Abstract
Aim
The purpose of the present study was to assess the dietary fat intake, glucose, insulin, Homeostasis model assessment for insulin resistance HOMA-IR, and endotoxin levels and correlate them with adipokine serum concentrations in obese adolescents who had been admitted to long-term interdisciplinary weight-loss therapy.
Design
The present study was a longitudinal clinical intervention of interdisciplinary therapy. Adolescents (n = 18, aged 15–19 y) with a body mass index > 95th percentile were admitted and evaluated at baseline and again after 1 year of interdisciplinary therapy. We collected blood samples, and IL-6, adiponectin, and endotoxin concentrations were measured by ELISA. Food intake was measured using 3-day diet records. In addition, we assessed glucose and insulin levels as well as the homeostasis model assessment for insulin resistance (HOMA-IR).
Results
The most important finding from the present investigation was that the long-term interdisciplinary lifestyle therapy decreased dietary fat intake and endotoxin levels and improved HOMA-IR. We observed positive correlations between dietary fat intake and endotoxin levels, insulin levels, and the HOMA-IR. In addition, endotoxin levels showed positive correlations with IL-6 levels, insulin levels and the HOMA-IR. Interestingly, we observed a negative correlation between serum adiponectin and both dietary fat intake and endotoxin levels.
Conclusions
The present results indicate an association between dietary fat intake and endotoxin level, which was highly correlated with a decreased pro-inflammatory state and an improvement in HOMA-IR. In addition, this benefits effect may be associated with an increased adiponectin level, which suggests that the interdisciplinary therapy was effective in improving inflammatory pathways.
Similar content being viewed by others
Introduction
Saturated and trans fatty acids intake leads to inflammation, insulin resistance and a gain in body mass. Systemic low-level inflammation has been suggested to be both a cause and a consequence of comorbidities associated with obesity [1, 2]. Recently, studies have proposed that the microbial ecology in humans could be an important factor in determining energy homeostasis (i.e., obesity, diabetes, and fatty liver) [3–9]. Lipopolysaccharide (LPS), which is also referred to as endotoxin, has been implicated as a potent inducer of inflammation, and LPS increases tumor necrosis factor alpha (TNF-α) and interleukin 6 (IL-6) and reduces adiponectin levels. In normal circumstances, only small amounts of endotoxin cross from the intestinal lumen into systemic circulation, and the absorbed endotoxin is rapidly removed by monocytes, particularly resident Kupffer cells within the liver. Emerging evidence has indicated that chronic elevation of serum endotoxin levels may play a role in insulin-resistant states and obesity [4, 5, 10].
Interestingly, some authors described how physical inactivity leads to the accumulation of visceral fat and the activation of a network of inflammatory pathways that promote the development of insulin resistance, atherosclerosis, obesity, neurodegeneration, and tumor growth (i.e., the development of diseases belonging to the “diseasome of physical inactivity”) [11, 12].
Recently, our group has shown that long-term interdisciplinary lifestyle therapy is effective in controlling the psychological and physiological alterations that are commonly observed in obese patients [13–21]. Despite promising results, few studies have addressed the effects of long-term interdisciplinary intervention on dietary fat intake and endotoxin levels and their correlation with insulin resistance and adipokine levels.
Materials and methods
Population
Fifty-four adolescents were invited to participate in a 1-year-long Interdisciplinary Obesity Program at the Federal University of São Paulo- Paulista Medical School to promote changes in their sedentary lifestyle and nutritional habits. The basic requirements for participation were motivation and high attendance at the therapy sessions. Thirty-nine adolescents participated until the end of the therapy. The main reasons for dropping out in our study were financial and family problems, followed by school and job opportunities. For the present study, we used as exclusion criteria the lost fat mass < 5% at the end of therapy, where we selected 18 obese adolescents who lost more than 5% fat mass (the range was 5.4% to 22.5% fat mass).
