Abstract
Background
Malaria transmission in most of Latin America can be considered as controlled. In such a scenario, parameters of baseline immunity to malaria antigens are of specific interest with respect to future malaria eradication efforts.
Methods
A cross-sectional study was carried out in two indigenous population groups in Amazonas/Venezuela. Data from the regional malaria documentation system were extracted and participants from the ethnic groups of the Guahibo (n = 180) and Piaroa (n = 295) were investigated for the presence of Plasmodium parasites and naturally acquired antibodies to Plasmodium falciparum antigens in serum. The GMZ2 vaccine candidate proteins MSP3 and GLURP were chosen as serological markers.
Results
The incidence of P. falcip arum in both communities was found to be less than 2%, and none of the participants harboured P. falciparum at the time of the cross-sectional. Nearly a quarter of the participants (111/475; 23,4%) had positive antibody titres to at least one of the antigens. 53/475 participants (11.2%) were positive for MSP3, and 93/475 participants (19.6%) were positive for GLURP. High positive responses were detected in 36/475 participants (7.6%) and 61/475 participants (12.8%) for MSP3 and GLURP, respectively. Guahibo participants had significantly higher antibody titres than Piaroa participants.
Conclusions
Considering the low incidence of P. falciparum, submicroscopical infections may explain the comparatively high anti-P. falciparum antibody concentrations.
Similar content being viewed by others
Background
To date, malaria is among the top ten causes of death in low-income countries [1]. In Venezuela, particularly the southern states of Bolivar and Amazonas are affected by malaria transmission. However, mortality is insignificant and malaria can be considered as controlled [2]. Amazonas (180,145 km²) covers an area nearly twice as big as Portugal and is inhabited by approximately 150,000 persons. Roughly half of the population is of indigenous origin and - although the absolute number of cases is low - Amazonas has the highest malaria incidence per capita in Venezuela (2007: 68.4 cases/1,000 inhabitants). Overall, the main malaria species is Plasmodium vivax (ca. 80%) followed by Plasmodium falciparum (ca 20%, with declining tendency). Plasmodium malariae is only occasionally detected [3, 4].
As drug resistance continues to be a major problem, an effective malaria vaccine against P. falciparum would be a powerful tool in the control of malaria [5, 6]. The vaccine candidate GMZ2 is a fusion protein of P. falciparum merozoite surface protein 3 (MSP3) and glutamate rich protein (GLURP), which has been evaluated during phase I trials as a promising vaccine candidate in Germany and Africa [7, 8]. Antibodies against both antigens have been shown to provide partial protection in Saimiri sciureus monkeys [9] and were associated with protection from human clinical malaria [10]. However, no data are available in respect to naturally acquired immunity to MSP3 and GLURP from populations of Latin America [11]. This is of interest since a malaria vaccine such as GMZ2 might be used in other continents than Africa where exposure to P. falciparum is low.
In 2008, a pilot programme for the evaluation of blister-packed treatment in distinct ethnic groups was initiated. An initial cross-sectional study was carried out in two indigenous population groups in order to gain knowledge about the micro-epidemiology of malaria in the project area. A second cross-sectional study is planned to close the project. As serological markers are useful indicators to measure transmission variations especially in low endemicity areas [12], immune responses to MSP3 and GLURP antigens were investigated as indicators of naturally acquired immunity to P. falciparum antigens.
Methods
Study population
The study took place in June 2009 in the municipality of Atures, Amazonas, Venezuela. Three indigenous communities were visited. They were inhabited by two ethnic indigenous population groups, the Guahibo (also: Guajibo, Wahibo, Hiwi, Jivi) and the Piaroa: 1) Platanillal (475 inhabitants, Guahibo); 2) Cerro de Oro (60 inhabitants, Guahibo); 3) Paria Grande (463 inhabitants, Piaroa). The distance between the communities is small (less than 20 km linear distance) and they are comparable with respect to ecological, geographical and malariological conditions such as distance to Anopheles breeding sites. The majority of residences in the communities are non-traditional governmental housing projects. The communities of Platanillal and Paria Grande have a health post, each with a malaria microscopist.
