Abstract
Background
Accurate diagnosis and prompt treatment of pregnancy-associated malaria (PAM) are key aspects in averting adverse pregnancy outcomes. Microscopy is the gold standard in malaria diagnosis, but it has limited detection and availability. When used appropriately, rapid diagnostic tests (RDTs) could be an ideal diagnostic complement to microscopy, due to their ease of use and adequate sensitivity in detecting even sub-microscopic infections. Polymerase chain reaction (PCR) is even more sensitive, but it is mainly used for research purposes. The accuracy and reliability of RDTs in diagnosing PAM was evaluated using microscopy and PCR.
Methods
A cohort of pregnant women in north-eastern Tanzania was followed throughout pregnancy for detection of plasmodial infection using venous and placental blood samples evaluated by histidine rich protein 2 (HRP-2) and parasite lactate dehydrogenase (pLDH) based RDTs (Parascreen™) or HRP-2 only (Paracheck Pf® and ParaHIT®f), microscopy and nested Plasmodium species diagnostic PCR.
Results
From a cohort of 924 pregnant women who completed the follow up, complete RDT and microscopy data was available for 5,555 blood samples and of these 442 samples were analysed by PCR. Of the 5,555 blood samples, 49 ((proportion and 95% confidence interval) 0.9% [0.7 -1.1]) samples were positive by microscopy and 91 (1.6% [1.3-2.0]) by RDT. Forty-six (50.5% [40.5 - 60.6]) and 45 (49.5% [39.4 – 59.5]) of the RDT positive samples were positive and negative by microscopy, respectively, whereas nineteen (42.2% [29.0 - 56.7]) of the microscopy negative, but RDT positive, samples were positive by PCR. Three (0.05% [0.02 - 0.2]) samples were positive by microscopy but negative by RDT. 351 of the 5,461 samples negative by both RDT and microscopy were tested by PCR and found negative. There was no statistically significant difference between the performances of the different RDTs.
Conclusions
Microscopy underestimated the real burden of malaria during pregnancy and RDTs performed better than microscopy in diagnosing PAM. In areas where intermittent preventive treatment during pregnancy may be abandoned due to low and decreasing malaria risk and instead replaced with active case management, screening with RDT is likely to identify most infections in pregnant women and out-performs microscopy as a diagnostic tool.
Similar content being viewed by others
Background
Accurate diagnosis and prompt treatment of pregnancy-associated malaria (PAM) is essential to avert adverse pregnancy outcomes [1]. Detection of sub-microscopic infections is crucial in order to not only effect prompt treatment of asymptomatic cases, but also to identify and clear potential reservoirs of transmission [2, 3] and to reduce malaria related morbidity and mortality. Presumptive treatment of malaria based on clinical diagnosis is relatively cheap but it is unreliable due to overlapping symptoms with non-malarial infections caused by viruses or bacteria [4] and could lead to over-diagnosis [5] as well. Wrong diagnoses may lead to presumptive medication and hence many patients may leave the health facility without the right treatment. Rational prescription of anti-malarials is not only important in saving on the cost of expensive drugs but it also prevents drug overuse that might result in the development of resistance [6]. Sub-microscopic infections during pregnancy might be associated with increased risk of adverse pregnancy outcomes including low birth weight babies and maternal anaemia [7, 8]. Therefore, treatment of these infections may prevent potential risks of adverse pregnancy outcome [9].
PAM in the sub-Saharan Africa is caused by Plasmodium falciparum, and it is precipitated because VAR2CSA, member of the P. falciparum erythrocyte membrane protein 1 (Pf EMP-1) family expressed on the surface of infected erythrocytes (IEs) mediates sequestration of IEs in the intervillous spaces of the placenta by binding to chondroitin sulphate A (CSA) receptors [10, 11]. The pathogenesis of PAM and its association with adverse pregnancy outcome [12, 13], such as intrauterine growth retardation and low birth weight is not well understood but it is thought to be caused by impairment in nutrient transport to the foetus [14], with possible effects on growth regulating hormones [15] and trophoblast invasion [16]. As a result of placental sequestration it is often difficult to detect IEs in the peripheral blood using microscopy [17]. Furthermore, malarial infections are usually asymptomatic among adults in malaria endemic regions, decreasing the chances of clinical detection by using clinical algorithms. Primi- and secundigravidae as opposed to multigravidae are most affected as they lack sufficient previous exposure to allow the development of protective immunity [18, 19].
Microscopic examination of blood smears has been the gold standard for malaria diagnosis but it is compromised by poor infrastructure and the need for individuals with expertise in microscopy who are not necessarily available in many health facilities in malaria endemic regions [20]. Furthermore, microscopy is not sensitive enough [5, 9, 21–24], it requires good quality reagents, well maintained microscopes, and is time consuming [25]. Studies conducted in many malaria endemic regions show better sensitivity of RDTs as compared to microscopy [26–29] in malaria diagnosis and it is suggested that RDTs could be used as a supplementary diagnostic tool to aid evidence-based decision making in malaria treatment. The use of RDTs requires neither extensive training [30] nor substantial investment in infrastructure as compared to microscopy. However, there are a number of challenges that need to be addressed for optimal and effective utilization of RDTs in malaria diagnosis in order to provide reliable and credible diagnoses [31]. There should among others be; frequent quality controls and assurances, optimal storage conditions as well as updates on newly available or improved RDTs. If proper instructions are not given to staff especially in the rural communities on how to properly handle these RDTs, their expected usefulness as an alternative diagnostic tool for malaria diagnosis would be highly compromised.
