geographical information systems (GIS), remote sensing satellite imagery, geospatial techniques, and spatial statistics provide new methodologies and solutions to analyze the epidemiological and ecological context of malaria and other infectious diseases [29, 30]. Recent advances in local spatial statistics [31–33] have led to a growing interest in the detection of disease clusters or 'hot spots', for public health surveillance and for improving our understanding of the disease etiology and the pathogenesis of epidemics such as malaria. While global spatial autocorrelation statistics such as the global Moran's I [34] describes the overall spatial dependence of malaria over the entire region, local spatial autocorrelation statistics such as the local Moran's I [32] and G and G* [31] are useful in identifying local patterns or hot spots.
The present study aims to examine spatial patterns or clusters of malaria distribution using village level malaria incidence data. It seeks to identify malaria "hotspot" villages and produce "hotspot" maps in different periods of observation. In addition, it describes the temporal incidence of malaria by sex and age. The ultimate objective of the study is to build spatial models of malaria risk for predicting malaria epidemics across a region or state. The findings of this study can guide policy makers and managers at different administrative levels to make evidence-based policy decisions.
Methods
The study area
The study was conducted in East Shoa Zone (7.08°–9.11° N, 38.11°–40.02° E), located in the Rift Valley area of Central Ethiopia (Figure 1 – top right panel). East Shoa Zone covers about 200,000 km2, with elevation ranging from about 902 to 2846 m (mean 1830.4 m) above sea level (Figure 1 – lower panel). Average annual rainfall is 884 mm (range 553–1126 mm), 70% of which occurs from June to September (long rainy season). Average minimum and maximum temperatures are 11.3 and 25.9°c respectively. The area comprises numerous rivers and streams that drain into the Awash River and the lakes located in the Rift Valley. Landuse consists of farmlands interspersed by patches of forests and scattered trees, pastures, shrubs, wetlands and lakes. The economy is largely based on rural subsistence-agriculture. However, a number of irrigated farms and other agro-industrial activities, such as sugarcane, maize and cotton plantations, fruits and vegetables, and horticulture also exist along the Awash River system.
East Shoa is administratively divided into 12 districts and 543 localities known as Kebeles (Figure 1 – lower panel) with an estimated total population of 2.3 million in 2004 [35]. There are 103 health stations and health posts, 14 health centers, 6 specialized malaria laboratory and treatment centers, and 6 hospitals in East Shoa. Malaria transmission in this region, as is in similar regions of the country, is seasonal and unstable, characterized by frequent epidemics with peaks from September to December and from April and June. About 60% of the malaria is due to P. falciparum infections while the remaining 40% is due to P.vivax infections [36].
Data types and sources
Malaria morbidity data
We collected individual-level daily malaria morbidity data from six specialized Malaria Diagnosis and Treatment Centers (MDTC) between September 2002 and August 2006 in East Shoa. Patients self-presenting for ambulatory care are normally diagnosed and given antimalarial treatment service free of charge. Those who are negative for malaria are referred to the nearby health center or hospital for further investigation. Information related to each subject's characteristics and diagnosis outcome is recorded into a Microsoft Access database established in these laboratories. Data collected include patient identification number, date of examination, sex, age, place of residence, travel history, presence or absence of malaria, and malaria parasite species. Subjects who had malaria infections were treated in accordance with the national treatment guidelines. A trained laboratory technician at each laboratory (within the existing system) recorded and entered data for each individual patient into a (Microsoft Access) database on a daily basis, resulting in a complete patient database.
Geographic information system (GIS)
Trained field health workers, using global positioning system (GPS) units, recorded data on geo-reference coordinates (villages, kebeles, health facilities and schools), and altitude for each location. A structured village mapping survey questionnaire was used to record the location information and other relevant environmental and demographic data. Kebele, district and Zonal boundaries and polygon shapes for the entire study area and other geographic features were obtained from the Ethiopian Mapping Authority (EMA) and the WHO/HealthMapper. In addition, the centroid for each village was extracted using ArcGIS 9.2 software to verify data recorded using hand-held GPS units. Digital Elevation Models (DEM) data for the study area were also downloaded from the website http://eros.usgs.gov/products/elevation/gtopo30/e020n40.html and extracted using spatial analyst tools in ArcGIS 9.2. All the relevant shape geographical features were re-projected to WGS_1984_UTM_Zone_37N to integrate the dataset into one geodatabase, a data structure used in ArcGIS.