Ethical clearance, informed consent, and treatment
Ethical clearance was obtained from the institutional ethical committee of the Amazon Center for the Investigation and Control of Tropical Diseases 'Simón Bolívar', Autonomous Service, Puerto Ayacucho, Amazon State, Venezuela (SACAICET). Residents were informed about the ideas and procedures of the study, when necessary with the help of translators. All residents were invited to take part. Those consenting orally were interviewed and examined. Individuals with a blood smear positive for malaria were treated according to the national guidelines (P. falciparum: artesunate, mefloquine, and primaquine. P. vivax: chloroquine, primaquine) [13].
Data extraction of the regional malaria documentation system
Data from the regional malaria documentation system were extracted. Malaria cases detected in the health posts of Platanillal and Paria Grande before the study took place, from January 2003 to May 2009, were analysed.
Interviews and basic physical examination
Every participant, or the legal guardian, was interviewed using semi-structured interviews. Translators assisted if it was necessary, and standardized questions were phrased with the support of anthropologists. The structured part of the interviews concerned malaria antecedents, possession and use of mosquito nets, general condition, unspecific symptoms during the last seven days, and pregnancy. Every participant was examined physically including a check for splenomegaly and body temperature.
Smears and serum
Thick blood smears and thin films were taken from every participant, air-dried and stained for 45 min with 3% Giemsa using standard procedures1 [14]. Slides were read and re-read by trained professionals of the SACAICET and of the Regional Health Directory in Puerto Ayacucho. Ten ml of blood was taken from every participant into a vacutainer and centrifuged. Serum was stored at −20°C until further processing.
Recombinant antigens
Recombinant proteins were produced in Escherichia coli as described elsewhere [15]. The 48 kDa merozoite surface protein 3 (MSP3) is divided into two major allele types by sequence polymorphism. The C-terminal region of the molecule is highly conserved [16]. The 220 kDa glutamate-rich protein (GLURP) contains one non-repeat and two repeat regions. Both antigens are involved in antibody dependent cellular inhibition (ADCI) and are used as sub-units of the GMZ2 fusion protein [17]. For all experiments the conserved fragments MSP3212-318 and GLURP27-500 were used.
Antibody measurements
Serum antibodies to MSP3 and GLURP were measured applying a modified version of a quantitative ELISA [18]. In brief, microtitre plates were coated with antigens in a dilution of 0.5 mg/ml in PBS overnight at 4°C. After a first washing cycle (3 times) with PBS-T plus 0,5 mol/litre NaCl wells were blocked for one hour with a dilution of 30 g of defatted milk powder per litre PBS-T. As standard, after another washing cycle, duplicate rows were coated with samples, controls and a standard sample (with quantified high antibody concentration) in blocking buffer for two more hours. The standard sample was added in an X-fold serial dilution from 1/20 to 1/327,680. Samples and controls were added in duplicates in dilutions of 1/50 and 1/200. Samples with optical densities higher than the positive control were repeated at 1/800. After washing again, plates were incubated with peroxidase conjugated goat anti-human IgG (Caltag, 1/5,000) for one hour, washed, treated with TMB-One for 15 min in gloomieness until the reaction was stopped with sulphuric acid. Then absorbance was read at 450 nm. The standard sample was used to calculate IgG concentration of the other samples in mg/dl. Pooled serum from 20 individuals, never having lived in malaria-endemic areas, served as negative control. The arithmetic mean of negative controls was 0.0746 mg/dl (SD 0.0396 mg/dl) and 0.092 mg/dl (SD 0.0441 mg/dl) for MSP3 and GLURP, respectively.