The performance of Parascreen™ has previously been assessed under field conditions [32] involving children with clinical suspicion of malaria in a rural area of Kenya and gave results that were in agreement with other malarial diagnostic tests. Likewise, Paracheck Pf® and ParaHIT®f have also been assessed in community studies within the study area [33, 34]. However, during these cross-sectional and longitudinal community studies [33] it has been shown that Paracheck Pf® and ParaHIT®f which are HRP-2 based RDTs were not very sensitive in diagnosing parasite densities of less than 200 asexual stages/μl in asymptomatic children. The sensitivity of different RDTs can also be improved by increasing the concentration of detection antibodies. This is an important component in the manufacturing process, which is usually coupled by frequent evaluations of test performances. Nevertheless their use, despite the low sensitivity at very low parasitaemia has significantly reduced over-prescription of anti-malarials among individuals without malarial infection and they performed well in diagnosing those with symptoms of malaria [5].
Many studies that assess the sensitivity and specificity of RDTs of malaria mainly utilize microscopy as the gold standard [35–37]. However, RDTs detecting histidine rich protein 2 (HRP-2) have the problem of detecting HRP-2 antigen circulating in the blood more than two weeks after IEs have been cleared from the blood stream, resulting in high false positive rates [38, 39]. In the study presented here, RDTs that detect both HRP-2 and pLDH as well as HRP-2 only antigens were used in order to detect P. falciparum infections, and to also identify non-falciparum species in the area [40].
Other sensitive alternative tests superior to microscopy and RDTs such as PCR and real-time quantitative nucleic acid sequence-based amplification (real time QT-NASBA) are also available [28, 41], but they are mainly being utilized for epidemiological studies rather than facilitating treatment.
Failure to detect asymptomatic and sub-microscopic infections may leave a large part of the population with untreated infections that may lead to persistent maternal anaemia [42, 43] and adverse consequences for the foetus. Simple and easy to use malarial diagnostic tools with adequate sensitivity such as RDTs are therefore required [44] for effective management of PAM. As part of a study entitled strategies to prevent pregnancy-associated malaria (STOPPAM), a sub-study with the aim of assessing the reliability of RDTs in diagnosing PAM was conducted.
Methods
Study design
A prospective cohort study on pregnant women was conducted from September 2008 to October 2010. Enrolled women had gestational age of ≤ 24 weeks, were residents within an accessible area of Korogwe District in order to facilitate follow up, had given written informed consent to participate and were willing to deliver at Korogwe District Hospital (KDH). After inclusion, the cohort was followed up through three pre-scheduled antenatal clinic visits (every 2–6 weeks depending on gestational age) until delivery at KDH and satellite outreach dispensaries within Korogwe District, and they were also seen outside the pre-scheduled visits (at any time) whenever necessary. Venous blood samples were collected during each visit and placental blood at delivery for detection of malaria parasites and evaluation of haematological and other biological parameters. Ultrasound sonography was performed at inclusion to ascertain the gestational age and at each antenatal visit to assess intrauterine foetal growth.
Study site
This study was carried out in Korogwe District, north-eastern Tanzania. The district is inhabited by approximately 261,004 individuals, with a growth rate of 1.4% per annum according to the 2002 Tanzanian human population census report [45]. The district can be topographically stratified into lowland and highland zones, and malaria transmission is perennial with the highest transmission in the lowlands and after long rains [46, 47] and low transmission in the highlands at the onset of short rains. P. falciparum is the dominant malaria species transmitted by Anopheles gambiae s.s and Anopheles funestus[48] with entomological inoculation rates of 91 infective bites/person per year [46]. The district has been under constant surveillance of malaria since 2003. Of late, there has been a progressive decline in malaria parasite slide positivity rates in the area [49, 50] that transformed the area from hyper-endemic to meso/hypo endemic. Obstetric care is provided at KDH, and at other Health Centres and dispensaries within Korogwe District. More details about the study area can be found in Mmbando et al.[49]. According to the 2004–2005 demographic and health survey (DHS) report, the coverage of intermittent preventive treatment during pregnancy with sulphadoxine-pyrimethamine (IPTp-SP) in Tanga Region where Korogwe District is situated was 61.9% [51] as opposed to 90% during the STOPPAM study indicating the importance of sensitization and its impact on utilization of health services.
Ethical approval, sensitization meetings and informed consent
The study protocol was approved by the Tanzania Medical Research Coordinating Committee with reference number NIMR/HQ/R.8a/Vol. IX/688. Sensitization meetings about the study goals and expectations were held in all catchment villages. All procedures were conducted in consistent with good clinical and laboratory practices. All participants gave written informed consent.
Study samples
A cohort of 924 pregnant women was followed up from enrolment until delivery, and a total of 5,905 samples were collected. Of those, 5,167 venous and 388/650 placental blood samples, for which there were complete RDT and microscopy datasets, were randomly selected for analysis. The calculation of the sample size for the primary study “STOPPAM” was based on the placental hospital study that was previously conducted at KDH and reported a placental parasite prevalence ranging from 10 – 18%. The study screened 1,171 and excluded 176 pregnant women to have the final sample size of 995 pregnant women meeting the inclusion criteria for enrolment. Seventy one pregnant women were lost to follow up due to various reasons (Figure 1).
Blood drawing
Five to ten ml of venous blood was drawn at inclusion, at scheduled and unscheduled antenatal clinic visits, and just before/after delivery. Ten ml of unperfused placental blood was also collected within 15 minutes of delivery for women who gave birth at the labour ward of KDH. The venous and placental blood for malaria thick and thin blood smear preparations as well as filter paper blood spots for DNA extraction were collected in ethylenediamine-tetraacetic acid (EDTA) minicollect tubes, whereas for RDTs whole blood was directly added to the test device.
Malaria rapid diagnostic tests
Parascreen™ (Zephyr Biomedicals Goa, India) an RDT that detects histidine rich protein 2 (HRP-2) antigen from P. falciparum and parasite lactate dehydrogenase (pLDH) from the Plasmodium species was used for the majority of samples in this study. A minority of samples were tested by Paracheck Pf® (Orchid Biomedical Systems –Mumbai, India) or ParaHIT®f (Span diagnostics Ltd – Surat, India), the commonly available RDTs in the study area. Paracheck Pf® and ParaHIT®f only detect HRP-2 antigen from P. falciparum. All tests were performed following the manufacturer’s instructions. The laboratory and clinical personnel were trained on how to perform and interpret the RDTs results. As of the 2011 WHO round 3 data on malarial RDTs performances, all the RDTs used in this study have been shown to perform well in all three rounds of testing for performances.
