Abstract
Background
In order to use a combination of ivermectin and albendazole for the elimination of lymphatic filariasis, it is important to assess the potential risk of increased adverse events in individuals infected with both lymphatic filariasis and onchocerciasis. We compared the safety and efficacy of albendazole (400 mg) in combination with ivermectin (150 micrograms/kg), for the treatment of co-infections of Wuchereria bancrofti and Onchocerca volvulus with single infection of W. bancrofti.
Methods
The safety study on co-infections was a crossover, double blind design, while for the single infection of bancroftian filariasis an open design comparing two treatments was used. For co-infection, one group was allocated a single dose of ivermectin (150 micrograms/kg) plus albendazole (400 mg) (Group A). The other group received placebo (Group B). Five days later the treatment regime was reversed, with the Group A receiving placebo and Group B receiving treatment. For the single bancroftian filariasis infection, one group received a single dose of albendazole (400 mg) plus ivermectin (150 μg/kg) (Group C) while the other group received a single dose of albendazole (400 mg) alone (Group D). Blood and skin specimens were collected on admission day, day 0, and on days 2, 3, and 7 to assess drug safety and efficacy. Thereafter, blood and skin specimens were collected during the 12 months follow up for the assessment of drug efficacy. Study individuals were clinically monitored every six hours during the first 48 hours following treatment, and routine clinical examinations were performed during the hospitalisation period and follow-up.
Results
In individuals co-infected with bancroftian filariasis and onchocerciasis, treatment with ivermectin and albendazole was safe and tolerable. Physiological indices showed no differences between groups with co-infection (W. bancrofti and O. volvulus) or single infection (W. bancrofti). The frequency of adverse events in co-infected individuals was 63% (5/8, Group A, albendazole + ivermectin) and 57% (4/7, Group B, placebo) and of mild or moderate intensity. In single W. bancrofti infection the frequency of adverse events was 50% (6/12, Group C, albendazole + ivermectin) and 38% (5/13, Group D, albendazole) and of a similar intensity to those experienced with co-infection. There were no differences in adverse events between treatment groups. There was no significant difference in the reduction of microfilaraemia following treatment with albendazole and ivermectin in groups with single or co-infection.
Conclusion
Our findings suggest that ivermectin plus albendazole is a safe and tolerable treatment for co-infection of bancroftian filariasis and onchocerciasis.
Similar content being viewed by others
Background
Bancroftian filariasis and onchocerciasis are important causes of clinical disease and progressive disability in the tropics and subtropics, affecting more than 120 and 17.6 million people respectively [1, 2]. In Tanzania, more than 10 million people live in areas endemic for bancroftian filariasis, and of these 11.7% are affected by the infection [3]. Eleven foci for onchocerciasis have been established in Tanzania in which it is estimated 2 million people are at risk and of these 400,000 are already infected [4]. Studies conducted in Tanzania showed that bancroftian filariasis is prevalent along the entire coastal belt of the Indian Ocean, its islands, and in the regions around the Great Lake [5]. The clinical manifestations of the disease are hydrocoele, lymphoedema, orchitis, adenolymphangitis and elephantiasis. The acute and chronic pathologies caused by these diseases impose a significant impediment to socio-economic development [6, 7].
Chemotherapy is now considered as the most cost-effective tool to potentially interrupt transmission [8]. The most common strategy adopted is mass treatment of populations with either diethylcarbamazine (DEC) or ivermectin. DEC mass distribution has been the main strategy for lymphatic filariasis control programmes for many years in endemic areas based on annual or semi-annual administration [2]. However, DEC is contraindicated in individuals with onchocerciasis because of potentially severe treatment adverse reaction [1]. The severity of such reactions is reduced in ivermectin, which is considered safe and effective against either disease [1]. Recently albendazole has been introduced for use in combined chemotherapy with either ivermectin or DEC as the treatment regime for the global elimination of lymphatic filariasis [8]. Albendazole combined with either ivermectin or DEC has been demonstrated to effectively clear bancroftian microfilaraemia [9]. The new anti-filarial drug combinations are expected to improve compliance, coverage and reduce costs by introducing simple efficient drug delivery and distribution methods.