Selected 18 obese adolescents were evaluated at baseline and after long-term (1 year) weight loss intervention. The present study was conducted in accordance with the principles of the Declaration of Helsinki and was formally approved by the Institutional Ethical Committee (#0135/04). Informed consent was obtained from all subjects and/or their parents, and the agreement of the adolescents and their families to participate was voluntary.
The ages of the 18 participants ranged from 15–19 years (16.6 ± 1.67 years), and the average body mass index (BMI) was 37.98 ± 4.60 kg/m2 (7 boys and 11 girls). All participants met the inclusion criteria of postpubertal Stage V, based on the Tanner stages [22], and of obesity (BMI > 95th percentile) according to the Centers for Disease Control and Prevention (CDC) reference growth charts. Noninclusion criteria included identifiable genetic, metabolic or endocrine disease or previous drug utilization [23].
Study protocol and medical screening
Subjects were medically screened, and we assessed their pubertal stage and recorded their anthropometric measures (i.e., height, weight, BMI and body composition). The endocrinologist completed a clinical interview, which included questions to determine eligibility based on inclusion and exclusion criteria. Blood samples were collected and analyzed, and an ultrasound (US) was performed. The procedures were scheduled for the same time of day for all subjects to remove any influence of diurnal variations. After the initial screening, obese adolescents started the interdisciplinary weight loss program (described in a later section).
Anthropometric measurements and body composition
Subjects were weighed on a Filizola scale while wearing light clothing and no shoes, and their weight was recorded to the nearest 0.1 kg. Height was measured using a wall-mounted stadiometer (Sanny, model ES 2030) to the nearest 0.5 cm. Body mass index was calculated as body weight (wt) divided by height (h) squared (wt/ht2). Body composition was estimated by plethysmography using the BOD POD body composition system (version 1.69, Life Measurement Instruments, Concord, CA), which is the most advanced technique available for assessing body composition. The patented air displacement plethysmography used by the BOD POD and PEA POD is similar in principle to hydrostatic (or "underwater") weighing. The obvious difference between them is that air is more convenient and comfortable than water, and air displacement plethysmography provides a much simpler and safer testing environment, better reliability and significantly improved repeatability and accuracy [24].
Serum analysis
Blood samples were collected in the outpatient clinic at approximately 0800 h after an overnight fast. Adipokine (IL-6 and adiponectin) concentrations were measured using commercially available ELISA kits from eBioscience, Inc. (San Diego, CA, USA) and R&D Systems (USA) according to the manufacturer’s manuals.
Fasting insulin concentrations were determined using commercially available ELISA kits from Millipore (Millipore Corporate Headquarters: 290 Concord Road, Billerica, MA 01821), and glucose concentrations were determined by an enzymatic method (Labtest®). Homeostasis model assessment for insulin resistance (HOMA-IR) was calculated with assessed values of glucose and insulin.
Measurement of circulating endotoxin levels
Plasma endotoxin was assayed using a chromogenic limulus amebocyte lysate (LAL) test, which is a quantitative test for Gram-negative bacterial endotoxin (Cambrex Corporation, 8830 Biggs Ford Road, Walkersville – USA). Gram-negative bacterial endotoxin catalyzes the activation of a proenzyme in the LAL, and the initial rate of activation is directly determined by the concentration of endotoxin. The activated enzyme catalyzes the splitting of p-nitroaniline (pNA) from the colorless substrate Ac-lle-Glu-Ala-Arg-pNA, and the released pNA was measured photometrically at 405–410 nm following termination of the reaction. The correlation between the absorbance and the endotoxin concentration was linear in the range of 0.1–1.0 EU/ml. For the purposes of this study, all samples were run in duplicate within the same plate; therefore, no interassay variability was observed in this study.
To assess recovery of endotoxin within the assay, known concentrations of recombinant endotoxin (0.25 and 1.00 EU/ml) were added to diluted plasma to determine whether the expected concentration correlated with the actual observed value and whether there were any variations due to reaction with plasma contents. Lyophilized endotoxin (E. coli origin) was used to generate a standard curve with the chromogenic LAL test kit in accordance with the manufacturer's instructions.