Data preparation and analysis
Data recording errors related to village names in the malaria database were checked against the records in the geodatabase. All records were given a unique identification code. All individual-level patient data were then cross-linked to villages by unique identification codes to facilitate both the patient level and village level analysis. Data were then aggregated by sex, age and village to describe the characteristics of the distribution of malaria incidence among the study subjects and among the 543 villages. The temporal variation in malaria distribution over the four year study period was also noted by parasite species and month.
Population estimates for the entire East Shoa Zone by village, sex, and age for the years 2002 to 2006 is calculated based on the 1994 national census and the mean annual population growth rate of 2.96% [35]. People living up to 2200 m altitude are considered to be at risk of malaria and nearly all people in East Shoa are treated as an at risk population.
A distinction is often made between prevalence and incidence of a disease. Prevalence is a measure of the total number of cases of disease in a population at a point in time, while incidence rate is the occurrence of new cases of disease (incident number) in a population divided by the person-time over a specified period [37]. Thus, prevalence indicates the magnitude of disease burden whereas incidence conveys information about the risk of contracting malaria. In the present study, the measurement of incidence is complicated by changes in the population at risk, since sometimes the same person may report more than once during a month to the malaria clinic. Each episode of malaria roughly lasts for a week and utmost for one month in the presence of recrudescence. In these circumstances, the definition of incidence is usually restricted to the first event reported in that month. Once a person is classified as a malaria case, he or she is no longer liable to become a new case within the same month. Beyond one month, the person reporting and testing positive at a clinic is considered a new case. Therefore, the incidence density (ID) of malaria was calculated by relating the numbers of new cases to the person years at risk, calculated by adding together the periods during which each individual member of the population is at risk during the measurement period [37]. ID is defined as: Number of new cases/Total person years at risk.
The malaria incidence density per 1000 person-years is calculated from the total number of new cases occurring in each age cohort of females and males divided by the total person-years and then multiplied by 1000. We assumed a Poisson distribution given that the incidence in this study is count data. We used the Generalized linear model [34] (GENMOD) Procedure for Poisson regression analysis in SAS using the log link function to assess the significance of variability in the incidence density ratios (IDRs) by sex and age.
Log [E(y)/person-years] = Intercept + Sex + Age + Age2 + Sex*Age + Sex*Age2
Where E(y) is equal to the expected number of malaria cases. A quadratic model of age raised to the second power best fit the age variable in this dataset.
Spatial statistical analyses
Clustering in malaria incidence was analyzed using both global and local spatial autocorrelation statistics over four specific study periods (2002/2003–2005/2006). The spatial weight matrices were defined at varying distance lags (1 km, 2 km, 3 km, 5 km, 10 km, 15 km, 20 km, and 25 km). Two assumptions guided the choice of the threshold distances: i) the effective flight range of malaria vector mosquitoes; and ii) the estimated travel distance of patients' from home to the laboratories. For this analysis, we selected 353 villages out of a total of 543 villages since they had a consistent dataset over the entire study period, allowing comparison between years.