Data capture and analysis
All data were subjected to plausibility, double-entered and checked for transcription errors in Epidata v3.0®. Optical densities (ODs) were averaged and normalized. The cut-off value for the difference between duplicates was set at 25%. If the difference was higher, the measurement was repeated. All results were converted to values in mg/dl using the positive standard serum. Positivity and high positivity of samples was defined as any OD higher than the mean of negative controls plus three and five standard deviations (SD), respectively. Statistical analysis was performed using SPSS 19® software. T-Tests were run to screen for significant differences between the variables subgroups concerning antibody titres, Chi-Square-Tests to learn about disparities in respect to antibody positivity. Age in years, sex, self-reported incidence of malaria episodes during the last 12 months and lifetime, possession and frequent utilization of mosquito nets and ethnic affiliation were included in a binary logistic model to predict anti-MSP3 and anti-GLURP antibody positivity. This quite conservative model has the advantage to show an Odds ratio (OR) for each expression of a variable. Furthermore, a linear regression model was performed to expose the influence of the aforementioned independent variables on the direct IgG-titre against the GMZ2-subunits.To do so, antibody levels had to be transformed to their decadic logarithm to gain Gaussian distribution. The resulting model was then de-logarithmized to show comparable and comprehensible results.
Results
Study population
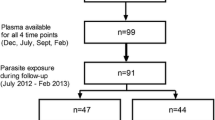
Four hundred and seventy-five persons participated in the study. Demographic data of participants and questionnaire results are summarized in Table 1.
Malaria infections in the two indigenous communities from 2003 to 2008
Platanillal
Within the six years preceding the cross-sectional study (2003 - 2008), the health post of Platanillal reported 573 cases of malaria in Guahibo patients (2003: 134 cases; 2004: 62 cases; 2005: 90 cases; 2006: 141 cases; 2007: 95 cases; 2008: 51 cases).
Paria grande
The health post of Paria Grande reported 270 cases of malaria in Piaroa patients within the six years preceding the cross-sectional study (2003: 11 cases; 2004: 65 cases; 2005: 29 cases; 2006: 70 cases; 2007: 74 cases; 2008: 21 cases). Of these, 45/573 cases (7.8%) and 36/270 cases (13.3%) were caused by P. falciparum in Platanillal and Paria Grande, respectively. All other infections were caused by P. vivax. P. malariae was not detected.
Malaria infections in the two indigenous communities from january 2009 to may 2009
Platanillal
Within the five months preceding the cross-sectional study (January 2009-May 2009), 154 slides were taken in the health post of Platanillal; 43/154 slides (27.9%) were positive for P. vivax, and 5/154 slides (3.2%) were positive for P. falciparum.
Paria grande
Within the five months preceding the cross-sectional study, 148 slides were taken in the health post of Paria Grande; 15/148 slides (10.1%) were positive for P. vivax, and none (0%) was positive for P. falciparum.
Clinical results
Participants (n = 475) complained about the following symptoms within the preceding seven days: headache (71; 14,9%), body ache (45; 9,5%), flu-like symptoms (101; 21,3%), cough (34; 7,2%), chills (5; 1,1%), fever (28; 5,9%), diarrhoea (46; 9,7%), abdominal pain (30, 6,3%), nausea (34, 7,2%), fatigue (14, 2,9%). The mean temperature of all participants was 37,02°C (Min. 35,8°C, Max. 38,9°C, SD. 0,4803). 9/475 participants (1.9%) had a body temperature over 38°C. None of the participants had palpable splenomegaly and none of the 475 participants was found positive for P. falciparum at the day of the cross-sectional study. Two participants (2/475; 0.4%) were found positive for P. vivax (both <100 parasites/μl). Both patients were from the Guahibo ethnic group and reported malaria antecedents. One patient was a 12-year-old anaemic boy (Hb 12.5 mg/dl) in reduced general condition and with normal body temperature (36.5°C) reporting chills during the last seven days. The other patient was a 26-year-old anaemic pregnant woman (Hb 9.7 mg/dl) with normal body temperature (37.1°C) complaining about a reduced general state of health.