In Tanzania, albendazole and ivermectin have been adopted as the combination treatment for the community-based control of bancroftian filariasis. In order to determine whether this treatment can be used safely and effectively in areas of co-endemicity with onchocerciasis, we examined the safety, tolerability, and efficacy of albendazole with ivermectin for the treatment of individuals with concurrent infections of bancroftian filariasis and onchocerciasis and single infection of bancroftian filariasis.
Methods
Patients
The Ethics Committee of the National Institute for Medical Research, Tanzania, the Research Ethics Committee of the Liverpool School of Tropical Medicine, UK and the Ethics committee of the World Health Organisation (WHO) approved the study. The clinical trial was conducted from April 1998 to May 1999 in Muheza district, Tanga, northeastern Tanzania, where bancroftian filariasis and onchocerciasis co-exist. Candidates for the trial were selected from rural communities of Maramba "A" and Mhinduro, which is the first time the co-existence of both diseases has been reported in the Western Usambara Mountains. The majority of the inhabitants are Moslems and their main source of income is farming, petty trade and animal husbandry. The villages have not previously been included in control activities against bancroftian filariasis, onchocerciasis or other helminths.
Fifteen males aged between 15 and 55 years with co-infection of bancroftian filariasis and onchocerciasis and 25 (11 male and 14 female [age range 15–55]) for single infection of bancroftian filariasis were recruited (see Trial Profile, Figure 1). Individuals were screened for inclusion into the study by finger-prick blood samples (100 μl) for bancroftian filariasis and by skin snip for onchocerciasis. Clinical evaluation was conducted at Bombo Regional Hospital, Tanga. The inclusion criteria for admission into this study included; apparently healthy individuals aged between 15 and 55 years, able to give oral consent to participate, weighing more than 31 kilograms, have no papular onchodermatitis and itching, with no history of taking herbal medication, anthelminthic or anti-filarial drugs three months prior to recruitment, microfilaria counts of ≥ 100 mf/ml in Wuchereria bancrofti, and/or Onchocerca volvulus microfilaria counts of ≥ 5 mf/skin snip. Women were excluded from the co-infection group due to the risk of inadvertent pregnancy and the potential effects of unforeseen adverse events on the foetus. In the single infection of bancroftian filariasis women selected for inclusion were tested for pregnancy.
Clinical examination and laboratory analysis
On admission to the hospital a full medical history was obtained and a physical examination was carried out prior to specimen collection. 7 ml of venous blood was collected into tubes containing ethylenediaminetetraacetic acid (EDTA) as an anti-coagulant between 21:00 and 01:00 h. 1 ml of anti-coagulated blood was thoroughly mixed with 4 ml of normal saline. The suspension was then passed through a membrane filter (3 μm pore; Nuclepore) and the trapped microfilariae (mf) counted. The pre-treatment mf count was calculated in each case by averaging counts of two samples, one-collected three days before admission and the other on day 0 before drug administration at the hospital. The remaining blood specimens were used for biochemical tests to estimate bilirubin, aspartate amino transferase (AST), and creatinine levels and examination of haematological indices, including total leucocyte count, differential white blood cell count and haemoglobin. Skin snips were obtained from the right and left iliac crests using a Walser corneoscleral biopsy punch after disinfecting the site with 70% alcohol. Skin snips were incubated in 0.9% saline overnight. The following day, specimens were microscopically examined for parasite identification and quantification. Blood specimens and skin snips were collected on admission day, Day 0, and on Day 2, 3, and 7 to assess drug safety and efficacy. Thereafter, blood specimens and skin snips were collected during the 12 months follow up for the assessment of drug efficacy. Study individuals were clinically monitored every six hours during the first 48 hours following treatment, and routine clinical examinations were performed during the hospitalisation period and follow-up. Clinical adverse reactions were monitored and assessed by a scoring method. The individuals were assigned scores according to the intensity of adverse reaction, thus a score of 0 = no alteration, no adverse reaction was reported and individuals could perform their usual daily tasks, 1 = mild alteration, mild adverse reaction recorded which individuals are aware of and can easily tolerate and continue with usual daily tasks, 2 = moderate alteration, moderate adverse reaction which can cause discomfort, interfere with usual daily tasks and require rest and/or analgesic before continuing with usual tasks, and 3 = severe alteration, severe reactions which would prevent usual daily tasks and require hospitalisation.
