Abstract
Background
Methicillin-resistant Staphylococcus aureus (MRSA) are clinically relevant pathogens that cause severe catheter-related nosocomial infections driven by several virulence factors.
Methods
We implemented a novel model of infection in vitro of reconstituted human epithelium (RHE) to analyze the expression patterns of virulence genes in 21 MRSA strains isolated from catheter-related infections in Mexican patients undergoing haemodialysis. We also determined the phenotypic and genotypic co-occurrence of antibiotic- and disinfectant-resistance traits in the S. aureus strains, which were also analysed by pulsed-field-gel electrophoresis (PFGE).
Results
In this study, MRSA strains isolated from haemodialysis catheter-related infections expressed virulence markers that mediate adhesion to, and invasion of, RHE. The most frequent pattern of expression (present in 47.6% of the strains) was as follows: fnbA, fnbB, spa, clfA, clfB, cna, bbp, ebps, eap, sdrC, sdrD, sdrE, efb, icaA, and agr. Seventy-one percent of the strains harboured the antibiotic- and disinfectant-resistance genes ermA, ermB, tet(M), tet(K), blaZ, qacA, qacB, and qacC. PFGE of the isolated MRSA revealed three identical strains and two pairs of identical strains. The strains with identical PFGE patterns showed the same phenotypes and genotypes, including the same spa type (t895), suggesting hospital personnel manipulating the haemodialysis equipment could be the source of catheter contamination.
Conclusion
These findings help define the prevalence of MRSA virulence factors in catheter-related infections. Some of the products of the expressed genes that we detected in this work may serve as potential antigens for inclusion in a vaccine for the prevention of MRSA-catheter-related infections.
Similar content being viewed by others
Introduction
Staphylococcus aureus is a bacterial pathogen that causes multiple infections in humans, ranging from superficial skin infections to endocarditis, bone and joint infections, septic shock [1], and severe haemodialysis catheter-related infections [2]. S. aureus produce a broad spectrum of extracellular and cell wall-associated virulence determinants that contribute to the severity of infection [3]. Microbial adherence to cells and extracellular matrix is an essential first step in the process of colonization and infection [4], for which S. aureus express numerous surface adhesins known as microbial surface components recognizing adhesive matrix molecules (MSCRAMMs). These adhesins mediate adherence to host extracellular matrix components such as fibrinogen, fibronectin, and collagen [5]. Pathogenic adhesins include Fibronectin-binding protein A and B (FnBPA and FnBPB); Staphylococcus protein A (Spa); clumping factor A (ClfA); clumping factor B (ClfB); collagen adhesion (Cna); sialoprotein-binding protein (Bbp); elastin-binding protein of Staphylococcus aureus (EbpS); extracellular adhesion protein (Eap); serine aspartate repeat proteins C, D, and E (SdrC, SdrD, and SdrE; [3]); and extracellular fibrinogen-binding protein (Efb; [6]). Furthermore, pathogenic S. aureus strains exhibit a great capacity for biofilm formation on surfaces, making endovascular catheters a favourable niche for infection. Biofilm formation requires synthesis of PNAG (polymeric N-acetylglucosamine); the enzymes responsible for its synthesis are encoded by the icaADBC operon [7]. Expression of most virulence factors in S. aureus is controlled by the agr locus [8].
The number of methicillin-resistant S. aureus (MRSA) strains has steadily increased and nosocomial infections caused by MRSA have become a serious problem worldwide, as its presence has dramatically reduced the number of effective antibiotics available for the prevention and treatment of infections in hospitals and communities [9]. The main mechanism of methicillin resistance involves expression of the mecA gene, which encodes penicillin-binding protein 2a (PBP2a), a transpeptidase with low affinity for β-lactams [10]. MRSA strains frequently carry genes for multidrug resistance such as blaZ, which codes β− lactamases and confers resistance to β-lactams; ermA, ermB, and ermC confer erythromycin resistance; aac(6 9)-Ie-aph(2 0)-Ia confers aminoglycoside resistance; tet(M), tet(O), and tet(K) confer resistance to tetracycline; and vanA and vanB confer vancomycin resistance [11]. Widespread use of quaternary ammonium compounds (QAC) in hospitals contributes to the selection of disinfectant-resistant S. aureus[12]. In several staphylococcal species, the qacA, qacB, and qacC genes have been identified in plasmids that also contain antibiotic-resistance genes [13–15].
The expression of virulence factors of S. aureus has been studied in vivo in animal models of infection [16, 17], but immune cellular factors and nutritional conditions have affected the expression of virulence determinants. To circumvent these problems, in this study we propose a novel model of infection in vitro of reconstituted human epithelium (RHE) to analyze the expression patterns of virulence genotypes of MRSA strains isolated from catheter-related infections in Mexican patients undergoing haemodialysis. We also determined the phenotypic and genotypic combinations of antibiotic- and disinfectant-resistance in the S. aureus strains, which also were analysed by pulsed-field-gel electrophoresis (PFGE).
