Abstract
Background
Aim of the study was to determine the clinical efficacy of a new antiseptic liquid soap (Stellisept® scrub), based on the combination of undecylenamidopropyltrimonium methosulphate (4%) and phenoxyethanol (2%), for eradication of MRSA among colonized patients who do not receive antibiotic therapy.
Methods
Over two years 50 MRSA patients in 6 hospitals were observed. Treatment was defined as the daily application of Stellisept scrub for the antiseptic body and hair wash (at least 60 s) in combination with nasal mupirocin. A treatment cycle was a minimum of 5 days treatment. Screening was carried out at least 48 h after the treatment cycle was finished, with 24 h between each of the requested three or more samplings, which included the nasopharynx, groin, axilla, perineum and other MRSA-positive skin areas.
Results
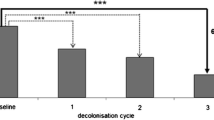
Fifteen cases were retrospectively excluded (lack of outcome documentation, concomitant antibiotic therapy, open wounds). All 35 patients had colonization with MRSA before antiseptic treatment on the skin, in the groin (80%), the axilla (25.7%), the perineum (20%) or other skin areas (14.3%). Colonization at more than one skin sites was found in 34.3%. Nasal colonization was found in 21 of 28 patients (75%), 7 patients were without nasal screening prior to the antiseptic treatment. After one treatment cycle MRSA was eradicated in 25 patients (71.4%), after a second cycle the total eradication rate was 91.4%, after a third cycle the rate increased to 94.2%. No patient discontinued the antiseptic treatment due to dermal intolerance of the product.
Conclusions
Progressive eradication of MRSA carriage was observed with the antiseptic soap and mupirocin. The eradication rate was not biased by concomitant antibiotic treatment, screening during treatment or lack of evidence for colonization in contrast to other studies with other preparations.
Similar content being viewed by others
Introduction
Methicillin-resistant Staphylococcus aureus (MRSA) continues to be a global problem in infection control. For many years it has been a major cause for nosocomial infections in many countries [1, 2]. The proportion of methicillin resistance among clinical isolates of S. aureus is still increasing. In southern European countries, the proportion may be as high as 55% [3, 4]. MRSA now even becomes an increasing problem in the community [5, 6]. Transmission of MRSA in community has been shown to be as high as 60% [7]. Family members who are living with MRSA carriers are in danger of MRSA transmission [7]. Dermal colonization with MRSA may be persistent, especially in the groin [8]. That is why attempts are often undertaken to treat colonized MRSA patients [9]. Antibiotics were shown to be effective in uncontrolled and controlled trials with eradication rates between 53% and 85% [10–12]. But antibiotics are considered to be inappropriate for patients who are only colonized and not infected with MRSA [13]. One reason is their potential to cause adverse effects, especially allergy, which can not be justified for patients who do not have an infection. More important is the risk of emergence of vancomycin-resistance in S. aureus [14]. Topical antiseptic measures, however, are normally employed [15]. The nasal cavity is usually treated with mupirocin or with tolerable antiseptics [16]. Dermal colonization is eradicated with antiseptic liquid soaps [13] Only few studies have addressed the question of MRSA eradication among colonized patients with liquid soaps in combination with nasal treatment. All of them are uncontrolled trials and most of them have different types of biases.
Aim of our study was to determine the efficacy of the antiseptic soap Stellisept scrub in combination with mupirocin for eradication of MRSA among colonized patients with evidence of dermal colonization (no selection bias), without concomitant antibiotic therapy (no treatment bias) and with regular screening investigations (no outcome bias).
Methods
Study design
An open clinical trial was chosen as a study design.
Determination of MRSA carriage
The MRSA carrier status was determined before and after treatment of the patients. Swabs were taken at least from the following body sites: nasopharynx, axilla, groin and perineum. Any patient with at least one MRSA positive skin site was regarded as a patient with evidence for dermal colonization irrespective of the nasal colonization status.
All swabs were processed on the same day. Briefly, swabs were plated directly on blood agar, oxacillin resistance screening agar base (Oxoid, UK), and dextrose broth for enrichment. After incubation of plates and broth at 37°C for 18 to 24 h, colonies resembling S. aureus were identified and tested for oxacillin resistance. This was done in two steps: disk diffusion with a 5 μg oxacillin disk on Mueller-Hinton agar (incubation at 30°C for 18 – 24 h) and agar screening on Mueller-Hinton agar supplemented with 6 mg/ml oxacillin and 4% saline (Oxa Screen Test Agar, bioMérieux, France; incubation at 35°C for 24 h). Isolates growing within 14 mm around the oxacillin disk and growing on the MRSA screening plates were regarded as oxacillin resistant.
