Abstract
For over 30 years, stem cells have been used in the replenishment of blood and immune systems damaged by the cancer cells or during treatment of cancer by chemotherapy or radiotherapy. Apart from their use in the immuno-reconstitution, the stem cells have been reported to contribute in the tissue regeneration and as delivery vehicles in the cancer treatments. The recent concept of 'cancer stem cells' has directed scientific communities towards a different wide new area of research field and possible potential future treatment modalities for the cancer. Aim of this review is primarily focus on the recent developments in the use of the stem cells in the cancer treatments, then to discuss the cancer stem cells, now considered as backbone in the development of the cancer; and their role in carcinogenesis and their implications in the development of possible new cancer treatment options in future.
Similar content being viewed by others
Background
Cancer is the most common cause of mortality and morbidity in U.K. Despite recent advances in the treatments of cancer, the clinical outcome is yet far away from expectation. Use of stem cells in immuno-modulation or reconstitution is one of the methods used for decades in cancer therapy. Stem cells have self-renewal capacity with highly replicative potential in multilineage differentiation capacity [1].
Stem cells can be divided into main three categories: embryonic, germinal, and somatic. Embryonic stem cells (ESCs) originate from the inner cell mass of the blastocyst. ESCs are omnipotent and have indefinite replicative life span, which is attributable to their telomerase expression[2]. Germinal stem cells are derived from primary germinal layers of embryo. They differentiate into progenitor cells to produce specific organ cells. Somatic/adult stem cells are progenitor cells as they are less totipotent i.e. less replicative life span than ESCs. They exist in mature tissues such as haematopoietic, neural, gastrointestinal and mesenchymal tissues. The most commonly used adult stem cells (ASCs) derived from bone marrow are haemopoietic stem cells (HSCs) and other primitive progenitor cells including mesenchymal stem cells (MSCs) and multipotent adult progenitor cells (MAPCs)[3, 4] The microRNAs expression has been reported as a requisite to bypass G1/S checkpoint, thus for the self-renewal characteristic of stem cells[5]. Figure 1 shows hierarchy of stem cells with cell determination and differentiation. In this review, we highlight the potential of the adult stem cells in the cancer treatment and also focus on the new concept of the cancer stem cell.
Hierarchy of stem cells with cell determination, differentiation and maturation. It also shows potential areas of A. Trans-germal plasticity – differentiation from one stem to other stem cell type; B. De-differentiation – regression of a fixed lineage cell type to a more primitive cell type; C. Trans-determination – differentiation from one progenitor cells to another; and D. Trans-differentiation – hypothetical differentiation of one cell type to another without dedifferentiation.
The choice of source of stem cells for cancer therapy
Ideally, ESCs would be the source of stem cells for therapeutic purposes due to higher totipotency and indefinite life span compared to ASCs with lower totipotency and restricted life span. However, use of ESCs have ethical constraints (Department of Health, UK, National Institutes of Health and International Society for Stem Cell Research) and their use for research and therapeutic purposes are restricted[6] and prohibited in many countries throughout the world. In addition, the stem cells with higher totipotency have been shown to be more tumorogenic in mice [7]. Thus, for ease of availability and lesser constrained on ethical issue, ASCs are the stem cells most commonly used for research and therapeutic purposes. The other reason for the use of ASCs is their easy accessibility compared to ESCs. According to literature, ASCs from bone marrow (HSCs & MSCs) are the most commonly studied[8] stem cells. MSCs support HSCs in the bone marrow and have the ability to differentiate both in vivo and in vitro into the different mesenchymal cells such as bone, cartilage, fat, muscle, tendon and marrow stroma[9].
Stem cell sources
ESCs are derived from a 5-day old pre-implantation human embryos, however it posses potential risk of destroying the embryo. ASCs can be obtained from many tissues including bone, synovium, deciduous teeth, adipose tissue, brain, blood vessels, blood and umbilical cord blood[10–13]. Due to legal and ethical reasons, use of ESCs is restricted in research and clinical fields and ASCs remain the main supplement for the stem cells. Although ASCs can be obtained from the various sites, the ideal source of ASCs is yet to be found. Most commonly, ASCs are acquired from the bone marrow and peripheral blood. The bone marrow (BM) aspiration is one of the common procedures performed to obtain ASCs, but it is associated with morbidity in the form of wound infection and sepsis complications[14]. ASCs can also be obtained from adipose tissues such as abdominal fat and infra-patellar fat[15, 16] which is less invasive and less morbid procedure than the bone marrow aspiration. It has been shown that there is no significant difference in the cell growth kinetics, cell senescence, gene transduction of adherent stromal cells and yield from stem cells obtained from bone marrow or adipose tissues[17]. The peripheral blood also provides a safe and easily accessible route for isolating ASCs with minimal morbidity. Use of ASCs through peripheral blood has shown to induce more T and NK (Natural Killer) cells compared to bone marrow ASCs[18]. Recently, the stem cells have been claimed to be obtained from the amniotic fluid without any harm to mother and embryo (posted on cnn.com on 08/01/2007).
Stem cells in immuno-reconstitution
The stem cells have been used since many years in immuno-reconstitution following cancer development or following cancer treatments. The high dose chemotherapy have the adverse effects on the bone marrow causing myelosupression[19]. Usually this is followed by the blood cell recovery through the haematopoietic progenitor cells residing in the bone marrow by the complex interactions between the progenitor cells and the marrow microenvironment under the influence of various stimulatory and inhibitory factors [20–22]. However, time for haematopoietic recovery is proportional to the doses and number of cycles of chemotherapy [23] It has been shown that chemotherapy can induce inhibitory factors such as Tumour Growth Factor (TGF)-β, Interferon(IFN)-γ – IFN-α, Tumour Necrosis Factor(TNF)-α and Interleukin(IL)-4 with cytokines that causes myelosupression[24]. HSCs are the most commonly used and they are the stem cells of choice for the haematopoietic cell transplantation following high dose chemotherapy to restore bone marrow and immune system to pre-chemotherapy levels [25]. Randomised clinical trials regarding the use of HSCs for haematopoietic cell transplantation have been published with controversial results, however most of the trials suggested improved disease free survival rates, shorter hospital stay, overall survival rates and event free survival rates[26–31], while fewer of the studies have reported no statistically significant differences when assessed those parameters[32–35]. The adequate number of the stem cells therapy is also reported a crucial factors for speedy recovery[36]. Some of the chemotherapeutic agents, especially alkaylating agents, should be avoided as they are reported to adversely affect stem cell yield and haemotopoietic recovery[36, 37]. The post-transplant period thrombocytopenia and neutropenia may be reduced by re-infusion of ex vivo expanded megacaryocyte progenitors[38] and re-infusion of ex vivo expanded peripheral blood stem cells (PBSC)[39] respectively.