Materials and methods
Bacterial strains
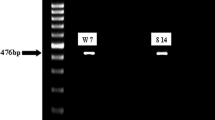
Twenty-one S. aureus strains were donated by the Laboratorio Clínico de la Facultad de Estudios Superiores Iztacala (Universidad Nacional Autónoma de México) for phenotypic and molecular analysis. These strains were isolated from catheter-related infections of ambulatory patients (n = 21) undergoing treatment at a public hospital in Estado de México, México from January to May 2013. The bacterial strains were identified by classical microbiologic methods: Gram staining; mannitol, catalase, and coagulase activity (Bactident-coagulase, Merck); and the Api 32 Staph test (BioMerieux). S. aureus strains were molecularly characterized by PCR amplification of 23S rRNA, coagulase (coa), thermonuclease (nuc), clumping factor (clf A), protein A region X (spa), femA, and femB[18, 19]. Bacterial DNA was extracted with the Wizard Genomic DNA Purification Kit (Promega). Resistance to methicillin was determined by the cefoxitin disc diffusion test (Becton Dickinson; inhibition zone, ≤21 mm) [20]. β-Lactamase enzymes were detected by using paper discs impregnated with the chromogenic cephalosporin nitrocephin (Becton Dickinson, USA). This substrate changes from yellow to red after the amide bond of the β-lactam ring is hydrolysed by β-lactamase. The change in colour was observed from 5 min–1 h. The mecA gene, which encodes methicillin resistance, was identified by conventional PCR [21]. S. aureus ATCC 25923 (mecA -) and ATCC 33592 (mecA+) were used as controls in each test.
Antibiotic susceptibility testing
The standard disc diffusion method of Kirby-Bauer in Mueller Hinton agar (Bioxon) was used to evaluate antibiotic susceptibility. Multidiscs for Gram-positive bacteria were used (Bio-Rad). Results were interpreted in accordance with Clinical and Laboratory Standards Institute guidelines [20]. The antibiotics were ampicillin (AM, 10 μg), cefalotin (CF, 30 μg), cefotaxime (CTX, 30 μg), levofloxacin (LEV, 5 μg), cefuroxime (CXM, 30 μg), dicloxacillin (DC, 1 μg), erythromycin (E, 15 μg), gentamycin (GE, 10 μg), cefepime (FEP, 30 μg), penicillin (PE, 10 U), tetracycline (TE, 30 μg), and trimethoprim-sulfamethoxazole (SXT, 25 μg). S. aureus ATCC 25923 (mecA-) and ATCC 33592 (mecA+) strains were used as controls in each test.
Detection of antibiotic and disinfectant resistance genes
The tet(M), tet(O), tet(K), vanA, vanB, aac(6 9)-Ie-aph(2 0)-Ia and blaZ genes were identified by PCR as described by Rizzotti et al.[11] and ermA, ermB, ermC, msrA, mef, qacA, qacB, and qacC as described by Zmantar et al.[12].
SCCmec types and agr groups
A multiplex PCR with four primer pairs was used to identify the five main known SCCmec types [22] and another multiplex PCR with five primers was used to identify the agr groups [23].
RHE inoculation with S. aureus
Reconstituted human epithelium (RHE; SkinEthic Laboratories, Nice, France) consists of human epithelial cell lines cultured on polycarbonate filters in vitro at the air-liquid interface in serum-free chemically defined medium. A total of 2 × 106 S. aureus cells suspended in 50 μL PBS were inoculated onto the surface of the RHE and incubated at 37°C for 72 h with 5% CO2 and saturated humidity. The maintenance media was changed every 24 h.
S. aureus RNA purification and reverse transcription
S. aureus cells were harvested from the RHE and suspended in 1 mL RNA Protect Bacteria Reagent (Qiagen). The sample was vortexed 30 s and incubated at room temperature 5 min. After centrifugation at 9400 rpm for 10 min, the cells were resuspended in 200 μL TE buffer (10 mM Tris–HCl, 1 mM EDTA, pH 8) containing 10 mg/mL lysozyme and 40 mg/mL lysostaphin. The sample was vortexed 10 s and incubated at room temperature 5 min. Total RNA was purified with the RN easy Mini Kit (Qiagen) according to the manufacturer’s instructions, including DNase treatment. The concentration and purity of total RNA were analysed with a NanoDrop 2000 spectrophotometer (Thermo Scientific). cDNA synthesis was performed with the QuantiTec Reverse transcription kit (Qiagen) according to the manufacturer’s instructions.
Real-Time PCR amplification
The primers for Real-Time PCR were described previously as follows: fnbA, fnbB, spa, clfA, clfB, cna, bbp, ebpS, eap, SdrC, sdrD, sdrE, and efb[3]; and agr[24]. The Rotor-Gene SYBR Green PCR kit (Qiagen) was used for Real-Time PCR expression profiling of icaA[25] and gyrB (reference gene; [26]) using a Rotor Gene Probe PCR Kit (Qiagen). S. epidermidis ATCC 35984 and Escherichia coli ATCC 11775 were used as negative controls. S. aureus ATCC 33592 was used as the positive control.