Study protocol
In each sub-study individuals were randomly allocated to one of the treatment regimens. The study on co-infections was a crossover, double blind design, while the study on single infection of W. bancrofti was an open comparison of the two treatments (see trial profile Figure 1). For co-infection one group was allocated a single dose of ivermectin (150 μg/kg) plus albendazole (400 mg) (Group A). The other group received 6 saccharine tablets as a placebo (Group B). Five days later the treatment regime was administered in reverse, with the Group A receiving placebo and Group B receiving treatment. For the bancroftian filariasis infection, one group received a single dose of albendazole (400 mg) plus ivermectin (150 μg/kg) (Group C) while the other group received a single dose of albendazole (400 mg) alone (Group D). Trial drugs plus placebo were supplied by WHO/CTD, the Carter Centre (Atlanta, USA) and the Liverpool School of Tropical Medicine (Liverpool, UK).
Statistical analysis
Data analysis was done using Epi-Info version 6.04 C and Stata 6. Geometric mean microfilarial intensity (GMI) were calculated as antilog [(log (x+1)/n]-1 where x was the number of mf/ml counted and n is the total number of individuals. A non-parametric test (Mann-Whitney test) was used for comparing GMI of different study days and severity of adverse reactions. Fisher's exact test was used to compare prevalence of infection. P-values of less than 0.05 were considered to be statistically significance.
Results
Pre-treatment parasitological, physiological, haematological and clinical data
Co-infections of W. bancrofti and O. volvulus
The pre-treatment microfilaria counts ranged from 108–2232 mf/ml in W. bancrofti, and from 5–206 microfilariae/skin snip in O. volvulus. The geometric mean microfilarial intensity (GMI) for W. bancrofti, was 378.4 mf/ml in Group A, and 465.2 mf/ml in Group B. The microfilarial GMI for O. volvulus was 49.1 and 12.9 microfilariae/skin snips in Groups A and B respectively. There was no significant difference in terms of mf GMIs in W. bancrofti in the two treatment regimens (P = 0.7). However, the geometric mean microfilarial intensity between the two treatment groups was statistically significant in O. volvulus (P = 0.02). The physiological and haematological indices showed no changes for each individual, during the pre-treatment period or at Day 2/3 or Day 7 in both co-infected and single infections. Clinically, there was no significant variation in blood pressure, both systolic and diastolic between the treatment groups (data not shown).
Single infection of W. bancrofti
In the single infection the geometric mean microfilarial intensity in the two-treatment regimens was 508 mf/ml for each treatment group. There was no significant difference in geometric mean microfilarial intensity in the two treatments (P = 0.9).
Post-treatment safety evaluation
Post-treatment levels of the physiological tests and haematological indices in the single and co-infections between the two treatment regimens, placebo, albendazole alone and the combination of albendazole with ivermectin showed no change compared to pre-treatment levels. Likewise, the other parameters assessed, blood pressure, heart rate and body weight also showed no change. The mean level of AST in the co-infections of W. bancrofti and O. volvulus observed were 18.1 and 27 IU in Groups A and B respectively. There was no significant difference in the mean AST levels between Groups A and B (P = 0.07). The mean AST levels for single infection of bancroftian filariasis were 21.9 IU and 23.6 IU for albendazole alone and the combination respectively (P = 0.6).
Adverse Reactions
The adverse reactions occurred at 24 and 48 hours and on day 6 post-drug administration and were generally mild and well tolerated (Tables 1 and 2). These effects lasted for approximately 48 hours. Localised pruritis was observed in the co-infection of bancroftian filariasis plus onchocerciasis. Adverse reactions such as headache, dizziness and itching were reported in individuals with single infection of bancroftian filariasis. In the co-infections 9 out of 15 individuals who experienced adverse reaction, 5 had received albendazole plus ivermectin whereas 4 received placebo.