Visceral and subcutaneous adiposity measurements
All abdominal ultrasonographic procedures and measurements of visceral and subcutaneous fat tissue were performed by the same physician who was blinded to the subjects’ assignment group. This physician was a specialist in imaging diagnostics using a 3.5-MHz multifrequency transducer (broad band), which reduces the risk of misclassification. The intra-examination coefficient of variation for US was 0.8%.
We took US measurements of intra-abdominal (¨visceral¨) and subcutaneous fat. Ultrasound-determined subcutaneous fat was defined as the distance between the skin and external face of the recto abdominis muscle, and visceral fat was defined as the distance between the internal face of the same muscle and the anterior wall of the aorta. Cutoff points to define visceral obesity by ultrasonographic parameters were based on previous methodological descriptions [25].
Clinical intervention
Dietary program
Energy intake was set at the levels recommended by the dietary reference intake for subjects with low levels of physical activity of the same age and gender following a balanced diet as previously described [20]. No drugs or antioxidants were recommended. Once a week, adolescents had a dietetics lesson, which provided information on the food pyramid, diet record assessment, weight loss diets and miracle diets, food labels, dietetics, fat-free and low-calorie foods, fats (kinds, sources and substitute foods), fast food calories and nutritional composition, good nutritional choices in special occasions, healthy sandwiches, shakes and products to promote weight loss, functional foods and decisions on food choices. All patients received individual nutritional consultation during the intervention program. In addition, a dietitian encouraged the parents to call if they needed extra information.
Exercise program
During the one-year interdisciplinary intervention period, adolescents followed a personalized aerobic training program that included a 60-minute session completed three times each week (180-minute/week) under the supervision of a sports therapist. Each program was developed according to the results of an initial oxygen uptake test for aerobic exercises (cycle-ergometer and treadmill). The intensity was set at a work load corresponding to a ventilatory threshold of 1 (50% to 70% of oxygen uptake test). Adolescents were under heart-rate monitoring during the aerobic sessions. The exercise program was based on the 2009 recommendations of the American College of Sports Medicine [26].
Psychological intervention
Diagnoses of common psychological problems associated with obesity, such as depression, disturbances of body image, anxiety and decreased self-esteem, were established by validated questionnaires. During the interdisciplinary intervention, the adolescents had weekly psychological support group sessions. During these sessions, the adolescents discussed body image; alimentary disorders, including bulimia, anorexia nervosa and binge eating; the signs, symptoms and health consequences of these disorders; the relationship between feelings and food; and family problems, such as alcoholism. Individual psychological therapy was recommended if individuals were found to have nutritional or behavioral problems [16].
Statistical analysis
The data distribution was checked by Bartlett's test for equal variances, and the data are reported as the mean ± SD. Statistical outliers within each treatment group were identified using Grubbs’ test (GraphPad Software) and subsequently removed. All remaining data were analyzed by GraphPad Prism (version 5.00). The differences between groups for all parameters were assessed by a paired Student’s t test. The Pearson correlation coefficient was calculated to assess the relationship between variables, and all analyses were carried out with the significance level set at p < 0.05.
Results
Long-term therapy was effective in reducing body weight (15%), BMI (15%), percent fat (24%), and fat mass (33%). These results are shown in Table 1.
Characteristics of the food intake in obese adolescents are shown in Table 2. Energy intake was reduced 38%, carbohydrate intake was reduced 28%, protein intake was reduced 43%, and fat intake was reduced 47%.
Glucose, insulin, IL-6, adiponectin and endotoxin levels as well as the HOMA-IR are shown in Table 3. Glucose (the range before therapy was 4.38 – 5.66 μU/mL, and the range after therapy was 4.32 – 4.77 μU/mL), insulin (the range before therapy was 7.10 – 23.3 μU/mL, and the range after therapy was 5.00 – 18.9 μU/mL), IL-6 (the range before therapy was 0.97 – 2.22 in Log pg/mL, and the range after therapy was 0.97 – 2.30 Log in pg/mL), adiponectin (the range before therapy was 0.78 – 1.14 Log in ng/mL, and the range after therapy was 0.92 – 1.20 Log in ng/mL), HOMA-IR (the range before therapy was 1.45 – 5.23 μU/mL, and the range after therapy was 1.01 – 3.87 μU/mL), and endotoxin (the range before therapy was 0.112 – 0.394 in Log EU/mL, and the range after therapy was 0.095 – 0.309 in Log EU/mL) were reduced after therapy.