Treatment of patients
Definition of treatment and treatment cycle: Treatment was defined as the daily application of Stellisept scrub for the antiseptic body and hair wash (at least 60 s) in combination with nasal mupirocin. A treatment cycle was defined as a minimum of 5 days treatment.
Treatment of the nasal cavity
The nasal cavity was treated with mupirocin which was applied twice per day as recommended by the manufacturer (Turixin®, GlaxoSmithKline, Munich, Germany).
Treatment of the skin
The skin and hair was treated once a day with the antiseptic liquid soap (Stellisept scrub, Bode Chemie GmbH & Co., Hamburg, Germany) which is based on two active ingredients: 4% (w/w) undecylenamidopropyltrimonium methosulphate and 2% (w/w) phenoxyethanol. The minimum duration of antiseptic skin treatment was 60 s. This application time is derived from in vitro data on the activity of the product against various epidemic MRSA strains and various clinical MRSA isolates [17].
For body washing the skin was moistened with tap water and the liquid soap applied without dilution. Mobile patients washed themselves under supervision of a healthcare worker. Immobile patients were washed by healthcare workers. After the 60 s application residual soap had to be rinsed or washed off with tap water. Linen and clothes were changed during the antiseptic treatment and the surrounding surfaces treated with a surface disinfectant [13].
Patient selection and data
Six hospitals participated in the study. The local infection control nurse of a hospital was responsible for data collection. Patients were included
-
if there was evidence for dermal colonization with MRSA irrespective of the colonized body site (minimum screening of axilla, groin and perineum) and
-
if they did not receive antibiotics at the beginning of the treatment and
-
if they had no signs of a clinical infection and
-
if compliance with the treatment could be expected for the anticipated duration of hospital stay.
Patients were excluded
-
if antibiotics were given during the treatment or during the surveillance culture interval or
-
antiseptic treatment was initiated for treatment of colonized or infected wounds and
-
if patients were discharged before screening cultures could be obtained after treatment.
The following data were collected for each patient: gender, hospital, MRSA positive body sites before and after the antiseptic treatment (nasopharynx, axilla, groin, perineum, other body sites) and additional information if relevant for the outcome assessment. The microbiological method in each hospital for identification of MRSA from initial and follow-up swabs was not evaluated for its sensitivity and specificity since it has become routine in German laboratories.
Post treatment screening
Post treatment screening was done according to the German recommendation on MRSA patients issued by the Robert-Koch Institut [13]. A minimum wash-out period of 48 h was required between the last treatment and the first set of screening swabs. Screening swabs had to be taken for three consecutive days and at least from the following sampling sites: nasopharynx, axilla, groin and perineum. Additional body sites were included if they were found to be MRSA positive before antiseptic treatment.
Results
Fifty patients were treated between 2001 and 2002 in the 6 hospitals, mainly in surgery, internal medicine, intensive care or other departments such as gynecology (n = 2), neurology (n = 2), urology (n = 1) or dermatology (n = 1; Table 1). Four of the 50 patients were discharged early resulting in a lack of information on the outcome (colonization with MRSA after antiseptic treatment). Eight patients received concomitant systemic antibiotic therapy initiated after inclusion in the study. Three patients had a colonized or infected wound which was treated during the study. All of them were excluded resulting in a total of 35 cases with proven dermal MRSA colonization and without concomitant systemic antibiotic therapy.
21 of the 35 patients were male (60%), the mean age was 69.1 years (minimum 27 years, maximum 91 years). Nasal colonization was found in 21 of 28 patients (75%), 7 patients were without nasal screening prior to the antiseptic treatment. Dermal colonization was documented mainly in the groin (80%), followed by axilla (25.7%), perineum (20%), forehead (5.7%), umbilicus (5.7%) and upper leg (2.9%; Table 2). Multiple colonization of the skin was found in 34.3% of the patients.