Choice of type of stem cell : bone marrow or peripheral blood
The source of stem cells is most commonly either from the bone marrow or the peripheral blood. The procedure of the bone marrow aspiration is invasive and is associated with the potential possible complications including fracture, wound infection and sepsis while the procedure for PBSCs isolation is much less invasive and less morbid. PBSCs have also been shown to induce higher number of CD4 T and NK cells compared to stem cells obtained from the bone marrow [18]. Thus, the stem cells from peripheral blood are considered the preferred source of stem cells however various clinical trials have publicized controversial conclusions comparing PBSCs and BM stem cells. It is also noticed that the occurrence of graft versus host reaction varies with PBSCs compared to BM stem cells [40, 41]. Table 1 shows published human clinical trials comparing outcomes following transplantation of stem cells from BM and peripheral blood. These clinical trials provide different outcomes such as Storek et al suggested that PBSC yields higher lymphocyte subset counts[42] while Hernandez et al noticed no difference in the number of lymphocyte counts but noted faster reconstitution of cytotoxic subsets [43]. Similarly, these trials present controversial results including graft versus host disease, overall survival, disease free survival and immune recovery. Double stem cell transplantation has been documented to improve overall survival compared to single stem cell transplantation[44]. Granulocyte-colony stimulating factor (G-CSF) helps in proliferation and differentiation of haematopoietic progenitor cells [45]. G-CSF has also been reported to mobilise autologous peripheral blood stem cells and to preserve and increase the length of telomerase [45]. There are various different agents which are shown to enhance the G-CSG activity in mobilising stem cell. These are paclitaxel and docetaxel[46], recombinant human thrombopoietin[47], lithium[48] and recombinant methionyl human stem cell factor (r-metHuSCF)[49].
Role of purging in the isolation of stem cells
The isolation of stem cells from the allogeneic donor is the most preferable method, however only 30% of candidates are eligible due to the lack of donors and age restrictions[50]. Stem cells from autologous source are easily available but they carry the risk of coexistence of normal haematopoietic progenitors with malignant counterparts and may lead to the relapse of cancer. In population of patients with breast cancer, PBSC transplantation has been related to a rapid and sustained haematopoietic engraftment and has shown to be less contaminated than bone marrow stem cells[51]. There was however no overall improvement in survival outcome[52].
The contamination of the retrieval of stem cells with tumour cells have been major problem which reported by many studies [51, 53, 54], however the effect on clinical cell therapy has been less problematic[55, 56].
Purging procedures are used in an attempt to remove these contaminant cancer cells from stem cells. Table 2 shows published clinical trials with various in vitro and in vivo techniques to purge the stem cells such as use of monoclonal antibodies, continuous flow immunoadsorption technique, dielectroforetic-field-flow-fractionation, use of rituximab, pulsed electric field, and hyperthermia. Amifostine has been shown to protect normal haematopoietic progenitor cells from damage by alkylating agents used for purging of stem cells[57, 58]. The double procedure using 'positive CD34' and 'negative CD19' double selection method for purging is reported to be better than single procedure in the poor prognosis lymphoproliferative disorders, but it is associated with increased risk of life-threatening infections [59].
Stem cells in tissue regeneration and as delivery vehicles
Apart from long lasting replicative property of stem cells, stem cells from haemopoietic tissues seem to have 'extraordinary' abilities to generate or switch between haematopoietic and non-haematopoietic lineages, exhibiting an unexpected degree of developmental or differentiation potential. On theoretical grounds, this allows HSC to be used to regenerate any non-haematopoietic tissue [60]. This technique has particular implications in bone tumours as reconstruction of bone following chemotherapy and surgery is always a major problem. The stromal stem cells derived from bone marrow have been used in the cell-based bone reconstruction following chemotherapy and surgery in osteosarcoma and Ewing sarcoma[61]. Jager et al have shown the regeneration of osteoblasts from the survived mesenchymal progenitor cells following COSS-96 (the cooperative osteosarcoma study) polychemotherapy in vitro and its potential in vivo use [62]. There are clinical trials showing role of the stem cells in the regeneration of myocardial tissue following myocardial infarction [63–65].
Systematic delivery of drug or gene therapy has promising future but is currently limited by various factors such as immune detection, non-specific accumulation in normal tissues and poor permeation. The effects of many anticancer agents are limited due to either their toxicities or their short half lives such as interferon β, which shows anti-proliferative and pro-apoptotic activities in vitro, but has shown restricted effects on human malignancies in vivo [66–68]. One proposed solution for these would be the cell-based carriers that may target the desired site.
The recent concept of use of stem cells as delivery vehicles came from the fact that the tumours, similar to the wounds, send out chemo-attractants such as the vascular endothelial growth factor (VEGF) to recruit MSC to form the supporting stroma of the tumour, and pericytes for angiogenesis. MSC transduced with an adenoviral expression vector carrying interferon-β gene has been demonstrated to increase the production of interferon-β at the local site[69]. However this in vivo function of MSC depends partly on signals from the target tissue microenvironment, for example, the tissues such as skin would have high cell turn over where there would be more signals for MSC compared to connective tissues where the high cell turn over is apparent only during healing process[70]. Likewise, MSC engineered to release interferon-β has been reported to create high local interferon-β levels in the mice glioma[71]. The neural stem cells have been reported as the delivery vehicles for the gene therapy for CNS disorders[72]. Similarly, interest has been shown in the use of the endothelial progenitor cells as the delivery vehicles for gene therapy because of their attraction towards the site of angiogenesis rather than the quiescent vasculature[73]. It may be possible to deliver immune-activating cytokines and other secreted proteins to brain and breast tumours though the stem cells.
Life span of ASC
The major limiting factor in the use of stem cells in clinical area is the life span of the stem cells. Theoretically, the embryonic stem cells are best from this perspective due to their indefinitive replicative life span attributed to their telomerase expression[2]. However, practically, use of the embryonic stem cells in clinical area is very much restricted. Most of ASC do not possess sufficient telomerase activity and thus cannot prevent loss of telomerase. At each division, the telomerase shortens and the replication slows down (aging) and at the end, cells cease to divide (crisis phase) [74]. Thus we may not be able to obtain enough adult stem cells to perform our clinical task. One proposed solution is the use of genetic manipulation to extend the replicative span of the stem cells through the introduction of genes involved in controlling the replicative lifespan. In humans, this can be achieved by overcoming the replicative senescence by using the ectopic expression of telomerase hTERT gene [75]. In recent years, many studies suggested that hTERT-expressing stem cells continue to proliferate longer and maintain their ability to differentiate[76, 77, 7, 78, 9] Similarly, hMSCs have been immortalized by transduction with HPV16 E6/E7 in vitro without any neoplastic changes[79]. If it becomes successful to imply this principle in clinical practice, quantitative amount of the stem cells may not be one of the prognostic factors in the outcome in future.
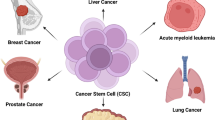
Cancer stem cells
Why a tumour does not respond to treatment? Why tumours recur? Why cancer cells develop resistance to treatment? These and many other raised questions may be answered by the new concept of "Cancer Stem Cells"[80].
Cancer stem cells can be defined as cells in the tumour growth with a tumour initiating potential. Normal stem cells are characterised by three properties: 1 Capability of self-renewal; 2 Strict control on stem cell numbers; 3 Ability to divide and differentiate to generate all functional elements of that particular tissue [81]. Compared to normal stem cells, the cancer stem cells are believed to have no control on the cell numbers. Cancer stem cells form very small numbers in whole tumour growth and they are said to be responsible for the growth of the tumour cells.
