Abstract
Background
The erythrocyte binding antigen 175 (EBA-175) is a 175 kDa antigen of Plasmodium falciparum and plays a major role in erythrocyte recognition by the parasite. The antigen is also supposed to be partly responsible for the invasion of erythrocytes by merozoites. EBA-175 has been sequenced from the FCR-3 and CAMP strains of P. falciparum. The sequences were identical in most parts of the gene. Differences were apparent in a 423 bp segment in the FCR-3 strain, the F-Fragment, that is not found in the CAMP-strain and a 342 bp segment, the C-Fragment, which is present in the CAMP-strain but not in the FCR-3-strain. The aim of this study was to assess the distribution of the two EBA-175-alleles in the Lao PDR.
Materials & Methods
Altogether, 240 blood-samples were collected in two areas of the country: Attapeu in the south and Lung Namtha in the north. Subsequently, the material was scanned for the F-and C-fragments.
Results
In the whole study population, 52% carried the F-fragment, and 41% the C-fragment while seven percent of the patients were infected with at least two parasite strains and showed both alleles.
Conclusion
Distribution of the alleles showed significant differences between the north and the south province. Reasons for this include possible importation of different parasite strains from neighbouring countries.
Similar content being viewed by others
Introduction
The erythrocyte binding antigen-175 (EBA-175) of Plasmodium falciparum is localized in the merozoites and seems to be one of the key players during the fast cascade of interactions between the parasite and host molecules before the merozoite completely invades the erythrocyte [1]. Following initial contact of the merozoite with the erythrocyte, reorientation brings the apical end in contact with the erythrocyte surface [2]. The content of the apical organelles, including the rhoptries and micronemes, are discharged and a tight junction is formed between the erythrocyte membrane and the surface of the merozoite [3]. EBA-175 is localized in the micronemes and has been identified as the merozoite ligand that binds a sialic acid-dependent site on glycophorin A [4]. It therefore acts as a "bridge" between parasite and host cell.
EBA-175 is divided into a number of domains including three cysteine-rich regions (F1, F2 and C). F1 and F2 at the N-terminus are responsible for the glycophorin A binding on the erythrocyte membrane [4]. There is a very low amount of polymorphic regions in the cysteine-rich regions. Most EBA-175 sequences have this in common. An exception is the central part of the gene, region III. Here, sequence analysis of two different P. falciparum strains identified highly dimorphic segments, FCR-3 and CAMP [5–7]. The sequences of both strains are nearly identical, except for one dimorphic region in the FCR-3 strain (referred as F-Fragment) and one in the CAMP-stain (referred as C-Fragment).
The FCR-3 gene consists of 1462 amino acids (aa) whereas the CAMP strain gene is 1435 aa long. This length variation of 27aa is caused by differences in the 423 bp F-fragment (141aa) and the 342 bp (114aa) C-fragment. These two alleles are inserted at slightly different positions in region III of the EBA-175 gene where the F-fragment is 91aa upstream of the C-fragment. Parasite strains possess either one or the other fragment, never both [6]. Functions and potential effects of these dimorphic regions remain unclear. Earlier studies indicated that the dimorphic regions are also involved in the invasion process following the initial binding between merozoite and red blood cell. It is assumed that proteolytic cleavage of EBA-175 is followed by binding of the dimorphic regions to the glycophorin A backbone of the erythrocyte [8, 6].
The distribution of the two EBA-175 fragments has been studied in five African populations. Results did not indicate a natural selection concerning one of the two alleles [9]. In a serological study in The Gambia, it was shown that the C and F polymorphisms of EBA-175 were not associated with subsequent protection from clinical malaria [10].
The objective of this project was to study the distribution of the F- and C-fragment in a South East Asian country, the Lao PDR and to assess potential protective associations of the C and F dimorphisms in that region. Following two field studies in north and south Laos [11, 12], 240 blood samples derived from P. falciparum positive individuals were screened for EBA-175 alleles by a nested PCR method [13]. In order to link EBA-175 alleles to pathological findings, results were correlated with clinical data.
