Abstract
Background
Spreading resistance of Plasmodium falciparum to existing drugs calls for the search for novel anti-malarial drugs and combinations for the treatment of falciparum malaria.
Methods
In vitro and ex vivo investigations were conducted with fresh P. falciparum field isolates and culture-adapted P. falciparum clones to evaluate the anti-malarial potential of mirincamycin, a lincosamide, alone and in combination with tafenoquine (TQ), dihydroartemisinin (DHA), and chloroquine (CQ). All samples were tested in a histidine-rich protein 2 (HRP2) drug susceptibility assay.
Results
Interaction analysis showed additive to synergistic interaction profiles with these potential partner drugs, with an overall geometric mean fractional inhibitory concentration at 50% inhibition (FIC50) of 0.78, 0.80 and 0.80 for mirincamycin with TQ, DHA, and CQ, respectively. Antagonism was not found in any of the tested field isolates or clones. The strongest tendency toward synergy (i.e. the lowest FIC) was seen with a combination ratio of 1:0.27 to 1:7.2 (mean 1:2.7) for the combination with tafenoquine. The optimal combination ratios for DHA and CQ were 1:444.4 to 1:36,000 (mean 1:10,755.5) and 1:2.7 to 1:216 (mean 1:64.5), respectively. No evidence of an activity correlation (i.e. potential cross-resistance) with DHA, mefloquine, quinine or chloroquine was seen whereas a significant correlation with the activity of clindamycin and azithromycin was detected.
Conclusions
Mirincamycin combinations may be promising candidates for further clinical investigations in the therapy and prophylaxis of multidrug-resistant falciparum malaria or in combination with 4 or 8-aminoquinolines for the treatment and relapse prevention of vivax malaria.
Similar content being viewed by others
Background
Artemisinin-based combination therapy (ACT) has been adopted as first-line treatment for Plasmodium falciparum malaria in virtually all malaria-endemic countries. In the view of spreading anti-malarial drug resistance and the emergence of the first cases of compromised susceptibility to artemisinins along the Thai-Cambodian border the development of novel compounds and combinations for the treatment of falciparum malaria has become an issue of utmost importance [1, 2]. First studies conducted in 1969 and 1970 in rhesus monkeys infected with Plasmodium cynomolgi, a malaria parasite of monkeys similar to Plasmodium vivax, have shown that mirincamycin, a synthetically-produced lincosamide antibiotic similar to clindamycin, has substantial antiplasmodial activity for prophylaxis as well as for radical cure in animal models [3, 4]. Moreover in the above-mentioned P. cynomolgi model mirincamycin was shown to be superior compared to clindamycin in both, prophylaxis and radical cure. In 1985 Schmidt et al. showed that concomitant administration of mirincamycin improved the hypnozoitocidal efficacy of primaquine in a P. cynomolgi model suggesting that the primaquine dose required for radical cure could be reduced by one-half to two-thirds by coadministration with mirincamycin [5]. In 2010, Held et al.[6] assessed the in vitro activity of mirincamycin in P. falciparum field isolates from Gabon and indicated that mirincamycin is more active than the comparator drugs clindamycin and doxycycline. In Gabon, the observed mean IC50 measure after six days of incubation was 10,000-fold lower than on day 3, suggesting a slow onset of action (delayed death phenomenon) as previously described for several other antibiotics [6–8]. A recent study by Khemawoot et al. found a more than 100-fold increased potency against field isolates of P. falciparum cultured ex vivo in primate plasma compared to in vitro investigations with the W2 clone [9]. A challenge for the radical cure of P. vivax remains the haemolytic toxicity of primaquine in G6PD-deficient individuals. Earlier studies suggest that mirincamycin may improve the efficacy of 8-aminoquinolines, thereby potentially allowing for lower doses and reducing toxicity when given in combination [5].
Therefore, mirincamycin has been investigated as a promising combination partner for prophylaxis and treatment of falciparum malaria.
Methods
Study area
The study was carried out at the MARIB (Malaria Research Initiative Bandarban) field site in Bandarban in southeastern Bangladesh and at the laboratories of the Medical University of Vienna, Austria.
