Abstract
Background
The mechanism behind the triggering effect of fine particulate matter (PM) air pollution on cardiovascular events remains elusive. We postulated that elevated levels of PM would be associated with increased blood levels of inflammatory and thrombotic markers in elderly individuals. We also hypothesized that elevated PM would increase levels of cytokines in individuals with heart disease.
Methods
We measured these blood markers in 47 elderly individuals with (23) and without (16 COPD and 8 healthy) cardiovascular disease (CVD) on 2 or 3 mornings over a 5 or 10-day period between February 2000 and March 2002. Blood measures were paired with residence level outdoor PM measured by nephelometry. Analyses determined the within-individual effect of 24-hour averaged outdoor PM on blood measures.
Results
Analyses found no statistically significant effect of a same day 10 ug/m3 increase in fine PM on log transformed levels of CRP 1.21 fold-rise [95% CI: 0.86, 1.70], fibrinogen 1.02 fold-rise [95% CI: 0.98, 1.06], or D-dimer 1.02 fold-rise [95% CI: 0.88, 1.17] in individuals with CVD. One-day lagged analyses in the CVD subgroup found similar null results. These same models found no change in these blood markers at the same-day or 1-day lag in the group without CVD. In 21 individuals with CVD, a 10 μg/m3 increase in same-day PM was associated with a 1.3 fold-rise [95% CI: 1.1, 1.7] in the level of monocyte chemoattractant protein-1.
Conclusion
We did not find consistent effects of low ambient levels of PM on blood measures of inflammation or thrombosis in elderly individuals.
Similar content being viewed by others
Background
Epidemiological studies have found associations between elevation in levels of fine particulate matter air pollution (PM) and risk of cardiovascular morbidity and mortality in the elderly [1–4]. Moreover, short-term elevations in PM2.5 have been associated with triggering the onset of myocardial infarction and AICD discharges [5–7]. However, the mechanism behind this triggering of cardiovascular events by PM2.5 remains unclear.
The cardiac effects of air pollution may be induced by a systemic inflammatory response [8–16]. Recent studies indicate that ischemic heart disease is likely mediated at least in part by inflammation [17]. Inflammation plays a substantial role in atherogenic progression, alterations in endothelial function and potentially mediates acute plaque rupture [17, 18]. Similarly, in vitro and animal studies have highlighted the potential for PM2.5 to induce a systemic inflammatory response and systemic oxidative stress that could result in impaired endothelial function [19, 20].
Epidemiological studies have suggested that elevated fine PM is associated with increased CRP [21] and fibrinogen [22] levels in healthy middle-age individuals. However, there are inconsistent findings of pollutant effect on fibrinogen after controlled exposures to ambient PM in healthy volunteers [14, 23]. Moreover, these controlled exposure studies to concentrated ambient PM have not detected increased levels of interleukin-6 (IL-6), CRP or other pro-atherogenic cytokines [13, 14, 23]. Last, the only study that assessed the effect of short-term elevations in PM levels on systemic markers of inflammation in a susceptible elderly population found no effect on IL-6 or fibrinogen levels and inconsistent effect on CRP [24]. To determine whether PM2.5 is associated with changes in within-individual measures of inflammation or thrombosis, we performed a repeated measures study of these blood markers at the residence level in elderly individuals with and without heart disease. We hypothesized that increased levels of fine PM would be associated with intra-individual increases in CRP levels in those with heart disease. Moreover, we postulated that endothelin-1 and IL-6 levels would be elevated on high air pollution exposure days in individuals with pre-existing heart disease.