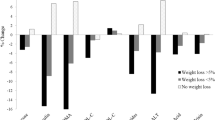
Pearson correlation analyses showed positive correlations between dietary fat intake and endotoxin levels (r = 0.36, p < 0.01), dietary fat diet intake and insulin levels (r = 0.38, p < 0.05), and dietary fat intake and HOMA-IR (r = 0.41, p < 0.04). In addition, there was a negative correlation between dietary fat intake and adiponectin (r = −0.42, p < 0.01) (Figure 1A-D).
We also observed positive correlations between endotoxin and IL-6 levels (r = 0.35, p < 0.03), endotoxin and insulin levels (r = 0.36, p < 0.05), and endotoxin levels and HOMA (r = 0.35, p < 0.05). Interestingly, we observed a negative correlation between endotoxin and adiponectin levels (r = −0.28, p < 0.06) (Figure 2A-D).
Discussion
The present study showed that long-term therapy was effective in reducing dietary fat intake and endotoxin levels. In addition, these data were positively correlated with improvements in insulin resistance in obese adolescents.
The chronic endotoxemia, have promoted glucose intolerance and hepatic insulin resistance, suggesting its role as a link between innate immunity, inflammation, and insulin resistance [27].
Decreased endotoxin levels have been found with consumption of a low-fat diet compared with a high-fat diet [28–30]. In addition, the type of fatty acid in the diet could have important effects on endotoxinemia. Recently, several studies have shown that omega-3 (ω-3) fatty acids, particularly eicosapentaenoic acid (EPA), reduces endotoxin and pro-inflammatory cytokine concentrations [29, 30]. Moreover, Oz et al. [31] demonstrated that a diet rich in EPA, docosahexaenoic acid (DHA), and prebiotic fructooligosaccharides (FOS) protects against LPS-induced systemic inflammatory responses. In contrast to the present study, Al-Attas et al. [3] showed that a diet-controlled program in diabetic individuals did not significantly decrease endotoxin levels compared with individuals who only received insulin. Interestingly, herbs used in food dishes reduce the production of LPS and pro-inflammatory cytokines [32]. In the present study, we observed that interdisciplinary therapy was able to decrease the fat intake, which least in part, was sufficient to reduce endotoxin concentrations and insulin resistance. The reduced endotoxin levels to be related with recovery metabolism and inflammation status that leads to anti-inflammatory status.
The present study found a positive correlation between endotoxin and both pro-inflammatory cytokines (especially, IL-6) and insulin resistance. After interdisciplinary therapy, endotoxinemia, pro-inflammatory status and insulin resistance were decreased. These results showed the importance of making lifestyle changes (i.e., nutritional modification) to reduce the pro-inflammatory state in obese individuals. We have previously shown that long-term therapy is effective in reducing body fat (especially visceral fat), TNF-α and IL-6 and increasing IL-10 and adiponectin. In addition, we observed a positive correlation between pro-inflammatory cytokines (IL-6 and TNF-α levels) and visceral fat [20]. In addition, we can suggested a significant improvement of inflammatory profile once adiponectin, the anti-inflammatory adipokine, increased significantly after the long-term intervention (12%) and reduction of HOMA-IR, an index that present association to inflammatory pathways, such as increase of IL-6 and TNF-alpha.