Microscopic examination of thick and thin blood smears
Thick and thin blood smears from whole EDTA venous and placental blood samples were prepared on glass slide, air dried, stained for 30 minutes with 5% Giemsa stain, then washed gently in tap water, air dried and finally examined with a 100x objective lens under oil immersion. Before a slide was declared negative 100 microscopical thick film fields were scanned. Asexual parasite density was recorded as number of asexual stage parasites per 200 leucocytes, and converted to parasite count per microlitre, by using the actual count of leucocytes as estimated by Sysmex KX-21 N haematological analyser (Kobe, Japan). If the parasite count was less than 10, it was recorded per 500 leucocytes. All slides were read twice by two independent experienced microscopists and results from the two readings with a difference of less than 50% were considered definitive. Smears with discordant results were re-examined by a third experienced microscopist (blinded to the first two readings) and results from two readers that were in agreement were considered final. All laboratory technologists reading the blood slides participated in the proficiency microscopy examination and were certified by the National Institute for Communicable Diseases (NICD), South Africa.
Plasmodium species diagnostic PCR
In order to circumvent the problem of false negatives due to the inability of microscopy in detecting sub-microscopic infections or false positives due to the detection of circulating HRP-2 antigen by RDT even after parasite clearance, all the RDT positive but microscopy negative samples as well as a proportion of both the RDT and microscopy negative samples were analysed using nested Plasmodium species diagnostic PCR assay. Fifty microlitre of EDTA blood was added on a premade template of Whatman number 3 filter paper and allowed to dry at room temperature and stored in silica gel to preserve the DNA integrity. Briefly, half sector of the filter spot was excised and incubated with 0.5% saponin (SIGMA™) in 1x PBS and incubated overnight to remove the haemoglobin. The DNA was extracted by Chelex 100 resin method as explained by Wooden et al.[52] with some modifications. The DNA supernatant was carefully transferred to a new 96 wells PCR plate without touching the Chelex 100 resin and stored at −20°C until use. The parasite DNA was amplified by outer and nested species diagnostic PCR according to Snounou et al.[53] and the PCR products were analysed in 1.5% ethidium bromide stained UltraPure™ agarose gel (Invitrogen) with a Gene ruler™ 50 bp DNA ladder (Lonza, Belgium). The gels were visualized under UV trans-illuminator from BIO-RAD.
Management of malaria
All women with confirmed malarial infection based on RDTs and/or microscopy were treated with anti-malarial drugs. Uncomplicated and asymptomatic infections were treated by administration of quinine in the first trimester and artemether-lumefantrine during the second or third trimester.
Data management and analyses
All data were documented on case record forms and double entered into Microsoft Access database, cleaned, validated and transferred into R. version 2.12.0 statistical package for analyses. Statistical significance level was considered at α = 0.05. Baseline characteristics (demographic, clinical and parasitological) were analysed using descriptive statistics. Sensitivity was defined as the proportion of true malarial cases (positive blood smears and/or PCRs) that were correctly identified by positive RDTs whereas specificity was the proportion of true negative malarial cases (negative blood smears/negative PCRs) that were correctly identified by negative RDTs. Positive predictive value was the proportion of true malarial cases (positive blood smears and/or PCR) among the individuals with the positive RDTs. Negative predictive value was the proportion of true negative malarial cases (negative blood smears/PCRs) among the total number of negative RDT tests. Accuracy was defined as the proportion of all tests that gave correct results (True Positive + True Negative)/ number of all tests.
Results
In total, 1,171 pregnant women were screened, 995 (85%) met the inclusion criteria and were enrolled and followed up. Seventy-one women were lost to follow up or excluded before delivery due to spontaneous abortion or moving out of the study area. Of the enrolled cohort, 924/995 (93%) successfully completed follow up, from whom 5,555 blood samples with complete RDT and microscopy data were selected for further analyses (Figure 1). Of the enrolled cohort, 471 women were primi/secundigravid and 524 were multigravid with mean ages of 22.6 ± 4.2 and 30.7 ± 5.3 years for primi/secundigravid and multigravid women, respectively. There were 899 successful live births among the 924 pregnant women who successfully completed the follow up. P. falciparum was the only malarial parasite detected by microscopy. In women with a positive slide reading, the median asexual parasite density/μl was 2,090 [range; 40–390,748] and 4,163 [range; 40–45, 760] for primi-/secundigravid and multigravid, respectively, (Table 1). 3,892 samples were tested with Parascreen™, an RDT which detects both P. falciparum and non-falciparum parasites. Thirteen samples (0.3% [95% CI: 0.2 – 0.6] were RDT positive for non-falciparum species, and of these 11 were also RDT-positive for P. falciparum. As stated above non-falciparum parasites were not detected by slide reading and the remaining part of the article only compares detection of P. falciparum by the different methods employed since it is the one mainly involved in PAM pathogenesis.
Comparison of rapid diagnostic test with microscopy results
Overall 91/5,555 (1.6% [1.3-2.0]) samples were positive for malarial parasite antigen based on RDTs whereas 49/5,555 (0.9% [95% CI; 0.7 –1.1]) were positive by microscopy (Table 2). Of the 91 RDT positive samples, 46 (50.5% [95% CI: 40.5 - 60.6] were microscopy positive whilst 45 (49.5% [95% CI; 39.4 – 59.5]) were microscopy negative. To test whether the 45 microscopy negative but RDT positive samples were genuinely negative or false positive, a species diagnostic PCR assay was performed. Three (0.05% [0.02 - 0.2]) samples were positive by microscopy but negative by RDT. These samples were not tested by PCR assay, but the slide readings were confirmed by two independent expert slide readers as positive with median parasite density of 224.75 [range; 86 – 486].