Methods
We performed repeated blood measures of inflammation and thrombosis in 47 elderly individuals with and without cardiovascular disease (CVD) or chronic obstructive pulmonary disease (COPD) participating in a larger prospective study on health effects of air pollution in Seattle [25]. Briefly, subjects were monitored intensively for air pollution exposures and health outcomes over a 10-day period between February 2000 and May 2001, or a 5-day period between December 2001 and March 2002. Blood samples were collected at the subject's home at approximately the same time on two or three mornings during this monitoring period. This blood was assayed for measures of inflammation, and thrombosis. In a subset of 21 participants with CVD, bloods were also assayed for cytokine responses. These data were paired with outdoor nephelometry measures of fine PM made at the individuals' homes. These data were further enhanced by meteorological variables: hourly averages of relative humidity (RH), and temperature; daily questionnaire responses on: medication use (3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors (statins), aspirin, prednisone, warfarin, heparin, and clopidrogel) and clinic visits. The study protocol was approved by the University of Washington Human Subjects Division.
Study population
Individuals were eligible if they were living in the greater metropolitan Seattle area and >=55 years of age. The CV population had physician diagnosed ischemic heart disease or congestive heart failure. COPD participants had an FEV1<70% and >40% of predicted. Subjects were excluded if they had unstable angina, myocardial infarction, pneumonia or COPD exacerbation within 30 days of study. Subjects were non-smokers who lived with non-smokers.
Subject recruitment
Subjects were recruited by advertisement in senior centers and local newspapers and from medical clinics.
Exposure measures
The primary exposure metric was 24-hour averaged fine PM (from 8-8 am) measured at 0-day and 1-day lags prior to blood measures. PM was measured by nephelometry (Radiance Research, Seattle), as a light scattering coefficient, outside of the participant's residence. Nephelometry data correlate well with gravimetric particle measurements in the 0.1–1.4 aerodynamic range [26]. To allow for comparability to other studies, we calibrated the nephelometric measure of PM against a gravimetric PM2.5 measure. In 10 individuals where outdoor nephelometry data were not measured, we used a closest home outdoor nephelometer to capture local PM levels. This nephelometer was located within 2-miles of the subjects' residence. A total of 18 person-days of surrogate nephelometer exposure measures were used in our final analysis.
Blood measures
Blood samples were drawn from an antecubital vein from the seated subject following the recommendations of the International Committee for Standardization in Haematology[27]. Blood samples were immediately placed on ice and centrifuged within 2 hours. The serum was stored at -70°C for later batched analysis.
High sensitivity C-reactive protein (CRP) was measured using the Dade-Behring radioimmunoassay method[28]. This assay had a lower limit of detection at 0.02 mg/l. The intra-assay coefficient of variation was less than 5%. Fibrinogen levels were measured in citrated plasma by the Clauss method[29]. D-dimer was measured in citrated plasma using an enzyme immunoassay (Diagnostica Stago). D-dimer results are reported in ng/ml of fibrinogen equivalent units (FEU).
The measures of endothelin-1(ET-1), interleukin-6(IL-6), interleukin-6 receptor (IL-6r), tumor necrosis factor-α (TNF-α), tumor necrosis factor-receptors (p55, p75) and monocyte chemoattractant protein-1(MCP-1) were performed in duplicate using standard ELISA techniques (R&D Systems, Minneapolis). The intra-assay coefficient of variation for ELISA assays ranged from 2.7% for IL-6 to 5% for ET-1.
Statistical analysis
The data were analyzed using the statistical package SAS (version 8.02, Cary NC). The inflammatory and thrombotic measures were log transformed prior to analyses. For ease of clinical interpretation, we present the data after the beta coefficient has been converted to a natural scale. Effect sizes can be interpreted as the multiplicative change in mean outcome associated with a 10 ug/m3 increase in fine PM.
Primary analysis
We used a mixed model with random intercepts for unique subject-sessions (SAS Proc Mixed procedure) to determine the within-individual effect of zero-day and one-day lagged 24-hour averaged outdoor PM on measures of inflammation (CRP and fibrinogen) and thrombosis (D-dimer) for individuals in each health group. Final models were adjusted for age, gender, medication use, and meteorological variables (temperature and relative humidity as both linear and quadratic terms), and the interaction of outdoor PM with anti-inflammatory medication use (aspirin, prednisone) and statin use were also considered. We found no significant interaction effect of medication use with fine PM and report only overall effects.