Creely et al. [5] found that circulating serum endotoxin was higher in type 2 diabetes mellitus (T2DM) patients than in lean healthy subjects, and endotoxin can activate the innate immune pathway in isolated abdominal adipocytes to stimulate secretion of pro-inflammatory cytokines. Creely et al. [5] suggested that the subclinical inflammation seen in type 2 diabetes patients was related to the increase in endotoxin. Mehta et al. [33] observed that endotoxemia (3 ng/kg intravenous bolus in healthy adults) induced an elevation in TNF-α and systemic insulin resistance in humans. Furthermore, insulin resistance measured at 24 h post-LPS was preceded by specific modulation of adipose inflammatory and insulin signaling pathways. Leuwer et al. [34] have shown that endotoxemia leads to major increases in inflammatory adipokine (TNF-α, IL-6, and MCP-1) gene expression in white adipose tissue in mice. In addition, previous studies in human adipose tissue have shown that obesity and T2DM induce upregulation of inflammatory genes [5]. These results are in agreement with the present study in which endotoxin showed a close correlation with IL-6, which was reduced after 1 year of interdisciplinary therapy.
Although we did not directly analyze the effect of exercise, we cannot exclude that the exercise protocol used in the present study contributed to the beneficial effects of the interdisciplinary therapy in obese adolescents. Many studies [11, 35–37] have actually demonstrated the benefits of exercise training, which induces an anti-inflammatory state in obese rat and human models. Bradley et al. [36] suggested that voluntary exercise in diet-induced obese mice reduced adiposity despite continued consumption of a high-fat diet. In addition, exercise normalized insulin sensitivity and decreased adipose tissue inflammation (reduced IKK-β gene expression) in these obese mice. These data demonstrated the positive role of exercise training in preventing the development of several diseases, including obesity, diabetes, and fatty liver.
Starkie et al. [38] demonstrated that an intravenous infusion of endotoxin induced a two to threefold increase in the plasma TNF-α level. When human subjects adopted an acute exercise protocol (75% VO2max), however, the production of TNF-α elicited by low-grade endotoxemia was inhibited. Similarly, Chen et al. [39] found that chronically exercised rats exhibited minor pathological changes in the heart, liver, and lung after endotoxemia. In addition, Lira et al. [40] observed that a lifestyle change associated with high-intensity, high-volume exercise induced favorable changes in chronic low-grade inflammatory markers and may reduce the risk for obesity, diabetes and cardiovascular diseases.
Although the small number of participants could be a limitation of the present study, the results contribute to the understanding of the mechanisms linking insulin resistance, adiponectinemia in obesity and endotoxemia to the inflammatory state. In addition, the present study highlights the importance of lifestyle interdisciplinary therapy intervention as clinical practice for obesity treatment.
In summary, the present study demonstrated an important association between dietary fat intake and endotoxin level, which reduced significantly after the long-term intervention. Indeed, based on these data, we can hypothesize a link between dietary fat intake, insulin resistance, endotoxin and inflammatory pathways. Taken together, these results suggest that interdisciplinary therapy is effective in decreasing inflammatory markers related to obesity.
References
Bruunsgaard H: Physical activity and modulation of systemic low-level inflammation. J Leukoc Biol. 2005, 78: 819-835. 10.1189/jlb.0505247.
Pimentel GD, Lira FS, Rosa JC, Oliveira JL, Losinskas-Hachul AC, Souza GI, Das Gracas TCM, Santos RV, De Mello MT, Tufik S, et al: Intake of trans fatty acids during gestation and lactation leads to hypothalamic inflammation via TLR4/NFkappaBp65 signaling in adult offspring. J Nutr Biochem. 2012, 23: 265-271. 10.1016/j.jnutbio.2010.12.003.
Ley RE, Backhed F, Turnbaugh P, Lozupone CA, Knight RD, Gordon JI: Obesity alters gut microbial ecology. Proc Natl Acad Sci USA. 2005, 102: 11070-11075. 10.1073/pnas.0504978102.
Al-Attas OS, Al-Daghri NM, Al-Rubeaan K, da Silva NF, Sabico SL, Kumar S, McTernan PG, Harte AL: Changes in endotoxin levels in T2DM subjects on anti-diabetic therapies. Cardiovasc Diabetol. 2009, 8: 20-10.1186/1475-2840-8-20.
