Abstract
Background
Effective treatment remains a mainstay of malaria control, but it is unfortunately strongly compromised by drug resistance, particularly in Plasmodium falciparum, the most important human malaria parasite. Although P. falciparum chemoresistance is well recognized all over the world, limited data are available on the distribution and prevalence of pfcrt and pfmdr1 haplotypes that mediate resistance to commonly used drugs and that show distinct geographic differences.
Methods
Plasmodium falciparum-infected blood samples collected in 2007 at four municipalities of Luanda, Angola, were genotyped using PCR and direct DNA sequencing. Single nucleotide polymorphisms in the P. falciparum pfcrt and pfmdr1 genes were assessed and haplotype prevalences were determined.
Results and Discussion
The most prevalent pfcrt haplotype was StctVMNT (representing amino acids at codons 72-76). This result was unexpected, since the StctVMNT haplotype has previously been seen mainly in parasites from South America and India. The CVIET, CVMNT and CVI NT drug-resistance haplotypes were also found, and one previously undescribed haplotype (CVMDT) was detected. Regarding pfmdr1, the most prevalent haplotype was Y EYSNVD (representing amino acids at codons 86, 130, 184, 1034, 1042, 1109 and 1246). Wild haplotypes for pfcrt and pfmdr1 were uncommon; 3% of field isolates harbored wild type pfcrt (CVMNK), whereas 21% had wild type pfmdr1 (NEYSNVD). The observed predominance of the StctVMNT haplotype in Angola could be a result of frequent travel between Brazil and Angola citizens in the context of selective pressure of heavy CQ use.
Conclusions
The high prevalence of the pfcrt S VMNT haplotype and the pfmdr1 86Y mutation confirm high-level chloroquine resistance and might suggest reduced efficacy of amodiaquine in Angola. Further studies must be encouraged to examine the in vitro sensitivity of pfcrt S VMNT parasites to artesunate and amodiaquine for better conclusive data.
Similar content being viewed by others
Background
More than 125 years after the discovery of the causative parasites, malaria continues to be one of the most important infectious diseases in the world. According to WHO, 3.3 billion people are at risk, and about 250 million malaria cases occur annually, causing nearly one million deaths, mostly in children below five years of age. Overall, 109 countries are endemic for malaria; 45 of these are in Africa [1]. While work continues toward a malaria vaccine, prompt diagnosis and effective treatment remain, in addition to vector control measures, mainstays of malaria control [2]. Unfortunately, disease control is strongly compromised by the emergence of resistance to commonly used drugs [3]. Of particular concern is resistance in Plasmodium falciparum, the most virulent human malaria parasite [4].
Important advances in the understanding of mechanisms of anti-malarial drug resistance have been made in recent years [5]. Resistance to chloroquine (CQ), which was previously the most widely used anti-malarial, is mainly conferred by single-nucleotide polymorphisms (SNPs) in pfcrt, a putative transmembrane transporter localized in the parasite digestive vacuole membrane [6]. In particular, the pfcrt K76T mutation plays a central role in mediating resistance to CQ, and it is considered a reliable molecular marker of resistance [7, 8]. Polymorphisms in another gene, pfmdr1, are associated with modulation of parasite susceptibility to a number of drugs, including CQ and amodiaquine [9].
Regarding the pfcrt gene, a haplotype defined by the K76T codon and adjacent amino acids (numbers 72-75) has been used to type malaria parasites. Three main pfcrt haplotypes have been identified [10]: CVMNK among CQ-sensitive isolates from all geographic regions, CVIET among CQ-resistant isolates from Southeast Asia and Africa, and S VMNT among CQ-resistant isolates from South America (type StctVMNT; the subscript represents codon usage) and some countries of Asia (type SagtVMNT) [11–15].
Although P. falciparum chemoresistance has been described in most malarious regions [5], limited data are available on the distribution and prevalence of pfcrt and pfmdr1 haplotypes. It was investigated the prevalence of mutations in these two genes in P. falciparum from Angola, where only two such molecular studies have been published previously [16, 17].