First, the global Moran's I test statistic [32] was computed to test the null hypothesis (Ho) of no significant clustering of malaria incidence in the entire study region (α = 0.05). The test was repeated using permutations of 100, to validate the consistency of results [34]. Second, we used local Moran's I test statistics [32] to examine the presence or absence of local spatial autocorrelation using the number of malaria cases between pairs of villages at varying distance lags for each of the four specific time periods, 2002/03–2005/06 (September-August). In this context, Local Moran's I statistics is defined as follows:
Where is the average number of malaria cases in villages, x i and x j are the number of malaria cases at village i and j, respectively, and wij is the spatial weight matrix based on the defined distance lags (in km) between village i and village j (where W ij (d) = 1 if the distance between village i and j is within d; otherwise W ij (d) = 0). The mean global and local Moran's I values were plotted as a function of distance lags (km) for each specific time period. In this case, large and positive mean Moran's I values (higher than zero), indicate presence of significant clustering while negative values (less than zero) indicate dissimilar or variable patterns, and values equal to zero indicate presence of a random pattern.
Third, local Gi* statistics [31] were calculated for each village based on the spatial weights using different threshold distances (d) as described above.
Where, w ij is a spatial weight matrix at a given distance lag in kilometers (d) (w ij (d)) is 1 when the distance from village j to i is within d, otherwise w ij (d) is 0). The presence of local clustering of malaria cases in the study villages (hotspot areas) was determined using Z-score values. A high and positive Z score value, >1.96, indicate that the village i is surrounded by relatively high malaria incidence villages, whereas a high but negative Z-score value indicates that the village i is surrounded by relatively low (cold spot) malaria incidence villages. Z-score values ≥ -1.96 and ≤ 1.96 indicates presence of a variable or random distribution. The results for each time period help in visualizing the temporal shifts in the location of hotspots in malaria over the four time periods.
Results
Characteristics of study subjects
A total of 297,046 outpatients were clinically (microscopically) examined for the presence or absence of malaria infections at the six malaria laboratory and treatment centers between September 2002 and August 2006. There were 221 observations (0.05%) with missing values either in the response or explanatory variables that were discarded from the analysis, resulting in a complete dataset of 296,825 patients. The median age of the study subjects was 19 years (range: <1–100 years). The age and sex distribution of the study subjects attending the six malaria laboratory centers are comparable with the last national population census data [35].
Distribution of malaria incidence by village
Table 1 shows the distribution of malaria cases amongst the 497 villages or kebeles out of a total of 543. There are no outpatients coming from the remaining 46 villages. There are wide variations in the distribution and proportion of malaria incidence between kebeles. The mean number of malaria cases is 165 while the mean of the P. falciparum is 99 and P. vivax is 68. However, the median age of malaria patients shows no significant variation across villages and is around 17–19 years.
The distribution of malaria cases by sex and age
Of the total 296,825 tested outpatients, 81,883 (about 28%) had confirmed malaria infections. Malaria was prevalent in about 30% of the total examined males and 25% of the total examined females. Overall, males comprise 61.1% of the total malaria cases. About 60% of the total malaria cases exhibited P. falciparum infections while the remaining 40% exhibited P. vivax infection. Mixed infections of both falciparum and vivax malaria were found in less than 0.1% of the cases. Figure 2 shows the incidence rate of malaria per 1000 person-years (Y-axis) in males and females by age (X-axis). In areas with unstable transmission such as East Shoa, the entire population has no immunity and is at risk for malaria. Hence one would expect the line graphs to be flat since all age groups and both sexes are at a similar risk. But that is not the case as shown in Figure 2. First, the cumulative incidence rates are higher in males than females in all ages (except around 80–88 years) indicating that males are at a higher risk. Second, the line graphs show the presence of a non-uniform relationship between the cumulative malaria incidence rate and age in both sexes, with a peak between 15 and 30 years of age, notably higher for males. These results are further supported by analysis in Table 2.
Poisson regression model results shown in Table 2 indicate the significance of age and sex on cumulative malaria incidence rates. A significant increase in the incidence rate is observed per one-year increase in age (1.07, 95% CI [1.06, 1.07], P =< 0.0001). The malaria incidence rate in females is found to be significantly lower than in males (0.86, 95% CI [0.84, 0.89], P =< 0.0001). The results also indicate a statistically significant interaction between age and sex (0.98, 95% CI [0.978, 0.984], P = 0.0001).