Creely SJ, McTernan PG, Kusminski CM, Fisher M, Da Silva NF, Khanolkar M, Evans M, Harte AL, Kumar S: Lipopolysaccharide activates an innate immune system response in human adipose tissue in obesity and type 2 diabetes. Am J Physiol Endocrinol Metab. 2007, 292: E740-E747.
Rinaldi AE, Pimentel GD, Pereira AF, Gabriel GF, Moreto F, Burini RC: Metabolic syndrome in overweight children from the city of Botucatu - Sao Paulo State - Brazil: agreement among six diagnostic criteria. Diabetol Metab Syndr. 2010, 2: 39-10.1186/1758-5996-2-39.
Pimentel GD, Portero-McLellan KC, Oliveira EP, Spada AP, Oshiiwa M, Zemdegs JC, Barbalho SM: Long-term nutrition education reduces several risk factors for type 2 diabetes mellitus in Brazilians with impaired glucose tolerance. Nutr Res. 2010, 30: 186-190. 10.1016/j.nutres.2010.03.003.
Pimentel GD, Arimura ST, de Moura BM, Silva ME, de Sousa MV: Short-term nutritional counseling reduces body mass index, waist circumference, triceps skinfold and triglycerides in women with metabolic syndrome. Diabetol Metab Syndr. 2010, 2: 13-10.1186/1758-5996-2-13.
Pimentel GD, Zemdegs JC, Theodoro JA, Mota JF: Does long-term coffee intake reduce type 2 diabetes mellitus risk?. Diabetol Metab Syndr. 2009, 1: 6-10.1186/1758-5996-1-6.
Pimentel GD, Micheletti TO, Pace F, Rosa JC, Santos RV, Lira FS: Gut-central nervous system axis is a target for nutritional therapies. Nutr J. 2012, 11: 22-10.1186/1475-2891-11-22.
Pedersen BK: The diseasome of physical inactivity–and the role of myokines in muscle–fat cross talk. J Physiol. 2009, 587: 5559-5568. 10.1113/jphysiol.2009.179515.
Ropelle ER, Flores MB, Cintra DE, Rocha GZ, Pauli JR, Morari J, de Souza CT, Moraes JC, Prada PO, Guadagnini D, et al: IL-6 and IL-10 anti-inflammatory activity links exercise to hypothalamic insulin and leptin sensitivity through IKKbeta and ER stress inhibition. PLoS Biol. 2010, 8: e1000465-10.1371/journal.pbio.1000465.
Tock L, Prado WL, Caranti DA, Cristofalo DM, Lederman H, Fisberg M, Siqueira KO, Stella SG, Antunes HK, Cintra IP, et al: Nonalcoholic fatty liver disease decrease in obese adolescents after multidisciplinary therapy. Eur J Gastroenterol Hepatol. 2006, 18: 1241-1245. 10.1097/01.meg.0000243872.86949.95.
Caranti DA, de Mello MT, Prado WL, Tock L, Siqueira KO, de Piano A, Lofrano MC, Cristofalo DM, Lederman H, Tufik S, Damaso AR: Short- and long-term beneficial effects of a multidisciplinary therapy for the control of metabolic syndrome in obese adolescents. Metabolism. 2007, 56: 1293-1300. 10.1016/j.metabol.2007.05.004.
Carnier J, Lofrano MC, Prado WL, Caranti DA, de Piano A, Tock L, Do Nascimento CM, Oyama LM, Mello MT, Tufik S, Damaso AR: Hormonal alteration in obese adolescents with eating disorder: effects of multidisciplinary therapy. Horm Res. 2008, 70: 79-84. 10.1159/000139148.
Lofrano-Prado MC, Antunes HK, Do Prado WL, De Piano A, Caranti DA, Tock L, Carnier J, Tufik S, De Mello MT, Damaso AR, Lofrano-Prado MC, Antunes HK, Do Prado WL, De Piano A, Caranti DA, Tock L, Carnier J, Tufik S, De Mello MT, Damaso AR: Quality of life in Brazilian obese adolescents: effects of a long-term multidisciplinary lifestyle therapy. Health Qual Life Outcomes. 2009, 7: 61-10.1186/1477-7525-7-61.