Secondary analysis
An analysis restricted to those with pre-existing heart disease, used a linear mixed effects model to determine the within subject-session effect of a zero-day or one-day lagged 10 μg/m3 increase in fine PM on the log-transformed levels of MCP-1 and ET-1 after adjusting for age, gender, medication use, temperature and relative humidity (as linear and quadratic terms), and the interaction with medication use.
Results
We performed 133 plasma measures of inflammation and thrombosis in 47 individuals with (23) and without (16 COPD and 8 Healthy) cardiovascular disease over 23 study sessions. The overall study population was older (median age 77, range 56–89) and 43% were female (Table 1). The CV and non-CV study populations did not differ by demographic factors (Table 1). The CV population was composed of 6 individuals with heart failure and 17 individuals with ischemic heart disease without overt heart failure. Statin drugs were used in 31% of individuals with heart disease.
Table 2 demonstrates that the range of exposure decreased when restricting to session and within-individual concentration of outdoor PM2.5. Accounting for concentrations measured on 133 subject-days across study sessions, the median concentration of 24-hour averaged outdoor PM2.5 was 7.7 μg/m3 (range 1.3–33.9). Restricting exposure to within the 23 study sessions, the within session median 24-hour averaged outdoor PM concentration was 6.4 μg/m3 (range 0.7–23.7 μg/m3). Within individual, within session median 24-hour averaged outdoor PM concentration was 4.7 μg/m3(range 0.06–23.7 μg/m3). Only 6 individuals (4 CV and 2 non-CV) experienced an intra-session variation of 24-hour averaged PM2.5 exposure of greater than 15 μg/m3.
Table 3 summarizes our measures of inflammation and thrombosis. These data demonstrate similar thrombotic and inflammatory marker levels in the cardiovascular, pulmonary and healthy subgroups. Interestingly, the individuals with cardiac disease have a median value of CRP [0.20 mg/l] that was within the lowest quintile of CRP distribution in apparently healthy elderly participants in other studies (17). Last, the range of values of CRP, D-dimer and fibrinogen in this study population were consistent with prior results in elderly populations (30).
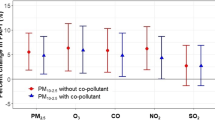
Our analyses found no effect of fine PM at 0-day lag on CRP 1.2 fold-increase [95% CI: 0.9, 1.6], fibrinogen 1.0 fold-increase [95% CI: 1.0, 1.1] or D-dimer 1.1 fold-increase [95% CI: 0.9, 1.2] in those with CV disease after adjusting for RH and temperature. The 1-day lagged analyses in the CV subgroup found similar null results, Table 4. These same models found the same null association between fine PM and these blood measures in the healthy and COPD subgroups, Table 4. Further stratification of these models by covariates known to influence measures of thrombosis including age, gender, anti-inflammatory or anticoagulant medication use, diabetes, active angina or CHF did not modify the null association between fine PM and CRP, fibrinogen and D-dimer levels in the CV, COPD or healthy subgroups, data not shown.
Moreover, using these same models, we found no effect from a 1-ppb increase in either 0-day or 1-day lagged 24-hour average NO2 or a 1-ppm increase in 0-day or 1-day lagged 24-hour average CO level on inflammatory or thrombotic measures in the CV, COPD or healthy subgroups, data not shown.
Our final model did not find a significant effect of a same day 10 ug/m3 increase in fine PM on measures of CRP 1.21 fold-rise [95% CI: 0.86, 1.70], fibrinogen 1.02 fold-rise [95% CI: 0.98, 1.06], or D-dimer 1.02 fold-rise [95% CI: 0.88, 1.17] in individuals with pre-existing CV disease (Table 5). These same models found no change in these blood markers in the COPD or healthy subgroups, (Table 5). Moreover, stratifying by statin use did not modify the absence of association between 0-day or 1-day lagged increased PM and levels of CRP or fibrinogen in CV, COPD or healthy subgroups, data not shown.