Temporal variation in the distribution of the incidence of malaria cases
Figure 3 presents the temporal variations in the monthly number and relative proportion of malaria cases out of the total over a period of four contiguous years (September 2002–August 2006). The average (standard deviations) number of malaria cases per month is about 1706 (1729 standard deviations). Higher malaria incidence, above normal, is observed from September 2002 to December 2003, with a peak during the month of October. Most of the malaria incidence, 25% of the annual total number of incident malaria cases, is observed in October and a great majority of this is due to P. falciparum infections. However, there is a general decreasing trend, characterized by a similar seasonal pattern, in the number and relative percentage of incident malaria cases beginning in January 2004. The frequency P. falciparum gametocyte carriers are shown to be high during 2002/2003.
Spatial distribution of malaria incidence by village
Figure 4 shows the spatial distribution of the proportion of malaria cases (all malaria types, the two malaria parasite species) over the four-year study period. Panel 1 shows a higher incidence of all malaria in the northern villages as well as some pockets in the south. Panel 2 shows a higher proportion of P. falciparum cases in low altitude areas while Panel 3 shows P. vivax in high altitude areas. Villages with high (above 5%) gametocyte carriers are shown in red and yellow colors in Panel 4. These maps suggest that the spatial pattern in the incidence of malaria could be correlated to critical determining factors, such as elevation, rainfall and landuse
Global and local patterns of the incidence of malaria at village level
Moran's I test statistics for global spatial autocorrelation
First, global spatial statistics are estimated using the Moran's I measure. The test results indicate the presence of significant global spatial autocorrelation for the incidence of malaria (all malaria types, P. falciparum and P. vivax) at 1 km threshold distance lag for all villages. However, these global Moran's I test statistics are not significant at distances greater than 2 km (Figure 5). The test results are similar for both P. falciparum and P. vivax cases (data not shown here). However, these global results suggest that there are strong local patterns in the distribution of malaria that need to be further explored using local spatial statistics.
Local Moran's I test statistics for local spatial autocorrelation of malaria incidence
Local Moran's I statistics are estimated for the incidence of malaria (all types,P. falciparum and P. vivax) for the four specific time periods 2002/03–2005/06 (September-August). Figure 6 shows graphical plots of the overall mean local Moran's I value as a function of distance (in km). Highest mean local Moran's I values are observed at 5 and 10 km distance lags, although the overall mean test results indicate no statistically significant local clustering of malaria incidence at the 0.05 level. However, statistically significant local clustering of malaria incidence is detected in four villages (Basaku Ilala, Meja Karsa, Aga, and Gonde Gurati) out of a total of 353 villages in 2002/03, 2003/04, 2004/05 and 2005/06, respectively, at 5 km distance lags. Similarly, significant local clustering of malaria incidence is detected in the following three villages, namely Mechafera, Faji Sole, and Aleche Hare Bate, in 2002/03, 2003/04, 2004/05 and 2005/06 at 10 km respectively. Similar local clustering patterns are also observed for each of the two parasite species over the four time periods. These local statistics reveal distinct spatial patterns.
To better visualize Local Moran's I values, we performed a spatial interpolation procedure to transform our village (point) data into area based maps using Thiessen polygon interpolation.
Figure 7 shows the spatio-temporal distribution of standardized local Moran's I for malaria incidence over the four time periods. The maps show villages with significant clustering, Moran's I values of greater than 1.96 Z score values, in red. There is more significant local clustering in the 2002–03 and 2005–06 time periods, with clusters in northern and southern villages.
Local G* test statistics results for malaria incidence
Local spatial statistics G* is calculated for each village to detect the presence of significant local clustering of malaria incidence over the four time periods at different threshold distances. Figure 8 shows the frequency distribution of villages against standardized (G*) values, indicating the presence of malaria hotspots at 1–2 km distance lags. However, the number of villages with significant local clustering decreases at 2 km distance lags. No malaria hotspots are detected beyond 2 km distance lags. The local G* test statistics for each parasite species, P. falciparum and P. vivax, display similar results.