Antibodies to MSP3 and GLURP
The cut-off value for a positive sample was set at 0.193 mg/dl and at 0.224 mg/dl for MSP3 and GLURP, respectively. 111/475 participants (23.4%) were positive for at least one of the antibodies. 53/475 participants (11.2%) were positive for MSP3, and 93/475 participants (19.6%) were positive for GLURP. 35/475 participants (7.4%) had positive antibody levels against both antigens. The average value (geometric mean) of positive samples was 0.36 mg/dl (95% CI 0.32 mg/dl - 0.41 mg/dl) and 0.47 mg/dl (95% CI 0.41 mg/dl - 0.55 mg/dl) for MSP3 and GLURP, respectively. The cut-off value for a high-positive sample was set at 0.27 mg/dl and at 0.31 mg/dl for MSP3 and GLURP, respectively. 78/475 participants (16.4%) were high-positive for at least one of the antibodies. 36/475 participants (7.6%) were high-positive for MSP3, and 61/475 participants (12.8%) were high-positive for GLURP. 19/475 participants (4%) had high-positive antibody levels for both antigens. The highest titres measured were 2.8 mg/dl and 3.36 mg/dl for MSP3 and GLURP, respectively.
Stratification for age and sex
Antibody titres were significantly increasing with age (Spearman Rank Test, RSpGLURP = 0.130, p = 0.005. RSpMSP3 = 0.259, p < 0.001). When the study population was grouped by age - each group with a span of 10 years - a significantly higher number of positives and high-positives was seen in the older age groups (ANOVA: positives: pMSP3 < 0.001, pGLURP = 0.001, high-positives: pMSP3 < 0.001, pGLURP = 0.028). No significant differences in antibody titres or positivity rates were found regarding the sex of the persons (T-test: pGLURP = 0.101, pMSP3 = 0.169, Chi-square: pGLURP = 0.101, pMSP3 = 0.184).
Stratification for possession and use of mosquito nets
Comparing possessors (428/475, 90.1%) and non-possessors (47/475, 9.9%) of mosquito nets, holders were found to have lower levels of GLURP (T-test, pGLURP < 0.001), but there was no significant difference respective to MSP3 (T-test, pMSP3 = 0.489). Participants who reported daily use of mosquito nets during the previous 30 nights were defined frequent users. 392/475 participants (82.5%) were found to be frequent users. No significant difference in antibody titres nor positivity rates were found between frequent users and the rest of the study population (T-test, pGLURP = 0.125, pMSP3 = 0.991; Chi-square-test, pGLURP = 0.182, pMSP3 = 0.084).
Stratification for self-reported malaria episodes
282/475 participants (59.4%) stated they had at least one malaria episode in their life, and 85/475 (17.9%) reported a malaria episode during the previous 12 months. Those who reported to have suffered malaria at least once in their life showed significantly higher IgG-levels than the group reporting no previous malaria episode. This difference was significant for MSP3 (T-test, pMSP3 = 0.032), but not for GLURP (T-test, pGLURP = 0.062). Those who stated a malaria episode within the previous 12 months had slightly more positive responses against both antigens. This difference was significant for GLURP and for MSP3 (Chi-square, pGLURP = 0.002; pMSP3 < 0.001).
Stratification for ethnic origin
Participants from the ethnic Guahibo group displayed significantly higher antibody titres and positivity rates for both antigens when compared to the ethnic Piaroa group (Table 2).
Binary logistic and linear regression model
The above-mentioned parameters were included in a binary logistic and a linear regression model to predict positivity and titres of antibodies against MSP3 and GLURP. In the binary logistic model, the parameters age, possession of mosquito nets, and ethnic origin had a significant outcome: For every year of age, risk of positivity raised with an OR of 1.03 for both MSP3 (CI: 1.018; 1.051, p < = 0.001) and GLURP (CI: 1.020; 1.049, p < = 0.001). Non-possession of a mosquito net increased the chance to have GLURP by 4.05-fold (CI: 1.258; 13.014, p < = 0.001). Guahibo individuals had a 8.04-fold (CI: 4.061; 15.898, p < = 0.001) chance for MSP3 antibody positivity compared to Piaroa individuals. With respect to GLURP, the chance for positivity was 2.81-fold higher for Guahibo in comparison to Piaroa individuals (CI: 1.677; 4.721, p < = 0.001). Results of the linear regression model are shown in Table 3.