Methods
Study site and population
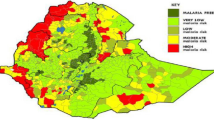
Clinical samples were collected in 2007 at Luanda, the capital of Angola, from individuals living in the municipalities of Sambizanga, Imgombotas, Cazenga and Viana. Luanda has a population of approximately 4.5 million and is considered a meso-endemic malaria area, according to parasitological surveys in children < 5 years and number of malaria deaths at local hospitals. Malaria is present throughout the year, with a marked increase after rains peak during April and May [18]. The treatment policy in Angola for uncomplicated falciparum malaria in absence of first trimester of pregnancy included artemether + lumefantrine or alternatively artesunate + amodiaquine.
Patients diagnosed with falciparum malaria based on Giemsa-stained thick smear were included in this study, after obtaining informed consent. Inclusion criteria were individuals with age ≥ 18 years, uncomplicated malaria, monoinfection with P. falciparum and unaware of first trimester pregnancy. The study was approved by the National Institute of Public Health/Angola Ethics Research Committee with concurrence from the Instituto Oswaldo Cruz/Fiocruz.
Study procedures
After enrollment, 5 ml of blood was collected by venipuncture and placed into ethylenediaminetetraacetic acid (EDTA) vacutainer tubes (Becton Dickinson). The samples were centrifuged (350 g, 10 minutes), pellets were frozen with an equal volume of cryopreservation solution (0.9% sodium chloride, 4.2% sorbitol and 28% glycerol) and transported frozen to the Instituto Oswaldo Cruz (Fiocruz), Rio de Janeiro, Brazil.
DNA preparation
Blood samples were thawed, and 1 ml was used for DNA extraction with the QIAamp midi kit, as described by the manufacturer (Qiagen). Samples were resuspended in a final volume of 50 μl.
Nested PCR for pfcrt amplification
The pfcrt amplification protocol was described elsewhere [19]. Briefly, 5 μl of DNA solution was added to a 45 μl mixture containing 10 pmol of primers CRTP1 (5' CCG TTA ATA ATA AAT ACA CGC AG 3') and CRTP2 (5' CGG ATG TTA CAA AAC TAT AGT TAC C 3'). In a subsequent PCR, 5 μl of the initial PCR product was mixed with 10 pmol of primers CRTD1 (5' TGT GCT CAT GTG TTT AAA CTT 3') and CRTD2 (5' CAA AAC TAT AGT TAC CAA TTT TG 3'), to amplify a 134 bp fragment comprising the pfcrt SNPs C72S, M74I, N75E/D and K76T. PCR reactions were run twice with the GeneAmp PCR System 9700 (Applied Biosystems). DNA positive and negative controls were also used in each round of amplification. The positive control consisted of DNA from blood samples from patients diagnosed with falciparum malaria based on Giemsa-stained thick smear and the negative control consisted of DNA from blood samples of individuals without history of visiting endemic areas as well as a blank tube without DNA.
Single PCRs for pfmdr1 amplification
Pfmdr1 gene analysis was performed with two PCR reactions that were made two times using 3 μl of DNA solution in a 47 μl mixture containing 2.5 mM of MgCl2, 250 μM of dNTPs, 2.5 units of Amplitaq Gold® DNA polymerase (Applied Biosystems), and 10 pmol of primers MDR1STF (5' CCG TTT AAA TGT TTA CCT GCA C 3') and MDR1STR (5' TTG CAA CAG TTC TTA TTC CCA 3') to amplify a 604 bp region comprising SNPs N86Y, E130K and Y184F; or primers MDR1ENDF (5' GCG GAG TTT TGC ATT TAG TTC 3') and MDR1ENDR (5' CAA TGT TGC ATC TTC TCT TCC A 3') to amplify a 935 bp region comprising SNPs S1034C, N1042D, V1109I and D1246Y. The first reaction was incubated at 95°C for 10 minutes, followed by 45 cycles (94°C/1 minute, 58°C/1 minute and 72°C/1 minute) plus one final incubation at 72°C for 10 minutes. The second reaction was incubated at 95°C for 10 minutes, followed by 45 cycles (94°C/1 minute and 30 seconds, 60°C/1 minute and 30 seconds and 72°C/1 minute and 30 seconds) and a final incubation at 72°C for 10 minutes. As for pfcrt PCR, it was also used DNA positive and negative controls in each PCR.