Discussion
This study describes the non-spatial and spatial pattern of malaria distribution in areas of seasonal unstable transmission using routinely collected individual-level patient morbidity data from health care facilities. Our findings are presented below.
First, malaria transmission varies due to gender and age. The high incidence rate observed in males as compared with females might be due to different exposure rates or other behavioral risk factors. Males in the age group 15–35 years may be at risk due to greater mobility and work related activity in the fields and risky areas. Females and children tend to stay indoors and travel less, and may use mosquito netting and other precautions against exposure. The presence of interaction between sex and age further highlights the differences in exposure to the risk of infection. It is important to point out that the relative proportion of males and females attending the malaria laboratory centers in the present study are comparable to the national census figure, indicating an absence of differential use of these health care services across groups. Malaria affects all age groups of the population in areas with unstable malaria transmission [4, 38, 39]. However, the observed quadratic relationship between the incidence rate of malaria and age remains to be understood. Hence, further investigation is warranted to determine the underlying differences in exposure or behavioral risk factors to prevent incidence spikes in certain age groups and in men.
There are temporal variations in the incidence of malaria that may be related to variations in climate [12, 13], and other local environmental risk factors [24, 40]. Most malaria occurs during September and December with peaks during the month of October, immediately after the main rainy season. But there are significant inter-annual variations, with elevated incidence in 2002–2004 and reduced incidence in 2005–2006. In 2003, unusually severe and intense malaria epidemics were reported in several other highland areas (1500–2500 m) in four regions in the country [8, 41]. These epidemics have partly been associated with climate abnormalities (lower rainfall and warmer temperature) linked to El Nino events, and partly due to an increase and spread of antimalarial drug resistant-falciparum malaria, and the neglect/breakdown of vector control operations [8, 11–13]. The relative contribution of these risk factors needs to be fully investigated.
Similar severe malaria epidemics, associated with climate abnormalities, have also been reported to occur in several Eastern and Southern African countries [41]. On the other hand, the decreasing trend in malaria incidence after 2003/2004 is perhaps due to unfavorable climatic conditions coupled with a decrease in the proportions of susceptible populations, and the likely impact of control measures intensively implemented soon after 2003/2004. P. falciparum generally predominates P. vivax during the period of increased transmission or epidemic years, while P. vivax dominates during low transmission or non-epidemic years. Such temporal variation in the relative frequency of the two parasite species might be related to a decrease in temperature and the effect of antimalarial drugs used. In addition, high Pfalciparum. gametocyte carriages in the population are observed during these peak periods. Such high carriage rates might be related to delay or ineffective treatment. This factor also plays a significant role in increasing the transmission rates.
None of the global Moran's I test statistic shows significant clustering above 1 km. The global Moran's I test is likely to be biased towards the null hypothesis since small variations in malaria incidence in villages or higher variations at few villages are not effectively captured by an overall global measure of spatial association. A climate-altitude based gradient of malaria transmission is not observed in the entire study region, although altitude in these villages varies form 940 m to 2800 m and climate can be expected to vary in relation to altitude. The lack of a climate-altitude based gradient of malaria transmission suggests that local environmental and socioeconomic factors that operate at smaller spatial scales might be more critical [42–46]. Further investigation is warranted to understand the effect of climatic and topographic factors on malaria incidence in the study region.
Significant local clustering of malaria incidence occurs between pairs of villages within 1–10 km distance lags with high values observed at 5 and 10 km for local Moran's and at 1–2 km for local G* statistics. The local test statistics Moran's I and G* results suggest that there are significant clusters or hotspots of malaria incidence. Local risk factors such as proximity to water bodies, topography, access to health facilities, control measures and others might all be important in explaining the observed local clustering of malaria incidence. Thus, our study suggests that local spatial variations at the village level are more useful and add value in prevention programs. Certain clusters of villages have persistent increases in malaria incidence and thus anti-malarial interventions such as insecticide treated bed nets (ITNs) and indoor residual spraying of houses (IRS) can be targeted to those persistent hot spots, eliminating wasteful spending.