Ethics
Written informed consent was obtained from all study participants or their legal representatives and the study protocol was approved by the Ethical Review Committees of the ICDDR,B and the Medical University of Vienna.
Sampling
Blood samples were taken from male and non-pregnant female patients aged 8 to 65 years, presenting with microscopically confirmed P. falciparum monoinfections and parasite densities between 1,000 and 100,000 asexual parasites per μl. Blood samples exceeding 1% parasitemia were diluted with uninfected red blood cells before testing. Pregnant or breastfeeding women and patients with anti-malarial drug therapy in the preceding 30 days were excluded from participation.
Drug susceptibility testing
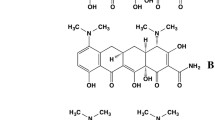
Mirincamycin (4’-trans-mirincamycin hydrochloride, molecular weight [MW] 475.47) was provided by Richard Westerman (Maldevco), tafenoquine (MW 463.49) by GlaxoSmithKline (GSK), clindamycin hydrochloride (MW 461.44), azithromycin (MW 748.98), dihydroartemisinin (MW 284.3), chloroquine diphosphate (MW 515.90), quinine sulphate (MW 782.96) and mefloquine hydrochloride (MW 414.77) were obtained from Sigma Aldrich. All drugs were dissolved in 70% ethanol to obtain a 1 mg/ml stock solution.
All samples were cultured for 72 hours to allow for a direct comparison among all test substances and combinations and growth inhibition assessed using the histidine-rich-protein 2 (HRP2) in vitro drug susceptibility assay. The culture and enzyme linked immunosorbent assay (ELISA) were performed as previous described [8, 10, 11].
To investigate interaction profiles and most effective ratio of concentrations of mirincamycin in combination with standard anti-malarials, fresh P. falciparum field isolates and culture-adapted P. falciparum clones K1 (chloroquine-resistant) and 3D7 (chloroquine-sensitive) were tested in checkerboard assays and data analysis was done as previously described [11–13]. Checkerboards assessing optimum concentrations of various drugs in combination were performed by diluting trans-mirincamycin (MIR 27.43 to 20,000 ng/ml) vertically and either chloroquine (CQ 3.43 to 2,500 ng/ml), tafenoquine (TQ 34.29 to 25,000 ng/ml) or dihydroartemisinin (DHA 0.02 – 15 ng/ml) horizontally in a three-fold serial dilution using a standard 8x8 well design on microtiter plates.
In addition single compounds were testes with fresh P. falciparum field isolates in the presence of three-fold serial dilutions of the anti-malarial drugs trans-mirincamycin (MIR; 137.2 to 100,000 ng/ml), clindamycin (CLM; 68.6 to 50,000 ng/ml), azithromycin (AZM; 68.6 to 50,000 ng/ml), dihydroartemisinin (DHA; 0.034 to 25.0 ng/ml), chloroquine (CHL; 3.4 to 2,500 ng/ml), quinine (QNN; 3.4 to 2,500 ng/ml) and mefloquine (MEF; 0.3 to 250 ng/ml) and subsequently growth inhibition was quantified in a HRP2 ELISA. In a subset of samples trans-mirincamycin and clindamycin were also tested after 24 h incubation using the WHO microtest [14].
Data analysis
The 50 and 90% inhibitory concentrations (IC50s and IC90s, respectively) were calculated from optical density readings by nonlinear regression analysis. ICs were used to calculate fractional inhibitory concentrations (FICs) as previously described [11, 13]. Isobolograms were plotted to demonstrate synergism (FIC < 0.5) and/or antagonism (FIC > 2) for drug combinations. Activity correlations were calculated by nonparametric correlation analysis (Spearman).
Results
Results of mirincamycin in combination with DHA, CQ and TQ are shown in Table 1 and Figure 1. All combinations with mirincamycin were additive with a slight trend to synergism, with an overall geometric mean fractional inhibitory concentration at 50% inhibition (FIC50) of 0.78, 0.80 and 0.80 for TQ, DHA, and CQ, respectively. Antagonism was not detected for any of the tested field isolates or clones. The highest level of synergism (i.e. the lowest FICs) was found for the combination of tafenoquine with mirincamycin at a ratio of 1:0.27 to 1:7.2 (mean 1:2.7). The optimal combination ratios were 1:444.4 to 1:36,000 (mean 1:10,755.5) and 1:2.7 to 1:216 (mean 1:64.5) for DHA and CQ, respectively.