It has been well-known that in order to induce a tumour in an animal model, hundreds of thousands of cancer cells need to be injected [82]. This has been explained to be due to limitations in the assay to support tumour growth, or due to tumour formation deficiency [1]. With the recent concept of the cancer stem cells, it may be explained that higher numbers of cancer cells are needed to maximize the probability of injecting cancer stem cells in animal model. At present, the shrinkage in the size of a tumour is considered as a response to the treatment. However, tumour often shrinks in response to the treatment only to recur again. This may be explained by cancer stem cells that the treatment targeting the cancer cells may not be able to target the cancer stem cells
A fundamental problem in the cancer is the identification of the cell type capable of sustaining the neoplastic growth. There is evidence that the majority of the cancers are clones and that the cancer cells represent the progeny of one cell, however it is not clear which cells possess the tumour-initiating cell (TIC) function (cancer stem cells) and how to recognise them [83]. Though the idea of cancer stem cells is considered as a new concept in science, it was thought almost 35 years back in 1971 when they were called as leukaemic stem cells [84]. A small subset of cancer cells capable of extensive proliferation in leukaemia and multiple myeloma were found and named as leukaemic stem cells (LSC) [84]. Two possibilities were proposed: either all leukaemia cells had a low probability of proliferation and therefore all leukaemia cells behave as LSC, or only a small subset was clonogenic. The later theory was favoured by Dick and colleagues who were able to separate the LSC as CD34+CD38- from patients' samples [85]. Despite being small in numbers (0.2%), these were the only cells capable to transfer Acute Myeloid Leukaemia from patients to NOD-SCID (non-obese diabetic-severe combined immunodeficiency) mice.
Recently, the cancer stem cells were also shown in the solid tumours such as breast cancer and brain tumours [86, 87]. The cancer stem cells have been shown to have not only self-renewal capability but also generating wide spectrum of progeny, like normal stem cells [88]. In paediatric brain tumours, including medulloblastomas and gliomas, a subset of cells, called neurospheres, have been shown to have self-renewal capability. In conditions to promote differentiation, these neuospheres gave rise to neurones and glia, in proportion that reflect the amount in the tumour [89].
Origin of cancer stem cells
The cancer stem cells may be able to answer some of the questions related to a cancer growth, however origin of the cancer stem cells is yet to be defined. To recognise the origin of the cancer stem cells, two important factors need to be considered; 1 a number of mutations are required for a cell to be cancerous[90] and 2 a stem cell needs to overcome any genetic constraints on both self-renewal and proliferation capabilities[91]. It is unlikely that all the mutations could occur in the lifespan of a progenitor/mature cell. Therefore, cancer stem cells should be derived from either the self-renewing normal stem cells or from the progenitor cells that have acquired the ability of self-renewal due to mutations [92] (figure 2[92, 93]).
A simplified model of suggested hypothesis about origin of the cancer stem cells. The cancer stem cells may develop when self-renewing normal stem cells acquire mutations and are transformed by altering only proliferative pathways. It is also possible that the cancer stem cells originate by multiple oncogenic mutations in the restricted progenitor cells which acquire the capability of self-renewal (Created from NEJM [103]).
The hypothesis that cancer stem cells are derived from normal stem cells rather than more committed progenitor cells have been addressed in the cases of AML where leukaemia initiating cells (LIC) from various subtypes of AML with different stages of differentiation have been shown to share the same cell-surface markers with normal haematopoietic stem cells [85, 94]. However, some of the studies have suggested that cancer stem cells can be derived from the normal stem cells, as well as from the committed short-lived progenitors, giving rise to the tumours with comparable latencies, phenotypes and gene expression profiles[95–97] In the solid tumours, lack of the markers to characterise the tumour initiating cells (TIC) in the tumours has made it difficult to study the origins of the cancer stem cells, however there have been identification of cell-surface markers in the lung[4], brain[98–100] and prostate[101] which may allow the separation of the stem or progenitor cells with the tumour initiating function.
Implications for cancer treatment
At present, the cancer treatment is targeted at its proliferation potential and its ability to metastasise, and hence the majority of treatments are targeted at rapidly dividing cells and at molecular targets that represent the bulk of the tumour. This may explain the failure of treatments to eradicate the disease or the recurrence of the cancer [1]. Although current treatments can shrink the size of the tumour, these effects are transient and usually do not improve patient's survival outcomes [102]. For tumours in which the cancer stem cells play role, three possibilities exist. First, the mutation of normal stem cells or progenitor cells into cancer stem cells can lead to the development of the primary tumour. Second, during chemotherapy, most of the primary tumour cells may be destroyed but if cancer stem cells are not eradicated, they become refractory cancer stem cells and may lead to recurrence of tumour. Third, the cancer stem cells may emigrate to distal sites from the primary tumour and cause metastasis[103]. Theoretically, identification of the cancer stem cells may allow the development of treatment modalities that target the cancer stem cells rather than rapidly dividing cells in the cancer. This may cure the cancer as the remaining cells in the cancer growth have limited proliferative capability (figure 3). If cytotoxic agents spare TICs, the disease is more likely to relapse. The TICs have been shown to have different sensitivity to different chemotherapeutic agents such as TICs in leukaemia are less sensitive to daunorubicin[104] and cytarabine[105].
Although the idea of the therapies focused on the cancer stem cells may look exciting, targeting the cancer stem cells may not be easy. The cancer stem cells are relatively quiescent compared to other cancer cells and do not appear to have the hyper-proliferation signals activated such as tyrosine kinase. These make the cancer stem cells resistant to the toxicity of the anti-cancer drugs, which traditionally target the rapidly dividing cells. In addition, the tumour suppressor gene PTEN[106], polycomb gene Bmi1 [107] and the signal transduction pathways such as the Sonic Hedgehog (Shh), Notch and Wnt that are crucial for normal stem cell regulation, have been shown to be deregulated in the process of cancinogenesis[87]. These deregulated signalling pathways and gene expressions may have impact on response to cancer therapy. One approach to target the cancer stem cells may be the identification of the markers that are specific for the cancer stem cells compared to normal stem cells such as haematopoietic stem cells express Thy-1 and c-kit whereas leukaemic stem cells express IL-3 (interleukin-3) receptor α-chain [108, 109].
Much of the research is now focused on targeting the essential genes or pathways crucial for the cancer development through the cancer stem cells, with any possible therapies targeted against TICs. One such example is the use of Gleevec® in chronic myeloid leukaemia that targets the ATP-binding domain of the Abl kinase. Most patients in this study experienced the complete cytogenetic responses[110, 111]. although the therapy may not be curative due to reported presence of the fusion transcript[112]. A comparison of the pathways that regulate the stem cell homing with those responsible for metastasis may prove useful to minimise the toxic effects of the drugs. Treatment of mice with a Hedgehog (Hh) pathway inhibitor such as cyclopamine [113] inhibits the growth of medulloblastomas in mouse models, without any apparent toxicity. Thus, the Hh pathway may be inactive in most normal adult tissues, thus minimising the toxicity effects of these inhibitors [114]. Thus, the concept of the cancer stem cells has opened new areas of research in carcinogenesis and future treatment options.