De Piano A, Tock L, Carnier J, Oyama LM, Oller Do Nascimento CM, Martinz AC, Foschini D, Sanches PL, Ernandes RM, De Mello MT, et al: Negative correlation between neuropeptide Y/agouti-related protein concentration and adiponectinemia in nonalcoholic fatty liver disease obese adolescents submitted to a long-term interdisciplinary therapy. Metabolism. 2010, 59: 613-619. 10.1016/j.metabol.2009.09.003.
Carnier J, De Piano A, De Lima Sanches P, Tock L, Do Nascimento CM, Oyama LM, Correa FA, Ernandes RH, Lederman H, De Mello MT, et al: The role of orexigenic and anorexigenic factors in an interdisciplinary weight loss therapy for obese adolescents with symptoms of eating disorders. Int J Clin Pract. 2010, 64: 784-790. 10.1111/j.1742-1241.2009.02306.x.
De Lima Sanches P, De Mello MT, Elias N, Fonseca FA, De Piano A, Carnier J, Oyama LM, Tock L, Tufik S, Damaso AR: Improvement in HOMA-IR is an independent predictor of reduced carotid intima-media thickness in obese adolescents participating in an interdisciplinary weight-loss program. Hypertens Res. 2011, 34: 232-238. 10.1038/hr.2010.225.
Lira FS, Rosa JC, Dos Santos RV, Venancio DP, Carnier J, Sanches Pde L, Do Nascimento CM, De Piano A, Tock L, Tufik S, et al: Visceral fat decreased by long-term interdisciplinary lifestyle therapy correlated positively with interleukin-6 and tumor necrosis factor-alpha and negatively with adiponectin levels in obese adolescents. Metabolism. 2011, 60: 359-365. 10.1016/j.metabol.2010.02.017.
De Mello MT, De Piano A, Carnier J, Sanches Pde L, Correa FA, Tock L, Ernandes RM, Tufik S, Damaso AR: Long-term effects of aerobic plus resistance training on the metabolic syndrome and adiponectinemia in obese adolescents. J Clin Hypertens (Greenwich). 2011, 13: 343-350. 10.1111/j.1751-7176.2010.00388.x.
Tanner JM, Whitehouse RH: Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976, 51: 170-179. 10.1136/adc.51.3.170.
Nobili V, Marcellini M, Devito R, Ciampalini P, Piemonte F, Comparcola D, Sartorelli MR, Angulo P: NAFLD in children: a prospective clinical-pathological study and effect of lifestyle advice. Hepatology. 2006, 44: 458-465. 10.1002/hep.21262.
Fields DA, Goran MI: Body composition techniques and the four-compartment model in children. J Appl Physiol. 2000, 89: 613-620.
Ribeiro-Filho FF, Faria AN, Azjen S, Zanella MT, Ferreira SR: Methods of estimation of visceral fat: advantages of ultrasonography. Obes Res. 2003, 11: 1488-1494. 10.1038/oby.2003.199.
Bennett GG, Wolin KY, Puleo EM, Masse LC, Atienza AA: Awareness of national physical activity recommendations for health promotion among US adults. Med Sci Sports Exerc. 2009, 41: 1849-1855. 10.1249/MSS.0b013e3181a52100.
Park HK, Qatanani M, Briggs ER, Ahima RS, Lazar MA: Inflammatory induction of human resistin causes insulin resistance in endotoxemic mice. Diabetes. 2011, 60: 775-783. 10.2337/db10-1416.
Amar J, Burcelin R, Ruidavets JB, Cani PD, Fauvel J, Alessi MC, Chamontin B, Ferrieres J: Energy intake is associated with endotoxemia in apparently healthy men. Am J Clin Nutr. 2008, 87: 1219-1223.