Isobolograms of mirincamycin in combination with tafenoquine, dihydroartemisinin and chloroquine. Isobolograms for the checkerboards assays of mirincamycin in combination with tafenoquine, dihydroartemisinin and chloroquine at various concentration ratios for all successfully tested isolates at FIC50 level. All individual data points (pooled FIC50s) at various concentration ratios are presented on the left hand side, isobolograms on the right side point out the geometric mean of the individual data points. The straight lines in each panel are representing the type of interaction. Data points below the 0.5-line show synergism (FIC < 0.5), around the 1.0-line are additive (FIC 0.5-2) and above the 2-line are antagonistic (FIC > 2).
Out of a total of 55 patient samples 43 (78.2%; 95% confidence interval [CI]: 64.6 to 87.8) were successfully tested with a geometric mean parasite density of 7,646 per μL (95% CI: 5,399 to 10,827). The geometric mean of the 50% inhibitory concentration (IC50) for trans-mirincamycin was 1,212.6 nM (N = 43; 95% CI: 703.9 to 2,088.9) and the corresponding value for clindamycin was 880.4 nM (N = 43; 95% CI: 469.7 to 1,650.1). IC50, IC90, IC99 values with 95% confidence intervals for all drugs tested are shown in Table 2. No correlation was found between parasite density and inhibitory concentrations (IC50) of mirincamycin (R = 0.14; P = 0.4) and clindamycin (R = 0.10; P = 0.5) suggesting little influence of the inoculum size on the validity of in vitro assays. Individual IC values were calculated for all drugs tested in parallel and compared by nonparametric correlation analysis to determine potential cross-sensitivity and/or cross-resistance patterns between the drugs. Mirincamycin showed significant activity correlation with clindamycin (R = 0.64; P = 0.0002; N = 28) and azithromycin (R = 0.390; P = 0.040; N = 28) but no evidence of a correlation with any of the other tested anti-malarials (dihydroartemisinin: R = 0.269; P = 0.166; N = 28, mefloquine: R = 0.031; P = 0.875; N = 28, quinine: R = 0.025; P = 0.901; N = 28 and chloroquine: R = 0.319; P = 0.098; N = 28).
IC50s for trans-mirincamycin and clindamycin were 111 and 79 times higher after only 24 h incubation than after 72 h incubation, suggesting a slow mode of action in malaria parasites.
Discussion
So far there is only limited evidence for the in vitro[6] and ex vivo activity [9] of mirincamycin. P. cynomolgi animal models have proven that mirincamycin was curative even when given as monotherapy [3, 4]. Interestingly, the substance seems to show considerable activity against hypnozoites [4], and may enhance the effect of primaquine when given in combination [5].
For the first time, these results prove that mirincamycin has an additive mode of interaction in vitro with a slight trend to synergism when combined with various standard anti-malarials. Similar drug interaction profiles were found 2003 by Ramharter et al. for clindamycin in combination with DHA where effective concentrations of clindamycin were comparable to our results for mirincamycin [15]. Subsequently conducted clinical trials have proven high efficacy of clindamycin in combination with conventional anti-malarial drugs [16]. Clinical studies will need to show in how far this is also the case for mirincamycin.
8-aminoquinolines (like primaquine and tafenoquine) can cause severe haemolysis in individuals with G6PD deficiency. The challenge is therefore either to improve the efficacy and thereby potentially reduce the dose of 8-aminoquinolines with new combination partners possibly resulting in a reduced risk of haemolysis or to overcome this side effect with safer replacement drugs.
Mirincamycin alone or in combination (e.g. with 8-aminoquinolines) may be a promising candidate for malaria prophylaxis in nonimmune subjects, such as tourists and soldiers and could potentially help to enhance the hypnozoitocidal activity of 8-aminoquinolines by concomitant administrion, as previously demonstarted in a P. cynomolgi model [4, 5]. A lower dose could potentially also result in improved safety of 8-aminoquinolines (e.g. in glucose-6-phosphatedehydrogenase-deficient subjects).