After one cycle of antiseptic body wash and concomitant nasal antisepsis with mupirocin, 25 of the 35 patients were found to be MRSA free (71.4%; Table 2). The mean duration of treatment was 6.7 ± 2.5 days. Successful eradication of MRSA was confirmed with three negative consecutive series of swabs in 16 patients (64%). Two consecutive series of swabs were negative in five patients (20%) and one series of swabs was negative in four patients (16%) which was explained by early discharge of the patient. Treatment failures after the first cycle were due to persistent colonization of the same skin area (5 of 10), colonization of another skin area (4 of 10) and persistent colonization of the nasopharynx (1 of 10). Of the remaining 10 patients, two were not treated any further due to discharge and 8 underwent a second treatment cycle with seven of them being MRSA negative afterwards (total of 91.4% being MRSA negative). The mean duration of treatment in the second cycle was 6.4 ± 2.1 days. In order to confirm successful eradication of MRSA after the second cycle, three consecutive series of swabs were negative in six patients (85.7%) and two consecutive series of swabs were negative in one patient (14.3%). The one patient remained colonized on the same skin area without nasal carriage and underwent a third treatment cycle resulting in dermal MRSA eradication (total of 94.2% being MRSA negative; Table 2). Three series of consecutive swabs were negative to confirm successful eradication of MRSA.
No patient had to discontinue the antiseptic body wash due to dermal intolerance or uncomfortable perception of the product.
Discussion
Although eradication of MRSA from colonized patients is regarded as a key element in prevention of transmission in a hospital, so far only few studies have addressed the clinical efficacy of antiseptic soaps in combination with a nasal antiseptic for that purpose. No study was found with a positive or negative control for the antiseptic skin treatment, only one study was found with a negative control for nasal mupirocin (Table 3). In addition, most of the uncontrolled trials contain substantial biases which limit or even diminish the value of them.
In our study, we found an eradication rate after one treatment cycle of 71.4% which is comparable to antibiotic treatment [10, 18]. After two treatment cycles, the rate was 91.4% and came up to 94.2% after a third treatment cycle. With no other antiseptic soap we were able to find comparable data which are not confounded by a lack of evidence for initial MRSA colonization, concomitant antibiotic therapy or screening cultures during antiseptic treatment.
One limitation of our study is the lack of a control. We can not exclude that washing with plain soap and water or doing nothing would not have had a similar effect regarding the eradication of MRSA, although it is very unlikely based the persistence of MRSA colonization in the groin [8]. It would have been much more interesting to compare Stellisept scrub with either a non-medicated soap (negative control) or another antiseptic soap (e.g. based on chlorhexidine). But the use of non-medicated liquid soap would have been acting against the German recommendation for MRSA patients (antiseptic soaps or liquid preparations should be used for treatment of the skin) [13]. The use of medicated soap, however, would have been an interesting option, ideally in a double-blind randomized design. But chlorhexidine as the most common active agent for this type of treatment has been described in recent studies with artificial contamination of fingers with MRSA to have no advantage compared with non-medicated liquid soap [19, 20]. It was therefore not considered to be suitable as a positive control [21]. That is why an open uncontrolled design was chosen.
Another limitation is the rather short follow-up of 5 days after termination of the treatment (2 days wash-out and 3 days screening cultures). Most patients stayed as long in their hospital as it was necessary to complete the screening cultures. The main reason for even shorter follow-up is discharge of the patient from a hospital. Continuation of hospital stay with the only aim to complete screening cultures was not possible in our study. Follow-up was unknown in some studies [22, 23], shorter in others [24] or longer [10, 18], but in some studies not for all patients [8, 25].
Treatment failures after the first cycle were mainly observed at the same or another skin site. The surrounding may also contribute to re-colonization of a patient. It was shown in one of our cases to originate from an electric shaver which was not disinfected at all. MRSA may survive on inanimate surfaces and cotton for more than 90 days [26]. Even making the bed leads to a large increase of MRSA in the air for 15 minutes [27]. Careful disinfection of these possible sources and changing linen after the antiseptic treatment is therefore crucial to ensure prevention of re-colonization as recommended in the German guideline on MRSA patients [13].
Identification of MRSA was not carried out for all screening swabs in one laboratory but with the same test method. Differences in the sensitivity and specificity have been described [28–30] which may have an impact on the identification of a MRSA patient. But it is unlikely to have an impact on the result of the antiseptic treatment because the method would have been the same before and after treatment of the same patient. That is why it was justified not to carry out the identification of MRSA in one specific laboratory especially because recent data indicate that determination of phenotypic resistance may largely underestimate the genotypic resistance in MRSA [31].
Another finding is the good dermal tolerance of the antiseptic soap. All 35 patients tolerated repetitive use of the preparation very well, even more than one treatment cycle. Another preparation (Octenisept) has been described to lead to skin redness in 4 of 28 patients resulting in termination of the treatment [25]. The excellent dermal tolerance of Stellisept scrub on intact and scarified skin has been described before [32].