Conclusion and future prospectus
Presently, cancer therapy has entered in to an exciting new era, with traditional therapies such as chemotherapy, radiotherapy and surgery on one side while the stem cells on the other hand. Apart from their well-known role in immuno-reconstitution, the stem cells have attracted much attention especially with the new gene technologies such as the gene incorporation into the eukaryotic cells allowing more focused delivery of the anti-cancer agents. Now the cancer may be considered as a cancer stem cell disorder rather than that of rapidly growing cells. Although the origin of the cancer stem cells is yet to be defined, the concept of the cancer stem cells may allow new treatment options in the possible cure of the cancer. However, further research is required to identify and separate the cancer stem cells in various cancers from normal stem cells and other cancer cells. Further work is also required to differentiate the genes and signalling pathways in the process of the carcinogenesis from cancer stem cells for development of new therapies, with the eventual goal of eliminating the residual disease and recurrence.
References
Reya T, Morrison SJ, Clarke MF, Weissman IL: Stem cells, cancer, and cancer stem cells. Nature. 2001, 414: 105-111. 10.1038/35102167.
Soltysova A, Altanerova V, Altaner C: Cancer stem cells. Neoplasma. 2005, 52: 435-440.
Jiang Y, Jahagirdar BN, Reinhardt RL, Schwartz RE, Keene CD, Ortiz-Gonzalez XR, Reyes M, Lenvik T, Lund T, Blackstad M, Du J, Aldrich S, Lisberg A, Low WC, Largaespada DA, Verfaillie CM: Pluripotency of mesenchymal stem cells derived from adult marrow. Nature. 2002, 418: 41-49. 10.1038/nature00870.
Kim CF, Jackson EL, Woolfenden AE, Lawrence S, Babar I, Vogel S, Crowley D, Bronson RT, Jacks T: Identification of bronchioalveolar stem cells in normal lung and lung cancer. Cell. 2005, 121: 823-835. 10.1016/j.cell.2005.03.032.
Hatfield SD, Shcherbata HR, Fischer KA, Nakahara K, Carthew RW, Ruohola-Baker H: Stem cell division is regulated by the microRNA pathway. Nature. 2005, 435: 974-978. 10.1038/nature03816.
Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS, Jones JM: Embryonic stem cell lines derived from human blastocysts. Science. 1998, 282: 1145-1147. 10.1126/science.282.5391.1145.
Serakinci N, Guldberg P, Burns JS, Abdallah B, Schrodder H, Jensen T, Kassem M: Adult human mesenchymal stem cell as a target for neoplastic transformation. Oncogene. 2004, 23: 5095-5098. 10.1038/sj.onc.1207651.
Sylvester KG, Longaker MT: Stem cells: review and update. Arch Surg. 2004, 139: 93-99. 10.1001/archsurg.139.1.93.
Simonsen JL, Rosada C, Serakinci N, Justesen J, Stenderup K, Rattan SI, Jensen TG, Kassem M: Telomerase expression extends the proliferative life-span and maintains the osteogenic potential of human bone marrow stromal cells. Nat Biotechnol. 2002, 20: 592-596. 10.1038/nbt0602-592.
Awad HA, Wickham MQ, Leddy HA, Gimble JM, Guilak F: Chondrogenic differentiation of adipose-derived adult stem cells in agarose, alginate, and gelatin scaffolds. Biomaterials. 2004, 25: 3211-3222. 10.1016/j.biomaterials.2003.10.045.
Lee OK, Kuo TK, Chen WM, Lee KD, Hsieh SL, Chen TH: Isolation of multipotent mesenchymal stem cells from umbilical cord blood. Blood. 2004, 103: 1669-1675. 10.1182/blood-2003-05-1670.
Miura M, Gronthos S, Zhao M, Lu B, Fisher LW, Robey PG, Shi S: SHED: stem cells from human exfoliated deciduous teeth. Proc Natl Acad Sci U S A. 2003, 100: 5807-5812. 10.1073/pnas.0937635100.
Sottile V, Halleux C, Bassilana F, Keller H, Seuwen K: Stem cell characteristics of human trabecular bone-derived cells. Bone. 2002, 30: 699-704. 10.1016/S8756-3282(02)00674-9.
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR: Multilineage potential of adult human mesenchymal stem cells. Science. 1999, 284: 143-147. 10.1126/science.284.5411.143.
Dragoo JL, Samimi B, Zhu M, Hame SL, Thomas BJ, Lieberman JR, Hedrick MH, Benhaim P: Tissue-engineered cartilage and bone using stem cells from human infrapatellar fat pads. J Bone Joint Surg Br. 2003, 85: 740-747.
Huang JI, Zuk PA, Jones NF, Zhu M, Lorenz HP, Hedrick MH, Benhaim P: Chondrogenic potential of multipotential cells from human adipose tissue. Plast Reconstr Surg. 2004, 113: 585-594. 10.1097/01.PRS.0000101063.27008.E1.
De Ugarte DA, Morizono K, Elbarbary A, Alfonso Z, Zuk PA, Zhu M, Dragoo JL, Ashjian P, Thomas B, Benhaim P, Chen I, Fraser J, Hedrick MH: Comparison of multi-lineage cells from human adipose tissue and bone marrow. Cells Tissues Organs. 2003, 174: 101-109. 10.1159/000071150.
Talmadge JE, Reed E, Ino K, Kessinger A, Kuszynski C, Heimann D, Varney M, Jackson J, Vose JM, Bierman PJ: Rapid immunologic reconstitution following transplantation with mobilized peripheral blood stem cells as compared to bone marrow. Bone Marrow Transplant. 1997, 19: 161-172. 10.1038/sj.bmt.1700626.
Fisher DC, Peters WP: Advances in the clinical use of granulocyte colony-stimulating factor and granulocyte-macrophage colony-stimulating factor to intensify cancer chemotherapy. Curr Opin Hematol. 1994, 1: 221-227.
Allen TD, Dexter TM: The essential cells of the hemopoietic microenvironment. Exp Hematol. 1984, 12: 517-521.
Mayani H, Guilbert LJ, Janowska-Wieczorek A: Biology of the hemopoietic microenvironment. Eur J Haematol. 1992, 49: 225-233.
Yoder MC, Williams DA: Matrix molecule interactions with hematopoietic stem cells. Exp Hematol. 1995, 23: 961-967.
O'Shaughnessy JA, Tolcher A, Riseberg D, Venzon D, Zujewski J, Noone M, Gossard M, Danforth D, Jacobson J, Chang V, Goldspiel B, Keegan P, Giusti R, Cowan KH: Prospective, randomized trial of 5-fluorouracil, leucovorin, doxorubicin, and cyclophosphamide chemotherapy in combination with the interleukin-3/granulocyte-macrophage colony-stimulating factor (GM-CSF) fusion protein (PIXY321) versus GM-CSF in patients with advanced breast cancer. Blood. 1996, 87: 2205-2211.
Schwartz GN, Warren MK, Rothwell SW, Zujewski J, Halverson DC, Cowan KH, Tolcher A, O'Shaughnessy J, Gress RE: Post-chemotherapy and cytokine pretreated marrow stromal cell layers suppress hematopoiesis from normal donor CD34+ cells. Bone Marrow Transplant. 1998, 22: 457-468. 10.1038/sj.bmt.1701364.