PCR analysis and product purification
PCR products were separated by 2% agarose-gel electrophoresis. Products were purified through the Wizard SV Gel and PCR Clean-Up System (Promega), according to the manufacturer's instructions.
Sequencing
DNA sequencing was performed using pfcrt nested or pfmdr1 single PCR primers plus the purified product according to Big Dye® Terminator Cycle Sequencing Ready Reaction version 3.1 instructions (Applied Biosystems). Sequences were read using an ABI PRISM DNA Analyzer 3730 (Applied Biosystems) from the Genomic Platform/PDTIS/Fiocruz [20].
Sequence analysis
The forward and reverse sequences were analysed using the free software Bioedit Sequence Alignment Editor version 7.0.5.2.
Results
DNA blood samples from 114 patients with uncomplicated falciparum malaria were tested. The majority of samples were composed by adults with 21 to 30 years and their parasitemia range was 500-100,000 parasites/μl. We detected 102 PCR-positive samples for pfcrt (32 from Sambizanga, 42 from Ingombotas, 21 from Cazenga and 7 from Viana) and 28 samples for both pfmdr1 PCR amplifications (5 from Sambizanga, 13 from Ingombotas, 6 from Cazenga and 4 from Viana). Frequent failures to amplify pfmdr1 might be attributed to primer limitations due to polymorphisms in target sequences; for all these samples fragments were amplified using other primers developed for diagnosis, confirming the presence of parasite DNA in the samples [21].
Mixed infections with two different pfcrt genotypes were common (Table 1). The most prevalent haplotype for pfcrt was StctVMNT (58/102). This result was unexpected, since the StctVMNT haplotype has previously been seen mainly in parasites from South America and India [22, 23]. The CVIET, CVMNT and CVI NT drug-resistance haplotypes were also found, and one previously undescribed haplotype (CVMDT) was detected. Regarding pfmdr1, the most prevalent haplotype was Y EYSNVD (17/28) (representing amino acids at positions 86, 130, 184, 1034, 1042, 1109 and 1246) with wild type sequence except for the 86 codon (Table 2). No significant difference between the four municipalities was observed for both genes.
Wild haplotypes for pfcrt and pfmdr1 were uncommon; 3% (3/102) of field isolates harbored wild type pfcrt (CVMNK), whereas 21% (6/28) had wild type pfmdr1 (NEYSNVD). The co-analysis of pfcrt and pfmdr1 genes (n = 28) revealed some prevalent pfcrt and pfmdr1 associations: pfcrt CVIET coexisted with pfmdr1 Y EYSNVD in 29% of samples, StctVMNT with Y EYSNVD in 14% of samples and CVIET with NEYSNVD in 11% of samples. Only one sample, from Imgombotas, was entirely wild type in the pfcrt and pfmdr1 genes, and three samples, from Cazenga and Imgombotas, harbored only one mutation, this at pfmdr1 codon 184.
Discussion
In this study, the pfcrt and pfmdr1 haplotypes of P. falciparum from Angola (Luanda) were characterized. Well-known as well as unusual pfcrt haplotypes were identified: CVMNK representing the sensitive haplotype, StctVMNT, CVMNT, CVI NT and CVIET representing previously described drug-resistance-mediating haplotypes, and CVMDT, a previously undescribed haplotype. These results offer insight into the spread of drug resistance in malaria parasites.