Three individuals in Group A experienced fever, while in Group B, 3 reported palpitations and one presented oedema on the right thigh. On day six post-treatment one individual from the albendazole and ivermectin group developed painful swelling on the right inguinal gland, which resolved by the third week post-treatment. In the single infection of bancroftian filariasis, 11 out of 25 individuals reported adverse reactions, of which 5 had received albendazole alone, while 6 had albendazole plus ivermectin. In the albendazole plus ivermectin group, two individuals experienced fever and 3 reported generalised itching and 1 had palpitations. Of those who received albendazole alone, one individual reported frontal headache, 2 dizziness, 1 adenitis and another 1 oedema of the right arm. Adverse reaction intensity mean score for the single regimen of albendazole alone and the combination of albendazole plus ivermectin in both co-infected and single infection was 1 (mild).
Treatment efficacy
Co-infections of W. bancrofti and O. volvulus
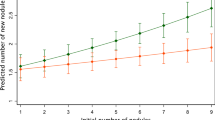
The treatment of co-infection with albendazole and ivermectin resulted in a rapid reduction of microfilarial intensity over the first week. For O. volvulus and W. bancrofti this reduction was sustained throughout the 12 months of the follow up period (Figure 2 & Figure 2b). Microfilarial prevalence of O. volvulus and W. bancrofti was reduced to 13 and 6% respectively at 14 days post treatment but increased throughout the rest of the follow up ranging from 33–53% for O. volvulus and 40–67% for W. bancrofti (Figure 2c).
Co-infected individuals treated with albendazole and ivermectin. a – Geometric mean intensity (95% confidence intervals) of W. bancrofti microfilariae in co-infected individuals treated with albendazole and ivermectin. b – Geometric mean intensity (95% confidence intervals) of O. volvulus microfilariae in co-infected individuals treated with albendazole and ivermectin. c – Microfilarial prevalence (%) in co-infected individuals treated with albendazole and ivermectin.
Single infection
Treatment of single W. bancrofti infection with albendazole resulted in a sustained reduction of microfilarial intensity throughout the follow up period (Figure 3a). The addition of ivermectin significantly improved efficacy at the time points sampled (P < 0.05 for all time points). The prevalence of microfilaraemia showed a dramatic difference between treatment with albendazole and albendazole plus ivermectin. Treatment with albendazole alone resulted in a 15–38% reduction in prevalence, compared to reductions of 73–100% in combined treatments (Figure 3b).
Single infections treated with albendzole or ivermectin. a – Geometric mean intensity (95% confidence intervals) of W. bancrofti microfilariae in single infections treated with albendazole or albendazole and ivermectin. b – Prevalence of microfilariaemia (%) in single infections of W. bancrofti treated with albendazole or albendazole and ivermectin.
There was no significant difference between single and co-infected individuals in the GMI of W. bancrofti during albendazole and ivermectin treatment.
Discussion
This is the first hospital-based trial of a combination of ivermectin and albendazole for the treatment of co-infection of bancroftian filariasis and onchocerciasis. We found that 400 mg of albendazole plus 150 μg/kg of ivermectin were safe and tolerable in individuals co-infected with W. bancrofti and O. volvulus infections. Due to the relatively low numbers of individuals with co-infection in this endemic area, only a small number of patients could be recruited to the study. Monitoring of haematological indices and physiological functions for liver, heart, muscle, kidney and blood showed no alteration as a result of any treatment regimen. There was no significant variation in AST levels during pre-and post-treatment for both co-infected and single W. bancrofti infected individuals in both treatment regimens. The absence of clinical response to treatment may be associated with the lower dosages administered in the current trial as compared to previous studies where higher doses were used, leading to transient elevation of the enzymes and increased frequency and intensity of adverse reaction [10].
Adverse reactions to treatment in patients with co-infection were equivalent to those experienced in individuals with single infection and were categorised as mild. The low frequency and intensity of adverse reactions observed in the study individuals probably reflects the low intensity of infections. Quantitatively it has been shown that the intensity of these adverse reactions is proportional to the pre-treatment microfilarial density [9] and is associated with the release of Wolbachia endosymbionts into the blood [11, 12]. These results are consistent with the conclusions from a multi-study analysis of the safety of two drug regimens for the treatment of lymphatic filariasis [13] and onchocerciasis [14].
In co-infected individuals albendazole and ivermectin treatment produced a reduction in microfilarial levels over the first week of treatment for both O. volvulus and W. bancrofti. Thereafter microfilarial levels were sustained at a low level throughout the follow-up period. Prevalence of infection ranged from 33–53% for O. volvulus and 40–67% for W. bancrofti from 30–360 days after drug administration.