PFGE typing
MRSA isolates were PFGE typed by preparation of DNA and resolution of the SmaI-digested fragments as described by McDougal et al.[27]. Samples were separated on a CHEF-DR II system (Bio-Rad). Gels were photographed and digitized using a Bio-Rad Gel Doc. PFGE patterns were analysed as described by Tenover et al.[28] for bacterial strain typing.
Data analysis
PFGE patterns were analysed with Gene Tool and Gene Directory software (Syngene). Reference standard S. aureus NCTC 8325 was included in each gel for band normalization. Percent similarities were obtained from the weighted pair group with mathematical average (UPMGA) based on Dice coefficients. Band position tolerance was set at 1.25%. A similarity coefficient of 80% was selected to define the pulsed-field type clusters.
spa typing
The polymorphic X region of the protein A coding gene (spa) was amplified and sequenced as described [29]. Corresponding spa-types were assigned using the SPA Searcher website (http://seqtools.com). Ridom spa types were subsequently assigned using the spa-typing website (http://www.spaserver.ridom.de/) developed by Ridom Gmb.
Results
All S. aureus strains (n = 21) were resistant to methicillin (Table 1). All MRSA strains (n = 21) expressed 7/15 studied genes: spa, clfB cna, bbp, sdrC, icaA, and agr. [group II (n = 18); group I (n = 3)] during in vitro infection of RHE (Table 2); 95.2% (n = 20) expressed sdrD and efb; 90.4% (n = 19) expressed fnbA, clfA, ebps, and eap; 85.7% (n = 18) expressed sdrE; and 80.9% (n = 17) expressed fnbB.
Without considering the 7 genes expressed by all MRSA strains, ten distinct expression patterns of virulence markers were found during MRSA infection of RHE in vitro (Table 3). Pattern 1, formed by the other 8 studied genes (fnbA, fnbB, clfA, ebps, eap, sdrD, sdrE, ebf) was present in ten (n = 47.7%) MRSA isolates, whereas patterns 2 and 3, both composed of 7 genes each, were expressed by two strains. The other seven patterns were constituted by 4–7 genes and were expressed only by one MRSA strain (Table 3).
PFGE analysis showed that MRSA strains were distributed in 15 distinct electrophoretic patterns (data not shown). MRSA strains S-22 and S-36 (Table 2), isolated from the catheters of different patients, have identical electrophoretic patterns (data not shown) and the same spa type as the S-59 and S-66 MRSA strains (spa type t895). Three strains isolated from different patients showed 100% similarity by PFGE (S-77, S-79, S-82; Table 2) and belonged to the same spa type t895. Two closely related strains (S-8 and S108) were isolated from the catheters of two different patients and two possibly related strains (S-16 and S-19) were isolated from two different patients. The strains with identical PFGE patterns (S-22 and S-36; S-59 and S-66; S-77, S-79 and S-82) showed the same phenotypes and genotypes (Table 1). The most frequent spa types were t895 (76.2%; n = 16) and t008 (14.2%; n = 3; Table 2).
All MRSA strains were resistant to erythromycin (E), ampicillin (AM), tetracycline (TE), and penicillin (PE; Table 1). The frequency of resistance to other antibiotics tested was: cefotaxime (CTX) 95.2%, n = 20; dicloxacillin (DC) 95.2%, n = 20; cefepime (FEP) 90.5%, n = 19; cefuroxime (CXM) 66.7%, n = 14; cefalotin (CF) 62%, n = 13; levofloxacin (LEV) 57.1%, n = 12; trimethoprim-sulfamethoxazole (SXT) 14.3%, n = 3; and gentamycin (GE) 14.3%, n = 3 (Table 1). All MRSA strains were β-lactamase producers (Table 1). The following patterns of antibiotic resistance were found: 5 antibiotics (1 strain), 6 antibiotics (2 strains), 7 antibiotics (5 strains), 9 antibiotics (1 strain), 10 antibiotics (8 strains), 11 antibiotics (3 strains), and 12 antibiotics (1 strain) (Table 1).
Type IV SCCmec was identified by PCR in 12 MRSA strains, whereas type II SCCmec was detected in 6 strains, and type I SCCmec in 3 strains (Table 1). The ermA and ermB genotypes were identified in all strains, whereas ermC was detected only in S-73. All strains carried the tet(M), tet(K), and blaZ genes. The aac(6 9)-Ie- aph(2 0)-Ia gene was identified in gentamycin-resistant strains S-19, S-58, and S-108 (Table 2). The mrsA, mef, tet(O), vanA, and vanB antibiotic resistance genes were not identified in any of the MRSA strains.
Our evaluation of disinfectant resistance revealed 100% (n = 21) of the MRSA strains carried qacC, 76% (n = 16) carried qacA, and 76% (n = 16) carried qacB. Fifteen strains (71.4%) showed the same phenotype/genotype pattern: resistance to erythromycin, ampicillin, tetracycline, cefotaxime, penicillin, β-lactamase production/ermA, ermB, tet(M), tet(K), blaZ, qacA, qacB, and qacC positivity.
Discussion
Haemodialysis patients who are infected with methicillin-resistant Staphylococcus aureus (MRSA) are considered to have healthcare-associated (HA) infections [30, 31].