Calder PC: Fatty acids and immune function: relevance to inflammatory bowel diseases. Int Rev Immunol. 2009, 28: 506-534. 10.3109/08830180903197480.
Supinski GS, Vanags J, Callahan LA: Eicosapentaenoic acid preserves diaphragm force generation following endotoxin administration. Crit Care. 2010, 14: R35-10.1186/cc8913.
Oz HS, Chen TS, Neuman M: Nutrition intervention: a strategy against systemic inflammatory syndrome. JPEN J Parenter Enteral Nutr. 2009, 33: 380-389. 10.1177/0148607108327194.
Tuntipopipat S, Muangnoi C, Failla ML: Anti-inflammatory activities of extracts of Thai spices and herbs with lipopolysaccharide-activated RAW 264.7 murine macrophages. J Med Food. 2009, 12: 1213-1220. 10.1089/jmf.2009.1118.
Mehta NN, McGillicuddy FC, Anderson PD, Hinkle CC, Shah R, Pruscino L, Tabita-Martinez J, Sellers KF, Rickels MR, Reilly MP: Experimental endotoxemia induces adipose inflammation and insulin resistance in humans. Diabetes. 2010, 59: 172-181. 10.2337/db09-0367.
Leuwer M, Welters I, Marx G, Rushton A, Bao H, Hunter L, Trayhurn P: Endotoxaemia leads to major increases in inflammatory adipokine gene expression in white adipose tissue of mice. Pflugers Arch. 2009, 457: 731-741. 10.1007/s00424-008-0564-8.
Beavers KM, Brinkley TE, Nicklas BJ: Effect of exercise training on chronic inflammation. Clin Chim Acta. 2010, 411: 785-793. 10.1016/j.cca.2010.02.069.
Bradley RL, Jeon JY, Liu FF, Maratos-Flier E: Voluntary exercise improves insulin sensitivity and adipose tissue inflammation in diet-induced obese mice. Am J Physiol Endocrinol Metab. 2008, 295: E586-E594. 10.1152/ajpendo.00309.2007.
Lira FS, Rosa JC, Yamashita AS, Koyama CH, Batista ML, Seelaender M: Endurance training induces depot-specific changes in IL-10/TNF-alpha ratio in rat adipose tissue. Cytokine. 2009, 45: 80-85. 10.1016/j.cyto.2008.10.018.
Starkie R, Ostrowski SR, Jauffred S, Febbraio M, Pedersen BK: Exercise and IL-6 infusion inhibit endotoxin-induced TNF-alpha production in humans. FASEB J. 2003, 17: 884-886.
Chen HI, Hsieh SY, Yang FL, Hsu YH, Lin CC: Exercise training attenuates septic responses in conscious rats. Med Sci Sports Exerc. 2007, 39: 435-442. 10.1249/mss.0b013e31802d11c8.
Lira FS, Rosa JC, Pimentel GD, Souza HA, Caperuto EC, Carnevali LC, Seelaender M, Damaso AR, Oyama LM, De Mello MT, Santos RV: Endotoxin levels correlate positively with a sedentary lifestyle and negatively with highly trained subjects. Lipids Health Dis. 2010, 9: 82-10.1186/1476-511X-9-82.
Acknowledgements
FINANCIAL SUPPORT - FAPESP, Brazil, Processo nº 2011/50356-0 and 2011/50414-0.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
FSL, JCR, GDP participated of sample collected, assess samples, design of the study and performed the statistical analysis, and writing of paper, RVS, ST and MS helped carry out design of the study, JC, PLS, AP and LT participated of data collection and analysis, MTM, CMON, LMO, CTS and ARD performed the design of the study and discussion of paper. All authors read and approved the final manuscript and apply to add the new author.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lira, F.S., Rosa, J.C., Pimentel, G.D. et al. Long-term interdisciplinary therapy reduces endotoxin level and insulin resistance in obese adolescents. Nutr J 11, 74 (2012). https://doi.org/10.1186/1475-2891-11-74
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2891-11-74