Edwards RG: Stem cells today: B1. Bone marrow stem cells. Reprod Biomed Online. 2004, 9: 541-583.
Fermand JP, Katsahian S, Divine M, Leblond V, Dreyfus F, Macro M, Arnulf B, Royer B, Mariette X, Pertuiset E, Belanger C, Janvier M, Chevret S, Brouet JC, Ravaud P: High-dose therapy and autologous blood stem-cell transplantation compared with conventional treatment in myeloma patients aged 55 to 65 years: long-term results of a randomized control trial from the Group Myelome-Autogreffe. J Clin Oncol. 2005, 23: 9227-9233. 10.1200/JCO.2005.03.0551.
Nitz UA, Mohrmann S, Fischer J, Lindemann W, Berdel WE, Jackisch C, Werner C, Ziske C, Kirchner H, Metzner B, Souchon R, Ruffert U, Schutt G, Pollmanns A, Schmoll HJ, Middecke C, Baltzer J, Schrader I, Wiebringhaus H, Ko Y, Rosel S, Schwenzer T, Wernet P, Hinke A, Bender HG, Frick M: Comparison of rapidly cycled tandem high-dose chemotherapy plus peripheral-blood stem-cell support versus dose-dense conventional chemotherapy for adjuvant treatment of high-risk breast cancer: results of a multicentre phase III trial. Lancet. 2005, 366: 1935-1944. 10.1016/S0140-6736(05)67784-7.
Balduzzi A, Valsecchi MG, Uderzo C, De Lorenzo P, Klingebiel T, Peters C, Stary J, Felice MS, Magyarosy E, Conter V, Reiter A, Messina C, Gadner H, Schrappe M: Chemotherapy versus allogeneic transplantation for very-high-risk childhood acute lymphoblastic leukaemia in first complete remission: comparison by genetic randomisation in an international prospective study. Lancet. 2005, 366: 635-642. 10.1016/S0140-6736(05)66998-X.
Berthold F, Boos J, Burdach S, Erttmann R, Henze G, Hermann J, Klingebiel T, Kremens B, Schilling FH, Schrappe M, Simon T, Hero B: Myeloablative megatherapy with autologous stem-cell rescue versus oral maintenance chemotherapy as consolidation treatment in patients with high-risk neuroblastoma: a randomised controlled trial. Lancet Oncol. 2005, 6: 649-658.
Dreyling M, Lenz G, Hoster E, Van Hoof A, Gisselbrecht C, Schmits R, Metzner B, Truemper L, Reiser M, Steinhauer H, Boiron JM, Boogaerts MA, Aldaoud A, Silingardi V, Kluin-Nelemans HC, Hasford J, Parwaresch R, Unterhalt M, Hiddemann W: Early consolidation by myeloablative radiochemotherapy followed by autologous stem cell transplantation in first remission significantly prolongs progression-free survival in mantle-cell lymphoma: results of a prospective randomized trial of the European MCL Network. Blood. 2005, 105: 2677-2684. 10.1182/blood-2004-10-3883.
Valteau-Couanet D, Faucher C, Auperin A, Michon J, Milpied N, Boiron JM, Bourhis JH, Gisselbrecht C, Vernant JP, Pinna A, Bendahmane B, Delabarre F, Benhamou E: Cost effectiveness of day 5 G-CSF (Lenograstim) administration after PBSC transplantation: results of a SFGM-TC randomised trial. Bone Marrow Transplant. 2005, 36: 547-552. 10.1038/sj.bmt.1705097.
Peters WP, Rosner GL, Vredenburgh JJ, Shpall EJ, Crump M, Richardson PG, Schuster MW, Marks LB, Cirrincione C, Norton L, Henderson IC, Schilsky RL, Hurd DD: Prospective, randomized comparison of high-dose chemotherapy with stem-cell support versus intermediate-dose chemotherapy after surgery and adjuvant chemotherapy in women with high-risk primary breast cancer: a report of CALGB 9082, SWOG 9114, and NCIC MA-13. J Clin Oncol. 2005, 23: 2191-2200. 10.1200/JCO.2005.10.202.
Pico JL, Rosti G, Kramar A, Wandt H, Koza V, Salvioni R, Theodore C, Lelli G, Siegert W, Horwich A, Marangolo M, Linkesch W, Pizzocaro G, Schmoll HJ, Bouzy J, Droz JP, Biron P: A randomised trial of high-dose chemotherapy in the salvage treatment of patients failing first-line platinum chemotherapy for advanced germ cell tumours. Ann Oncol. 2005, 16: 1152-1159. 10.1093/annonc/mdi228.
Breems DA, Boogaerts MA, Dekker AW, Van Putten WL, Sonneveld P, Huijgens PC, Van der LJ, Vellenga E, Gratwohl A, Verhoef GE, Verdonck LF, Lowenberg B: Autologous bone marrow transplantation as consolidation therapy in the treatment of adult patients under 60 years with acute myeloid leukaemia in first complete remission: a prospective randomized Dutch-Belgian Haemato-Oncology Co-operative Group (HOVON) and Swiss Group for Clinical Cancer Research (SAKK) trial. Br J Haematol. 2005, 128: 59-65. 10.1111/j.1365-2141.2004.05282.x.
Schmid P, Schippinger W, Nitsch T, Huebner G, Heilmann V, Schultze W, Hausmaninger H, Wischnewsky M, Possinger K: Up-front tandem high-dose chemotherapy compared with standard chemotherapy with doxorubicin and paclitaxel in metastatic breast cancer: results of a randomized trial. J Clin Oncol. 2005, 23: 432-440. 10.1200/JCO.2005.06.072.
Tricot G, Jagannath S, Vesole D, Nelson J, Tindle S, Miller L, Cheson B, Crowley J, Barlogie B: Peripheral blood stem cell transplants for multiple myeloma: identification of favorable variables for rapid engraftment in 225 patients. Blood. 1995, 85: 588-596.
Boccadoro M, Palumbo A, Bringhen S, Merletti F, Ciccone G, Richiardi L, Rus C, Bertola A, Giaccone L, Omede P, Musto P: Oral melphalan at diagnosis hampers adequate collection of peripheral blood progenitor cells in multiple myeloma. Haematologica. 2002, 87: 846-850.
Blair A, Baker CL, Pamphilon DH, Judson PA: Ex vivo expansion of megakaryocyte progenitor cells from normal bone marrow and peripheral blood and from patients with haematological malignancies. Br J Haematol. 2002, 116: 912-919. 10.1046/j.0007-1048.2002.03354.x.
McNiece I, Jones R, Bearman SI, Cagnoni P, Nieto Y, Franklin W, Ryder J, Steele A, Stoltz J, Russell P, McDermitt J, Hogan C, Murphy J, Shpall EJ: Ex vivo expanded peripheral blood progenitor cells provide rapid neutrophil recovery after high-dose chemotherapy in patients with breast cancer. Blood. 2000, 96: 3001-3007.