For colonization and infection, bacterial adhesion to host extracellular matrix components like fibrinogen, fibronectin, and collagen is essential [5]. Therefore, there has been a strong interest in studying the involvement of proteins of the MSCRAMMs family of S. aureus using in vivo and in vitro models of infection [32–35]. In this study we implemented a novel model of infection in vitro of reconstituted human epithelium (RHE) to analyze the expression patterns of the MSCRAMMs family adhesion genes, and icaA and agr in S. aureus strains isolated from catheter-related infections in Mexican patients subjected to haemodialysis. Our data show that most of the genes that we studied were expressed by MRSA after infection of RHE (Table 2), which reflects the pathogenic behaviour of these strains. We identified ten different patterns of expression (Table 3), of which pattern No. 1, represented by the 15 genes studied (fnbA, fnbB, spa, clfA, clfB, cna, bbp, ebps, eap, sdrC, sdrD, sdrE, efb, icaA, agr), was present in ten MRSA strains (47.7%; Table 3). These results show that during infection of RHE, the MRSA strains expressed 11 to 13 genes coding for bacterial surface proteins; icaA, which participates in biofilm formation [7]; and the agr locus, which is a global regulator of multiple virulence factors [8]. These findings are consistent with the notion that pathogenesis of most S. aureus infections cannot be explained by the action of an unique virulence factor, but by several distinct factors acting in concert during the infective process [36]. Cna has been associated with endocarditis [37] and keratitis [38]. Fibronectin-binding proteins mediate adherence to human airway epithelium [4]. Clumping factor A (ClfA) plays an antiphagocytic role in neutrophils and macrophages [39] and is necessary for infection/pathogenesis in in vivo models of arthritis, sepsis, and endocarditis [40, 41]. Clumping factor B (ClfB) mediates respiratory infection and attachment to cytokeratins on nasal epithelial cells [42] and the role of protein A (Spa) in S. aureus virulence has been demonstrated in models of sepsis and pneumonia [43]. Although the precise role of Sdr adhesins in staphylococcal infection is unknown, a strong correlation between the sdr genes of S. aureus and certain diseases has been reported. There is a significantly increased prevalence of the sdrE gene in invasive S. aureus strains [44], in S. aureus strains responsible for osteomyelitis [45] and in S. aureus isolates responsible for bone infections [46]. A recent report noted that Eap is associated with invasive diseases [33].
Earlier findings suggested a possible relationship between particular agr groups with the capacity of MRSA to cause specific illnesses. The agr I and agr II strains are associated with suppurative infections; agr III is associated with toxic shock syndrome toxin (TSST-1) mediated disease, and agr IV is associated with exfoliative toxin- and impetigo-producing strains [47]. Consistent with these findings, the strains reported in this work were isolated from suppurative catheter-related infections, or initiating suppurative catheter-related infections, and carried agr II (85.7%, n = 18) or agr I (14.3%, n = 3; Table 2).
Most of the strains reported here carried the SCCmec type IV (57%, n = 12; Table 1), an allele initially considered to be a characteristic of community-acquired MRSA (CA-MRSA; [48]). However, MRSA infections in dialysis-dependent patients have been considered to be mainly HA (healthcare-associated) according to epidemiologic classifications [49], and there are several reports of MRSA strains harbouring SCCmec type IV in HA infections [30, 31, 50–52]. The increase in multiple drug-resistant (MDR) MRSA has become a major challenge for the treatment of infectious diseases caused by what are known as superbugs. Strikingly, all the strains reported here were multidrug resistant β-lactamase producers. They were resistant to 5 to 12 antibiotics. None of the strains was sensitive to erythromycin, ampicillin, tetracycline, or penicillin (Table 1). On the other hand, only three strains (14.3%) were resistant to sulfamethoxasole/Trimethoprim or gentamycin. The high frequency of resistance to these antibiotics may reflect the fact that physicians of the public health service in Mexico prescribe all of these antibiotics, which are considered essential drugs in this sector.
The most frequent combination of antibiotic- and disinfectant-resistance phenotype/genotype in the MRSA strains (71.4%, n = 15) was: resistance to erythromycin, ampicillin, tetracycline, cefotaxime, penicillin, and β-lactamase production in association with ermA, ermB, tet(M), tet(K), blaz, qacA, qacB, and qacC genotypes (Table 1). These strains are not only resistant to five antibiotics, but also harbour three of the six plasmid-encoded MDR efflux pumps which mediate resistance to several biocides such as antimicrobial organic cations, including intercalating dyes (e.g., acriflavine and ethidium bromide), and quaternary ammonium compounds (e.g., benzalkonium chloride; [53]). Staphylococcal strains resistant to disinfectant have been identified in clinical isolates of MRSA from China (62%; [54]), Taiwan (55.4%; [55]), and Hong Kong (42%; [56]). All the erythromycin-resistant MRSA strains reported here carried the ermA and ermB genes and two strains (S-73 and S-108) carried the ermC gene. The msrA and mef genes were not detected in either strain (Table 1). We did not find discordances between the presence of erm genes and phenotypic resistance to erythromycin, as has been reported in other studies [12, 57]. The incidence of ermA genes in our MRSA strains (100%) is higher than those reported in erythromycin-resistant S. aureus: 7.7% in Tunisia [12] and 16% in Denmark [58].