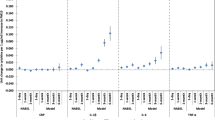
We analyzed PM effect on cytokine levels in 21 individuals with known cardiac disease by pairing 59 repeated-measures of endothelin-1, IL-6 and IL-6 receptor, TNF-α and TNF-α receptors [p55, p75], and MCP-1 to outdoor residence level measures of PM. The median level of MCP-1 was 156 pg/ml (range: 66–647 pg/ml) and the median level of endothelin-1 was 3.6 pg/ml (range: 1.5–6.6 pg/ml). We were unable to assess the effect of PM on levels of TNF-α and IL-6 as most values were below the limit of detection of our assays, which were 2.0 pg/ml and 0.3 pg/ml, respectively.
Our analyses found that a 10 μg/m3 increase in zero-day outdoor PM was associated with a 1.3 fold increase [95% CI: 1.1, 1.7] in the level of MCP-1 in these individuals after controlling for age, gender, RH, temperature and medication use (Table 6). This effect was not evident at the 1-day lag exposure 1.0 [95% CI: 0.9, 1.3]. A 10 μg/m3 increase in PM was not associated with a significant increase in ET-1 levels at the 0-day lagged exposure 1.0 [95% CI: 0.8, 1.2] and 1-day lagged exposures 1.1 [95% CI: 0.9, 1.2] (Table 6). The use of statin medications did not modify the association between the same day fine PM levels and levels of MCP-1 or ET-1.
Discussion
Our study was unable to find consistent associations between increased PM2.5 levels and elevations in blood indices of inflammation or thrombosis. Our finding of an increased MCP-1 level from a 10 ug/m3 increase in fine PM should be interpreted with caution given the multiple analyses conducted in this project.
Although in vitro and animal studies support an inflammatory mechanism of PM effect [31–34], it is possible that PM exerts cardiac effect through direct interaction with the heart and vascular endothelium [35] or through neurogenic mechanisms [15, 36]. We chose our blood measures to reflect the production of acute-phase proteins (CRP and fibrinogen) and circulating inflammatory mediators (cytokines) that characterize the systemic inflammatory response. Therefore, our null results likely reflect the small variation in PM2.5 exposure over the study sessions; inadequate control for personal and medication effects on blood measures; and within-subject physiologic variability of these blood markers.
Small excursions in fine PM levels may not result in appreciable changes in blood measures of inflammation or thrombosis even in susceptible individuals. Our null findings for IL-6, CRP and fibrinogen are consistent with a repeated blood measures study in 108 elderly individuals performed over an 18-month interval by Seaton that only found consistent increases in red blood cell indices (packed cell volume) from the multiple blood measures of inflammation and thrombosis [24]. Our results are also in agreement with controlled exposure studies to ambient PM in healthy volunteers that find no effect of PM on multiple blood markers of inflammation and thrombosis with the exception of fibrinogen. Our results contrast with results from a cohort study of 631 middle-age men in Germany' that found a greater than 2-fold risk of CRP level>99% (10.8 mg/l) from a 5-day average 26 ug/m3 increase in total suspended particles (TSP)[21]. Due to differences in exposure measures (3-day and 5-day moving averages) and analytic method in this study, it is difficult to make a direct comparison of relative effect of PM between studies. Our results are consistent with a PM effect on CRP between a 20 percent decline to a 70 percent increase in blood measure.
The absence of PM effect on blood markers of inflammation and thrombosis at exposure levels of 50–120 ug/m3 PM2.5 in both healthy and asthmatic young volunteers suggests that an inflammatory effect of fine PM may be limited to susceptible populations [14]. Despite their underlying medical conditions, our subjects did not generally have elevated levels of inflammatory measures over the study. This may suggests that our small sample of elderly individuals are not those at greatest risk of PM effect. Epidemiological studies suggest that acute bronchitis, and pneumonia potentiate the cardiac effect of PM in individuals with underlying cardiovascular and pulmonary disease [37]. The mechanism behind the augmentation of PM effect is unclear, but may be explained by changes in transcription of pro-inflammatory genes secondary to the acute infection. Moreover, we speculate that the null results could reflect differences in genetic determinants of susceptibility to PM. Individuals with GSTM1 null and GSTP1 1/1 genotypes have demonstrated increased sensitivity to diesel particulate matter and environmental tobacco smoke suggesting that common genetic variants may influence susceptibility to PM [38]. Unfortunately, our small sample size does not permit further gene-environment analyses as a source of the null results.
