Abstract
Background
Malaria is one of the most serious health problems in Kenya. In 2004, the Kenya Medical Research Institute and the US Army Medical Research Unit – Kenya surveyed adults in Samburu, Malindi, and Busia districts to determine socioeconomic risk factors for infection.
Methods
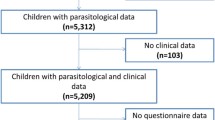
Sociodemographic, health, and antimalarial data were collected along with blood for malaria testing. A smear was considered negative only if no Plasmodium falciparum parasites were observed in 100 high-powered fields. Univariate analysis was performed with Pearson's Chi-square test and univariate logistic regression. A multivariate logistic regression model was then created which included only variables found to be at least marginally significant in univariate analysis.
Results
A total of 1,141 subjects were recruited: 238 from Samburu, 442 from Malindi, and 461 from Busia. Smear positivities for P. falciparum were 1.7% in Samburu, 7.2% in Malindi and 22.3% in Busia. Interdistrict differences were statistically significant (p < 0.001) in univariate analysis and in a multivariate logistic regression model which included district, literacy, occupation, and recent illness as independent variables. In the model, literacy and recent diarrhoeal illness were positively and at least marginally significantly associated with parasitaemia (p = 0.023 and p = 0.067, respectively). Neither age, sex, occupation, history of malaria in the previous three months, nor use of antimalarials in the previous four weeks were significantly associated with parasitaemia.
Conclusion
While district of residence was the variable most highly predictive for parasitaemia among Kenyan adults surveyed, both a recent history of diarrhoeal illness and literacy were at least marginally statistically significant predictors.
Similar content being viewed by others
Background
Malaria is one of the most serious health problems in Kenya. According to the World Health Organization (WHO), in 2002, there were over 124,000 reported cases of malaria nationwide in a population reported at just over 32 million [1]. Moreover, cases are likely grossly underreported [2]. According to one study, the mortality from malaria in one area of the Lake Victoria Basin was 20.8 per 1000 person-years [3]. The malaria burden is increased by high levels of resistance to antimalarial drugs [4–9] and by frequent self-administration of antimalarials [10–17].
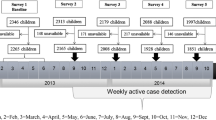
Between June and September 2004, researchers from the Kenya Medical Research Institute (KEMRI) and the United States Army Medical Research Unit – Kenya (USAMRU-K) carried out a community-based malaria parasitaemia and arboviral serologic survey of residents of three ecologically and culturally diverse Kenyan districts: Samburu, Malindi, and Busia, to assess potential socioeconomic risk factors for exposure to these pathogens. Extensive demographic, socioeconomic, health history, and recent antimalarial use data were collected along with blood for malaria smear and arboviral antibody testing. The malaria parasitaemia rates found in these three districts are reported here. Additionally, this study examines individual risk factors for parasitaemia, such as occupation, literacy, recent illness, health care utilization, and use of antimalarials.
Methods
Study design
The study employed a population-based, cross-sectional design. Two villages were selected from each of the three districts under study. A two-stage cluster sampling technique was used to select villages for enrollment. The study population enrolled consisted of all consenting adults aged 18 years and above living in any of these six villages for at least five years. A standardized questionnaire was administered and a malaria smear taken at enrollment. This study was performed under a protocol approved by the KEMRI/National Ethical Review Committee.
Site selection
District
The districts of Samburu, Malindi and Busia were selected for their ecological and social diversity. Samburu is located in semi-arid northern Kenya, where malaria is mesoendemic, and is sparsely populated, mostly by semi-nomadic herdsmen. Malindi is an Indian Ocean coastal district, with endemic malaria and a population of mostly fishermen and agriculturalists. Busia is located in the Lake Victoria basin region on the Ugandan border. It is a center of cross-border commerce and trade, but also has a large agrarian population and is endemic for malaria.
Village
Kenya is divided into provinces, districts, subdistricts, divisions, locations, sublocations and villages. To obtain a representative sample of adults residing in the districts, a two-stage cluster sampling technique was used. A sampling frame was created for each district, from which two sublocations were selected using probability proportional to population size sampling without replacement [18]. The second stage sampling frames were then created for each of these six sublocations with the enumeration units being the sublocation's villages. Using the same sampling technique, one village from each sublocation was selected. All eligible and consenting adults from each selected village were enrolled.
Subject recruitment and informed consent
At each of the selected sites, both the community leaders and the community were engaged prior to conducting the study. These leaders organized community meetings at which study staff explained the study and answered any questions posed in this open forum.
Enrollment was conducted in community centers, such as schools or clinics, selected by local community leaders. These leaders verified that all potential subjects had been residents of the selected villages for at least five years. Before any potential subject was enrolled, a trained field worker explained the study in the local language and offered the opportunity for potential subjects to ask questions. Investigators were available to answer any questions posed. Witnessed informed consent was obtained if the potential subject demonstrated understanding of the study and was willing to enroll. In the case of an illiterate subject, a thumbprint was obtained on the consent forms and a separate Witness to Consent form was signed by a literate witness who had observed the consent process.
Questionnaire
The study questionnaire was developed to obtain demographic, socioeconomic, and health information. Local medical authorities participated in questionnaire design. The questionnaire was modeled partly on the Kenya Demographic and Health surveys: 1988–1989 [19], 1998 [20], and 2002 [21]. The questionnaire was piloted in communities similar to those in the actual study, and was administered by trained interviewers. Before the interview ended, a principal investigator verified that recorded questionnaire responses were clear, complete, and internally consistent.
Laboratory
Thick and thin smears were prepared and read on-site by the project's laboratory technicians. A smear was considered to be negative if no P. falciparum parasites were observed in 100 high-powered fields. Subjects with positive smears were treated, free of charge, with an artemisinin-containing combination antimalarial, as recommended by the Kenyan Ministry of Health. This treatment constituted the study's direct benefit to the participants.
Data analysis
Questionnaire information included a categorical age variable (18–25, 26–35, 36–45, and 46+ years old), sex, literacy (defined as being able to read or write a simple line and being able to read a newspaper), and occupational group. Subjects reported whether or not they had been ill in the past three months and, if so, what illness they had (unsure, malaria, common cold, diarrhoea, HIV/AIDS, STI, respiratory, other). Additionally, subjects were asked to report whether they had used antimalarials in the past month and which antimalarials were taken. Malaria smear results were examined as a dichotomous variable (positive or negative).
Questionnaire and laboratory data were double-entered into a Microsoft Access® (Microsoft Co., Redmond, WA) database and cross-checked for accuracy. Stata version 7 for Windows (Stata Corp., College Station, TX) was used for all statistical analysis. To obtain a valid estimate of associations between exposure variables and parasitaemia, univariate analysis was performed with Pearson's Chi-square test and univariate logistic regression. Mantel-Haenszel stratified relative odds (ROs) were calculated prior to further multivariate analysis to detect possible interaction between variables examined. As no interaction was detected, these results are not reported. A multivariate logistic regression model was then created which included only variables found to be at least marginally significant in univariate analysis (district, literacy, occupation, illness in previous three months), calculating maximum likelihood estimates of the adjusted ROs and 95% confidence intervals. If a categorical variable did not demonstrate a log-linear correlation with the outcome, dummy dichotomous variables were created and used in the logistic regression model. A p-value of <= 0.05 is considered statistically significant, while a p-value of > 0.05 and <= 0.10 is reported as marginally significant.
Results
Study population
A total of 1,141 subjects were enrolled, representing 27.8% of the adult populations of the selected villages: 238 from Samburu, 442 from Malindi, and 461 from Busia. Of these, 731 (64.1%) were female and 410 (35.9%) were male. There was a marked difference in sex distribution in the different age ranges (p < 0.001), with younger males being less proportionally represented than younger females. However, there was no statistically significant difference in the age or sex distribution of subjects among the three districts (p = 0.104, p = 0.909, respectively). Of the 814 who answered questions about literacy, 322 (39.6%) were literate. Of the 1,110 subjects who responded to occupational questions, 585 (52.7%) were involved in agriculture, followed by home duties, which accounted for 167 (15.1%). No other occupational groups constituted more than 10% of the study population, so these other groups are not analysed separately.
Malaria smear results
Malaria smear results are summarized in Table 1.
District
Of the 1,141 subjects tested, 139 (12.2%) had a positive smear for P falciparum. The rate of positives varied markedly by district (p < 0.001), with 1.7% positive in Samburu, 7.2% in Malindi, and 22.3% in Busia.
Sociodemographics
Those who were literate had significantly higher parasitaemia rates than nonliterates with 13.7% of literates positive but only 6.9% of illiterates (p = 0.001). The rates of parasitaemia were lower in those engaged in home duties, at 2.4%, than those in agriculture, at 14.4%, or other employment areas, at 12.8% (p < 0.001). Neither age nor sex were associated with differences in parasitaemia rates (p = 0.872, p = 0.387, respectively).
Recent Illness History
Those who reported either a malarial or a diarrhoeal illness in the past three months had significantly increased rates of parasitaemia (p = 0.050, p = 0.010, respectively). Of the 307 with a history of malaria, 15.3% were parasite positive on enrollment, while for the 45 reporting diarrhoea, the parasitaemia rate was 25.9%. The parasitaemia rate for those with other reported illness or no illness was 10.5%.
Antimalarials
Among those who had taken antimalarials in the past four weeks and those who had not, 13.3% and 11.9%, respectively, were smear-positive (p = 0.625). Analysis for each medication separately failed to demonstrate any statistically significant association with smear positivity (p = 0.603).
Logistic regression models
Relative odds and 95% confidence intervals are presented in Table 1. A multiple logistic regression model that included variables found to be significant in univariate analysis demonstrated a statistically significant increased relative odds of parasitaemia for subjects in Malindi (p = 0.012) and Busia (p < 0.001) and those who were literate (p = 0.023), and a marginally significantly increased odds of parasitaemia in those with diarrhoeal illness in the previous three months (p = 0.067). No association remained of parasitaemia with primary occupation of home duties (p = 0.327) or with history of malaria in the previous three months (p = 0.849).
Discussion
Overall, this study found an association between parasitaemia and district of residence, literacy, and a history of diarrhoeal illness in the previous three months.
An interesting finding of this survey is that a history of diarrhoeal illness is a significant predictor for parasitaemia in Kenyan adults. The literature on the association of diarrhoea with malaria is somewhat conflicting and generally refers to the relationship between diarrhoea and acute malaria, while this survey correlates a history of diarrhoea in the past three months with a current parasitaemia. While diarrhoea is an often-cited symptom of malaria [22–24], there are several studies in the literature which demonstrate a negative correlation or lack of association between diarrhoea and malaria, both in non-immune travelers and in residents of endemic areas [25–28]. It is important to ascertain whether malaria is presenting as diarrhoeal illnesses in these populations to avoid missing the diagnosis of malaria and to avoid unnecessary antibacterial therapy for diarrhoea.
This positive relationship between a history of diarrhoea in the past three months and a positive malaria smear reached only marginal statistical significance in the aggregate, but was consistent in the individual districts, making type I error an unlikely explanation for this association. There are certainly many possible explanations for this association. It is of considerable interest that self-reported diarrhoea was associated with smear-positivity, whereas self-reported malaria was not. In these semi-immune populations, it is quite possible for diarrhoea to be the predominant symptom of malaria. As a diarrhoeal illnesses may not be recognized as malaria, treatment for malaria may not be sought or provided. While this difference in obtaining antimalarial therapy could explain a higher risk of parasitaemia among those with self-reported diarrhoea than self-reported malaria, this study does not support this as the explanation. While 30% of those with a history of malaria report taking an antimalarial in the previous month, 29% of those with a history of diarrhoea also report doing so. This difference is not statistically significant (p = 1.000). However, both of these groups were more likely to have taken an antimalarial than those with other recent reported illnesses, of whom 14% took antimalarials (RO = 2.62, 95% CI 1.84 – 3.75) or those with no reported illness, of whom 6% took antimalarials (RO = 6.52, 95% CI 4.06 – 10.48). Of those with a history of either diarrhoea or malaria, those with a positive malaria smear were no more or less likely to have taken an antimalarial in the past month than those with a negative smear (p = 0.531, p = 0.708). There was no difference in the antimalarials taken by those with diarrhoea and those with malaria (p = 0.869). Further study of this association of diarrhea with parasitaemia would be useful in providing guidance for evaluation of diarrhoea in these populations and perhaps would prevent inappropriate antibiotic therapies from being administered.
Literacy was another significant risk factor for parasitaemia in this study, even after controlling for potential confounding effects. This was a consistent finding in all three districts, although not reaching statistical significance for individual districts. This association cannot be attributed to occupation, recent antimalarial treatment, or other known factors. Literacy can directly impact health-seeking behaviors and also serves as a marker for other socioeconomic differences between individuals. It is plausible that differences in health-seeking behaviors or other socioeconomic factors would affect rates of malaria infection. However, literacy would have been anticipated to be protective against, not a risk factor for, infection as literacy and education are believed to be associated with more appropriate use of medical care [29–35]. There is some evidence, though, that higher educational level does not correlate with appropriate judgment of illness severity [36]. This observation of higher parasitemia rates among literate subjects warrants further study.
A clear finding of this study is that district of residence is the factor most strongly associated with differences in parasitaemia rates at the time of enrollment. Specifically, compared to those enrolled in Samburu, the subjects enrolled from Busia and, less so, Malindi, had higher odds of parasitaemia, even after adjustment for known potential confounders. The difference in ecologies of a semi-arid, a coastal, and a Lake Victoria basin district could well result in different disease transmission rates, particularly for vector-borne diseases [37–39]. District differences in public health infrastructure, sanitation, and cultural practices could also account for differences in disease occurrence and health perceptions.
There was no statistically significant association between history of antimalarial use in the past four weeks and the presence of parasitaemia on enrollment. This study did not have sufficient power to detect an association between specific antimalarial use and parasitaemia, even if such an association actually existed. Given an overall rate of 12.2% positivity, to find a 5% difference in malaria positivity with a power of 80% would require 826 subjects with a history of antimalarial use, a much higher number than the 187 enrolled.
There are several further limitations of this study. First is the use of self-reported data, particularly in the area of recent health histories and antimalarial usage. As noted above, the low number of patients with a recent history of antimalarial use limits the study's ability to investigate antimalarial resistance. Also, as previously noted, the enumeration unit was the village, not the individual subject.
Conclusion
While district of residence was the variable most highly predictive of parasitaemia among Kenyan adults surveyed, both a recent history of diarrhoeal illness and literacy were at least marginally statistically significant predictors. No other demographic or occupational variable, including age and sex, was associated with parasitaemia in these populations. Further study is required to determine the nature of these associations.
References
Country Health Profiles: Kenya. [http://www.afro.who.int]
Arudo J, Gimnig JE, ter Kuile FO, Kachur SP, Slutsker L, Kolczak MS, Hawley WA, Orago AS, Nahlen BL, Phillips-Howard PA: Comparison of government statistics and demographic surveillance to monitor mortality in children less than five years old in rural western Kenya. Am J Trop Med Hyg. 2003, 30-37. Suppl 4
Korenromp EL, Williams BG, Gouws E, Dye C, Snow RW: Measurement of trends in childhood malaria mortality in Africa: an assessment of progress toward targets based on verbal autopsy. Lancet Infect Dis. 2003, 3: 349-358. 10.1016/S1473-3099(03)00657-1.
Mbaisi A, Liyala P, Eyase F, Achilla R, Akala H, Wangui J, Mwangi J, Osuna F, Alam U, Smoak BL, Davis JM, Kyle DE, Coldren RL, Mason C, Waters NC: Drug susceptibility and genetic evaluation of Plasmodium falciparum isolates obtained in four distinct geographical regions of Kenya. Antimicrob Agents Chemother. 2004, 48: 3598-3601. 10.1128/AAC.48.9.3598-3601.2004.
Wongsrichanalai C, Pickard AL, Wernsdorfer WH, Meshnick SR: Epidemiology of drug-resistant malaria. Lancet Infect Dis. 2002, 2: 209-218. 10.1016/S1473-3099(02)00239-6.
Omar SA, Adagu IS, Gump DW, Ndaru NP, Warhurst DC: Plasmodium falciparum in Kenya: high prevalence of drug-resistance-associated polymorphisms in hospital admissions with severe malaria in an epidemic area. Ann Trop Med Parasitol. 2001, 95: 661-669. 10.1080/00034980120103234.
Wellems TE, Plowe CV: Chloroquine-resistant malaria. J Infect Dis. 2001, 184: 770-776. 10.1086/322858.
Oloo AJ, Adoyo A, Kariuki D, Boriga DA, Magiri C, Were JB, Koech DK: Sensitivity of falciparum malaria to chloroquine and amodiaquine in four districts of western Kenya (1985–1987). East Afr Med J. 1991, 68: 606-610.
Spencer HC, Masaba SC, Kiaraho D: Sensitivity of Plasmodium falciparum isolates to chloroquine in Kisumu and Malindi, Kenya. Am J Trop Med Hyg. 1982, 31: 902-906.
Amin AA, Marsh V, Noor AM, Ochola SA, Snow RW: The use of formal and informal curative services in the management of paediatric fevers in four districts in Kenya. Trop Med Int Health. 2003, 8: 1143-1152. 10.1046/j.1360-2276.2003.01140.x.
Nyamongo IK: Health care switching behaviour of malaria patients in a Kenyan rural community. Soc Sci Med. 2002, 54: 377-386. 10.1016/S0277-9536(01)00036-3.
Siringi S: Over-the-counter sale of antimalaria drugs stalls Kenyan disease strategy. Lancet. 2001, 357: 1862-10.1016/S0140-6736(00)05025-X.
Hamel MJ, Odhacha A, Roberts JM, Deming MS: Malaria control in Bungoma District, Kenya: a survey of home treatment of children with fever, bednet use and attendance at antenatal clinics. Bull World Health Organ. 2001, 79: 1014-1023.
Ongore D, Nyabola L: Role of shops and shopkeepers in malaria control. East Afr Med J. 1996, 73: 390-394.
Foster S: Treatment of malaria outside the formal health services. J Trop Med Hyg. 1995, 98: 29-34.
Ruebush TK, Kern MK, Campbell CC, Oloo AJ: Self-treatment of malaria in a rural area of western Kenya. Bull World Health Organ. 1995, 73: 229-236.
Snow RW, Peshu N, Forster D, Mwenesi H, Marsh K: The role of shops in the treatment and prevention of childhood malaria on the coast of Kenya. Trans R Soc Trop Med Hyg. 1992, 86: 237-239. 10.1016/0035-9203(92)90290-S.
Levy PLS: Sampling of populations: Methods and applications. 1999, New York: John Wiley & Sons, Inc
Kenya Demographin and Health Survey 1989. [http://www.measuredhs.com/start.cfm]
Kenya Demographic and Health Survey 1998. [http://www.measuredhs.com/start.cfm]
Central Bureau of Statistics MoH, Kenya Medical Research Institute, Centers for Disease Control and Prevention, and MEASURE DHS: Kenya Demographic and Health Survey 2003. 2004
Lutalo SK, Mabuwa C: Complications of seasonal adult malaria at a central hospital. Cent Afr J Med. 1990, 36: 268-273.
Kean BH, Reilly PC: Malaria – the mime. Recent lessons from a group of civilian travellers. Am J Med. 1976, 61: 159-164. 10.1016/0002-9343(76)90164-9.
Saeed IE, Ahmed ES: Determinants of malaria mortality among displaced people in Khartoum state, Sudan. East Mediterr Health J. 2003, 9: 593-599.
Casalino E, Le Bras J, Chaussin F, Fichelle A, Bouvet E: Predictive factors of malaria in travelers to areas where malaria is endemic. Arch Intern Med. 2002, 162: 1625-1630. 10.1001/archinte.162.14.1625.
Sodemann M, Jakobsen MS, Molbak K, Alvarenga IC, Martins C, Aaby P: Malaria parasitemia and childhood diarrhea in a peri-urban area of Guinea-Bissau. Am J Trop Med Hyg. 1999, 61: 336-338.
Sodeinde O, Gbadegesin RA, Ademowo OG, Adeyemo AA: Lack of association between falciparum malaria parasitemia and acute diarrhea in Nigerian children. Am J Trop Med Hyg. 1997, 57: 702-705.
Sodeinde O, Adeyemo AA, Gbadegesin RA, Olaleye BO, Ajayi-Obe KE, Ademowo OG: Interaction between acute diarrhoea and falciparum malaria in Nigerian children. J Diarrhoeal Dis Res. 1996, 14: 269-273.
Sharma AK, Aggarwal OP, Chaturvedi S, Bhasin SK: Is education a determinant of knowledge about malaria among Indian tribal population?. J Commun Dis. 2003, 35: 109-117.