Discussion
Results show that the two GMZ2 antigens are recognized by antibodies acquired through natural infections in the Venezuelan Amazon. Overall, the results correspond - except high responders - to rather low responses which are roughly two-fold higher than the cut-off value for positives. As antibody subclasses are of great importance [19] further studies on IG-subclasses have to show whether functional antibodies are acquired through natural exposure. The question if a GMZ2 vaccine would be effective in this area remains open, because antibodies stimulated by vaccines do not automatically protect as do naturally acquired antibodies [20]. In respecto to vaccine efficacy, only clinical trials with disease as endpoint can prove the impact of a vaccine.
The two main findings of this study were 1) the high prevalence of antibodies against conserved parts of MSP3 and GLURP antigens in the two population groups with low incidence of P. falciparum malaria, and 2) the significantly higher prevalence of MSP3 and GLURP antibodies in the Guahibo group when compared to the Piaroa group.
The total population of the Piaroa is about 12,000 persons. Anthropologists describe them as peaceful and egalitarian. Traditionally, the Piaroa's agroforestal subsistence strategy implicated small, dispersed and mobile ways of settlement in groups of about 50 individuals. Nowadays they are living in bigger communities mostly built by the Venezuelan government in the periphery of their ancestral territories, which they still use as cropland and hunting grounds [21].
The Guahibo consist of about 30,000 persons settling mainly around Puerto Ayacucho and neighbouring Colombian areas. As a patriarchal society, great importance is placed on the nuclear family. Traditionally, they inhabited vast flatlands in Colombia and Venezuela as nomadic foragers. Nowadays, they inhabit communities constructed by the Venezuelan government. They are mainly assimilated according to language and clothing style, but still are threatened by pauperisation [22].
The serological results of this study confirm previous investigations hinting to an elevated risk for malaria in the Guahibo population [2, 23]. Living conditions, socioeconomic parameters, adherence to medicaments, confidence in the health system, and cultural habits may explain the different transmission levels in the two ethnic groups under study. Different immune responses with different protection patterns in genetically different populations are also a possible factor [24, 25]. Further research involving multidisplinary expertise as well as members of the communities should focus on this "hot spot" of malaria transmission in the Venezuelan Amazon.
The positive correlation of antibody titeres and prevalences with age has been known for a long time [26]. When people live in an area endemic for malaria the chances of contact with the antigen raise with the years, and so do antibody titres and prevalences. Similarly, the chances of contact decrease with the use of mosquito nets. Such, as shown in other studies [27], a difference in GLURP antibody titres and prevalences could be observed between mosquito net users and non-users.
This cross-sectional study evaluated immune responses against two blood stage antigens considered as promising vaccine candidates on the basis of studies carried out in completely different settings. Samples were taken in the period of low transmission when the direct contact with P. falciparum parasites is expected to be minimal. Indeed, only two persons in nearly half a thousand participants were found harbouring parasites (2/475; 0.4%). Both patients were positive for P. vivax, none was positive for P. falciparum. Nevertheless, nearly a quarter of participants had antibodies to at least one of both antigens. As adding up immune responses to individual antigens might not be an appropriate procedure for results, which show - not surprisingly for outbred human populations - an extensive variation between individuals, it is important to note that 7.6% and 12,8% of participants had high antibody titres against MSP3 and GLURP, respectively. Possibly only high-positive antibody responses are relevant and/or specific results in this endemic area. Moreover, it should be taken into account that higher antibody responses might persist longer than lower ones.