The inherent physiologic variability of our inflammatory and thrombotic measures may outweigh the small effects from PM even after restricting our change in blood measure to a within-person, within-session effect. We may have inadequately controlled for disease-related (silent ischemia, CHF and COPD exacerbations, and medication use) and non-disease related factors (stress, depression) that are known to transiently increase the levels of inflammatory and thrombotic markers independently of PM effect.
Last, the higher fraction of secondary aerosols rich in sulfates and transition metals composing PM in the European studies may account for the difference in effect of PM on inflammation and thrombosis between the studies.
Our study had several strengths that add to the validity of results. It was performed in an elderly population with and without cardiac and respiratory disease. Our intensive residential level exposure monitoring potentially decreased exposure misclassification. We controlled for diurnal variation in inflammatory and thrombotic markers by performing blood measures at the same time in each individual.
Conclusion
Our small study was unable to find a pro-inflammatory or pro-thrombotic effect of fine PM at low ambient levels. As the mechanism of PM effect on cardiovascular function remains unknown, we encourage performance of systemic measures of inflammation, thrombosis and oxidative stress in larger panel studies of susceptible populations and in controlled exposure studies to ambient PM in elderly individuals with and without cardiac and respiratory disease.
References
Dockery DW, Pope CA, Xu X, Spengler JD, Ware JH, Fay ME, Ferris BG, Speizer FE: An association between air pollution and mortality in six U.S. cities. N Engl J Med. 1993, 329 (24): 1753-9. 10.1056/NEJM199312093292401.
Le Tertre A, Medina S, Samoli E, Forsberg B, Michelozzi P, Boumghar A, Vonk JM, Bellini A, Atkinson R, Ayres JG, Sunyer J, Schwartz J, Katsouyanni K: Short-term effects of particulate air pollution on cardiovascular diseases in eight European cities. J Epidemiol Community Health. 2002, 56 (10): 773-9. 10.1136/jech.56.10.773.
Samet JM, Zeger SL, Dominici F, Curriero F, Coursac I, Dockery DW, Schwartz J, Zanobetti A: The National Morbidity, Mortality, and Air Pollution Study. Part II: Morbidity and mortality from air pollution in the United States. Res Rep Health Eff Inst. 2000, 94 (Pt 2): 5-70. discussion 1–9
Samet JM, Dominici F, Curriero FC, Coursac I, Zeger SL: Fine particulate air pollution and mortality in 20 U.S. cities, 1987–1994. N Engl J Med. 2000, 343 (24): 1742-9. 10.1056/NEJM200012143432401.
Peters A, Liu E, Verrier RL: Air pollution and incidence of cardiac arrhythmia. Epidemiology. 2000, 11 (1): 11-7. 10.1097/00001648-200001000-00005.
Peters A, Dockery DW, Muller JE, Mittleman MA: Increased particulate air pollution and the triggering of myocardial infarction. Circulation. 2001, 103 (23): 2810-5.
D'Ippoliti D, Forastiere F, Ancona C: Air pollution and myocardial infarction in Rome: a case-crossover analysis. Epidemiology. 2003, 14 (5): 528-35. 10.1097/01.ede.0000082046.22919.72.
Ghio AJ, Devlin RB: Inflammatory lung injury after bronchial instillation of air pollution particles. Am J Respir Crit Care Med. 2001, 164 (4): 704-8.
Godleski JJ, Verrier RL, Koutrakis P, Catalano P, Coull B, Reinisch U, Lovett EG, Lawrence J, Murthy GG, Clarke RW, Nearing BD, Killingsworth C: Mechanisms of morbidity and mortality from exposure to ambient air particles. Res Rep Health Eff Inst. 2000, 5-88. discussion 9–103, 91
Li XY, Gilmour PS, Donaldson K, MacNee W: Free radical activity and pro-inflammatory effects of particulate air pollution (PM10) in vivo and in vitro. Thorax. 1996, 51 (12): 1216-22.