All MRSA strains were resistant to tetracycline and possessed the tet(M) and tet(K) genes (Table 1). Tetracycline is an antibiotic commonly used in Mexico to treat human and animal bacterial infections, contributing to the selection and propagation of resistant strains. Tetracycline resistance in S. aureus is encoded by the pT181 plasmid [59] and the tet (M) gene can be found in combination with ermB in the Tn916 transposon. The simultaneous presence of these genes has been found frequently in enterococci, as well as in streptococci and staphylococci [60]. Consistent with this, all the strains studied here carried these two genes, suggesting the presence of these genetic elements in the MRSA we analysed.
The gene aac(6 9)-Ie-aph(2 0)-Ia was detected in three strains (S-19, S-58, and S-108) that were also resistant to gentamycin; the vanA and vanB genes were not detected in any MRSA strain.
The strains with identical PFGE patterns showed the same phenotypes, genotypes, and spa type, suggesting that hospital personnel manipulating the haemodialysis equipment could be the cause of catheter contamination by these strains.
Our results are relevant because they demonstrate that MRSA strains isolated from catheter-related infections in haemodialysis patients express several virulence markers involved in the adhesion and invasion of RHE. We also analysed the phenotypes and genotypes of antibiotics and disinfectant resistance. These results will help define the incidence of virulence factors in MRSA associated with catheter-related infections and improve therapies in haemodialysis patients. In addition, some of the products of the expressed genes that we detected in this work may serve as potential antigens for inclusion in a vaccine for the prevention of MRSA-catheter-related infections.
References
Diekema DJ, Pfaller MA, Schmitz FJ, Smayevsky J, Bell J, Jones RN, Beach M: Survey of infections due to Staphylococcus species: frequency of occurrence and antimicrobial susceptibility of isolates collected in the United States, Canada, Latin America, Europe, and the Western Pacific region for the SENTRY Antimicrobial Surveillance Program, 1997–1999. Clin Infect Dis 2001,32(Suppl 2):S114-S132.
Viale P, Stefani S: Vascular catheter-associated infections: a microbiological and therapeutic update. J Chemother 2006, 18: 235-249. 10.1179/joc.2006.18.3.235
Campbell SJ, Deshmukh HS, Nelson CL, Bae IG, Stryjewski ME, Federspiel JJ, Tonthat GT, Rude TH, Barriere SL, Corey R, Fowler VG Jr: Genotypic characteristics of Staphylococcus aureus isolates from a multinational trial of complicated skin and skin structure infections. J Clin Microbiol 2008, 46: 678-684. 10.1128/JCM.01822-07
Mongodin E, Bajolet O, Cutrona J, Bonnet N, Du-puit F, Puchelle E, de Bentzmann S: Fibronectin-binding proteins of Staphylococcus aureus are involved in adherence to human airway epithelium. Infect Immun 2002, 70: 620-630.
Navarre W, Schneewind O: Surface proteins of Gram-positive bacteria and mechanisms of their targeting to the cell wall envelope. Microbiol Mol Biol Reviews 1999, 63: 174-229.
Lee LY, Liang X, Hook M, Brown EL: Identification and characterization of the C3 binding domain of the Staphylococcus aureus extracellular fibrinogen- binding protein (Efb). J Biol Chem 2004, 279: 50710-50716. 10.1074/jbc.M408570200
Götz F: Staphylococcus and Biofilms. Mol Microbiol 2002, 43: 1367-1378. 10.1046/j.1365-2958.2002.02827.x
Ji G, Beavis RC, Novick RP: Cell density control of staphylococcal virulence mediated by an octapeptide pheromone. Proc Natl Acad Sci USA 1995, 92: 12055-12059. 10.1073/pnas.92.26.12055
Gould IM: The clinical significance of methicillin-resistant Staphylococcus aureus . J Hosp Infect 2005, 61: 277-282. 10.1016/j.jhin.2005.06.014
Hartman BJ, Tomasz A: Low-affinity penicillin-binding protein associated with beta-lactam resistance in Staphylococcus aureus . J Bacteriol 1984, 158: 513-516.
Rizzotti L, Simeoni D, Cocconcelli P, Gazzola S, Dellaglio F, Torriani S: Contribution of enterococci to the spread of antibiotic resistance in the production chain of swine meat commodities. J Food Prot 2005, 68: 955-965.