Materials and Methods
Parasite DNA samples
Blood samples and clinical data like age, sex, parasitaemia on day 0 and day 14 and clinical outcome were collected from 240 P. falciparum-infected individuals during two in vivo drug resistance studies in Lao PDR carried out by the University of Munich, Germany, the Ministry of Health, Lao PDR and the WHO Laos Office [10, 11]. The number of isolates and their exact sources were as follows: study site Attapeu province in the south of Lao PDR which borders Vietnam and Cambodia (figure 1). Community recruitment was carried out in all five districts of Attapeu province between August and October 2001 [11]. Altogether, 162 samples of patients were collected, clinical data were available for 147 of them. The other study was conducted from November 2001 till February 2002 in Luang Namtha province (northern Lao PDR, figure 1), bordering China and Myanmar [12]. Seventy-eight samples of P. falciparum positive individuals were collected and clinical data were available for 64 of them.
All samples were obtained with informed consent from patients and guardians. Ethical clearance was received from the ethics commission of the University of Munich and from the Ministry of Health of the Lao PDR. Blood was collected from consenting volunteers on Whatman filter paper and stored as dried blood samples. To prepare the DNA, 1–2 blood-spots were cut out of the filter, transferred into a tube containing 200 μl of 5% Chelex-100 (Bio-Rad Laboratories, Munich, Germany) and mixed intensively. After incubation in boiling water for 15 minutes the tube was vortexed for 30 seconds. The Chelex was separated by centrifugation (12,000 × g for two minutes, repeated twice) and the supernatant containing the DNA was transferred to a fresh tube [13].
PCR amplification and product analysis
The primers to detect the different EBA-175 fragments were used as described by Touré et al. [13]. EBA1 5'-CAAGAAGCAGTTCCTGAGGAA-3' (forward) and EBA2 5'-TCTCAACATTCATATTAACAATTC-3' (reverse) for the first amplification and EBA3 5'-GAGGAAAACACTGAAATAGCACAC-3' (forward) and EBA4 5'-CAATTCCTCC-AGACTGTTGAACAT-3' (reverse) for the second amplification. Amplification was performed under following conditions: 4 μl of DNA-Template for nest 1 and 2 μl PCR-product for nest 2, 1 μM of each Primer, 1 U Taq DNA polymerase (Qbiogene, Germany), 2 μl PCR-Buffer (Qbiogene, Germany) as supplied by the manufacturer and 200 μM dNTP in a 20 μl reaction volume. Denaturation at 94°C was performed for five minutes, followed by 29 cycles of denaturation at 94°C for one minute, primer-annealing at 56.4°C for one minute and extension at 72°C for another two minutes, with final extension at 72°C for three minutes. The outcome of the amplification was controlled by electrophoresis in an ethidium bromide-stained 1.5% agarose gel. For detection of the stained DNA, an ultraviolet transiluminator and specific detection software was used (Grabit®). A band size of 795 bp indicated the infection with the F-fragment and a band of 714 bp the infection with the C-fragment. Both bands in one lane indicated a mixed infection of the patient with at least two different parasite clones.
Statistic analysis
Statistical analysis was carried out using SPSS 11.5/SPSS Tables 11.5 for Windows. Alleles were scored separately for each of the 2 alleles. To investigate the difference between the two study sites a Chi2-test was performed (significance: p < 0.05). A Chi2-test was used to check for a correlation between fragment type and clinical outcome and fragment type and sex of the patients. In order to analyse correlations between parasitaemia on day 0, age of the patients and fragment type, the median-values were compared by Mann-Whitney-Test (significance: p < 0.05).
Results
Fragment distribution in Southern Laos
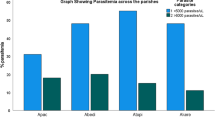
In the region of Attapeu, 162 patients with falciparum malaria were screened for the EBA-175 fragment types of the parasites. The distribution of the EBA-175-alleles was as follows: 46% F-fragment, 45% C-fragment and 9% mixed-infections.
Fragment distribution in Northern Laos
Seventy-eight blood samples of P. falciparum positive patients were screened for the two alleles of the EBA-175 gene in the province of Luang Namtha, in the north of Lao PDR. In contrast to the region around Attapeu, the northern area (study-site: Luang Namtha) showed different frequencies. The F-fragment was more frequently present (64%) than the C-fragment (33%) and 3% of the samples had mixed infections.