Weiss L, Or R, Slavin S, Naparstek E, Reich S, Abdul-Hai A: Immunotherapy of murine leukemia following non-myeloablative conditioning with naive or G-CSF mobilized blood or bone marrow stem cells. Cancer Immunol Immunother. 2004, 53: 358-362. 10.1007/s00262-003-0440-5.
Couban S, Simpson DR, Barnett MJ, Bredeson C, Hubesch L, Howson-Jan K, Shore TB, Walker IR, Browett P, Messner HA, Panzarella T, Lipton JH: A randomized multicenter comparison of bone marrow and peripheral blood in recipients of matched sibling allogeneic transplants for myeloid malignancies. Blood. 2002, 100: 1525-1531. 10.1182/blood-2002-01-0048.
Storek J, Dawson MA, Storer B, Stevens-Ayers T, Maloney DG, Marr KA, Witherspoon RP, Bensinger W, Flowers ME, Martin P, Storb R, Appelbaum FR, Boeckh M: Immune reconstitution after allogeneic marrow transplantation compared with blood stem cell transplantation. Blood. 2001, 97: 3380-3389. 10.1182/blood.V97.11.3380.
Hernandez MD, del Canizo MC, Gonzalez M, Caballero MD, Lopez-Berges MC, Vazquez L, Orfao A, Corral M, Nieto MJ, San Miguel JF: [Immune reconstitution after autologous progenitor hemopoietic cell transplantation. A study comparing autologous bone marrow and autologous peripheral blood transplantation]. Med Clin (Barc ). 1998, 110: 768-773.
Attal M, Harousseau JL, Facon T, Guilhot F, Doyen C, Fuzibet JG, Monconduit M, Hulin C, Caillot D, Bouabdallah R, Voillat L, Sotto JJ, Grosbois B, Bataille R: Single versus double autologous stem-cell transplantation for multiple myeloma. N Engl J Med. 2003, 349: 2495-2502. 10.1056/NEJMoa032290.
Szyper-Kravitz M, Uziel O, Shapiro H, Radnay J, Katz T, Rowe JM, Lishner M, Lahav M: Granulocyte colony-stimulating factor administration upregulates telomerase activity in CD34+ haematopoietic cells and may prevent telomere attrition after chemotherapy. Br J Haematol. 2003, 120: 329-336. 10.1046/j.1365-2141.2003.04043.x.
Danova M, Porta C, Ferrari S, Brugnatelli S, Comolli G, Riccardi A, Ascari E: Cell cycle status and apoptosis of hematopoietic progenitor cells released into the peripheral blood after taxanes and granulocyte colony-stimulating factor in breast cancer patients. Oncol Rep. 2000, 7: 585-589.
Somlo G, Sniecinski I, ter Veer A, Longmate J, Knutson G, Vuk-Pavlovic S, Bhatia R, Chow W, Leong L, Morgan R, Margolin K, Raschko J, Shibata S, Tetef M, Yen Y, Forman S, Jones D, Ashby M, Fyfe G, Hellmann S, Doroshow JH: Recombinant human thrombopoietin in combination with granulocyte colony-stimulating factor enhances mobilization of peripheral blood progenitor cells, increases peripheral blood platelet concentration, and accelerates hematopoietic recovery following high-dose chemotherapy. Blood. 1999, 93: 2798-2806.
Canales MA, Arrieta R, Hernandez-Garcia C, Bustos JG, Aguado MJ, Hernandez-Navarro F: A single apheresis to achieve a high number of peripheral blood CD34+ cells in a lithium-treated patient with acute myeloid leukaemia. Bone Marrow Transplant. 1999, 23: 305-10.1038/sj.bmt.1701566.
Prosper F, Sola C, Hornedo J, Arbona C, Menendez P, Orfao A, Lluch A, Cortes-Funes H, Lopez JJ, Garcia-Conde J: Mobilization of peripheral blood progenitor cells with a combination of cyclophosphamide, r-metHuSCF and filgrastim in patients with breast cancer previously treated with chemotherapy. Leukemia. 2003, 17: 437-441. 10.1038/sj.leu.2402750.
Hernandez-Boluda JC, Carreras E, Cervantes F, Marin P, Arellano-Rodrigo E, Rovira M, Sole F, Lloveras E, Espinet B, Ocejo A, Montserrat E: Collection of Philadelphia-negative stem cells using recombinant human granulocyte colony-stimulating factor in chronic myeloid leukemia patients treated with alpha-interferon. Haematologica. 2002, 87: 17-22.
Ross AA, Cooper BW, Lazarus HM, Mackay W, Moss TJ, Ciobanu N, Tallman MS, Kennedy MJ, Davidson NE, Sweet D, .: Detection and viability of tumor cells in peripheral blood stem cell collections from breast cancer patients using immunocytochemical and clonogenic assay techniques. Blood. 1993, 82: 2605-2610.
Dal CL, Cottu PH, Lotz JP, Robert I, Extra JM, Miclea JM, Marty M, Marolleau JP: Residual tumor cell contamination in peripheral blood stem cells collections of 117 breast cancer patients evaluated by immunocytochemical technique. J Hematother Stem Cell Res. 2001, 10: 855-862. 10.1089/152581601317210944.
Kruger W, Togel F, Kroger N, Rossing S, Gieseking F, Gutensohn K, Lindner C, Janicke F, Zander AR: Tumour cell detection in G-CSF mobilised stem cell harvests of patients with breast cancer. Med Oncol. 1999, 16: 17-22.
Passos-Coelho JL, Ross AA, Kahn DJ, Moss TJ, Davis JM, Huelskamp AM, Noga SJ, Davidson NE, Kennedy MJ: Similar breast cancer cell contamination of single-day peripheral-blood progenitor-cell collections obtained after priming with hematopoietic growth factor alone or after cyclophosphamide followed by growth factor. J Clin Oncol. 1996, 14: 2569-2575.
Pedrazzoli P, Battaglia M, Da Prada GA, Lanza A, Cuomo A, Bertolini F, Pavesi L, Robustelli della CG: Role of tumor cells contaminating the graft in breast cancer recurrence after high-dose chemotherapy. Bone Marrow Transplant. 1997, 20: 167-169. 10.1038/sj.bmt.1700854.
Cooper BW, Moss TJ, Ross AA, Ybanez J, Lazarus HM: Occult tumor contamination of hematopoietic stem-cell products does not affect clinical outcome of autologous transplantation in patients with metastatic breast cancer. J Clin Oncol. 1998, 16: 3509-3517.
Cagnoni PJ, Jones RB, Bearman SI, Ross M, Hami L, Franklin WA, Capizzi R, Schein PS, Shpall EJ: Use of amifostine in bone marrow purging. Semin Oncol. 1996, 23: 44-48.
Poloni A, Leoni P, Curzi L, Cantori I, Mancini S, Montanari M, Masia MC, Olivieri A: Ex vivo pharmacological purging of leukapheresis collections with nitrogen mustard: amifostine pretreatment improves both early and late peripheral blood progenitor cell recovery. Exp Hematol. 1999, 27: 1548-1556. 10.1016/S0301-472X(99)00086-7.