Zmantar T, Kouidhi B, Miladi H, Bakhrouf A: Detection of macrolide and disinfectant resistance genes in clinical Staphylococcus aureus and coagulase-negative staphylococci. BMC Res Notes 2011, 4: 453. 10.1186/1756-0500-4-453
Anthonisen IL, Sunde M, Steinum TM, Sidhu MS, Sorum H: Organization of the antiseptic resistance gene qacA and Tn552-related β-lactamase genes in multidrug-resistant Staphylococcus haemolyticus strains of animal and human origins. Antimicrob Agents Chemother 2002, 46: 3606-3612. 10.1128/AAC.46.11.3606-3612.2002
Mayer S, Boos M, Beyer A, Flui AC, Schmitz FJ: Distribution of the antiseptic resistance genes qacA, qacB and qacC in 497 methicillin resistant and susceptible European isolates of Staphylococcus aureus . J Antimicrob Chemother 2001, 47: 896-897. 10.1093/jac/47.6.896
Sidhu MS, Heir E, Sorum H, Holck A: Genetic linkage between resistance to quaternary ammonium compounds and β lactam antibiotics in food related Staphylococccus spp. Microb Drug Resis 2001, 7: 363-371. 10.1089/10766290152773374
Burian M, Rautenberg M, Kohler T, Fritz M, Krismer B, Unger C, Hoffmann WH, Peschel A, Wolz C, Goerke C: Temporal expression of adhesion factors and activity of global regulators during establishment of Staphylococcus aureus nasal colonization. J Infect Dis 2010, 201: 1414-1421. 10.1086/651619
Montgomery CP, Boyle-Vavra S, Adem PV, Lee JC, Husain AN, Clasen J, Daum RS: Comparison of virulence in community associated methicillin-resistant Staphylococcus aureus pulsotypes USA300 and USA400 in a rat model of pneumonia. J Infect Dis 2008, 198: 561-570. 10.1086/590157
Kobayashi N, Wu H, Kojima K, Taniguchi K, Urasawa S, Uehara N, Omizu Y, Kishi Y, Yagihashi A, Kurokawa I: Detection of mecA , femA and femB genes in clinical strains of staphylococci using polymerase chain reaction. Epidemiol Infect 1994, 113: 259-266. 10.1017/S0950268800051682
Nashev D, Toshkova K, Salasia ISO, Hassan AA, Lämmler C, Zschöck M: Distribution of virulence genes of Staphylococcus aureus isolated from stable nasal carriers. FEMS Microbiol Lett 2004, 233: 45-52. 10.1016/j.femsle.2004.01.032
CLSI Twenty-Third Informational Supplement M100-S23. In Performance Standards for Antimicrobial Susceptibility Testing. Wayne, PA: Clinical and Laboratory Standards Institute; 2013.
Geha DJ, Uhl JR, Gustaferro CA, Persing DH: Multiplex PCR for identification of methicillin-resistant staphylococci in the clinical laboratory. J Clin Microbiol 1994, 32: 1768-1772.
Boye K, Bartels MD, Andersen IS, Møller JA, Westh HA: New multiplex PCR for easy screening of methicillin-resistant Staphylococcus aureus SCC mec types I–V. Clin Microbiol Infect 2007, 13: 725-727. 10.1111/j.1469-0691.2007.01720.x
Gilot P, Lina G, Cochard T, Poutrel B: Analysis of the genetic variability of genes encoding the RNA III-activating components Agr and TRAP in a population of Staphylococcus aureus strains isolated from cows with mastitis. J Clin Microbiol 2002, 40: 4060-4067. 10.1128/JCM.40.11.4060-4067.2002
van Leeuwen W, van Nieuwenhuizen W, Gijzen C, Verbrugh H, Van Belkum A: Population studies of methicillin-resistant and sensitive Staphylococcus aureus strains reveal a lack of variability in the agrD gene, encoding a staphylococcal autoinducer peptide. J Bacteriol 2000, 182: 5721-5729. 10.1128/JB.182.20.5721-5729.2000
Valle J, Toledo-Arana A, Berasain C, Ghigo JM, Amorena B, Penades JR, Lasa I: SarA and not σB is essential for biofilm development by Staphylococcus aureus . Mol Microbiol 2003, 48: 1075-1087. 10.1046/j.1365-2958.2003.03493.x
Beenken KE, Dunman PM, McAleese F, Macapagal D, Murphy E, Projan SJ, Blevins JS, Smeltzer MS: Global gene expression in Staphylococcus aureus biofilms. J Bacteriol 2004, 186: 4665-4684. 10.1128/JB.186.14.4665-4684.2004
McDougal LK, Steward CD, Killgore GE, Chaitram JM, McAllister SK, Tenover FC: Pulsed-field gel electrophoresis typing of oxacillin-resistant Staphylococcus aureus isolates from the United States: Establishing a National Database. J Clin Microbiol 2003, 41: 5113-5120. 10.1128/JCM.41.11.5113-5120.2003
Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, Persing DH, Swaminathan B: Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol 1995, 33: 2233-2239.
Shopsin B, Gomez M, Montgomery SO, Smith DH, Waddington M, Dodge DE, Bost DA, Riehman M, Naidich S, Kreiswirth BN: Evaluation of protein A gene polymorphic region DNA sequencing for typing of Staphylococcus aureus strains. J Clin Microbiol 1999, 37: 3556-3563.
Johnson LB, Venugopal AA, Pawlak J, Saravolatz LD: Emergence of community-associated methicillin-resistant Staphylococcus aureus infection among patients with end-stage renal disease. Infect Control Hosp Epidemiol 2006, 27: 1057e62.
