Abstract
Background
Cefoperazone has not been reported to cause vasculitic complications before. Here, we report a case of hypersensitivity vasculitis associated with cefoperazone/sulbactam.
Case presentation
A 13-year-old girl with appendicitis developed hypersensitivity vasculitis on the fifth day of cefoperazone/sulbactam therapy. Hypersensitivity vasculitis resolved gradually after removal of the agent on the seventh day and did not recur. Although hypersensitivity vasculitis has multiple causes, coexistence of hypersensitivity vasculitis and cefoperazone treatment, and the quite resolution of the disease after removal of the drug, strongly favours a causative relationship.
Conclusion
To our knowledge, this is the first report of a hypersensitivity vasculitis associated with cefoperazone.
Similar content being viewed by others
Background
Cefoperazone is a common antibiotic drug used mainly to treat serious infections. Reported adverse effects of this drug include urticaria, maculopapular and erythematous skin rash and rarely anaphylaxis and bronchospasm [1, 2]. Cefoperazone has not been reported to cause vasculitic complications before. We report a case of hypersensitivity vasculitis associated with cefoperazone/sulbactam.
Case Presentation
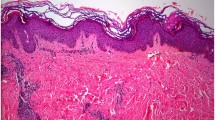
A 13-year-old girl was admitted to Ondokuz May1s University Hospital with a 3-day history of abdominal pain and fever. She had no history of allergic reactions, connective tissue disease, respiratory tract infection and/or use of antibiotics or another drug. Physical examination revealed abdominal tenderness and defense, and positive Rovsing's sign in the right lower quadrant. The white-cell count was 20.700 per cubic milimeter with 78 percent neutrophils, 20 percent lymphocytes and 2 percent monocytes. Hemoglobin was 12.1 g/dl. Erythrocyte sedimentation rate (ESR) was slightly elevated at 46 mm/hour. The patient was referred to the pediatric surgery department and acute perforated appendicitis was considered. Cefoperazone/sulbactam 100 mg/kg/day two in divided doses was initiated on the first day of admission. Abdominal exploration was performed on the second day of admission and a gangrenous appendicitis with adhesions to peripheral tissue and purulent material around the caecum was observed. Biopsy specimen revealed necrosis of mucosa, excessively lymphocyte, neutrophil, plasma cell infiltration in the layers of appendix, and gangrenous appendicitis. No vasculitic changes were observed. E. coli was detected in the peritoneal fluid culture. On the fifth day of admission, an erythematous maculopapular rash without edema developed symmetrically along the legs and feet. By the 7th day the rash gradually spread to buttocks and changed to slightly elevated palpable purpuric lesions 3 to 8 mm in diameter, all at the same stage and which did not blanch on pressure. On the 7th day of admission, assuming the antimicrobial agent was the causative agent, cefoperazone/sulbactam regimen was changed to ampicillin (200 mg/kg/day in four divided doses) plus netilmycin (5 mg/kg/day in three divided doses) and an antihistaminic (clemastine, 2 × 1 mg/per day) was initiated. The patient was afebril after the 6th day of admission. The patient had no vomiting, melena, abdominal pain, arthritis or arthralgia. Antinuclear antibody (ANA), anti-deoxyribonucleic acid (anti-DNA) and rheumatoid factor were negative. Serum complements (C3, C4), prothrombin time, partial thromboplastin time, urinalysis, platelet and white blood cell counts were normal. Kidney and liver function tests were within normal limits. A skin biopsy of a new purpuric lesion from the anterior of the leg was done on the second day of the rash and was revealed a cutaneous vasculitis characterized by perivascular mononuclear cell infiltration. Direct immunfluorescence revealed IgA, IgG and fibrin deposits on the vessel walls. The cutaneous lesions faded within a few days and disappeared on seventh day after discontinuation of cefoperazone/sulbactam therapy. Ampicillin and netilmycin as well as antihistaminic agent were administered for ten days. The patient was discharged on the 18th day of hospitalization. On periodic controls, she is quite well and purpura no recurred.
Hypersensitivity vasculitis presents usually as drug or infection induced purpura and involves dominantly the small vessels. The disease has been reported to be triggered by many factors including bacterial infections, drugs, immun complexes, blood stasis and systemic disease [3]. The criteria of the classification of hypersensitivity vasculitis are age at disease onset >16 years, medication at disease onset, palpable purpura, maculopapular rash and biopsy showing granulocytes in a perivascular or extravascular location. The presence of any 3 or more criteria has been shown to have a sensitivity of 71% and a specificity of 84% [4]. Our patient meets three of five criteria (medication at disease onset, palpable purpura and maculopapular rash) for hypersensitivity vasculitis.
In hypersensitivity vasculitis, the pathogenic mechanism responsible for the blood vessel injury seems to be a type III immun complex reaction or a type IV cell mediated reaction. When the triggering antigen is drug, the term "hypersensitivity" seems apt [5]. The vascular damage is believed to be triggered by the deposition of immun complexes in vessel walls, with activation of complement cascade. Polymorphonuclear leukocytes then migrate to the area and release lysosomal enzymes that damage blood vessels, leading to extravasation of erythrocytes, fibrin deposition, and necrosis. Because leukocytoclastic inflammation is such a prominent feature, these lesions are referred to as "leukocytoclastic vasculitis". Hypersensitivity vasculitis can be divided into neutrophilic and lymhocytic subtypes. The former is frequently associated with hypocomplementemia, whereas the latter is not [6]. Our patient was of lymhocytic type and complement level was normal. In the literature, it is reported that lymphocytic infiltration might represent the resolving phase of an immun complex-mediated neutrophilic vasculitis in lesions more than 48 hours old [7]. On the other hand, there was no relationship between appendicitis and vasculitis. Although IF characteristically shows IgA deposits within vessel walls in HSP while, in most other types of leukocytoclastic vasculitis, IgG or IgM deposits are seen [8]. In our patient, lymphocytic infiltration may be due to delayed biopsy in resolving phase and IgA and IgG deposits do not exclude a leukocytoclastic vasculitis.