Comparison of the two study-sites
A mixed-infection consists of at least two single infections with two individual parasites in one patient. Therefore, samples with mixed infections can be counted for both fragment types. When comparing the two study-sites (figure 2), a significant difference between the two areas in Laos PDR (p = 0.031, Chi2-test) was noticeable. In Attapeu (n* = 176), the proportion of F-fragments was 51%, while 49% of the isolates had C-fragments while the distribution was 65% F-fragments and 35% C-fragments in the northern region around Luang Namtha (n* = 80). However, when looking at F- and C-fragments only without the mixed infection, statistical significance of this finding disappeared (p = 0.098, Chi2-test).
Correlation of fragment type and parasitaemia on day-0/clinical outcome/sex/age
The median-values of the parasitaemia on day 0 and the age of the patients where analyzed by Mann-Whitney-Test and showed no significant correlation between the fragment type and one of the parameters (data: table 1). However, individuals that carried a C-fragment showed a higher median-parasitaemia on day 0 in both study-sites. There was also no significant correlation between one of the two EBA-175-alleles and the sex of the patient, the distribution of the fragments was as follows. Attapeu: 52% F-fragment and 48% C-fragment in male patients and 48% F-fragments and 52% C-fragments in female (p = 0.585, Chi2-Test). In Luang Namtha, 64% F-fragments and 36% C-fragments were found in male and 61% F-fragments and 39% C-fragments in female patients (p = 0,795, Chi2-Test). An analysis of the data pool in regards of clinical outcome and in vivo resistance and their correlation to one of the two EBA-175-allele-groups did not show any significant results in both study-sites (Attapeu: p = 0,871; Luang Namtha: p = 0,527; Chi2-Test).
Discussion
A nested PCR method was used [12] in order to detect two alleles of EBA-175 (F-fragment and C-fragment) and to map their distribution in the Lao PDR. In this study with a combined pool of isolates derived from 240 patients in two surveys in north and south Laos, both fragment types had nearly the same distribution within the population. However, fragment types were not equally distributed between the two study sites. While isolates from Attapeu (Southern Laos) showed a almost equal distribution of the two fragments (51% F-fragment, 49% C-fragment), the F-fragment was clearly dominating in Luang Namtha, Northern Laos (65% F-fragment, 35% C-fragment) (figure 2). This difference is statistically significant when discounting mixed infections in patients who were infected with at least two different P. falciparum strains. This result confirms earlier work with samples from five African countries [9]. As in our study, Binks et al. had found a different distribution in five countries. In four of them (Nigeria, Gambia, Gabon, S. Africa) the F-fragment dominated, whereas the C-Fragment was dominating in the Sudan.
The higher prevalence of the F-fragment EBA-175 in the north of Laos is not readily explained. One of the reasons could be a difference in the parasite populations of the different regions in Lao PDR. The province of Attapeu borders Vietnam and Cambodia whereas the province of Luang Namtha borders Myanmar and China. An exchange of parasite strains over the local borders is possible. Genetic differences in the host population may also play a role when selection of specific fragments is involved. In Laos there are about 68 ethnic minorities that exhibit major differences and often live isolated from each other. The study-site in Attapeu is dominated by groups of Lao Thung and Lao Loum while the northern province of Luang Namtha is predominantly inhabited by Lao Sung, an entirely different minority. As Binks et al. [9] speculate in their study of the EBA-175 allele frequency in five African countries, a genetic difference in the human host population may be a reason for fragment selection. Obviously, a random selection of allelic frequencies may also be possible. More studies on larger populations are necessary to understand the pattern distribution of EBA-175 alleles.
Correlation of fragment type and clinical data showed that there was no significant correlation between parasitaemia on day-0, age, sex, clinical outcome and fragment type. However, the observed trend towards a higher parasitaemia at day 0 in patients with a C-fragment infection is potentially interesting. Further studies should be done to investigate whether parasites expressing a C-fragment enjoy a natural advantage compared those with a F-fragment.
References
Barnwell JW, Galinski MR: Invasion of vertebrate cells: erythrocytes. American Society of Microbiology Press. 1998, Washington, DC, 93-120.
Mitchell GH, Bannister LH: Malaria parasite invasion: interactions with the red cell membrane. CRC Crt Rev Oncol Hematol. 1988, 8: 225-310.
Aikawa M, Miller LH, Johnson J, Rabbege J: Erythrocyte entry by malaria parasites. J Cell Biol. 1978, 77: 72-88.