The surveillance data analyzed in this study has obvious limitations related to coverage and completeness, and thus can underestimate the actual malaria incidence rate in the population, especially in some remote locations. Nonetheless, this study illustrates the importance of surveillance data in identifying malaria hotspots, which cannot be accomplished using population surveys.
Findings from this study can be used for designing early warning decision support systems that enable the efficient and timely spatial targeting of preventive and control measures against the disease. The study has practical utility in making timely risk maps that can be used to communicate disease risk easily. This study is part of an ongoing research project undertaken by the authors.
Disclaimer
This manuscript was completed by Asnakew Kebede in partial fulfillment of the Master of Arts degree at the Department of Geography and Environment, Boston University. The opinions of the authors expressed in the manuscript do not reflect the views of the authors' affiliated organizations.
References
WHO/UNICEF: The world malaria report 2005. 2005, Geneva: World Health Organization
Snow RW, Guerra CA, Noor AM, Myint HY, Hay SI: The global distribution of clinical episodes of Plasmodium falciparum malaria. Nature. 2005, 434: 214-217.
Snow Robert, Marsh Kevin: The consequences of reducing transmission of Plasmodium falciparum in Africa. Adv Parasitol. 2002, 52: 235-264.
Kiszewski AE, Tekelehaimanot A: A review of the clinical and epidemiologic burdens of epidemic malaria. Am J Trop Med Hyg. 2004, 71 (Suppl 2): 128-135.
WHO/UNICEF: The Africa Malaria Report 2003. 2003, World Health Organization/UNICEF
Worrall E, Rietveld A, Delacollette C: The burden of malaria epidemics and cost-effectiveness of interventions in epidemic situations in Africa. Am J Trop Med Hyg. 2004, 71 (Suppl 2): 136-40.
Ghebreyesus TA, Derressa Witten KH, Getachew A, Seboxa T: The epidemiology and ecology of health and disease in Ethiopia. Malaria. Edited by: Berehane Y, Haile Mariam D, Kloos H. 2006, 556-576.
Negash K, Kebede A, Medhin A, Argaw D, Babaniyi O, Guintran JO, Delacollette C: Malaria epidemics in the highlands of Ethiopia. East Afr Med J. 2005, 82: 186-192.
Gebremariam N: The ecology of health and disease in Ethiopia. Malaria. Edited by: Kloos H, Zein AZ. 1988, Boulder Westview Press, 136-150.
Tulu NA: The ecology of health and disease in Ethiopia. Malaria. Edited by: Kloos H, Zein AZ. 1993, Boulder Westview Press, 341-352.
Abeku A, van Oortmarssen GJ, Borsboom SJ, Habbema JDF: Spatial and temporal variations of malaria epidemic risk in Ethiopia: factors involved and implications. Acta Tropica. 2003, 8: 331-340.
Abeku TA, de Vlas SJ, Borsboom GJJM, Tadege A, Gebreyesus Y, Gebreyohannes H, Alamirew D, Seifu A, Nagelkerke NJD, Habbema JDF: Effects of meteorological factors on epidemic malaria in Ethiopia: a statistical modeling approach based on theoretical reasoning. Parasitology. 2004, 128: 585-593.
Teklehaimanot HD, Lipsitch M, Teklehaimanot A, Schwartz J: Weather-based prediction of Plasmodium falciparum malaria in epidemic-prone regions of Ethiopia I. Patterns of lagged weather effects reflects biological mechanisms. Malar J. 2004, 3 (1): 41-
Schaller KF, Kuls W: Äthiopien: Eine geographisch-medizinische Landeskunde (Ethiopia: A Geomedical Monograph). 1972, Heidelberg, Springer-Verlag, Berlin
Cox J, Craig M, le Sueur D, Sharp B: Mapping Malaria Risk in the Highlands of Africa. Mapping Malaria Risk in Africa/Highland Malaria Project (MARA/HIMAL) Technical Report, MARA/Durban. 1999, London School of Hygiene and Tropical Medicine, London, 96-
Craig MH, Snow RW, le Sueur D: A climate-based distribution model of malaria transmission in sub-Saharan Africa. Parasitol Today. 1999, 15: 105-
Kleinschmidt I, Bagayoko M, Clarke GPY, Craig M, Le Sueur D: A spatial statistical approach to malaria mapping. Int J Epidemiol. 2000, 29: 355-61.