Drugs are implicated in up to 10–30% of cases of hypersensitivity vasculitis. Penicillins and sulfonamids are most frequently associated with such a reaction, but many other agents have been implicated as well [3, 9]. The other more common agents are antihypertensives, antiarrythmics, allopurinol, cimetidine, furosemid, hydantoins, penicillins, phenylbutazone, hydralazine and sulfonamides [10].
Since its introduction in 1985, the third generation cephalosporin antibiotic cefoperazone has gained widespread use, and much information has accumulated about its possible adverse effects. Hypersensitivity reactions are the most common side effects. Urticaria, maculopapular and erythematous rash are more common reactions than other immediate reactions such as anaphylaxis and bronchospasm [1, 2, 11, 12]. Although some anecdotal cases of vasculitis have been reported related with cephotaxim, cefuroxim and cefprozil, cefoperazone has not been reported to cause vasculitic complications before [13–15].
Conclusion
In the case presented here, occurence of the typical skin lesions after five days of intake of cefoperazone, in addition to resolution of lesions on discontinuation of cefoperazone are strong evidence in support of a role of cefoperazone in the development of vasculitis. To our knowledge, this is the first reported case of hypersensitivity vasculitis associated with cefoperazone. We believe that cefoperazone may be considered among the possible drugs causing hypersensitivity vasculitis.
References
Cohen MS, Washton HE, Barranco SF: Multicentre clinical trial of cefoperazone sodium in the United States. Am J Med. 1985, 79 (suppl 1B): S35-S41.
Meyers BR: Comparative toxicities of third-generation cephalosporins. American Journal of Medicine. 1985, 79 (suppl 2A): S96-S103.
Blaiss MS, deShazo RD: Drug allergy. Pediatr Clin North Am. 1988, 35: 1131-1147.
Calabrese LH, Michel BA, Bloch DA, Arend WP, Edworthy SM, Fauci AS, Fries JF, Hunder GG, Leavitt RY, Lie JT: The American College of Rheumatology, 1990 criteia for the classification of hypersensitivity vasculitis. Arthritis Rheum. 1990, 33: 1108-1113.
Gibson LE, Su WPD: Cutaneous vasculitis. Rheum Dis Clin North Am. 1990, 16: 309-324.
Lie JT, and members and consultants of the American College of Rheumatoyogy Subcommittee on classification of vasculitis : Illustrated histopathologic classification criteria for selected vasculitis syndromes. Arthritis Rheum. 1990, 33: 1074-1087.
Zax RH, Hodge SJ, Callen JP: Cutaneous leukocytoclastic vasculitis: serial histopatologic evaluation demonstrates the dynamic nature of the infiltrate. Arch Dermatol. 1990, 126: 69-72. 10.1001/archderm.126.1.69
Smoller BR, McNutt S, Contreras F: The natural history of vasculitis. Arch Dermatol. 1990, 126: 84-89. 10.1001/archderm.126.1.84
de Vega T, Blanco S, Lopez C, Pacual E, Sanchez M, Zamarron A: Clarithromycin-induced leucocytoclastic vasculitis. Eur J Clin Microbiol Infect Dis. 1993, 12: 563-
VanArdsel PP: Drug hypersensitivity. In: Allergy, Asthma and Immunology from Infancy to Adulthood. Edited by: Bierman CW, Pearlman DS, Shapiro GG, Busse WW. 1996, 320-345. Philadelphia, WB Saunders Co, 3rd,
Fekety FR: Safety of parenteral third-generation cephalosporins. Am J Med. 1990, 88 (suppl 4A): S39-S44.
Reese RE, Betts RF, Gumustop B: Handbook of Antibiotics. Philadelphia, Lippincott Williams Wilkins. 2000, 3rd,
Feriozzi S, Muda AO, Gomes V, Montanaro M, Faraggiana T, Ancarani E: Cephotaxime-associated allergic interstitial nephritis and MPO-ANCA positive vasculitis. Ren Fail. 2000, 22: 245-251. 10.1081/JDI-100100869
Escudero A, Lucas E, Vidal JB, Sanchez-Guerrero I, Martinez A, Illan F, Ramos J: Drug-related Henoch-Schonlein Purpura. Allergol Immunopathol (Madr). 1996, 24: 22-24.
Totan M, Islek I: Hypersensitivity vasculitis induced by cefprozil. Ann Saudi Med. 2002, 22: 269-270.
Acknowledgment
Written consent was obtained from the patient or their relative for publication of study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
II followed the patient as hypersensitivity vasculitis and wrote this case report. SB made pathologic investigations and revised edition of this article. AOK followed clinically the patient as gangrenous appendicitis. EA followed clinically the patient as gangrenous appendicitis and helped to editing this report. NG followed the patient as hypersensitivity vasculitis and helped to editing this case report
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Islek, I., Baris, S., Katranci, A.O. et al. Hypersensitivity vasculitis induced by cefoperazone/sulbactam. Ann Clin Microbiol Antimicrob 2, 1 (2003). https://doi.org/10.1186/1476-0711-2-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-0711-2-1