Sim BKL, Chitnis EC, Wasniowska K, Hadley TJ, Miller LH: Receptor and ligand domains for invasion of erythrocytes by Plasmodium falciparum. Science. 1994, 246: 1941-1944.
Kevin CK, David L: Determination of genetic variation within Plasmodium falciparum by using enzymatically amplified DNA from filter papers disks impregnated with whole blood. J Clin Microbiol. 1991, 29: 1171-1171.
Ware LA, Kain KC, Sim BKL, Haynes JD, Baird JK, Lanar DE: Two alleles of the 175-kilodalton Plasmodium falciparum erythrocyte binding antigen. Mol Biochem Parasitol. 1993, 60: 105-110. 10.1016/0166-6851(93)90033-T.
Sim BKL: EBA-175 an erythrocyte-binding ligand of Plasmodium falciparum. Parasitol Today. 1995, 11: 213-217. 10.1016/0169-4758(95)80080-8.
Kain KC, Orlandi PA, Haynes JD, Sim BKL, Lanar DE: Evidence for two-stage binding by the 175-kD erythrocyte binding antigen of Plasmodium falciparum. J Exp Med. 1993, 178: 1497-1505.
Binks RH, Baum J, Oduola AMJ, Arnot E, Babiker HA, Kremsner PG, Roper C, Greenwood BM, Conway DJ: Population genetic analysis of the Plasmodium falciparum erythrocyte binding antigen-155 (eba-175) gene. Mol Biochem Parasitol. 2001, 114: 63-70. 10.1016/S0166-6851(01)00240-7.
Okenu DMN, Riley EM, Bickle QD, Agomo PU, Barbose A, Daugherty JR, Lanar DE, Conway DJ: Analysis of human antibodies to erythrocyte binding antigen 175 of Plasmodium falciparum. Infect Immun. 2000, 68: 5559-5566. 10.1128/IAI.68.10.5559-5566.2000.
Schwöbel B, Jordan S, Vanisaveth V, Phetsouvanh R, Christophel EM, Phompida S, von Sonnenburg F, Jelinek T: Therapeutic efficiency of the combination chloroquine plus sulfadoxine/pyrimethamine compared to monotherapy with either chloroquine or sulfadoxine/ pyrimethamine in uncomplicated Plasmodium falciparum malaria in the Lao PDR. Trop Med Int Health. 2003, 8: 19-24. 10.1046/j.1365-3156.2003.00977.x.
Schwöbel B, Jordan S, Vanisaveth V, Phetsouvanh R, Christophel EM, Phompida S, von Sonnenburg F, Jelinek T: Chloroquine and sulfadoxine/pyrimethamine for treatment of uncomplicated P. falciparum malaria on the Laos-China and Laos-Myanmar border. Acta Tropica.
Touré FS, Mavoungou E, Mezu Me Ndong J, Tshipamba P, Deloron P: Eryhtrocyte binding antigen (EBA-175) of Plasmodium falciparum : improved genotype determination by nested polymerase chain reaction. Trop Med Int Health. 2001, 6: 767-769. 10.1046/j.1365-3156.2001.00789.x.
Long GW, Fries Lou, Watt GH, Hoffmann S: Polymerase chain reaction amplification from Plasmodium falciparum on dried blood spots. Am J Trop Med Hyg. 1995, 52: 344-346.
Acknowledgements
We thank Dr. Bounlay Phommasak (Deputy Director, Department of Hygiene and Prevention, Ministry of Health), the Center of Malariology, Parasitology and Entomology, Vientiane, the Attapeu Provincial Health Service, the Attapeu Provincial Malaria Station and all participating villagers from Attapeu for their cooperation, support and assistance in the field work.
We are also grateful to the WHO Office Vientiane for facilitating various stages of the project.
Financial support was received by the Friedrich Baur Trust, Munich, and the WHO Western Pacific Regional Office.
Author information
Authors and Affiliations
Corresponding author
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Dittrich, S., Schwöbel, B., Jordan, S. et al. Distribution of the two forms of Plasmodium falciparum erythrocyte binding antigen-175 (eba-175) gene in Lao PDR. Malar J 2, 23 (2003). https://doi.org/10.1186/1475-2875-2-23
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2875-2-23