Tanner M, Vlassoff C: Treatment-seeking behaviour for malaria: a typology based on endemicity and gender. Soc Sci Med. 1998, 46: 523-532. 10.1016/S0277-9536(97)00195-0.
Safeukui-Noubissi I, Ranque S, Poudiougou B, Keita M, Traore A, Traore D, Diakite M, Cisse MB, Keita MM, Dessein A, Doumbo OK: Risk factors for severe malaria in Bamako, Mali: a matched case-control study. Microbes Infect. 2004, 6: 572-578. 10.1016/j.micinf.2004.02.007.
Saeed IE, Ahmed ES: Determinants of acquiring malaria among displaced people in Khartoum state, Sudan. East Mediterr Health J. 2003, 9: 581-592.
Biritwum RB, Welbeck J, Barnish G: Incidence and management of malaria in two communities of different socio-economic level, in Accra, Ghana. Ann Trop Med Parasitol. 2000, 94: 771-778. 10.1080/00034980020013037.
Tarimo DS, Lwihula GK, Minjas JN, Bygbjerg IC: Mothers' perceptions and knowledge on childhood malaria in the holendemic Kibaha district, Tanzania: implications for malaria control and the IMCI strategy. Trop Med Int Health. 2000, 5: 179-184. 10.1046/j.1365-3156.2000.00537.x.
Tarimo DS, Urassa DP, Msamanga GI: Caretakers' perceptions of clinical manifestations of childhood malaria in holo-endemic rural communities in Tanzania. East Afr Med J. 1998, 75: 93-96.
Slutsker L, Chitsulo L, Macheso A, Steketee RW: Treatment of malaria fever episodes among children in Malawi: results of a KAP survey. Trop Med Parasitol. 1994, 45: 61-64.
Clarke SE, Brooker S, Njagi JK, Njau E, Estambale B, Muchiri E, Magnussen P: Malaria morbidity among school children living in two areas of contrasting transmission in western Kenya. Am J Trop Med Hyg. 2004, 71: 732-738.
Minakawa N, Sonye G, Mogi M, Githeko A, Yan G: The effects of climatic factors on the distribution and abundance of malaria vectors in Kenya. J Med Entomol. 2002, 39: 833-841.
Snow RW, Gouws E, Omumbo J, Rapuoda B, Craig MH, Tanser FC, le Sueur D, Ouma J: Models to predict the intensity of Plasmodium falciparum transmission: applications to the burden of disease in Kenya. Trans R Soc Trop Med Hyg. 1998, 92: 601-606. 10.1016/S0035-9203(98)90781-7.
Acknowledgements
The authors wish to thank Dr. Davy Koech, Director of the Kenya Medical Research Institute, for his generous support in making this research and publication possible. The authors also gratefully acknowledge the assistance of Shirley Segecha, Elizabeth Njogu, Ferdinard Adungo, Elias Muhidin, Salesio Mutembei, Sammy Leseita Lemonga, Jeremiah Kambe, Ruth Mupia, Dr. Steven Gaydos, Dr. Evan Scullin, Jennifer Gehrke, Sirley Peterson, and Norman Peterson; without their assistance, this study could not have been completed. The authors finally wish to thank Dr. Robert Chapman for his careful review and insightful input.
The opinions or assertions contained herein are the personal views of the authors and are not to be construed as official or reflecting the views of the Kenya Medical Research Institute, the United States Department of the Army or the United States Department of Defense.
Funding was provided by the Kenya Medical Research Institute, the United States Army Medical Research Unit – Kenya, the Walter Reed Army Institute of Research, and the United States Department of Defense Global Emerging Infectious Disease Surveillance and Response System.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
RLC served as overall Principal Investigator on the study, involved in all aspects of protocol design and execution, data analysis, and manuscript preparation. TP and FO designed the sociodemographic questionnaire, supervised field workers, and assisted in manuscript preparation. VOO designed the laboratory system and supervised the reading of malaria slides. NA conceived the study, supervised field and data entry personnel, and provided significant contribution to the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Coldren, R.L., Prosser, T., Ogolla, F. et al. Literacy and recent history of diarrhoea are predictive of Plasmodium falciparum parasitaemia in Kenyan adults. Malar J 5, 96 (2006). https://doi.org/10.1186/1475-2875-5-96
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2875-5-96