Using the records of the health information system of Amazonas the level of malaria transmission in the communities during the years and months before the study was approximated. As the health posts of Platanillal and Paria Grande were comparable in the volume of slides taken per year (e.g. 2009: Platanillal, 280 slides; Paria Grande, 269 slides) and data of ethnic origin, origin of infection, and population census were available, the prevalence in both communities could be estimated for malaria in general, and for P. falciparum in particular. The average pan-malarial incidence was higher in the Guahibo population of Platanillal (ca 18%) than in the Piaroa population of Paria Grande (ca 8%). However, this was due to P. vivax infections, whereas the transmission of P. falciparum was surprisingly low in both population groups. Within a time period of 6.5 years, only 50 and 36 cases of P. falciparum were detected in Guahibo and Piaroa people of the health posts of Platanillal and Paria Grande, respectively, and the average incidence of P. falciparum was estimated to be less than two percent in both population groups, without a significant difference.
MSP3 and GLURP antibodies last six-12 months if no boost infection takes place [8]. In order to explain the phenomenon that antibodies were detected in more individuals than expected, submicroscopical infections must be considered as an influencing variable. The use of other antigens (for example, pre-erythrocytic antigens) might have led to other results, yet it can be assumed that conclusions would have differed slightly only. This is in line with previous investigations demonstrating asymptomatic carriers in this area [28]; interestingly, more than 20% of those who denied they ever suffered from any type of malaria had positive IgG titres. Another - yet to be proven - hypothesis would be the polyclonal activation of effector T killer cells and memory B-cells against P. falciparum antigens by P. vivax [29].
Controlled malaria is the result of an interplay of host defense systems, public health measures, ambiental conditions, behavioural features, and epidemiology and infection biology of the parasite. Interventions should be weighed carefully in order not to destabilize an established equilibrium. The epidemiology and immunology of controlled malaria might be subject of growing interest for malariologists and decision makers, as lessons learnt in low endemic areas could be instructive after eradication and control efforts have been successful in high endemic areas.
References
World Health Organization: The top 10 causes of death. Fact sheet N°310. (retrieved 21/09/2011), [http://www.who.int/mediacentre/factsheets/fs310/en/index.html]
Metzger WG, Giron AM, Vivas-Martínez S, González J, Charrasco AJ, Mordmüller BG, Magris M: A rapid malaria appraisal in the Venezuelan Amazon. Malar J. 2009, 8: 291-10.1186/1475-2875-8-291.
Metzger WG, Vivas-Martínez S, Rodriguez I, Gonçalves J, Bongard E, Fanello CI, Vivas L, Magris M: Malaria diagnosis under field conditions in the Venezuelan Amazon. Trans R Soc Trop Med Hyg. 2008, 102: 20-24. 10.1016/j.trstmh.2007.08.007.
Metzger WG, Vivas-Martínez S, Giron A, Vaccari E, Campos E, Rodríguez I, Miranda E, Terán E, Olivio L, Magris M: Assessment of routine malaria diagnosis in the Venezuelan Amazon. Trans R Soc Trop Med Hyg. 2011, 105: 262-268. 10.1016/j.trstmh.2011.01.002.
Smith DL, Klein EY, McKenzie FE, Laxminarayan R: Prospective strategies to delay the evolution of anti-malarial drug resistance: weighing the uncertainty. Malar J. 2010, 9: 217-10.1186/1475-2875-9-217.
Mordmüller B: New medicines for malaria. Wien Klin Wochensch. 2010, 122 (Suppl 1): 19-22.
Esen M, Kremsner PG, Schleucher R, Gässler M, Imoukhuede EB, Imbault N, Leroy O, Jepsen S, Knudsen BW, Schumm M, Knobloch J, Theisen M, Mordmüller B: Safety and immunogenicity of GMZ2 - a MSP3-GLURP fusion protein malaria vaccine candidate. Vaccine. 2009, 27: 6862-6868. 10.1016/j.vaccine.2009.09.011.
Mordmüller B, Szywon K, Greutelaers B, Esen M, Mewono L, Treut C, Mürbeth RE, Chilengi R, Noor R, Kilama WL, Imoukhuede EB, Imbault N, Leroy O, Theisen M, Jepsen S, Milligan P, Fendel R, Kremsner PG, Issifou S: Safety and immunogenicity of the malaria vaccine candidate GMZ2 in malaria-exposed, adult individuals from Lambaréné, Gabon. Vaccine. 2010, 28: 6698-6703. 10.1016/j.vaccine.2010.07.085.