In individuals with a single infection of bancroftian filariasis a similar trend was seen, with a rapid clearance within a week in the albendazole and ivermectin group. Treatment with albendazole and ivermectin was significantly better than treatment with albendazole alone. Reduction in the prevalence of detectable microfilaraemia was observed to be greater in the combination of ivermectin and albendazole (~70–80%) compared to albendazole alone (~20–40%).
Previous studies have shown that 3–6 months post-treatment with ivermectin, when doses of 150 μg/kg or lower are given, mf do gradually return to pre-treatment levels. This is probably due to the lack of adulticidal activity and the transient effect of the drug on embryogenesis [14]. Albendazole alone can have some marginal adulticidal activity and is moderately microfilaricidal, particularly at high doses [10]. However, it is the effectiveness of these drugs in combination, which has led to their use in community-based control strategies [9].
The dosage tested in this trial has been adopted for the community-based treatment of W. bancrofti in Tanzania. It has been observed in a study in Ghana using a similar dose, that in single bancroftian infections combinations of ivermectin and albendazole show no significant improvement on ivermectin alone, with albendazole on its own showing only minor effects [15]. In another study in Haiti, combination of albendazole and ivermectin was more effective than treatment with ivermectin only [16]. Our study shows that albendazole and ivermectin is more effective than albendazole alone in the reduction of microfilarial intensity and prevalence. As the interruption of transmission is fundamental to the success of community-based treatments, this emphasises the need for sustained treatments with high community coverage if transmission is to be interrupted.
In Tanzania, the use of combinations of albendazole and ivermectin has been adopted as the strategy for the community-based elimination of lymphatic filariasis as a public health problem. The current study suggests that this combination is safe to be used in areas of co-endemicity with onchocerciasis.
Conclusions
In areas of co-infection of bancroftian filariasis and onchocerciasis, which in Tanzania includes approximately half a million people infected with O. volvulus, the use of albendazole (400 mg) and ivermectin (150 μg/kg) appears to be safe and tolerable. Since only a relatively small number of patients could be recruited to this study due to the low prevalence of co-infection, these results should be considered as preliminary and additional studies on individuals with co-infection in other endemic areas should be carried out.
References
Kale OO: Onchocerciasis: the burden of disease. Ann Trop Med Parasitol. 92: S101-S115. 10.1080/00034989859636.
WHO: Global programme to eliminate lymphatic filariasis. WHO/CDS/CPE/CEE/2002.28. 2002, [http://www.filariasis.org]
Michael E, Bundy DAP, Grenfell BT: Re-assessing the global prevalence and distribution of lymphatic filariasis. Parasitology. 1996, 112: 409-428.
Maegga BTA: Onchocerciasis. In: Health and Disease in Tanzania. Edited by: Mwaluko GMR, Kilama WL, Mandara MP, Murru M and Macpherson CNL. 1991, London, Harper Collins Academic Press, 159-176.
McMahon JE, Magayuka SA, Kolstrup N, Mosha FW, Bushrod FM, Abaru DE, Bryan JH: Studies on the transmission and prevalence of Bancroftian filariasis in four coastal villages of Tanzania. Ann Trop Med Parasitol. 1981, 75: 415-431.
Evans BD, Gelband H, Vlassoff C: Social and economical factors and the control of lymphatic filariasis a review. Acta Trop. 1993, 53: 1-26. 10.1016/0001-706X(93)90002-S.
Workneh W, Fletcher M, Olwit G: Onchocerciasis in field workers at Bay farm, Teppi coffee plantation project, south-western Ethiopia: prevalence and impact on productivity. Acta Trop. 1993, 54: 89-97. 10.1016/0001-706X(93)90054-F.
Ottesen EA, Duke BOL, Karam M, Behbehani K: Strategies and tools for the control/elimination of lymphatic filariasis. Bull World Health Organ. 1997, 75: 491-503.
Ottesen EA, Ismail MM, Horton J: The role of albendazole in programmes to eliminate lymphatic filariasis. Parasitol Today. 1999, 15: 382-386. 10.1016/S0169-4758(99)01486-6.