Limitations of this study include all potential shortcomings of an in vitro study as well as the potential bias arising from the fact that only P. falciparum has been tested which cannot be extrapolated to P. vivax or P. ovale in the absence of a well-established culture model [17]. Also among 8-aminoquinolines only tafenoquine was tested in this study, which in recent studies has demonstrated high efficacy in the treatment and relapse prevention of vivax malaria in combination with chloroquine [18]. However, currently primaquine remains the only 8-aminoquinolone widely used for P. vivax radical cure.
Conclusions
The study showed that mirincamycin has additive to synergistic interaction in combination with different classes of anti-malarials, exhibits no activity correlation with traditional anti-malarials and exerts substantial anti-malarial activity on its own. As a consequence mirincamycin may be a potential candidate for clinical exploration either in combination with faster acting anti-malarials in the treatment of multidrug-resistant falciparum malaria or in combination with other drugs for the treatment of non-falciparum malaria.
References
Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM: Artemisinin resistance in Cambodia 1 (ARC1) study consortium: evidence of artemisinin-resistant malaria in western Cambodia. N Engl J Med. 2008, 359: 2619-2620. 10.1056/NEJMc0805011.
Takala-Harrison S, Clark TG, Jacob CG, Cummings MP, Miotto O, Dondorp AM, Fukuda MM, Nosten F, Noedl H, Imwong M, Bethell D, Se Y, Lon C, Tyner SD, Saunders DL, Socheat D, Ariey F, Phyo AP, Starzengruber P, Fuehrer HP, Swoboda P, Stepniewska K, Flegg J, Arze C, Cerqueira GC, Silva JC, Ricklefs SM, Porcella SF, Stephens RM, Adams M: Genetic loci associated with delayed clearance of Plasmodium falciparum following artemisinin treatment in Southeast Asia. Proc Natl Acad Sci U S A. 2013, 110: 240-245. 10.1073/pnas.1211205110.
Powers KG: Activity of chlorinated lincomycin analogues against Plasmodium cynomolgi in rhesus monkeys. Am J Trop Med Hyg. 1969, 18: 485-490.
Schmidt LH, Harrison J, Ellison R, Worcester P: The activities of chlorinated lincomycin derivatives against infections with Plasmodium cynomolgi in Macaca mulatta. Am J Trop Med Hyg. 1970, 19: 1-11.
Schmidt LH: Enhancement of the curative activity of primaquine by concomitant administration of mirincamycin. Antimicrob Agents Chemother. 1985, 27: 151-157. 10.1128/AAC.27.2.151.
Held J, Westerman R, Kremsner PG, Mordmüller B: In vitro activity of mirincamycin (U24729A) against Plasmodium falciparum isolates from Gabon. Antimicrob Agents Chemother. 2010, 54: 540-542. 10.1128/AAC.01090-09.
Dahl EL, Rosenthal PJ: Multiple antibiotics exert delayed effects against the Plasmodium falciparum apicoplast. Antimicrob Agents Chemother. 2007, 51: 3485-3490. 10.1128/AAC.00527-07.
Starzengruber P, Thriemer K, Haque R, Khan WA, Fuehrer HP, Siedl A, Hofecker V, Ley B, Wernsdorfer WH, Noedl H: Antimalarial activity of tigecycline, a novel glycylcycline antibiotic. Antimicrob Agents Chemother. 2009, 53: 4040-4042. 10.1128/AAC.00312-09.
Khemawoot P, Saunders D, Rasameesoraj M, Melendez V, Imerbsin R, Ohrt C, Fracisco S, Teja-Isavadharm P: Absolute bioavailability of cis-mirincamycin and trans-mirincamycin in healthy rhesus monkeys and ex vivo antimalarial activity against Plasmodium falciparum. Antimicrob Agents Chemother. 2011, 55: 5881-5886. 10.1128/AAC.01619-10.
Noedl H, Attlmayr B, Wernsdorfer WH, Kollaritsch H, Miller RS: A histidine-rich protein 2-based malaria drug sensitivity assay for field use. Am J Trop Med Hyg. 2004, 71: 711-714.