Carvalho LJM, Oliveira SG, Theisen M, Alves FA, Andrade MCR, Zanini GM, Soe S, Druilhe P, Theisen M, Muniz JAPC, Daniel-Ribeiro CT: Immunization of Saimiri sciureus monkeys with Plasmodium falciparu merozoite surface protein-3 and glutamate-rich protein suggests that protection is related to antibody levels. Scand J Immunol. 2004, 59: 363-372. 10.1111/j.0300-9475.2004.01409.x.
Barry AE, Schultz L, Buckee CO, Reeder JC: Contrasting population structures of the genes encoding ten leading vaccine-candidate antigens of the human malaria parasite, Plasmodium falciparu. PLoS ONE. 2009, 4: e8497-10.1371/journal.pone.0008497.
Fowkes FJI, Richards JS, Simpson JA, Beeson JG: The relationship between anti-merozoite antibodies and incidence of Plasmodium falciparu malaria: A systematic review and meta-analysis. PLoS Med. 2010, 7: e1000218-10.1371/journal.pmed.1000218.
Bousema T, Youssef RM, Cook J, Cox J, Alegana VA, Amran J, Noor AM, Snow RW, Drakeley C: Serologic markers for detecting malaria in areas of low endemicity, Somalia, 2008. Emerging Infect Dis. 2010, 16: 392-399.
Grenfell P, Fanello CI, Magris M, Goncalves J, Metzger WG, Vivas-Martínez S, Curtis C, Vivas L: Anaemia and malaria in Yanomami communities with differing access to healthcare. Trans R Soc Trop Med Hyg. 2008, 102: 645-652. 10.1016/j.trstmh.2008.02.021.
Kilian AH, Metzger WG, Mutschelknauss EJ, Kabagambe G, Langi P, Korte R, von Sonnenburg F: Reliability of malaria microscopy in epidemiological studies: results of quality control. Trop Med Int Health. 2000, 5: 3-8. 10.1046/j.1365-3156.2000.00509.x.
Theisen M, Vuust J, Gottschau A, Jepsen S, Høgh B: Antigenicity and immunogenicity of recombinant glutamate-rich protein of Plasmodium falciparu expressed in Escherichia col. Clin Diagn Lab Immunol. 1995, 2: 30-34.
Borre MB, Dziegiel M, Høgh B, Petersen E, Rieneck K, Riley E, Meis JF, Aikawa M, Nakamura K, Harada M: Primary structure and localization of a conserved immunogenic Plasmodium falcipar m glutamate rich protein (GLURP) expressed in both the preerythrocytic and erythrocytic stages of the vertebrate life cycle. Mol Biochem Parasitol. 1991, 49: 119-131. 10.1016/0166-6851(91)90135-S.
Audran R, Cachat M, Lurati F, Soe S, Leroy O, Corradin G, Druilhe P, Spertini F: Phase I malaria vaccine trial with a long synthetic peptide derived from the merozoite surface protein 3 antigen. Infect Immun. 2005, 73: 8017-8026. 10.1128/IAI.73.12.8017-8026.2005.
Theisen M, Soe S, Oeuvray C, Thomas AW, Vuust J, Danielsen S, Jepsen S, Druilhe P: The glutamate-rich protein (GLURP) of Plasmodium falciparu is a target for antibody-dependent monocyte-mediated inhibition of parasite growth in vitro. Infect Immun. 1998, 66: 11-17.
Metzger WG, Okenu DMN, Cavanagh DR, Robinson JV, Bojang KA, Weiss HA, McBride JS, Greenwood BM, Conway DJ: Serum IgG3 to the Plasmodium falciparu merozoite surface protein 2 is strongly associated with a reduced prospective risk of malaria. Parasite Immunol. 2003, 25: 307-312. 10.1046/j.1365-3024.2003.00636.x.