Prahalad AK, Inmon J, Dailey LA, Madden MC, Ghio AJ, Gallagher JE: Air pollution particles mediated oxidative DNA base damage in a cell free system and in human airway epithelial cells in relation to particulate metal content and bioreactivity. Chem Res Toxicol. 2001, 14 (7): 879-87. 10.1021/tx010022e.
Kodavanti UP, Moyer CF, Ledbetter AD: Inhaled environmental combustion particles cause myocardial injury in the Wistar Kyoto rat. Toxicol Sci. 2003, 1 (2): 237-45. 10.1093/toxsci/71.2.237.
Holgate ST, Devlin RB, Wilson SJ, Frew AJ: Health effects of acute exposure to air pollution. Part II: Healthy subjects exposed to concentrated ambient particles. Res Rep Health Eff Inst. 2003, 31-50. discussion 1–67, 112
Ghio AJ, Huang YC: Exposure to concentrated ambient particles (CAPs): a review. Inhal Toxicol. 2004, 16 (1): 53-9. 10.1080/08958370490258390.
van Eeden SF, Tan WC, Suwa T: Cytokines involved in the systemic inflammatory response induced by exposure to particulate matter air pollutants (PM(10)). Am J Respir Crit Care Med. 2001, 164 (5): 826-30.
van Eeden SF, Hogg JC: Systemic inflammatory response induced by particulate matter air pollution: the importance of bone-marrow stimulation. J Toxicol Environ Health A. 2002, 65 (20): 1597-613. 10.1080/00984100290071685.
Ridker PM: High-sensitivity C-reactive protein: potential adjunct for global risk assessment in the primary prevention of cardiovascular disease. Circulation. 2001, 103 (13): 1813-8.
Blake GJ, Ridker PM: C-reactive protein and other inflammatory risk markers in acute coronary syndromes. J Am Coll Cardiol. 2003, 41 (4 Suppl S): 37S-42S. 10.1016/S0735-1097(02)02953-4.
Ulrich MM, Alink GM, Kumarathasan P, Vincent R, Boere AJ, Cassee FR: Health effects and time course of particulate matter on the cardiopulmonary system in rats with lung inflammation. J Toxicol Environ Health A. 2002, 65 (20): 1571-95. 10.1080/00984100290071676.
Gardner SY, Lehmann JR, Costa DL: Oil fly ash-induced elevation of plasma fibrinogen levels in rats. Toxicol Sci. 2000, 56 (1): 175-80. 10.1093/toxsci/56.1.175.
Peters A, Frohlich M, Doring A: Particulate air pollution is associated with an acute phase response in men; results from the MONICA-Augsburg Study. Eur Heart J. 2001, 22 (14): 1198-204. 10.1053/euhj.2000.2483.
Pekkanen J, Brunner EJ, Anderson HR, Tiittanen P, Atkinson RW: Daily concentrations of air pollution and plasma fibrinogen in London. Occup Environ Med. 2000, 57 (12): 818-22. 10.1136/oem.57.12.818.
Gong H, Linn WS, Sioutas C, Terrell S, Calrk K, Anderson K, Terrell LL: Controlled exposures of healthy and asthmatic volunteers to concentrated ambient fine particles in Los Angeles. Inhal Toxicol. 2003, 15 (4): 305-25. 10.1080/08958370304455.
Seaton A, Soutar A, Crawford V: Particulate air pollution and the blood. Thorax. 1999, 54 (11): 1027-32.
Liu LJS, Box M, Kalman D: Exposure Assessment of Particulate Matter for Susceptible Populations in Seattle. Environ Health Perspect. 2003, 111 (7): 909-18.