PCR confirmation of the RDT positive but microscopy negative cases
The 45 RDT positive but microscopy negative samples were checked by nested PCR to ascertain whether they were sub-microscopic infections. Interestingly, 19/45 (42.2% [95% CI; 29.0 - 56.7] were positive by PCR (Table 3).
Nested species diagnostic PCR correction of RDT and microscopy negative samples
A proportion 351/650 (54%) of the available placental blood samples that were malarial negative by both RDT and microscopy were checked by nested PCR targeting P. falciparum as it is the most prevalent species in the study area and the one responsible for PAM pathology. Only 650 placental blood samples could be collected due to clotted placental blood (e.g. retained placenta or the need for the project nurses to stay in the labour room to resuscitate the newborn, delaying the transportation of the placenta to the laboratory for processing) and 190 women gave birth outside the KDH setting making it impossible to collect placental blood. Due to limited resources and time, only a small proportion of all the negative samples could be checked by PCR. The 351 placental instead of venous blood samples were randomly selected as microscopy could have missed some parasites in the peripheral blood due to parasite sequestration in the placenta and also due to the presence of debris and other contaminants in the placental blood that might have resulted to poor quality blood smears not easily readable. Interestingly, all these samples were negative by PCR indicating that both microscopy and RDTs performed equally well in diagnosing true negative cases.
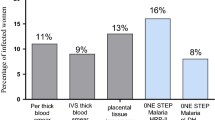
Performance of different RDTs after PCR correction
The performance of the different RDTs and microscopy was compared in the 442 samples in which PCR was performed and using the PCR results as the golden standard (Table 4). There was no statistically significant difference between the performances of the different RDTs. However, the study was not designed to directly compare the different RDTs and these RDTs were not employed on the same samples. All the PCR and slide positive samples were P. falciparum. Probably the use of a modified Snounou PCR using P. ovale. wallikeri and P. ovale. curtisi primers might have increased the number of positive PCRs and hence the overall performance of the RDTs.
Discussion
The performance of RDTs in diagnosing PAM was evaluated against microscopy and nested Plasmodium species diagnostic PCR in a cohort of pregnant women in north-eastern Tanzania. The use of RDTs might act as an appropriate complementary diagnostic tool for malaria instead of only relying on presumptive treatment based on clinical grounds in areas with limited expert microscopy and laboratory infrastructure. Prescription of any drug during pregnancy is a challenging task due to potential risks of harming the foetus [54], over-prescription and subsequent risk of drug resistance development [55]. Simple, cheap, reliable, accurate, easy to use, sensitive and specific diagnostic tests that can identify genuine malarial cases are the only means of allowing accurate malaria detection and rational treatment. With the escalating anti-malarial drug resistance which necessitates the deployment of expensive artemisinin-based combination therapy, there is a need to prescribe anti-malarial drugs only to patients with true malarial illness [56]. The present study demonstrates that RDTs can act as a diagnostic tool to manage malaria during pregnancy in resource poor settings with limited access to expert microscopy as they are easy to use and perform better than microscopy. Based on the PCR results, the different types of RDTs used in this study were able to capture over 40% of sub-microscopic infections missed by microscopy.
According to the current Ministry of Health and Social Welfare’s policy in Tanzania on malaria diagnosis, the use of RDTs is not yet implemented as a routine practice for pregnant women at antenatal clinics. Therefore, there is a need to provide evidence-based data on the best diagnostic supplement/alternative for malaria diagnosis during pregnancy in areas with limited laboratory infrastructure. This will assist the National Malaria Control Programme in Tanzania and beyond when considering RDTs as a possible routine diagnostic tool in malaria diagnosis during pregnancy. According to the recent WHO report [57] on the performance of different RDTs, it has been shown that they are easy to use, are heat stable and have the ability to detect parasitaemia as low as 200 asexual stages/μl. This makes RDTs an ideal diagnostic supplement to malaria diagnosis in resource constrained settings.
In many of the malaria endemic regions including Tanzania, healthcare delivery in peripheral settings is compromised by the lack of well equipped laboratories and personnel with sufficient expertise in malaria microscopy [58]. Microscopy could be as sensitive as RDTs or even more sensitive when done well. However, adequate infrastructure, maintenance of good quality microscopy and proper training on expert microscopy are not always present in many malaria endemic settings. Mismanagement of sub-microscopic infections could result in low but persistent parasitaemia that may culminate in adverse pregnancy outcomes [42, 43]. Under-diagnosis and/or wrong diagnosis of true malarial infections may lead to infections going untreated or being wrongly treated as non-malarial illnesses, with subsequent adverse pregnancy outcomes and/or acting as potential reservoirs of transmission. However, in all malaria endemic settings, children with febrile illnesses are treated by anti-malarials and/or other antimicrobials following the World Health Organization guidelines’ on integrated management of childhood illnesses.
Singer et al.[59] have shown that microscopy underestimates the real malarial burden during pregnancy. Nonetheless in their study, contrary to this study, PCR detected more positive cases as compared to RDTs, whilst assessing only placental blood samples. The present study might differ from that of Singer and colleagues in malaria transmission intensities and also in the current study only a small proportion of RDT and microscopy negative samples were checked by PCR due to limited resources and time. However, when taken as a proportion of placental blood the 351 samples checked by PCR accounts for 54% of the available placental blood samples with complete data. The message portrayed here is that microscopy was shown to have underestimated the true malarial prevalence after PCR correction.