Altes A, Sierra J, Esteve J, Martin-Henao G, Marin P, Sureda A, Briones J, Martino R, Villamor N, Colomer D, Carreras E, Garcia J, Brunet S, Montserrat E: CD34+-enriched-CD19+-depleted autologous peripheral blood stem cell transplantation for chronic lymphoproliferative disorders: high purging efficiency but increased risk of severe infections. Exp Hematol. 2002, 30: 824-830. 10.1016/S0301-472X(02)00828-7.
Martin-Rendon E, Watt SM: Exploitation of stem cell plasticity. Transfus Med. 2003, 13: 325-349. 10.1111/j.1365-3148.2003.00462.x.
Beccheroni A, Lucarelli E, Donati D, Sangiorgi L, Capponcelli S, Gorini M, Zambon BA, Giardino R, Mercuri M, Ferrari S, Bacci G, Picci P: Recovery of stromal stem cells in bone sarcoma patients after chemotherapy: implication for cell-based therapy in bone defect reconstruction. Oncol Rep. 2003, 10: 891-896.
Jager M, Schultheis A, Westhoff B, Krauspe R: Osteogenic progenitor cell potency after high-dose chemotherapy (COSS-96). Anticancer Res. 2005, 25: 947-954.
Kang HJ, Kim HS, Koo BK, Kim YJ, Lee D, Sohn DW, Oh BH, Park YB: Intracoronary infusion of the mobilized peripheral blood stem cell by G-CSF is better than mobilization alone by G-CSF for improvement of cardiac function and remodeling: 2-year follow-up results of the Myocardial Regeneration and Angiogenesis in Myocardial Infarction with G-CSF and Intra-Coronary Stem Cell Infusion (MAGIC Cell) 1 trial. Am Heart J. 2007, 153: 237-238. 10.1016/j.ahj.2006.11.004.
Klein HM, Ghodsizad A, Marktanner R, Poll L, Voelkel T, Mohammad Hasani MR, Piechaczek C, Feifel N, Stockschlaeder M, Burchardt ER, Kar BJ, Gregoric I, Gams E: Intramyocardial implantation of CD133+ stem cells improved cardiac function without bypass surgery. Heart Surg Forum. 2007, 10: E66-E69. 10.1532/HSF98.20061054.
Engelmann MG, Theiss HD, Hennig-Theiss C, Huber A, Wintersperger BJ, Werle-Ruedinger AE, Schoenberg SO, Steinbeck G, Franz WM: Autologous bone marrow stem cell mobilization induced by granulocyte colony-stimulating factor after subacute ST-segment elevation myocardial infarction undergoing late revascularization: final results from the G-CSF-STEMI (Granulocyte Colony-Stimulating Factor ST-Segment Elevation Myocardial Infarction) trial. J Am Coll Cardiol. 2006, 48: 1712-1721. 10.1016/j.jacc.2006.07.044.
Chawla-Sarkar M, Leaman DW, Borden EC: Preferential induction of apoptosis by interferon (IFN)-beta compared with IFN-alpha2: correlation with TRAIL/Apo2L induction in melanoma cell lines. Clin Cancer Res. 2001, 7: 1821-1831.
Lokshin A, Mayotte JE, Levitt ML: Mechanism of interferon beta-induced squamous differentiation and programmed cell death in human non-small-cell lung cancer cell lines. J Natl Cancer Inst. 1995, 87: 206-212. 10.1093/jnci/87.3.206.
Zhang H, Koty PP, Mayotte J, Levitt ML: Induction of multiple programmed cell death pathways by IFN-beta in human non-small-cell lung cancer cell lines. Exp Cell Res. 1999, 247: 133-141. 10.1006/excr.1998.4329.
Studeny M, Marini FC, Dembinski JL, Zompetta C, Cabreira-Hansen M, Bekele BN, Champlin RE, Andreeff M: Mesenchymal stem cells: potential precursors for tumor stroma and targeted-delivery vehicles for anticancer agents. J Natl Cancer Inst. 2004, 96: 1593-1603.
Studeny M, Marini FC, Champlin RE, Zompetta C, Fidler IJ, Andreeff M: Bone marrow-derived mesenchymal stem cells as vehicles for interferon-beta delivery into tumors. Cancer Res. 2002, 62: 3603-3608.
Nakamizo A, Marini F, Amano T, Khan A, Studeny M, Gumin J, Chen J, Hentschel S, Vecil G, Dembinski J, Andreeff M, Lang FF: Human bone marrow-derived mesenchymal stem cells in the treatment of gliomas. Cancer Res. 2005, 65: 3307-3318.
Muller FJ, Snyder EY, Loring JF: Gene therapy: can neural stem cells deliver?. Nat Rev Neurosci. 2006, 7: 75-84. 10.1038/nrn1829.
Anderson SA, Glod J, Arbab AS, Noel M, Ashari P, Fine HA, Frank JA: Noninvasive MR imaging of magnetically labeled stem cells to directly identify neovasculature in a glioma model. Blood. 2005, 105: 420-425. 10.1182/blood-2004-06-2222.
Hamada H, Kobune M, Nakamura K, Kawano Y, Kato K, Honmou O, Houkin K, Matsunaga T, Niitsu Y: Mesenchymal stem cells (MSC) as therapeutic cytoreagents for gene therapy. Cancer Sci. 2005, 96: 149-156. 10.1111/j.1349-7006.2005.00032.x.
Bodnar AG, Ouellette M, Frolkis M, Holt SE, Chiu CP, Morin GB, Harley CB, Shay JW, Lichtsteiner S, Wright WE: Extension of life-span by introduction of telomerase into normal human cells. Science. 1998, 279: 349-352. 10.1126/science.279.5349.349.
Abdallah BM, Haack-Sorensen M, Burns JS, Elsnab B, Jakob F, Hokland P, Kassem M: Maintenance of differentiation potential of human bone marrow mesenchymal stem cells immortalized by human telomerase reverse transcriptase gene despite [corrected] extensive proliferation. Biochem Biophys Res Commun. 2005, 326: 527-538. 10.1016/j.bbrc.2004.11.059.
Natesan S: Telomerase extends a helping hand to progenitor cells. Trends Biotechnol. 2005, 23: 1-3. 10.1016/j.tibtech.2004.11.009.
Roy NS, Nakano T, Keyoung HM, Windrem M, Rashbaum WK, Alonso ML, Kang J, Peng W, Carpenter MK, Lin J, Nedergaard M, Goldman SA: Telomerase immortalization of neuronally restricted progenitor cells derived from the human fetal spinal cord. Nat Biotechnol. 2004, 22: 297-305. 10.1038/nbt944.
Hung SC, Yang DM, Chang CF, Lin RJ, Wang JS, Low-Tone HL, Yang WK: Immortalization without neoplastic transformation of human mesenchymal stem cells by transduction with HPV16 E6/E7 genes. Int J Cancer. 2004, 110: 313-319. 10.1002/ijc.20126.
Finlan LE, Hupp TR: Epidermal stem cells and cancer stem cells: insights into cancer and potential therapeutic strategies. Eur J Cancer. 2006, 42: 1283-1292. 10.1016/j.ejca.2006.01.047.
Bixby S, Kruger GM, Mosher JT, Joseph NM, Morrison SJ: Cell-intrinsic differences between stem cells from different regions of the peripheral nervous system regulate the generation of neural diversity. Neuron. 2002, 35: 643-656. 10.1016/S0896-6273(02)00825-5.