Liu LJS, Slaughter JC, Larson TV: Comparison of light scattering devices and impactors for particulate measurements in indoor, outdoor, and personal environments. Environmental Science & Technology. 2002, 36 (13): 2977-86. 10.1021/es0112644.
Standardization of blood specimen collection procedure for reference values. International Committee for Standardization in Haematology (ICSH). Clin Lab Haematol. 1982, 4 (1): 83-6.
Rothkrantz-Kos S, Bekers O, Gubbels A, Drent M, Schmitz MP, van Dieijen-Visser MP: Evaluation of two new high-sensitivity methods for C-reactive protein. Ann Clin Biochem. 2003, 40 (Pt 4): 398-405. 10.1258/000456303766477057.
Clauss A: [Rapid physiological coagulation method in determination of fibrinogen]. Acta Haematol. 1957, 17 (4): 237-46.
Seaton A, Soutar A, Crawford V: Particulate air pollution and the blood. Thorax. 1999, 54 (11): 1027-32.
Carter JD, Ghio AJ, Samet JM, Devlin RB: Cytokine production by human airway epithelial cells after exposure to an air pollution particle is metal-dependent. Toxicol Appl Pharmacol. 1997, 146 (2): 180-8. 10.1006/taap.1997.8254.
Donaldson K, Stone V, Borm PJ: Oxidative stress and calcium signaling in the adverse effects of environmental particles (PM10). Free Radic Biol Med. 2003, 34 (11): 1369-82. 10.1016/S0891-5849(03)00150-3.
Ghio AJ, Devlin RB: Inflammatory lung injury after bronchial instillation of air pollution particles. Am J Respir Crit Care Med. 2001, 164 (4): 704-8.
Shukla A, Timblin C, BeruBe K: Inhaled particulate matter causes expression of nuclear factor (NF)-kappaB-related genes and oxidant-dependent NF-kappaB activation in vitro. Am J Respir Cell Mol Biol. 2000, 23 (2): 182-7.
Nemmar A, Nemery B, Hoet PH, Vermylen J, Hoylaerts MF: Pulmonary inflammation and thrombogenicity caused by diesel particles in hamsters: role of histamine. Am J Respir Crit Care Med. 2003, 168 (11): 1366-72. 10.1164/rccm.200306-801OC.
Verones B, Oortgiesen M: Neurogenic inflammation and particulate matter (PM) air pollutants. Neurotoxicology. 2001, 22 (6): 795-810. 10.1016/S0161-813X(01)00062-6.
Goldberg MS, Bailar JC, Burnett RT: Identifying subgroups of the general population that may be susceptible to short-term increases in particulate air pollution: a time-series study in Montreal, Quebec. Res Rep Health Eff Inst. 2000, 7-113. discussion 5–20, 97
Gilliland FD, Li YF, Saxon A, Diaz-Sanchez D: Effect of glutathione-S-transferase M1 and P1 genotypes on xenobiotic enhancement of allergic responses: randomised, placebo-controlled crossover study. Lancet. 2004, 363 (9403): 119-25. 10.1016/S0140-6736(03)15262-2.
Acknowledgements
We thank the individuals who participated in this study. This study was funded by the U.S. Environmental Protection Agency under Grant R827355 and by NIEHS Grant K23ES11139.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
JS contributed to the study design, acquisition of data, analysis and interpretation of data and drafting and revision of manuscript. RH and KS contributed to statistical analyses, interpretation of data and revisions of manuscript. CT contributed to study design, interpretation of data and critical revisions of manuscript. SL contributed to the study design, exposure assessment, drafting of the manuscript and critical revisions of manuscript. JQK contributed to study concept, study design, data acquisition and manuscript revision, WC contributed to study design, measurement of blood markers, interpretation of results and manuscript revision. JDK contributed to study design, data interpretation, manuscript preparation and critical revisions of manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Sullivan, J.H., Hubbard, R., Liu, S.LJ. et al. A community study of the effect of particulate matter on blood measures of inflammation and thrombosis in an elderly population. Environ Health 6, 3 (2007). https://doi.org/10.1186/1476-069X-6-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-069X-6-3