Omumbo JA, Hay SI, Snow RW, Tatem AJ, Rogers DJ: Modeling malaria risk in East Africa at high-spatial resolution. Trop Med Int Health. 2005, 10: 557-566.
Gemperli A, Vounatsou P, Sogoba N, Smith T: Malaria mapping using transmission models: applications to survey data from Mali. Am J Epidemiol. 2006, 163: 289-297.
Kazembe LN, Kleinschmidt I, Holtz TH, Sharp BL: Spatial analysis and mapping of malaria risk in Malawi using point-referenced prevalence of infection data. Int J Health Geogr. 2006, 5: 41-
Kiszewski AE: A global index representing the stability of malaria transmission. Am J Trop Med Hyg. 2004, 70 (5): 486-498.
Moffett A, Shackelford N, Sarkar S: Malaria in Africa: Vector Species' Niche Models and Relative Risk Maps. PLoS ONE. 2007, 2 (9): e824-
Carter R, Mendis KN, Roberts D: Spatial targeting of interventions against malaria. WHO Bull. 2000, 78 (12): 1401-1411.
Ghebreyesus TA, Haile M, Witten KH, Getachew A, Yohannes AM, Yohannes M, Teklehaimanot HD, Lindsay SW, Byass P: Incidence of malaria among children living near dams in northern Ethiopia: community based incidence survey. BMJ. 1999, 319: 663-666.
Ghebreyesus TA, Haile M, Witten KH, Getachew A, Yohannes M, Lindsay SW, Byass P: Household risk factors for malaria among children in the Ethiopian highlands. Trans R Soc Trop Med Hyg. 2000, 94 (1): 17-21.
Thomas CJ, Lindsay SW: Local-scale variation in malaria infection amongst rural Gambian children estimated by satellite remote sensing. Trans R Soc Trop Med Hyg. 2000, 94 (2): 159-63.
Staedke SG, Nottingham EW, Cox J, Kamya MR, Rosenthal PJ, Dorsey G: Short report: proximity to mosquito breeding sites as a risk factor for clinical malaria episodes in an urban cohort of Ugandan children. Am J Trop Med Hyg. 2003, 69: 244-246.
Ernst KC, Adoka SO, Kowuor DO, Wilson ML, John CC: Malaria hotspot areas in a highland Kenya site are consistent in epidemic and non-epidemic years and are associated with ecological factors. Malar J. 2006, 5: 78-
Tanser FC, Le Sueur D: The application of geographical information systems to important public health problems in Africa. Int J Health Geogr. 2002, 1: 4-
Boulos MN: Towards evidence-based, GIS-driven national spatial health information infrastructure and surveillance services in the United Kingdom. Int J Health Geogr. 2004, 3 (1): 1-
Getis A, Ord JK: The analysis of spatial association by use of distance statistics. Geographical Analysis. 1992, 24 (3): 189-206.
Anselin L: Local indicators of spatial associations-LISA. Geographical Analysis. 1995, 27: 93-115.
Cressie N: Statistics for Spatial Data. revised ed. 1993, Wiley, New York
McCullagh P, Nelder JA: Generalized Linear Models. 1989, Chapman and Hall, London
Central Statistical Authority (CSA): The 1994 population and housing census of Ethiopia. Analytical results at country level. 1998, Office of Population and Housing Census Commission, central Statistical authority, Addis Ababa, 1:
Deressa W, Chibsa S, Olana D: The distribution and magnitude of malaria in Oromia, Ethiopia. Ethiop J Health Dev. 2004, 18 (3): 164-170.