Noedl H, Krudsood S, Leowattana W, Tangpukdee N, Thanachartwet W, Looareesuwan S, Miller RS, Fukuda M, Jongsakul K, Yingyuen K, Sriwichai S, Ohrt C, Knirsch C: In vitro antimalarial activity of azithromycin, artesunate, and quinine in combination and correlation with clinical outcome. Antimicrob Agents Chemother. 2007, 51: 651-656. 10.1128/AAC.01023-06.
Ganesh D, Fuehrer HP, Starzengrüber P, Swoboda P, Khan WA, Reismann JA, Mueller MS, Chiba P, Noedl H: Antiplasmodial activity of flavonol quercetin and its analogues in Plasmodium falciparum: evidence from clinical isolates in Bangladesh and standardized parasite clones. Parasitol Res. 2012, 110: 2289-2295. 10.1007/s00436-011-2763-z.
Berenbaum MC: A method for testing for synergy with any number of agents. J Infect Dis. 1978, 137: 122-130. 10.1093/infdis/137.2.122.
World Health Organization: In vitro test (mark II) for the assessment of the response of Plasmodium falciparum to chloroquine, mefloquine, quinine, sulfadoxine/pyrimethamine and amodiaquine. [http://www.who.int/malaria/publications/atoz/markiii.pdf]
Ramharter M, Noedl H, Winkler H, Graninger W, Wernsdorfer WH, Kremsner PG, Winkler S: In vitro activity and interaction of clindamycin combined with dihydroartemisinin against Plasmodium falciparum. Antimicrob Agents Chemother. 2003, 47: 3494-3499. 10.1128/AAC.47.11.3494-3499.2003.
Ramharter M, Oyakhirome S, Klein Klouwenberg P, Adégnika AA, Agnandji ST, Missinou MA, Matsiégui PB, Mordmüller B, Borrmann S, Kun JF, Lell B, Krishna S, Graninger W, Issifou S, Kremsner PG: Artesunate-clindamycin versus quinine-clindamycin in the treatment of Plasmodium falciparum malaria: a randomized controlled trial. Clin Infect Dis. 2005, 40: 1777-1784. 10.1086/430309.
Noulin F, Borlon C, Van Den Abbeele J, D'Alessandro U, Erhart : 1912–2012: a century of research on Plasmodium vivax in vitro culture. Trends Parasitol. 2013, 29: 286-294. 10.1016/j.pt.2013.03.012.
Llanos-Cuentas A, Lacerda MV, Rueangweerayut R, Krudsood S, Gupta SK, Kochar SK, Arthur P, Chuenchom N, Möhrle JJ, Duparc S, Ugwuegbulam C, Kleim JP, Carter N, Green JA, Kellam L: Tafenoquine plus chloroquine for the treatment and relapse prevention of Plasmodium vivax malaria (DETECTIVE): a multicentre, double-blind, randomised, phase 2b dose-selection study. Lancet. 2014, 383: 1049-1058. 10.1016/S0140-6736(13)62568-4.
Acknowledgements
We thank all study participants, the staff of the Sadar Hospital Bandarban, the Civil Surgeon’s office Bandarban and the Ministry of Health and Family Welfare for their support and cooperation. We thank the Karl Landsteiner Gesellschaft for financial support, GSK for providing tafenoquine and Richard Westerman (Maldevco) for the mirincamycin supply.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors have declared that they have no competing interests.
Authors’ contributions
HN contributed to all steps from elaboration to the final review (study design, study coordination, overall supervision, data analysis and manuscript review). H-PF, DG PS and PSw carried out the in vitro studies. PS and PSw supervised and carried out patient samples collection in the field. PS wrote the first draft of the manuscript. PSw and H-PF contributed to the writing of the manuscript. RH helped to design the study protocol, monitored laboratory quality and corrected the manuscript. WAK participated in the coordination of patient samples collection in the field, drafted the manuscript and helped to analyze the data. WG helped to design the study protocol and revised the final manuscript. All authors read and gave their consent to the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Starzengruber, P., Fuehrer, HP., Swoboda, P. et al. Mirincamycin, an old candidate for malaria combination treatment and prophylaxis in the 21st century: in vitro interaction profiles with potential partner drugs in continuous culture and field isolates. Malar J 13, 228 (2014). https://doi.org/10.1186/1475-2875-13-228
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2875-13-228