The persistence of HRP-2 circulation in the blood more than two weeks even after successful clearance of IEs in the bloodstream is one of the concerns on the usefulness of HRP-2 based RDTs in malaria diagnosis, as has been reported by many studies [35, 36, 38, 39, 60]. However, in most of these studies microscopy was used as gold standard without PCR correction and this might have categorized sub-microscopic infections as false positives due to the limited sensitivity of microscopy. In the present study, all the RDT positive but microscopy negative samples were checked by PCR and the analyses showed that a large proportion of the RDT positive but microscopy negative samples were in fact sub-microscopic infections. Treatment of these few false positive women with anti-malarials might provide some prophylactic effect against subsequent infections outweighing the risk of not treating genuine sub-microscopic infections missed by microscopy that could have a profound effect on the pregnancy outcome. The relatively poor performance of microscopy compared to RDT cannot be explained by suboptimal conditions for microscopy as the present study was conducted in parallel with a large clinical trial [61]. Therefore, laboratory conditions were excellent and all the laboratory technologists had ample experience in malaria diagnosis and were undergoing proficiency microscopy tests on a regular basis.
The performance of RDTs in malaria diagnosis in the present study is in agreement with studies by Tjitra, Batwala and Tham et al.[26, 27, 62] showing that RDTs were performing better than microscopy in malaria diagnosis under field conditions. Likewise, Bell et al.[38] conducted a study in the Philippines in an area of low endemicity and reported that sub-microscopic infections missed by microscopy but captured by RDTs were actually true infections after PCR correction. On the other hand, the current study is not in agreement with a study by Schachterle et al.[63] that showed that RDTs had high rates of false positives and negatives in a region of hypoendemicity. However, the results of that study were purely based on microscopy data without PCR correction.
RDTs missed some few infections, which were positive in repeated microscopic investigations. This could be due to assay degradation as a result of humid conditions or batch variability of the RDTs [64], delay in HRP-2 surge after increased parasite density [38] or due to deletion of hrp-2 genes in some parasites [60]. Some studies have also reported reduced sensitivity of RDTs as a result of low parasitaemia [33, 65] and this could explain the reason for the few cases with low parasite densities missed by RDTs [49, 50].
This study indicates that RDTs outperform expert microscopy in detecting asymptomatic P. falciparum in pregnant women. Given the difficulties in establishing reliable microscopy based diagnostic services, RDTs are good alternative for the detection and in the management of P. falciparum infections in pregnant women. RDTs can both be used to detect infections not cleared by IPTp or to detect infections where the malaria endemicity is too low to warrant IPTp.
References
Mayor A, Serra-Casas E, Bardaji A, Sanz S, Puyol L, Cistero P, Sigauque B, Mandomando I, Aponte JJ, Alonse PL, Menendez C: Sub-microscopic infections and long-term recrudescence of Plasmodium falciparum in Mozambican pregnant women. Malar J. 2009, 8: 9-10.1186/1475-2875-8-9.
Karl S, Gurarie D, Zimmerman PA, King CH, St. Pierre TG, Davis TME: A sub-microscopic gametocyte reservoir can sustain malaria transmission. PLoS One. 2011, 6: e20805-10.1371/journal.pone.0020805.
Okell LC, Ghani AC, Lyons E, Drakeley CJ: Submicroscopic infection in Plasmodium falciparum-endemic populations: a systematic review and meta-analysis. J Infect Dis. 2009, 200: 1509-1517. 10.1086/644781.
Källander K, Nsungwa-Sabiiti J, Peterson S: Symptom overlap for malaria and pneumonia−policy implications for home management strategies. Acta Trop. 2004, 90: 211-214. 10.1016/j.actatropica.2003.11.013.
Reyburn H, Mbatia R, Drakeley C, Carneiro I, Mwakasungula E, Mwerinde O, Sangada K, Shao J, Kitua A, Olomi R, Greenwood BM, Whitty CJM: Overdiagnosis of malaria in patients with severe febrile illness in Tanzania: a prospective study. BMJ. 2004, 329: 1212-10.1136/bmj.38251.658229.55.
Verhoef H, Hodgins E, Eggelte TA, Carter JY, Lema O, West CE, Kok FJ: Anti-malarial drug use among preschool children in an area of seasonal malaria transmission in Kenya. AmJTrop Med Hyg. 1999, 61: 770-775.
Adegnika AA, Verweij JJ, Agnandji ST, Chai SK, Breitling LP, Ramharter MICH, Frolich M, Issifou S, Kremsner PG, Yazdanbakhsh M: Microscopic and sub-microscopic Plasmodium falciparum infection, but not inflammation caused by infection, is associated with low birth weight. AmJTrop Med Hyg. 2006, 75: 798-803.
Mockenhaupt FP, Rong B, Till H, Eggelte TA, Beck S, Gyasi-Sarpong C, Thompson WN, Bienzle U: Submicroscopic Plasmodium falciparum infections in pregnancy in Ghana. Trop Med Int Health. 2000, 5: 167-173. 10.1046/j.1365-3156.2000.00532.x.
Mockenhaupt F, Bedu-Addo G, von Gaertner C, Boye R, Fricke K, Hannibal I, Farakaya F, Schaller M, Ulmen U, Acquah PA, Dietz E, Eggelte TA, Bienzle U: Detection and clinical manifestation of placental malaria in southern Ghana. Malar J. 2006, 5: 119-10.1186/1475-2875-5-119.
Duffy PE, Fried M: Antibodies that inhibit Plasmodium falciparum adhesion to chondroitin sulfate a are associated with increased birth weight and the gestational age of newborns. Infect Immun. 2003, 71: 6620-6623. 10.1128/IAI.71.11.6620-6623.2003.
Salanti A, Dahlback M, Turner L, Nielsen MA, Barfod L, Magistrado P, Jensen ATR, Lavstsen T, Ofori MF, Marsh K, Hviid L, Theander T: Evidence for the involvement of VAR2CSA in pregnancy-associated malaria. J Exp Med. 2004, 200: 1197-1203. 10.1084/jem.20041579.
McGregor IA, Wilson ME, Billewicz WZ: Malaria infection of the placenta in The Gambia, West Africa; its incidence and relationship to stillbirth, birthweight and placental weight. Trans R Soc Trop Med Hyg. 1983, 77: 232-244. 10.1016/0035-9203(83)90081-0.