SOUTHAM CM: Relationships of immunology to cancer: a review. Cancer Res. 1960, 20: 271-291.
Hope KJ, Jin L, Dick JE: Human acute myeloid leukemia stem cells. Arch Med Res. 2003, 34: 507-514. 10.1016/j.arcmed.2003.08.007.
Park CH, Bergsagel DE, McCulloch EA: Mouse myeloma tumor stem cells: a primary cell culture assay. J Natl Cancer Inst. 1971, 46: 411-422.
Bonnet D, Dick JE: Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med. 1997, 3: 730-737. 10.1038/nm0797-730.
Dick JE: Breast cancer stem cells revealed. Proc Natl Acad Sci U S A. 2003, 100: 3547-3549. 10.1073/pnas.0830967100.
Galderisi U, Cipollaro M, Giordano A: Stem cells and brain cancer. Cell Death Differ. 2006, 13: 5-11. 10.1038/sj.cdd.4401757.
Al-Hajj M, Wicha MS, ito-Hernandez A, Morrison SJ, Clarke MF: Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci U S A. 2003, 100: 3983-3988. 10.1073/pnas.0530291100.
Hemmati HD, Nakano I, Lazareff JA, Masterman-Smith M, Geschwind DH, Bronner-Fraser M, Kornblum HI: Cancerous stem cells can arise from pediatric brain tumors. Proc Natl Acad Sci U S A. 2003, 100: 15178-15183. 10.1073/pnas.2036535100.
Knudson AG, Strong LC, Anderson DE: Heredity and cancer in man. Prog Med Genet. 1973, 9:113-58.: 113-158.
Morrison SJ, Qian D, Jerabek L, Thiel BA, Park IK, Ford PS, Kiel MJ, Schork NJ, Weissman IL, Clarke MF: A genetic determinant that specifically regulates the frequency of hematopoietic stem cells. J Immunol. 2002, 168: 635-642.
Al-Hajj M, Becker MW, Wicha M, Weissman I, Clarke MF: Therapeutic implications of cancer stem cells. Curr Opin Genet Dev. 2004, 14: 43-47. 10.1016/j.gde.2003.11.007.
Sell S: Stem cell origin of cancer and differentiation therapy. Crit Rev Oncol Hematol. 2004, 51: 1-28.
Wang JC, Dick JE: Cancer stem cells: lessons from leukemia. Trends Cell Biol. 2005, 15: 494-501. 10.1016/j.tcb.2005.07.004.
Cozzio A, Passegue E, Ayton PM, Karsunky H, Cleary ML, Weissman IL: Similar MLL-associated leukemias arising from self-renewing stem cells and short-lived myeloid progenitors. Genes Dev. 2003, 17: 3029-3035. 10.1101/gad.1143403.
Jamieson CH, Ailles LE, Dylla SJ, Muijtjens M, Jones C, Zehnder JL, Gotlib J, Li K, Manz MG, Keating A, Sawyers CL, Weissman IL: Granulocyte-macrophage progenitors as candidate leukemic stem cells in blast-crisis CML. N Engl J Med. 2004, 351: 657-667. 10.1056/NEJMoa040258.
Weissman IL: Normal and neoplastic stem cells. Novartis Found Symp. 2005, 265:35-50; discussion 50-4, 92-7.: 35-50.
Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T, Henkelman RM, Cusimano MD, Dirks PB: Identification of human brain tumour initiating cells. Nature. 2004, 432: 396-401. 10.1038/nature03128.
Yuan X, Curtin J, Xiong Y, Liu G, Waschsmann-Hogiu S, Farkas DL, Black KL, Yu JS: Isolation of cancer stem cells from adult glioblastoma multiforme. Oncogene. 2004, 23: 9392-9400. 10.1038/sj.onc.1208311.
Galli R, Binda E, Orfanelli U, Cipelletti B, Gritti A, De Vitis S, Fiocco R, Foroni C, Dimeco F, Vescovi A: Isolation and characterization of tumorigenic, stem-like neural precursors from human glioblastoma. Cancer Res. 2004, 64: 7011-7021. 10.1158/0008-5472.CAN-04-1364.
Xin L, Lawson DA, Witte ON: The Sca-1 cell surface marker enriches for a prostate-regenerating cell subpopulation that can initiate prostate tumorigenesis. Proc Natl Acad Sci U S A. 2005, 102: 6942-6947. 10.1073/pnas.0502320102.
Stockler M, Wilcken NR, Ghersi D, Simes RJ: Systematic reviews of chemotherapy and endocrine therapy in metastatic breast cancer. Cancer Treat Rev. 2000, 26: 151-168. 10.1053/ctrv.1999.0161.
Jordan CT, Guzman ML, Noble M: Cancer stem cells. N Engl J Med. 2006, 355: 1253-1261. 10.1056/NEJMra061808.
Costello RT, Mallet F, Gaugler B, Sainty D, Arnoulet C, Gastaut JA, Olive D: Human acute myeloid leukemia CD34+/CD38- progenitor cells have decreased sensitivity to chemotherapy and Fas-induced apoptosis, reduced immunogenicity, and impaired dendritic cell transformation capacities. Cancer Res. 2000, 60: 4403-4411.
Guzman ML, Swiderski CF, Howard DS, Grimes BA, Rossi RM, Szilvassy SJ, Jordan CT: Preferential induction of apoptosis for primary human leukemic stem cells. Proc Natl Acad Sci U S A. 2002, 99: 16220-16225. 10.1073/pnas.252462599.
Groszer M, Erickson R, Scripture-Adams DD, Lesche R, Trumpp A, Zack JA, Kornblum HI, Liu X, Wu H: Negative regulation of neural stem/progenitor cell proliferation by the Pten tumor suppressor gene in vivo. Science. 2001, 294: 2186-2189. 10.1126/science.1065518.
Park IK, Qian D, Kiel M, Becker MW, Pihalja M, Weissman IL, Morrison SJ, Clarke MF: Bmi-1 is required for maintenance of adult self-renewing haematopoietic stem cells. Nature. 2003, 423: 302-305. 10.1038/nature01587.
Blair A, Hogge DE, Ailles LE, Lansdorp PM, Sutherland HJ: Lack of expression of Thy-1 (CD90) on acute myeloid leukemia cells with long-term proliferative ability in vitro and in vivo. Blood. 1997, 89: 3104-3112.
Blair A, Sutherland HJ: Primitive acute myeloid leukemia cells with long-term proliferative ability in vitro and in vivo lack surface expression of c-kit (CD117). Exp Hematol. 2000, 28: 660-671. 10.1016/S0301-472X(00)00155-7.
Druker BJ, Tamura S, Buchdunger E, Ohno S, Segal GM, Fanning S, Zimmermann J, Lydon NB: Effects of a selective inhibitor of the Abl tyrosine kinase on the growth of Bcr-Abl positive cells. Nat Med. 1996, 2: 561-566. 10.1038/nm0596-561.
O'Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F, Cornelissen JJ, Fischer T, Hochhaus A, Hughes T, Lechner K, Nielsen JL, Rousselot P, