Abstract
The efficacy of pyrimethamine-sulfadoxine in the treatment of uncomplicated falciparum malaria in young children of a malaria holoendemic area in rural Burkina Faso is reported. Of 28 children treated with a standard single dose of pyrimethamine-sulfadoxine and followed-up over 14 days, only one Late Treatment Failure and four Late Parasitological Failures were observed, all with low-grade parasitaemia. In this area of very restricted use of pyrimethamine-sulfadoxine, the drug appears to be still sufficiently effective in the treatment of malaria. These findings provide further evidence for the justification of continued use of pyrimethamine-sulfadoxine as a second-line treatment for malaria in Burkina Faso.
Similar content being viewed by others
Background
The first cases of in vitro and in vivo chloroquine resistance in Burkina Faso were seen in 1983 and 1988, respectively, and reported clinical failure rates after use of chloroquine for treatment of uncomplicated malaria in children were already around 5% in the early 1990s [1]. More recently, the clinical failure rate of chloroquine in pre-school children was shown to be around 10% in western Burkina Faso [2, 3]. These findings have led to the conclusion that chloroquine still remains sufficiently effective after many years of resistance occurrence in this part of West Africa.
Little information exists on the dynamics of resistance development towards pyrimethamine-sulfadoxine, the usual second-line treatment choice in African countries with moderate chloroquine resistance. In Burkina Faso, only very low parasitological and clinical failure rates during use of have been reported in the past [1, 2].
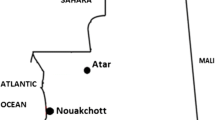
The efficacy of pyrimethamine-sulfadoxine in a rural area of north-western Burkina Faso is reported.
Methods
The study took place in six representative villages of the research area of the Centre de Recherche en Santé de Nouna (CRSN) in north-western Burkina Faso [4]. The Nouna area is a dry orchard savanna, populated mainly by subsistence farmers of different ethnic groups. Malaria is holoendemic but highly seasonal in the study area [4].
The study was nested into an ongoing insecticide-treated bed net (ITN) study [5]. All ITN cohort children from the six villages visited during a cross-sectional survey in October 2002 were enrolled if they fulfilled the following inclusion criteria: age >6 months, falciparum malaria (≥37.5°C axillary temperature + ≥2.000 Plasmodium falciparum parasites/μl blood in the absence of another obvious fever cause), absence of antimalarial treatment during previous two weeks, informed oral consent. All study children received a fully supervised single-drug treatment with 1/2 tablet Fansidar (12.5 mg pyrimethamine plus 250 mg sulfadoxine), taken from the essential drug stock of Nouna Health District. Children were observed for an hour after treatment. In the event of vomiting, they received another 1/2 tablet Fansidar.
Enrolled children were seen daily by village-based field staff over a 14-day period and, in case of fever (≥37.5°C axillary temperature), blood films were taken. Systematic blood slides were taken from all study children on day 0, 3, 7 and 14. Blood films were examined by two experienced laboratory technicians of the CRSN.
For the evaluation of treatment outcome, a modified definition of the WHO protocol for assessment of therapeutic efficacy of anti-malarial drugs in areas with intense transmission was used [6]. Early Treatment Failure (ETF) was defined as development of severe malaria on days 1–3 or axillary temperature ≥37.5°C on day 3 in the presence of parasitaemia, and Late Treatment Failure (LTF) as development of severe malaria and/or axillary temperature ≥37.5°C on days 4–14 in the presence of parasitaemia without previously meeting the criteria of ETF. Late Parasitological Failure (LPF) was defined as the presence of parasitaemia on day 7 and/or day 14. Approval for the study was granted by the Ethical Committee of the Heidelberg University Medical School and the Ministry of Health in Burkina Faso.
Results
Of 357 cohort children seen during the survey, 40 children (11%) were febrile and of those only 4 children had no detectable malaria parasitaemia. Overall, 28 children met the inclusion criteria and were enrolled into the study. At baseline, the mean age of these study children was 23 months (range 9–32), 17/28 (61%) were male, the mean temperature was 38.1°C (range 37.5–39.9), and the mean weight was 9.5 kg (range 5.5–12.9). The median baseline number of P. falciparum trophozoites was 13.100/μl (range 2.000–177.000), and 9/28 (32%) study children had P. falciparum gametocytes on day 0.
There was no loss to follow-up. No ETF was observed and only one LTF occurred in a 26 months old and 10.0 kg weighing male child, who had fever (38.7°C) and a low-grade parasitaemia (50/μl) on day 14. In addition, 7/28 (25%) study children still had measurable parasitaemia on day 3 (50–475/μl) without fever, and 4/28 (14%) study children had a LPF with low-grade parasitaemias (75–250/μl), two on day 7 and two on day 14 (all male). On day 7 and/or day 14, P. falciparum gametozytes were seen in 19/28 (68%) of study children.
Discussion
The findings from this study confirm the still very low level of resistance to pyrimethamine-sulfadoxine in West Africa [2, 7–9]. The likely reason for the continued efficacy of pyrimethamine-sulfadoxine is the low level of drug pressure in these areas, where the large majority of malaria cases is still treated with chloroquine [10]. These findings justify continued use of pyrimethamine-sulfadoxine for malaria second-line treatment in Burkina Faso, as in most of West Africa.
However, the question of which drug or drug combination should be the successor of chloroquine for malaria first-line treatment once this has reached unacceptable high failure rates remains largely unsolved for the poor malaria-endemic countries in sub-Saharan Africa (SSA) [11, 12]. Although, with regard to its still high efficacy, pyrimethamine-sulfadoxine would be a promising candidate for replacing chloroquine in West Africa, resistance is predicted to occur rapidly when the drug is used alone [11, 13]. Artemisinin combination therapy (ACT) is now recommended by the World Health Organization as a first-line treatment for malaria, but these combinations are comparably very expensive and their use in malaria control programmes will thus not be possible in many countries of SSA without sustainable external support [11, 14]. The combination of amodiaquine and pyrimethamine-sulfadoxine has recently been shown to be even more effective than ACT, and this combination has now been chosen as a pragmatic interim solution by some countries of SSA [15, 16]. Finally, the implications on the long-term effectiveness of intermittent pyrimethamine-sulfadoxine preventive treatment during pregnancy need to be taken seriously into consideration when using pyrimethamine-sulfadoxine as a first-line malaria therapy regimens in SSA [17].
References
Guigemdé TR, Aoba A, Ouedraogo JB, Lamizana L: Ten year surveillance of drug-resistant malaria in Burkina Faso (1982–1991). Am J Trop Med Hyg. 1994, 50: 699-704.
Tinto H, Zoungrana EB, Coulibaly SO, Ouedraogo JB, Traoré M, Guigemdé TR, Van Marck E, D'Alessandro U: Chloroquine and sulphadoxine-pyrimethamine efficacy for uncomplicated malaria treatment and haematological recovery in children in Bobo-Dioulasso, Burkina Faso during a 3-year period 1998–2000. Trop Med lnt Hlth. 2002, 7: 925-30. 10.1046/j.1365-3156.2002.00952.x.
Muller O, Traoré C, Kouyaté B: Clinical efficacy of chloroquine in young children with uncomplicated falciparum malaria – a community-based study in rural Burkina Faso. Trop Med Int Health. 2003, 8: 202-203.
Müller O, Becher H, Baltussen A, Ye Y, Diallo D, Konate M, Gbangou A, Kouyate B, Garenne M: Effect of zinc supplementation on malaria morbidity among West African children: a randomized double-blind placebo-controlled trial. B M J. 2001, 322: 1567-1572.
Müller O, Traoré C, Kouyaté B, Becher H: Effects of insecticide-treated mosquito nets (ITN) on malaria morbidity and all-cause mortality in infants of a malaria holoendemic area in rural Burkina Faso. Acta Trap. 2002, 83 (supplement): 71-72.