Johnson LB, Jose J, Yousif F, Pawlak J, Saravolatz LD: Prevalence of colonization with community-associated methicillin resistant Staphylococcus aureus among end-stage renal disease patients and healthcare workers. Infect Control Hosp Epidemiol 2009, 30: 4e8.
Bur S, Preissner KT, Herrmann M, Bischoff M: The Staphylococcus aureus extracellular adherence protein promotes bacterial internalization by keratinocytes independent of fibronectin-binding proteins. J Invest Dermatol 2013, 133: 2004-2012. 10.1038/jid.2013.87
Edwards AM, Bowden MG, Brown EL, Laabei M, Massey RC: Staphylococcus aureus extracellular adherence protein triggers TNFα release, promoting attachment to endothelial cells via protein A. PLoS One 2012, 7: e43046. 10.1371/journal.pone.0043046
Oogai Y, Matsuo M, Hashimoto M, Kato F, Sugai M, Komatsuzawa H: Expression of virulence factors by Staphylococcus aureus grown in serum. Appl Environ Microbiol 2011, 77: 8097-8105. 10.1128/AEM.05316-11
Veloso TR, Chaouch A, Roger T, Giddey M, Vouillamoz J, Majcherczyk P, Que YA, Rousson V, Moreillon P, Entenza JM: Use of a human-like low-grade bacteremia model of experimental endocarditis to study the role of Staphylococcus aureus adhesins and platelet aggregation in early endocarditis. Infect Immun 2013, 81: 697-703. 10.1128/IAI.01030-12
Peacock SJ, Day NPJ, Thomas MG, Berendt AR, Foster TJ: Clinical isolates of Staphylococcus aureus exhibit diversity in fnb genes and adhesion to human fibronectin. J Infection 2000, 41: 23-31. 10.1053/jinf.2000.0657
Hienz SA, Schennings T, Heimdahl A, Flock JI: Collagen binding of Staphylococcus aureus is a virulence factor in experimental endocarditis. J Infect Dis 1996, 174: 83-88. 10.1093/infdis/174.1.83
Rhem MN, Lech EM, Patti JM, McDevitt D, Hook M, Jones DB, Wilhelmus KR: The collagen-binding adhesin is a virulence factor in Staphylococcus aureus keratitis. Infect Immun 2000, 68: 3776-3779. 10.1128/IAI.68.6.3776-3779.2000
Higgins J, Loughman A, van Kessel KP, van Strijp JA, Foster TJ: Clumping factor A of Staphylococcus aureus inhibits phagocytosis by human polymorphonuclear leucocytes. FEMS Microbiol Lett 2006, 258: 290-296. 10.1111/j.1574-6968.2006.00229.x
Josefsson E, Hartford O, O’Brien L, Patti JM, Foster T: Protection against experimental Staphylococcus aureus arthritis by vaccination with clumping factor A, a novel virulence determinant. J Infect Dis 2001, 184: 1572-1580. 10.1086/324430
Vernachio J, Bayer AS, Le T, Chai YL, Prater B, Schneider A, Syribeys P, Robbins J, Patti JM: Anti-clumping factor A immunoglobulin reduces the duration of methicillin-resistant Staphylococcus aureus bacteremia in an experimental model of infective endocarditis. Antimicrob Agents Chemother 2003, 47: 3400-3406. 10.1128/AAC.47.11.3400-3406.2003
O’Brien LM, Walsh EJ, Massey RC, Peacock SJ, Foster TJ: Staphylococcus aureus clumping factor B (ClfB) promotes adherence to human type I cytokeratin 10: implications for nasal colonization. Cell Microbiol 2002, 4: 759-770. 10.1046/j.1462-5822.2002.00231.x
Bubeck WJ, Patel RJ, Schneewind O: Surface proteins and exotoxins are required for the pathogenesis of Staphylococcus aureus pneumonia. Infect Immun 2007, 75: 1040-1044. 10.1128/IAI.01313-06
Peacock SJ, Moore CE, Justice A, Kantzanou M, Story L, Mackie K, O’Neill G, Day NP: Virulent combinations of adhesin and toxin genes in natural populations of Staphylococcus aureus . Infect Immun 2002, 70: 4987-4996. 10.1128/IAI.70.9.4987-4996.2002
Sabath A, Melles DC, Martirosian G, Grundmann H, van Belkum A, Hryniewicz W: Distribution of the serine-aspartate repeat protein encoding sdr genes among nasal and invasive Staphylococcus aureus strains. J Clin Microbiol 2006, 44: 1135-1138. 10.1128/JCM.44.3.1135-1138.2006
Trad S, Allignet J, Frangeul L, Davi M, Vergassola M, Couve E, Morvan A, Kechrid A, Buchrieser C, Glaser P, El-Solh N: DNA macroarray for identification and typing of Staphylococcus aureus isolates. J Clin Microbiol 2004, 42: 2054-2064. 10.1128/JCM.42.5.2054-2064.2004
Jarraud S, Mougel C, Thioulouse J, Lina G, Meugnier H, Forey F, Nesme X, Etienne J, Vandenesch F: Relationships between Staphylococcus aureus genetic background, virulence factors, agr groups (alleles), and human disease. Infect Immun 2002, 70: 631-641. 10.1128/IAI.70.2.631-641.2002
Deurenberg RH, Vink C, Kalenic S, Friedrich AW, Bruggeman CA, Stobberingh EE: The molecular evolution of methicillin-resistant Staphylococccus aureus . Clin Microbiol Infect 2007, 13: 222-235. 10.1111/j.1469-0691.2006.01573.x
Buck JM, Como-Sabetti K, Harriman KH, Danila RN, Boxrud DJ, Glennen A, Lynfield R: Community-associated methicillin-resistant Staphylococcus aureus , Minnesota, 2000–2003. Emerg Infect Dis 2005, 11: 1532-1538. 10.3201/eid1110.050141
Centers for Disease Control and Prevention (CDC): Invasive methicillin-resistant Staphylococcus aureus infections among dialysis patients United States, 2005. MMWR Morb Mortal Wkly Rep 2007, 56: 197-199.
Lin CC, Wang JL, Lin CY, Chen SY, Wang JT, Wu KD: Methicillin-resistant Staphylococcus aureus bacteremia in patients with end-stage renal disease in Taiwan: distinguishing between community-associated and healthcare-associated strains. Infect Control Hosp Epidemiol 2009, 30: 89-92. 10.1086/593122
Strandén AM, Frei R, Adler H, Flückiger U, Widmer AF: Emergence of SCC mec type IV as the most common type of methicillin-resistant Staphylococcus aureus in a university hospital. Infection 2009, 37: 44-48. 10.1007/s15010-008-7430-7
Littlejohn TG, Paulsen IT, Gillespie MT, Tennent JM, Midgley M, Jones IG, Purewal AS, Skurray RA: Substrate specificity and energetics of antiseptic and disinfectant resistance in Staphylococcus aureus . FEMS Microbiol Lett 1992, 74: 259-265.
Wang C, Cai P, Zhan Q, Mi Z, Huang Z, Chen G: Distribution of antiseptic-resistance genes qacA/B in clinical isolates of methicillin-resistant Staphylococcus aureus in China. J Hosp Infect 2008, 69: 393-394. 10.1016/j.jhin.2008.05.009
Wang JT, Sheng WH, Wang JL, Chen D, Chen ML, Chen YC, Chang SC: Longitudinal analysis of chlorhexidine susceptibilities of nosocomial methicillin-resistant Staphylococcus aureus isolates at a teaching hospital in Taiwan. J Antimicrob Chemother 2008, 62: 514-517. 10.1093/jac/dkn208
Zhang M, O’Donoghue MM, Ito T, Hiramatsu K, Boost MV: Prevalence of antiseptic-resistance genes in Staphylococcus aureus and coagulase-negative staphylococci colonizing nurses and the general population in Hong Kong. J Hosp Infect 2011, 8: 113-117.
Sekiguchi J, Hama T, Fujino T, Araake M, Irie A, Saruta K, Konosaki H, Nishimura H, Kawano A, Kudo K, Kondo T, Sasazuki T, Kuratsuji T, Yoshikura H, Kirikae T: Detection of the antiseptic- and disinfectant-resistance genes qacA, qacB, and qacC in methicillin-resistant Staphylococcus aureus isolated in a Tokyo hospital. Jpn J Infect Dis 2004, 57: 288-291.
Westh H, Hougaard DM, Vuust J, Rosdahl VT: erm genes in erythromycin resistant Staphylococcus aureus and coagulase-negative staphylococci. APMIS 1995, 103: 225-232. 10.1111/j.1699-0463.1995.tb01099.x
Ito T, Okuma K, Ma XX, Yuzawa H, Hiramatsu K: Insights on antibiotic resistance of Staphylococcus aureus from its whole genome: genomic island SCC. Drug Resist Update 2003, 6: 41-52. 10.1016/S1368-7646(03)00003-7
Chopra I, Roberts M: Tetracycline antibiotics: mode of action, applications, molecular biology and epidemiology of bacterial resistance. Microbiol Mol Biol 2001, 65: 232-260. 10.1128/MMBR.65.2.232-260.2001
Acknowledgement
This project was supported through the PAPCA Nº 7 2013, FES-Iztacala, Universidad Nacional Autónoma de México.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
GLPC, EMP, JRRM and ENA have made substantial contributions to acquisition of data. FVP has made substantial contributions to analysis and interpretation of data. SV has been involved in drafting the manuscript and has given final approval of the version to be published. All authors have read and approved the manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Paniagua-Contreras, G.L., Monroy-Pérez, E., Vaca-Paniagua, F. et al. Implementation of a novel in vitro model of infection of reconstituted human epithelium for expression of virulence genes in methicillin-resistant Staphylococcus aureus strains isolated from catheter-related infections in Mexico. Ann Clin Microbiol Antimicrob 13, 6 (2014). https://doi.org/10.1186/1476-0711-13-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-0711-13-6