Metzger WG, Haywood M, D'Alessandro U, Drakeley CJ, Weiss H, Bojang K, Target GA, Greenwood BM: Serological responses of Gambian children to immunization with the malaria vaccine SPf66. Parasite Immunol. 1999, 21: 335-340. 10.1046/j.1365-3024.1999.00231.x.
Overing J: The aesthetics of production: the sense of community among the Cubeo and Piaroa. Dialect Anthropol. 1989, 14: 159-175.
Metzger DJ, Morey RV: Los Hiwis. Los Aborígenes de Venezuela. Edited by: Coppens W. 1983, Caracas: Instituto Caribe de Antropología, 2: 125-128.
Sojo-Milano M, Grande-Montalvo T: Epidemiologia de casos repetidores de Malaria en Amazonas, Venezuela. Boletín de Malariología y Salud Ambiental. 2009, 49: 73-89.
Greenwood BM, Groenendaal F, Bradley AK, Greenwood AM, Shenton F, Tulloch S, Hayes R: Ethnic differences in the prevalence of splenomegaly and malaria in The Gambia. Ann Trop Med Parasitol. 1987, 81: 345-354.
Arama C, Giusti P, Boström S, Dara V, Traore B, Dolo A, Doumbo O, Varani S, Troye-Blomberg M: Interethnic differences in antigen-presenting cell activation and TLR responses in Malian children during Plasmodium falciparu malaria. PLoS One. 2011, 6: e18319-10.1371/journal.pone.0018319.
Marsh K, Hayes RH, Carson DC, Otoo L, Shenton F, Byass P, Zavala F, Greenwood BM: Anti-sporozoite antibodies and immunity to malaria in a rural Gambian population. Trans R Soc Trop Med Hyg. 1988, 82: 532-537. 10.1016/0035-9203(88)90495-6.
Metzger WG, Maxwell CA, Curtis CF: Anti-sporozoite immunity and impregnated bednets in Tanzanian villages. Ann Trop Med Parasitol. 1998, 92: 727-729. 10.1080/00034989859195.
Rodríguez I, de Abreu N, Carrasquel A, Bolívar J, González M, Scorza JV, Pérez H: Infecciones maláricas en individuos asintomáticos en la población indígena Jivi, Amazonas, Venezuela. Boletín de Malariología y Salud Ambiental. 2010, 50: 197-205.
Chuangchaiya S, Jangpatarapongsa K, Chootong P, Sirichaisinthop J, Sattabongkot J, Pattanapanyasat K, Chotivanich K, Troye-Blomberg M, Cui L, Udomsangpetch R: Immune response to Plasmodium viva has a potential to reduce malaria severity. Clin Exp Immunol. 2010, 160: 233-239.
Acknowledgements
This study was financially supported by the Venezuelan Ministry for Science and Technology and by the Institute of Tropical Medicine, University of Tuebingen, Germany. We would like to thank Anibal Giron and Jose Antonio Charasco for providing the data of the Amazonas Health Information System. Thanks to all who collaborated in the study. Thanks to the participants of the communities of Platanillal, Cero de Oro, and Paria Grande.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AB coordinated and conducted field and laboratory work, analysed and interpreted the data, and drafted and revised the manuscript. MM conceived the study, supervized field and laboratory work and interpreted the data. SVM conceived the study, facilitated the overall collaboration and revised the manuscript. MLU and TH coordinated and conducted field and laboratory work. RD collaborated as anthropologist. ME and BGM supervized the laboratory work, gave statistical input, interpreted the data and revised the manuscript. MT and LA were responsible for the conception of the work. WGM conceived the study, interpreted the data, and drafted and revised the manuscript. All authors revised and approved the final manuscript. WGM and MM are the guarantors of the paper.
Andreas Baumann, Magda M Magris contributed equally to this work.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Baumann, A., Magris, M.M., Urbaez, ML. et al. Naturally acquired immune responses to malaria vaccine candidate antigens MSP3 and GLURP in Guahibo and Piaroa indigenous communities of the Venezuelan Amazon. Malar J 11, 46 (2012). https://doi.org/10.1186/1475-2875-11-46
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2875-11-46