WHO: Assessment of therapeutic efficacy of antimalarial drugs for uncomplicated Falciparum malaria in areas with intense transmission. World Health Organization, Geneva, WHO/MAL/96.1077. 1996
Müller O, Boele van Hensbroek M, Jaffar S, Drakeley C, Okorie C, Joof D, Pinder M, Greenwood B: A randomized trial of chloroquine, amodiaquine, and pyrimethamine-sulfadoxine in Gambian children with uncomplicated malaria. Trop Med lnt Hlth. 1996, 1: 124-132. 10.1046/j.1365-3156.1996.d01-13.x.
Diourté Y, Djimdé A, Doumbo O: Pyrimethamine-sulfadoxine efficacy and selection for mutations in Plasmodium falciparum dihydrofolate and dyhydropterate synthetase in Mali. Am J Trop Med Hyg. 1999, 60: 475-78.
Von Seidlein L, Ouilligan P, Pinder M, Bojang K, Anyalebechi C, Gosling R, Coleman R, Ude JI, Sadiq A, Duraisingh M, Warhust D, Alloueche A, Targett G, McAdam K, Greenwood B, Walraven G, Olliaro P, Doherty T: Efficacy of artesunate plus pyrimthamine-sulfadoxine for uncomplicated malaria in Gambian children: a double-blind, randomised, controlled trial. Lancet. 2000, 355: 352-57. 10.1016/S0140-6736(99)10237-X.
Müller O, Traoré C, Becher H, Kouyaté B: Malaria morbidity, treatment seeking behaviour, and mortality in a cohort of young children in rural Burkina Faso. Trop Med lnt Health. 2003, 8: 290-296.
Bloland PB, Ettling M, Meek S: Combination therapy for malaria in Africa: hype or hope?. Bull World Health Organ. 2000, 78: 1378-88.
Winstanley P: Modern chemotherapeutic options for malaria. Lancet Inf Dis. 2001, 1: 242-50. 10.1016/S1473-3099(01)00119-0.
Greenwood B: Treating malaria in Africa. Br Med J. 2004, 328: 534-35. 10.1136/bmj.328.7439.534.
International Artemisinin Study Group: Artesunate combinations for treatment of malaria: meta-analysis. Lancet. 2004, 363: 9-17. 10.1016/S0140-6736(03)15162-8.
Dorsey G, Njama D, Kamya R, Cattamanchi A, Kyabayinze D, Staedke SG, Gasasira A, Rosenthal PJ: Sulfadoxine/pyrimethamine alone or with amodiaquine or artesunate for treatment of uncomplicated malaria: a longitudinal randomised trial. Lancet. 2002, 360: 2031-38. 10.1016/S0140-6736(02)12021-6.
Abacassamo F, Enosse S, Aponte JJ, Gómez-Olivé FX, Quintó L, Mabunda S, Barreto A, Magnussen P, Ronn AM, Thompson R, Alonso PL: Efficacy of chloroquine, amodiaquine, sulfadoxine-pyrimethamine and combination therapy with artesunate in Mozambican children with non-complicated malaria. Trop Med lnt Hlth. 2004, 9: 200-08. 10.1046/j.1365-3156.2003.01182.x.
Goodman CA, Coleman PG, Mills AJ: The cost-effectiveness of antenatal malaria prevention in sub-Saharan Africa. Am J Trop Med Hyg. 2001, 64 (1-2 Suppl): 45-56.
Acknowledgments
The study was funded by the Deutsche Forschungsgemeinschaft (SFB 544, Control of Tropical Infectious Diseases).
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
OM was the Principal Investigator of the study. He was responsible for the design of the study, drafted the manuscript and made all necessary corrections. CT was responsible for the fieldwork during data collection and supervised data entry. BK was responsible for the overall organisation in Burkina Faso and contributed to data analysis. All co-authors contributed to the writing of the paper.
Competing interests
None declared.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Müller, O., Traore, C. & Kouyate, B. Efficacy of pyrimethamine-sulfadoxine in young children with uncomplicated falciparum malaria in rural Burkina Faso. Malar J 3, 10 (2004). https://doi.org/10.1186/1475-2875-3-10
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2875-3-10