CQ-resistant P. falciparum parasites were first detected in the 1950 s on the Thailand-Cambodia border and in South America [24]. In Africa, resistant parasites are thought to have originated from Southeast-Asian isolates that spread progressively in the 1970 s through the Indian subcontinent and then to East Africa. Different origins of chloroquine resistance are supported by the existence of different haplotypes in different areas, notably CVMNK among CQ-sensitive isolates from all regions, and, among resistance-mediating haplotypes CVIET in Southeast Asia and Africa, StctVMNT in South America, and SagtVMNT in some countries of Asia [11–15].
Surprisingly, in this study the most prevalent pfcrt haplotype was StctVMNT. In prior studies, this StctVMNT allele was the predominant haplotype in Brazil [25], and it has also been described in Guyana [26, 27] and Peru [28]. It has been reported only once in Africa, in 4% of P. falciparum samples from Ghana [26]. In addition, an S VMNT haplotype with different codon preference (SagtVMNT) was seen in 19% of samples from Tanzania [29, personal communication, Michael Alifrangis]. The observed predominance of the StctVMNT haplotype in Angola could be a result of frequent travels between Brazilian and Angolan citizens by means of trade, business and educational purposes, in the context of the selective pressure of heavy use of CQ. It is important to remark that Angola and Brazil have a singular relationship towards each other. Since 2000, commerce between these two countries was established and it is now flourishing. With trade enhancement, the presence of Brazilian companies in Angola has grown and consequently, short or long-terms travels from Brazil to Angola and vice-versa have also increased. An analysis of neutral microsatellite markers could help to explain if the high prevalence of the StctVMNT haplotype in Angola is related to a Brazilian geographical allelic exchange or to a novel selection of resistance in Angola [26, 30]. Likewise, the pfcrt C/S VIET mixed haplotype seen in Angola could give rise to the S VIET haplotype previously identified in the Democratic Republic of Congo [31]. Similar to potential transfer from Brazil to Angola, the presence of this haplotype in Angola might be due to traffic between the Democratic Republic of Congo and Angola. In fact, there is an expressive non-controlled migration from Congo to Angola mainly to find work at diamond mines and in a lesser extend from Angola to Congo to visit family members that were moved to Congo due to colonial Portuguese war.
The analysis of pfmdr1 haplotypes in Angola revealed the Y EYSNVD and NEYSNVD haplotypes, which were already observed in isolates from other African countries [26] and were also detected in Asia [32]. Although previous studies performed with Angolan samples only reported 2 mutations - 86Y for pfmdr1 gene and 76T for pfcrt gene - the frequencies informed for both genes are in accordance with our findings [16, 17].
It is important to notice that for the pfmdr1 gene, associations of polymorphisms with CQ sensitivity are less straightforward than for pfcrt. Mutations in pfmdr1 also impact on responses to other drugs. Indeed, the same mutations that apparently decrease sensitivity to CQ, amodiaquine, and quinine may increase sensitivity to some other drugs, including mefloquine and halofantrine [33]. Considering this complexity, the selective pressures that led to common pfmdr1 haplotypes in Angola are uncertain.
Of interest, pfcrt and pfmdr1 haplotypes also impact on sensitivity to amodiaquine. In particular, the SagtVMNT haplotype has been associated with decreased amodiaquine sensitivity compared to other haplotypes also containing the K76T mutation [12, 26, 34], and the pfmdr1 N86Y mutation mediated decreased in vitro sensitivity to amodiaquine [33], and was selected by prior amodiaquine therapy [35]. In this context, the 57% prevalence of the StctVMNT haplotype and 66% prevalence of pfmdr1 86Y might suggest widespread resistance to amodiaquine in Angola.
Conclusions
The high prevalence of the pfcrt S VMNT haplotype and the pfmdr1 86Y SNP confirm high-level chloroquine resistance and might suggest reduced efficacy of amodiaquine in Angola. Further in vitro studies must be conducted to evaluate the influence of pfcrt S VMNT haplotype to artesunate and amodiaquine sensitivity, for better conclusive data.