Steketee RW, Wirima JJ, Slutsker L, Heymann DL, Breman JG: The problem of malaria and malaria control in pregnancy in sub-Saharan Africa. AmJTrop Med Hyg. 1996, 55: 2-7.
Guyatt HL, Snow RW: Impact of malaria during pregnancy on low birth weight in sub-Saharan Africa. Clin Microbiol Rev. 2004, 17: 760-769. 10.1128/CMR.17.4.760-769.2004.
Umbers AJ, Boeuf P, Clapham C, Stanisic DI, Baiwog F, Mueller I, Siba P, King CL, Beeson JG, Glazier J, Rogerson SJ: Placental malaria-associated inflammation disturbs the insulin-like growth factor axis of fetal growth regulation. J Inf Dis. 2011, 203: 561-569. 10.1093/infdis/jiq080.
Muehlenbachs A, Mutabingwa TK, Edmonds S, Fried M, Duffy PE: Hypertension and maternal–fetal conflict during placental malaria. PLoS Med. 2006, 3: e446-10.1371/journal.pmed.0030446.
Mockenhaupt FP, Ulmen U, von Gaertner C, Bedu-Addo G, Bienzle U: Diagnosis of placental malaria. J Clin Microbiol. 2002, 40: 306-308. 10.1128/JCM.40.1.306-308.2002.
Fried M, Duffy PE: Adherence of Plasmodium falciparum to chondroitin sulfate a in the human placenta. Science. 1996, 272: 1502-1504. 10.1126/science.272.5267.1502.
Fried M, Nosten F, Brockman A, Brabin BJ, Duffy PE: Maternal antibodies block malaria. Nature. 1998, 395: 851-852. 10.1038/27570.
Jelinek T, Grobusch MP, Schwenke S, Steidl S, Von Sonnenburg F, Nothdurft HD, Klein E, Loscher T: Sensitivity and specificity of dipstick tests for rapid diagnosis of malaria in nonimmune travelers. J Clin Microbiol. 1999, 37: 721-723.
Bojang KA, Obaro S, Morison LA, Greenwood BM: A prospective evaluation of a clinical algorithm for the diagnosis of malaria in Gambian children. Trop Med Int Health. 2000, 5: 231-236. 10.1046/j.1365-3156.2000.00538.x.
Bejon P, Andrews L, Hunt-Cooke A, Sanderson F, Gilbert S, Hill A: Thick blood film examination for Plasmodium falciparum malaria has reduced sensitivity and underestimates parasite density. Malar J. 2006, 5: 104-10.1186/1475-2875-5-104.
Othnigué N, Wyss K, Tanner M, Genton B: Urban malaria in the Sahel: prevalence and seasonality of presumptive malaria and parasitaemia at primary care level in Chad. Trop Med Int Health. 2006, 11: 204-210. 10.1111/j.1365-3156.2005.01551.x.
Dhorda M, Piola P, Nyehangane D, Tumwebaze B, Nalusaji A, Nabasumba C, Turyakira E, McGready R, Ashley E, Guerin PJ, Snounou G: Performance of a histidine-rich protein 2 rapid diagnostic test, Paracheck Pf-for detection of malaria infections in Ugandan pregnant women. AmJTrop Med Hyg. 2012, 86: 93-95.
Gerstl S, Dunkley S, Mukhtar A, De Smet M, Baker S, Maikere J: Assessment of two malaria rapid diagnostic tests in children under five years of age, with follow-up of false-positive pLDH test results, in a hyperendemic falciparum malaria area. Sierra Leone. Malar J. 2010, 9: 28-
Tham JM, Lee SH, Tan TM, Ting RC, Kara UA: Detection and species determination of malaria parasites by PCR: comparison with microscopy and with ParaSight-F and ICT Malaria Pf Tests in a clinical environment. J Clin Microbiol. 1999, 37: 1269-1273.
Tjitra E, Suprianto S, Dyer M, Currie BJ, Anstey NM: Field evaluation of the ICT Malaria P.f/P.v immunochromatographic test for detection of Plasmodium falciparum and Plasmodium vivax in patients with a presumptive clinical diagnosis of malaria in eastern Indonesia. J Clin Microbiol. 1999, 37: 2412-2417.
de Oliveira AM, Skarbinski J, Ouma PO, Kariuki S, Barnwell JW, Otieno K, Onyona P, Causer LM, Laserson KF, Akhwale WS, Slutsker L, Hamel M: Performance of malaria rapid diagnostic tests as part of routine malaria case management in Kenya. AmJTrop Med Hyg. 2009, 80: 470-474.
Singh NEER, Saxena AJAY, Awadhia SB, Shrivastava RITA, Singh MP: Evaluation of a rapid diagnostic test for assessing the burden of malaria at delivery in India. AmJTrop Med Hyg. 2005, 73: 855-858.
Mayxay M, Newton PN, Yeung S, Pongvongsa T, Phompida S, Phetsouvanh R, White NJ: An assessment of the use of malaria rapid tests by village health volunteers in rural Laos. Trop Med Int Health. 2004, 9: 325-329. 10.1111/j.1365-3156.2004.01199.x.
McMorrow ML, Masanja MI, Abdulla SMK, Kahigwa E, Kachur SP: Challenges in routine implementation and quality control of rapid diagnostic tests for malaria in Rufiji District, Tanzania. AmJTrop Med Hyg. 2008, 79: 385-390.
Mens P, Spieker N, Omar S, Heijnen M, Schallig H, Kager PA: Is molecular biology the best alternative for diagnosis of malaria to microscopy? A comparison between microscopy, antigen detection and molecular tests in rural Kenya and urban Tanzania. Trop Med Int Health. 2007, 12: 238-244.
Ishengoma D, Francis F, Mmbando B, Lusingu J, Magistrado P, Alifrangis M, Theander TG, Bygbjerg IC, Lemnge MM: Accuracy of malaria rapid diagnostic tests in community studies and their impact on treatment of malaria in an area with declining malaria burden in north-eastern Tanzania. Malar J. 2011, 10: 176-10.1186/1475-2875-10-176.
Mboera LEG, Fanello CI, Malima RC, Talbert A, Fogliati P, Bobbio F, Molteni F: Comparison of the Paracheck-Pf test with microscopy, for the confirmation of Plasmodium falciparum malaria in Tanzania. Ann Trop Med Parasitol. 2006, 100: 115-122. 10.1179/136485906X78571. 3–1
Wongsrichanalai C, Barcus MJ, Muth S, Sutamihardja A, Wernsdorfer WH: A review of malaria diagnostic tools: microscopy and rapid diagnostic test (RDT). AmJTrop Med Hyg. 2007, 77: 119-127.
Kilian AHD, Mughusu EB, Kabagambe G, Von Sonnenburg F: Comparison of two rapid, HRP2-based diagnostic tests for Plasmodium falciparum. Trans R Soc Trop Med Hyg. 1997, 91: 666-667. 10.1016/S0035-9203(97)90514-9.
Moody A, Hunt-Cooke A, Gabbett E, Chiodini P: Performance of the OptiMAL malaria antigen capture dipstick for malaria diagnosis and treatment monitoring at the Hospital for Tropical Diseases, London. Br J Haematol. 2000, 109: 891-894. 10.1046/j.1365-2141.2000.01974.x.
Bell DR, Wilson DW, Martin LB: False-positive results of a Plasmodium falciparum histidine-rich protein - 2-detecting malaria rapid diagnostic test due to high sensitivity in a community with fluctuating low parasite density. AmJTrop Med Hyg. 2005, 73: 199-203.
Mayxay M, Pukrittayakamee S, Chotivanich K, Looareesuwan S, White NJ: Persistence of Plasmodium falciparum HRP-2 in successfully treated acute falciparum malaria. Trans R Soc Trop Med Hyg. 2001, 95: 179-182. 10.1016/S0035-9203(01)90156-7. 3–1
Lusingu J, Vestergaard L, Mmbando B, Drakeley C, Jones C, Akida J, Savaeli ZX, Kitua AY, Lemnge MM, Theander TG: Malaria morbidity and immunity among residents of villages with different Plasmodium falciparum transmission intensity in North-Eastern Tanzania. Malar J. 2004, 3: 26-10.1186/1475-2875-3-26.
Mens P, Schoone G, Kager P, Schallig H: Detection and identification of human Plasmodium species with real-time quantitative nucleic acid sequence-based amplification. Malar J. 2006, 5: 80-10.1186/1475-2875-5-80.
Shulman CE, Dorman EK: Importance and prevention of malaria in pregnancy. Trans R Soc Trop Med Hyg. 2001, 97: 30-35.
Shulman CE, Marshall T, Dorman EK, Bulmer JN, Cutts F, Peshu N, Marsh K: Malaria in pregnancy: adverse effects on haemoglobin levels and birthweight in primigravidae and multigravidae. Trop Med Int Health. 2001, 6: 770-778. 10.1046/j.1365-3156.2001.00786.x.
VanderJagt TA, Ikeh EI, Ujah IOA, Belmonte J, Glew RH, VanderJagt DJ: Comparison of the OptiMAL rapid test and microscopy for detection of malaria in pregnant women in Nigeria. Trop Med Int Health. 2005, 10: 39-41. 10.1111/j.1365-3156.2004.01349.x.
The United Republic of Tanzania: National Website: 2002 Population and Housing Census Results. 2012, , , [http:www.tanzania.go.tz/census]
Bǿdker R, Akida J, Shayo D, Kisinza W, Msangeni HA, Pedersen EM, Lindsay SW: Relationship between altitude and intensity of malaria transmission in the Usambara Mountains, Tanzania. J Med Entomol. 2003, 40: 706-717. 10.1603/0022-2585-40.5.706.
Lusingu JP, Jensen AT, Vestergaard LS, Minja DT, Dalgaard MB, Gesase S, Mmbando BP, Kitua AY, Lemnge MM, Cavanagh D, Hviid L, Theander TG: Levels of plasma immunoglobulin G with specificity against the cysteine-rich interdomain regions of a semiconserved Plasmodium falciparum erythrocyte membrane protein 1, VAR4, predict protection against malarial anemia and febrile episodes. Infect Immun. 2006, 74: 2867-2875. 10.1128/IAI.74.5.2867-2875.2006.
Mnzava AE, Kilama WL: Observations on the distribution of the Anopheles gambiae complex in Tanzania. Acta Trop. 1986, 43: 277-282.
Mmbando B, Vestergaard L, Kitua A, Lemnge M, Theander T, Lusingu J: A progressive declining in the burden of malaria in north-eastern Tanzania. Malar J. 2010, 9: 216-10.1186/1475-2875-9-216.
Thomsen TT, Ishengoma DS, Mmbando BP, Lusingu JP, Vestergaard LS, Theander TG, Lemnge MM, Bygbjerg IC, Alifrangis M: Prevalence of single nucleotide polymorphisms in the Plasmodium falciparum multidrug resistance gene (Pfmdr-1) in Korogwe District in Tanzania before and after introduction of artemisinin-based combination therapy. AmJTrop Med Hyg. 2011, 85: 979-983.
Tanzania Demographic and Health Survey 2004–2005. 2012, , , [http:www.measuredhs.com/pubs/pdf/FR173/FR173-TZ04-05.pdf]
Wooden J, Kyes S, Sibley CH: PCR and strain identification in Plasmodium falciparum. Parasitol Today. 1993, 9: 303-305. 10.1016/0169-4758(93)90131-X.
Snounou G, Viriyakosol S, Xin PZ, Jarra W, Pinheiro L, do Rosario VE, Thaithong S, Brown KN: High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol Biochem Parasitol. 1993, 61: 315-320. 10.1016/0166-6851(93)90077-B.
Bánhidy F, Lowry RB, Czeizel AE: Risk and benefit of drug use during pregnancy. Int J Med Sci. 2005, 2: 100-106.
White NJ: Antimalarial drug resistance. J Clin Invest. 2004, 113: 1084-1092.
Amexo M, Tolhurst R, Barnish G, Bates I: Malaria misdiagnosis: effects on the poor and vulnerable. Lancet. 1920, 364: 1896-1898.
WHO: Malaria Rapid Diagnostic Test Peformance. Results of WHO product testing of malaria rapid diagnostic tests. 2012, World Health Organization, Geneva, Round 1 (2008)
Ishengoma DRS, Rwegoshora RT, Mdira KY, Kamugisha ML, Anga EO, Bygbjerg IC, Rønn AM, Magesa SM: Health laboratories in the Tanga region of Tanzania: the quality of diagnostic services for malaria and other communicable diseases. Ann Trop Med Parasitol. 2009, 103: 441-453. 10.1179/136485909X451726.
Singer LM, Newman RD, Diarra AMID, Moran AC, Huber CS, Stennies G, Sirima SB, Konate A, Yameogo M, Sawadogo R, Barnwell JW, Parise ME: Evaluation of a malaria rapid diagnostic test for assessing the burden of malaria during pregnancy. AmJTrop Med Hyg. 2004, 70: 481-485.
Baker J, McCarthy J, Gatton M, Kyle DE, Belizario V, Luchavez J, Bell D, Cheng Q: Genetic diversity of Plasmodium falciparum Histidine-Rich Protein 2 (PfHRP2) and its effect on the performance of PfHRP2-based rapid diagnostic tests. J Inf Dis. 2005, 192: 870-877. 10.1086/432010.
First Results of Phase 3 Trial of RTS,S/AS01 Malaria Vaccine in African Children. N Eng J Med. 2011, 365: 1863-1875.
Batwala V, Magnussen P, Nuwaha F: Are rapid diagnostic tests more accurate in diagnosis of Plasmodium falciparum malaria compared to microscopy at rural health centres?. Malar J. 2010, 9: 349-10.1186/1475-2875-9-349.
Schachterle S, Mtove G, Levens J, Clemens EG, Shi L, Raj A, Munoz B, Reller ME, West S, Dumler SJ, Sullivan D: Prevalence and density related concordance of three diagnostic tests for malaria in hypoendemic Tanzania. J Clin Microbiol. 2011, 49: 3885-3891. 10.1128/JCM.01157-11.
Mason DP, Kawamoto F, Lin K, Laoboonchai A, Wongsrichanalai C: A comparison of two rapid field immunochromatographic tests to expert microscopy in the diagnosis of malaria. Acta Trop. 2002, 82: 51-59. 10.1016/S0001-706X(02)00031-1.
Forney JR, Wongsrichanalai C, Magill AJ, Craig LG, Sirichaisinthop J, Bautista CT, Miller RS, Ockenhouse CF, Kester KE, Aronson NE, Andersen EM, Quino-Ascurra HÁ, Vidal C, Moran KA, Murray CK, DeWitt CC, Heppner DG, Kain KC, Ballou WR, Gasser RA: Devices for Rapid Diagnosis of Malaria: Evaluation of Prototype Assays That Detect Plasmodium falciparum Histidine-Rich Protein 2 and a Plasmodium vivax-Specific Antigen. J Clin Microbiol. 2003, 41: 2358-2366. 10.1128/JCM.41.6.2358-2366.2003.
Acknowledgements
All study participants and the administration of KDH are thanked for allowing us to conduct the study in their area. Special thanks are also extended to Charles Tunuka, Francis Assenga, Sophia Kabome, Lydia Massawe, Halima Mpambile, Rose Mutua, Seif Azizi, Prisca Mavindi and Latifa Shaweji for providing the clinical and follow up support. Tilaus Gustav, Deusdedith Makingi and Thomson Mwampamba for assisting in sample collection and processing. Allen Mrango, Frank Mnango and Francis Mkongo are thanked for their wonderful logistic support. The team is indebted to the data management team comprised of Christopher Mhagama, Hassan Kilavo, Silas Msangi, Stella Andrew and Eva Rimoy. All students from the University of Copenhagen, Denmark, Hannah Elena Suhrs, Martyna Gassowski, Pernille Kofoed, Line Holm, Peter Cordes and Radboud University Nijmegen Medical Centre, The Netherlands, Alisha Walker, Neeltje Rutten and Nicolien Beld and all staff of NIMR-Korogwe Research Laboratory are thanked for their wonderful support and cooperation. Benno Mapunda, Lydia Lugomora, Christopher Masaka, Obedi Ole Kaondo and Bibiana Reuben are thanked for their administrative and financial support. NIMR administration is thanked for granting the permission to publish and other logistic support. Last and not the least Ulla Abildtrup is thanked for her technical assistance in the setting up of the PCR assays.
The funding for this study was kindly provided by the European Union (EU) through the Seventh Framework Programme STOPPAM (FP7) with contract number 200889 and the Danish International Development Agency (DANIDA) with grant number DFC file no.87-08-KU
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
All authors declare no any conflict of interest.
Authors’ contributions
DTRM, CS, JL, TT, AS, ML, PD, AJFL and MA designed the study. DTRM, JL, CS, MO, SB, CP, DJ, PM, DA and MA conducted the study and participated in the laboratory analyses. DTRM drafted the manuscript. All authors reviewed the manuscript and provided critical inputs. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Minja, D.T., Schmiegelow, C., Oesterholt, M. et al. Reliability of rapid diagnostic tests in diagnosing pregnancy-associated malaria in north-eastern Tanzania. Malar J 11, 211 (2012). https://doi.org/10.1186/1475-2875-11-211
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2875-11-211