Conclusions
Stellisept scrub in combination with nasal mupirocin was found to effectively and progressively eradicate MRSA from colonized patients. Antiseptic treatment may have to be repeated.
References
Gastmeier P, Sohr D, Geffers C, Nassauer A, Dettenkofer M, Rüden H: Occurence of methicillin-resistant Staphylococcus aureus infections in German intensive care units. Infection. 2002, 30: 198-202. 10.1007/s15010-002-2043-z
Simor AE, Ofner-Agostini M, Bryce E, McGeer A, Paton S, Mulvey MR: Laboratory characterization of methicillin-resistant Staphylococcus aureus in Canadian hospitals: results of 5 years of national surveillance, 1995-1999. The Journal of Infectious Diseases. 2002, 186: 652-660. 10.1086/342292
Voss A, Milatovic D, Wallrauch-Schwarz C, Rosdahl VT, Braveny I: Methicillin-resistant Staphylococcus aureus in Europe. Euro J Clin Microbiol Infect Dis. 1994, 13: 50-55.
Schmitz F-J, Verhoef J, Fluit AC: Prevalence of resistance to MLS antibiotics in 20 European university hospitals participating in the European SENTRY surveillance programme. Journal of Antimicrobial Chemotherapy. 1999, 43: 783-792. 10.1093/jac/43.6.783
Fergie JE, Purcell K: Community-acquired methicillin-resistant Staphylococcus aureus infections in south Texas children. Pediat Infect Dis J. 2001, 20: 860-863. 10.1097/00006454-200109000-00007.
Chambers HF: The changing epidemiology of Staphylococcus aureus?. Emerging Infectious Diseases. 2001, 7: 178-182.
Matsumoto K, Hohashi N, Sugishita C: A study on the transmission of MRSA among the family members including clients of visiting nurse and related infection control. Nippon Koshu Eisei Zasshi. 2001, 48: 190-199.
Harbarth S, Dharan S, Liassine N, Herrault P, Auckenthaler R, Pittet D: Randomized, placebo-controlled, double-blind trial to evaluate the efficacy of mupirocin for eradicating carriage of methicillin-resistant Staphylococcus aureus. Antimicrobial Agents and Chemotherapy. 1999, 43: 1412-1416.
Boyce JM: MRSA patients: proven methods to treat colonization and infection. Journal of Hospital Infection. 2001, 48: S9-S14. 10.1016/S0195-6701(01)90005-2
Asensio A, Guerrero A, Quereda C, Lizán M, Martinez-Ferrer M: Colonization and infection with methicillin-resistant Staphylococcus aureus: Associated factors and eradication. Infection Control and Hospital Epidemiology. 1996, 17: 20-28.
Walsh TJ, Standiford HC, Reboli AC, John JF, Mulligan ME, Ribner BS, Montgomerie JZ, Goetz MB, Mayhall CG, Rimland D, Stevens DA, Hansen SL, Gerard GC, Ragual RJ: Randomized double-blind trial of rifampin with either novobiocin or trimethoprim-sulphamethoxazole against methicillin-resistant Staphylococcus aureus colonization: prevention of antimicrobial resistance and effect of host factors on outcome. Antimicrobial Agents and Chemotherapy. 1993, 37: 1334-1342.
Roccaforte JS, Bittner MJ, Stumpf CA, Preheim LC: Attempts to eradicate methicillin-resistant Staphylococcus aureus colonization with the use of trimethoprim-sulfamethoxazole, rifampin, and bacitracin. American Journal of Infection Control. 1988, 16: 141-146.
Anonym: Empfehlung zur Prävention und Kontrolle von Methicillin-resistenten Staphylococcus aureus-Stämmen (MRSA) in Krankenhäusern und anderen medizinischen Einrichtungen. Bundesgesundheitsblatt. 1999, 42: 954-958.
Bartley J: First case of VRSA identified in Michigan. Infection Control and Hospital Epidemiology. 2002, 23: 480-
Wendt C, Martiny H: Die Sanierung von MRSA-Patienten - Stand des Wissens. Hygiene + Medizin. 2000, 25: 355-360.
Working party report: Revised guidelines for the control of epidemic methicillin-resistant Staphylococcus aureus. Journal of Hospital Infection. 1990, 16: 351-377. 10.1016/0195-6701(90)90008-C
Zschaler R, Nothhelfer B, Werner H-P, Heeg P: Wirksamkeit von Stellisept scrub gegenüber Methicillin-resistenten Staphylococcus aureus-Stämmen in vitro. Krankenhaushygiene und Infektionsverhütung. 2001, 23: 139-141.