References
WHO: World malaria report 2008. [http://malaria.who.int/wmr2008/malaria2008.pdf]
Walter B, Walter M: What does it take to control malaria?. Ann Trop Med Parasitol. 2007, 101: 657-672. 10.1179/136485907X229013.
Bloland PB: Drug resistance in malaria. [http://www.who.int/csr/resources/publications/drugresist/malaria.pdf]
Haivas I: Roll Back Malaria campaign still has a long way to go. BMJ. 2003, 326: 951-10.1136/bmj.326.7396.951/c.
Talisuna AO, Bloland P, D'Alessandro U: History, dynamics and public health importance of malaria parasite resistance. Clin Microbiol Rev. 2004, 17: 235-254. 10.1128/CMR.17.1.235-254.2004.
Fidock DA, Nomura T, Talley AK, Cooper RA, Dzekunov SM, Ferdig MT, Ursos LM, Sidhu AB, Naude B, Deitsch KW, Su XZ, Wootton JC, Roepe PD, Wellems TE: Mutations in the P. falciparum digestive vacuole transmembrane protein pfcrt and evidence for their role in chloroquine resistance. Molecular Cell. 2000, 6: 861-871. 10.1016/S1097-2765(05)00077-8.
Cooper RA, Hartwig CL, Ferdig MT: pfcrt is more than the Plasmodium falciparum chloroquine resistance gene: a functional and evolutionary perspective. Acta Trop. 2005, 94: 170-180.
Plowe CV: Monitoring the antimalarial drug resistance: making the most of the tools at hand. J Exp Biol. 2003, 206: 3745-3752. 10.1242/jeb.00658.
Duraisingh MT, Cowman AF: Contribution of the pfmdr1 gene to antimalarial drug-resistance. Acta Trop. 2005, 94: 181-190.
Wootton JC, Feng X, Ferdig MT, Cooper RA, Mu J, Baruch DI, Magill AJ, Su XZ: Genetic diversity and chloroquine selective sweeps in Plasmodium falciparum. Nature. 2002, 418: 320-333. 10.1038/nature00813.
Mehlotra RK, Fujioka H, Roepe PD, Janneh O, Ursos LM, Jacobs-Lorena V, McNamara DT, Bockarie MJ, Kazura JW, Kyle DE, Fidock DA, Zimmerman PA: Evolution of a unique Plasmodium falciparum chloroquine-resistance phenotype in association with pfcrt polymorphism in Papua New Guinea and South America. Proc Natl Acad Sci USA. 2001, 98: 12689-12694. 10.1073/pnas.221440898.
Dittrich S, Alifrangis M, Stohrer JM, Thongpaseuth V, Vanisaveth V, Phetsouvanh R, Phompida S, Khalil IF, Jelinek T: Falciparum malaria in the north of Laos: the occurrence and implications of the Plasmodium falciparum chloroquine resistance transporter (pfcrt) gene haplotype SVMNT. Trop Med Int Health. 2005, 10: 1267-1270. 10.1111/j.1365-3156.2005.01514.x.
Chen N, Wilson DW, Pasay C, Bell D, Martin LB, Kyle D, Cheng Q: Origin and dissemination of chloroquine-resistant Plasmodium falciparum with mutant pfcrt alleles in the Philippines. Antimicrob Agents Chemother. 2005, 49: 2102-2105. 10.1128/AAC.49.5.2102-2105.2005.
Huaman MC, Yoshinaga K, Suryanatha A, Suarsana N, Kanbara H: Short report: polymorphisms in the chloroquine resistance transporter gene in Plasmodium falciparum isolates from Lombok, Indonesia. Am J Trop Med Hyg. 2004, 71: 40-42.
Ursing J, Zakeri S, Gil JP, Björkman A: Quinoline resistance associated polymorphisms in the pfcrt, pfmdr1 and pfmrp genes of Plasmodium falciparum in Iran. Acta Trop. 2006, 97: 352-356. 10.1016/j.actatropica.2006.01.002.