Ismail MM, Jayakody RL, Weil GJ, Nirmalan N, Jayasinghe KSA, Abeyewickrema W, Rezvi Sheriff MH, Rajaratnam HN, Amarasekara N, DeSilva DCL, Michalski ML, Dissanaike AL: Efficacy of single dose combination of albendazole, ivermectin and diethylcarbamazine for the treatment of bancroftian filariasis. Trans R Soc Trop Med Hyg. 1998, 92: 94-97.
Keiser PB, Reynolds SM, Awadzi K, Ottesen EA, Taylor MJ, Nutman TB: Bacterial endosymbionts of Onchocerca volvulus in the pathogenesis of posttreatment reactions. J Infect Dis. 2002, 185: 805-811. 10.1086/339344.
Cross HF, Haarbrink M, Egerton G, Yazdanbakhsh M, Taylor MJ: Severe reactions to filarial chemotherapy and release of Wolbachia endosymbionts into blood. Lancet. 2001, 358: 1873-1875. 10.1016/S0140-6736(01)06899-4.
Horton J, Witt C, Ottesen EA, Lazdins JK, Addiss DG, Awadzi K, Beach MJ, Belizario VY, Dunyo SK, Espinel M, Gyapong JO, Hossain M, Ismail MM, Jayakody RL, Lammie PJ, Makunde W, Lenoble-Richard D, Selve B, Shenoy RK, Simonsen PE, Wamae CN, Weerasooriya MV: An analysis of the safety of the single dose, two drug regimens used in programmes to eliminate lymphatic filariasis. Parasitology. 2000, 121: S147-S160. 10.1017/S0031182000007423.
Awadzi K, Edwards G, Duke BO, Opoku NO, Attah SK, Addy ET, Ardrey AE, Quartey BT: The co-administration of ivermectin and albendazole – safety, pharmacokinetics and efficacy against Onchocerca volvulus. Ann Trop Med Parasitol. 2003, 97: 165-78. 10.1179/000349803235001697.
Dunyo SK, Nkrumah FK, Simonsen PE: Single-dose treatment of Wuchereria bancrofti infections with ivermectin and albendazole alone or in combination: evaluation of the potential for control at 12 months after treatment. Trans R Soc Trop Med Hyg. 2000, 94: 437-443.
Addiss DG, Beach MJ, Streit TG, Lutwick S, LeConte FH, Lafontant JG, Hightower AW, Lammie PJ: Randomised placebo-controlled comparison of ivermectin and albendazole alone and in combination for Wuchereria bancrofti microfilaraemia in Haitian children. Lancet. 1997, 16: 480-484. 10.1016/S0140-6736(97)02231-9.
Acknowledgements
We thank all the Bombo Regional Hospital staff that in one way or another made the clinical assessment of this trial possible. We also acknowledge the assistance given by Mr. Charles Guzo, Ms. Zaina Ali, and Mrs. Bibiana Reuben during the implementation of the trial. We are also grateful to Dr. Alphage Liwa, the former Medical officer in-charge, Bombo Regional Hospital, for providing space for the study and also the villagers of Maramba who participated in this trial. Drs. L.E.G. Mboera, Helen F. McGarry and Professor Chris Curtis are thanked for their useful comments on the earlier version of the manuscript and Dr. Sabine Kläger for statistical advice. Prof. David Molyneux, Dr. Eric Ottesen and Dr. Stefanie Merideth for supplying some of the trial drugs. The study received financial support from the UNDP/World Bank/WHO/ Special Programme for Research & Training in Tropical Diseases (TDR). MJT is a Senior Wellcome Research Fellow in Basic Biomedical Science.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors' contributions
WHM – Data collection, analysis and manuscript preparation.
LMK & FMS – Data analysis
RWM – Clinical evaluation and monitoring of adverse reactions
JJM – Randomization and treatment allocation
SZX & JA – Parasitological & biochemical examination
MT – PhD supervisor, interpretation of data and manuscript preparation
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Makunde, W.H., Kamugisha, L.M., Massaga, J.J. et al. Treatment of co-infection with bancroftian filariasis and onchocerciasis: a safety and efficacy study of albendazole with ivermectin compared to treatment of single infection with bancroftian filariasis. Filaria J 2, 15 (2003). https://doi.org/10.1186/1475-2883-2-15
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2883-2-15