Mahara B, van Halteren J, Verzijl JM, Wintermans RG, Buiting AG: Decolonization of methicillin-resistant Staphylococcus aureus using oral vancomycin and topical mupirocin. Clinical Microbiology and Infection. 2002, 8: 671-675. 10.1046/j.1469-0691.2002.00404.x
Huang Y, Oie S, Kamiya A: Comparative effectiveness of hand-cleansing agents for removing methicillin-resistant Staphylococcus aureus from experimentally contaminated fingertips. American Journal of Infection Control. 1994, 22: 224-227.
Guilhermetti M, Hernandes SE, Fukushigue Y, Garcia LB, Cardoso CL: Effectiveness of hand-cleansing agents for removing methicillin-resistant Staphylococcus aureus from contaminated hands. Infection Control and Hospital Epidemiology. 2001, 22: 105-108.
Kampf G: The value of using 4% chlorhexidine soap as a control in a trial on eradication of MRSA among colonized patients. Journal of Hospital Infection. 2004 in press
Kotilainen P, Routama M, Peltonen R, Evesti P, Eerola E, Salmenlinna S, Vuopio-Varkila J, Rossi T: Eradication of methicillin-resistant Staphylococcus aureus from a health care center ward and associated nursing home. Archives of Internal Medicine. 2001, 161: 859-863. 10.1001/archinte.161.6.859
Rengelshausen J, Nürnberger J, Philipp T, Kribben A: Decolonization of methicillin-resistant Staphylococcus aureus by disinfection of the skin. The American Journal of Medicine. 2000, 108: 685-686. 10.1016/S0002-9343(00)00404-6
Zastrow K-D, Kramer A, Bauch B: Konzept zur Dekontamination von MRSA-Patienten. Hygiene + Medizin. 2001, 26: 344-348.
Sloot N, Siebert J, Höffler U: Eradication of MRSA from carriers by means of whole-body washing with an antiseptic in combination with mupirocin nasal ointment. Zentralblatt für Hygiene und Umweltmedizin. 1999, 202: 513-523.
Neely AN, Maley MP: Survival of enterococci and staphylococci on hospital fabric and plastic. Journal of Clinical Microbiology. 2000, 38: 724-726.
Shiomori T, Miyamoto H, Makishima K, Yoshida M, Fujiyoshi T, Udaka T, Inaba T, Hiraki N: Evaluation of bedmaking-related airborne and surface methicillin-resistant Staphylococcus aureus contamination. Journal of Hospital Infection. 2002, 50: 30-35. 10.1053/jhin.2001.1136
Kampf G, Lecke C, Cimbal A-K, Weist K, Rüden H: Evaluation of mannitol salt agar for detection of oxacillin resistance in Staphylococcus aureus by disk diffusion and agar screen. Journal of Clinical Microbiology. 1998, 36: 2254-2257.
Kampf G, Lecke C, Cimbal AK, Weist K, Rüden H: Evaluation of the BBL Crystal MRSA ID system for detection of oxacillin resistance in Staphylococcus aureus. J Clin Pathol. 1998, 52: 225-227.
Kampf G, Weist K, Kegel M, Swidsinski S, Rüden H: Comparison of screening methods to identify methicillin-resistant Staphylococcus aureus. Eur J Clin Microbiol Infect Dis. 1997, 16: 301-307.
Kampf G, Adena S, Rüden H, Weist K: Inducibility and potential role of MecA-gene-positive oxacillin-susceptible Staphylococcus aureus from colonized healthcare workers as a source for nosocomial infections. Journal of Hospital Infection. 2003, 54: 124-129. 10.1016/S0195-6701(03)00119-1
Kampf G, Bielfeldt S, Pfannenbecker U, Rudolf M: Dermal and mucosal tolerance of a new antiseptic liquid soap. Occupational and Environmental Dermatology. 2001, 49: 198-201.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
GK designed the study, organized the participating hospitals, collected the data and analyzed them. AK participated in the design of the study and in the analysis of data. Both authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kampf, G., Kramer, A. Eradication of methicillin-resistant Staphylococcus aureus with an antiseptic soap and nasal mupirocin among colonized patients – an open uncontrolled clinical trial. Ann Clin Microbiol Antimicrob 3, 9 (2004). https://doi.org/10.1186/1476-0711-3-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-0711-3-9