Pinheiro L, Franco S, Adagu IS, Rosa R, Do Rosário VE, Warhurst DC: Detecção da mutação dupla 86TYR e 1246TYR no gene pfmdr1 em clones de uma amostra de Plasmodium falciparum da África Ocidental, resistente à cloroquina. Acta Med Portug. 2003, 16: 229-233.
Figueiredo P, Benchimol C, Lopes D, Bernardino L, do Rosario VE, Varandas L, Nogueira F: Prevalence of pfmdr1, pfcrt, pfdhfr and pfdhps mutations associated with drug resistance, in Luanda, Angola. Malar J. 2008, 7: 236-10.1186/1475-2875-7-236.
Republic of Angola, Ministry of, Health, National Program for Malaria Control: Plano estratégico nacional para o controlo da malária em Angola (2008-2012). Luanda. 2007
Gama BE, de Oliveira NK, Zalis MG, de Souza JM, Santos F, Daniel-Ribeiro CT, Ferreira-da-Cruz M de F: Chloroquine and sulphadoxine-pyrimethamine sensitivity of Plasmodium falciparum parasites in a Brazilian endemic area. Malar J. 2009, 8: 156-10.1186/1475-2875-8-156.
Otto TD, Vasconcellos EA, Gomes LHF, Moreira AS, Degrave WM, Mendonça-Lima L, Alves-Ferreira M: ChromaPipe: a pipeline for analysis, quality control and management for a DNA sequencing facility. Genet Mol Res. 2008, 7: 861-871. 10.4238/vol7-3X-Meeting04.
Zalis MG, Ferreira-da-Cruz MF, Balthazar-Guedes HC, Banic DM, Alecrim W, Souza JM, Druilhe P, Daniel-Ribeiro CT: Malaria diagnosis: standardization of a polymerase chain reaction for the detection of Plasmodium falciparum parasites in individuals with low-grade parasitemia. Parasitol Res. 1996, 82: 612-616. 10.1007/s004360050173.
Keen J, Farcas GA, Zhong K, Yohanna S, Dunne MW, Kain KC: Real-time PCR assay for rapid detection and analysis of PfCRT haplotypes of chloroquine-resistant Plasmodium falciparum isolates from India. J Clin Microbiol. 2007, 45: 2889-2893. 10.1128/JCM.02291-06.
Pati SS, Mishra S, Mohanty S, Mohapatra DN, Sahu PK, Priyadarshi N, Kumar S, Sharma SK, Tyagi PK, Chitnis CE, Das BS: Pfcrt haplotypes and in vivo chloroquine response in Sundergarh district, Orissa, India. Trans R Soc Trop Med Hyg. 2007, 101: 650-654. 10.1016/j.trstmh.2007.01.008.
Wernsdorfer WH, Payne D: The dynamics of drug resistance in Plasmodium falciparum. Pharmacol Ther. 1991, 1: 95-121. 10.1016/0163-7258(91)90074-V.
Vieira PP, Ferreira MU, Alecrim MG, Alecrim WD, da Silva LH, Sihuincha MM, Joy DA, Mu J, Su XZ, Zalis MG: pfcrt Polymorphism and the spread of chloroquine resistance in Plasmodium falciparum populations across the Amazon Basin. J Infect Dis. 2004, 190: 417-424. 10.1086/422006.
Mehlotra RK, Mattera G, Bockarie MJ, Maguire JD, Baird JK, Sharma YD, Alifrangis M, Dorsey G, Rosenthal PJ, Fryauff DJ, Kazura JW, Stoneking M, Zimmerman PA: Discordant patterns of genetic variation at two chloroquine resistance loci in worldwide populations of the malaria parasite Plasmodium falciparum. Antimicrob Agents Chemother. 2008, 52: 2212-2122. 10.1128/AAC.00089-08.
Best Plummer W, Pinto Pereira LM, Carrington CV: Pfcrt and pfmdr1 alleles associated with chloroquine resistance in Plasmodium falciparum from Guyana, South America. Mem Inst Oswaldo Cruz. 2004, 99: 389-392.