M Rothman KJ, Greenland S, Lash T: Measures of occurrence. Modern Epidemiology. 2008, Philadelphia: Lippincott Williams & Wilkins, 32-50. 3
Fantahun M, Alene GD: Burden of Diseases in Amhara Region, Ethiopia. Ethiop Med J. 2004, 165-172.
Gerritsen AM, Kruger P, Loeff van der MFS, Grobusch MP: Malaria incidence in Limpopo Province, South Africa, 1998–2007. Malar J. 2008, 7: 162-
Kreuels B, Kobbe R, Adjei S, Kreuzberg C, von Reden C, Bäter K, Klug S, Busch W, Adjei O, May J: Spatial variation of malaria incidence in young children from a geographically homogenous area with high endemicty. J Infect Dis. 2008, 197: 85-93.
Checchi F, Cox J, Balkan S, Tamrat A, Priotto G, Alberti KP, Zurovac D, Guthmann JP: Malaria Epidemics and Interventions, Kenya, Burundi, Southern Sudan, and Ethiopia, 1999–2004. Emerging Infectious Diseases. 2006, 12 (10): 1477-1485.
Brooker S, Clarke S, Njagi JK, Polack S, Mugo B, Estambale B, Muchiri E, Magnussen P, Cox J: Spatial clustering of malaria and associated risk factors during an epidemic in a highland area of western Kenya. Trop Med Int Health. 2004, 9 (7): 757-766.
Balls MJ, Bodker R, Thomas CJ, Kisinza W, Msangeni HA, Lindsay SW: Effect of topography on the risk of malaria infection in the Usambara Mountains, Tanzania. Trans R Soc Trop Med Hyg. 2004, 98: 400-408.
Mushinzimana E, Munga S, Minakawa N, Li L, Feng CC, Bian L, Kitron U, Schmidt C, Beck L, Zhou G, Githeko AK, Yan G: Landscape determinants and remote sensing of anopheline mosquito larval habitats in the western Kenya highlands. Malar J. 2006, 5: 13-
Githeko AK, Ayisi JM, Odada PK, Atieli FK, Ndenga BA, Githure JI, Yan G: Topography and malaria transmission heterogeneity in western Kenya highlands: prospects for focal vector control. Malar J. 2006, 5: 107-
Cohen MJ, Ernst KC, Lindblade KA, Vulule JM, John CC, Wilson ML: Topography-derived wetness indices are associated with household-level malaria risk in two communities in the western Kenyan highlands. Malar J. 2008, 7: 40-
Acknowledgements
We would like to thank the field and laboratory health workers in East Shoa Zone for their active involvement and dedication in this project. We would like to express my sincere thanks to Mr Amir Said, Abiy Mekuria and Jim McCann for their active participation and coordination in this project. We are indebted to the Federal Ministry of Health of Ethiopia, Oromia Regional Health Bureau, and the World Health Organization Office of Ethiopia for assistance during the field data collection. We are also grateful to Michael DiBlasi and Arun Ravindran for their technical support in reviewing this manuscript. We would like to thank Professors Cupples L. Adrienne and Surajit Ray for their assistance in reviewing the statistical analysis. We would like to thank three anonymous reviewers for their comments and feedback. This work was funded by a grant from the World Health Organization (RBM/WHO), Geneva, Switzerland and the African Studies Center, Boston University. AK was funded by the Stahelin Fellowship for his M.A. Program.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
The author AK was involved in the conceptualization, research design, data collection, implementation and manuscript writing. SG contributed in the design and analysis and manuscript writing. AT and DO were involved in the conceptualizing, research design, field data collection and contributed in reviewing the manuscript. HP contributed in data analysis and preparation of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Yeshiwondim, A.K., Gopal, S., Hailemariam, A.T. et al. Spatial analysis of malaria incidence at the village level in areas with unstable transmission in Ethiopia. Int J Health Geogr 8, 5 (2009). https://doi.org/10.1186/1476-072X-8-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-072X-8-5