Huaman MC, Roncal N, Nakazawa S, Long TT, Gerena L, Garcia C, Solari L, Magill AJ, Kanbara H: Polymorphism of the Plasmodium falciparum multidrug resistance and chloroquine resistance transporter genes and in vitro susceptibility to aminoquinolines in isolates from the Peruvian Amazon. Am J Trop Med Hyg. 2004, 70: 461-466.
Alifrangis M, Dalgaard MB, Lusingu JP, Vestergaard LS, Staalsoe T, Jensen AT, Enevold A, Rønn AM, Khalil IF, Warhurst DC, Lemnge MM, Theander TG, Bygbjerg IC: Occurrence of the Southeast Asian/South American SVMNT haplotype of the chloroquine-resistance transporter gene in Plasmodium falciparum in Tanzania. J Infect Dis. 2006, 193: 1738-1741. 10.1086/504269.
Vinayak S, Mittra P, Sharma YD: Wide variation in microsatellite sequences within each Pfcrt mutant haplotype. Mol Biochem Parasitol. 2006, 147: 101-108. 10.1016/j.molbiopara.2006.01.013.
Severini C, Menegon M, Sannella AR, Paglia MG, Narciso P, Matteelli A, Gulletta M, Caramello P, Canta F, Xayavong MV, Moura IN, Pieniazek NJ, Taramelli D, Majori G: Prevalence of pfcrt point mutations and level of chloroquine resistance in Plasmodium falciparum isolates from Africa. Infect Genet Evol. 2006, 6: 2602-2608. 10.1016/j.meegid.2005.07.002.
Zakeri S, Afsharpad M, Kazemzadeh T, Mehdizadeh K, Shabani A, Djadid ND: Association of pfcrt but not pfmdr1 alleles with chloroquine resistance in Iranian isolates of Plasmodium falciparum. Am J Trop Med Hyg. 2008, 78: 633-640.
Nsobya SL, Kiggundu M, Nanyunja S, Joloba M, Greenhouse B, Rosenthal PJ: In vitro sensitivities of Plasmodium falciparum to different antimalarial drugs in Uganda. Antimicrob Agents Chemother. 2010, 54: 1200-1206. 10.1128/AAC.01412-09.
Warhurst DC: Polymorphism in the Plasmodium falciparum chloroquine-resistance transporter protein links verapamil enhancement of chloroquine sensitivity with the clinical efficacy of amodiaquine. Malar J. 2003, 2: 31-10.1186/1475-2875-2-31.
Nsobya SL, Dokomajilar C, Joloba M, Dorsey G, Rosenthal PJ: Resistance-mediating Plasmodium falciparum pfcrt and pfmdr1 alleles after treatment with artesunate-amodiaquine in Uganda. Antimicrob Agents Chemother. 2007, 51: 3023-3025. 10.1128/AAC.00012-07.
Acknowledgements
We would also like to thank the staff from the Genomic Platform/PDTIS/Fiocruz. This work was financially supported by POM/PEF/Instituto Oswaldo Cruz, CNPq/PAPES-Fiocruz, FAPERJ and CAPES programs from Brazil and by Ministry of Health and Eduardo Santos Foundation from Angola.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
BEG participated in the design of the study, carried out the molecular analysis and drafted the manuscript; GALPC and FJILK were the responsible for blood samples collection; NKAO performed the PCR assays; FF helped in study design and field facilities; PJR and CTDR helped in the design of the study and reviewed the manuscript; MFFC conceived the study, coordinated its design, and finalized the manuscript. All authors have read and approved the final text.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Gama, B.E., Pereira-Carvalho, G.A., Lutucuta Kosi, F.J. et al. Plasmodium falciparum isolates from Angola show the StctVMNT haplotype in the pfcrt gene. Malar J 9, 174 (2010). https://doi.org/10.1186/1475-2875-9-174
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2875-9-174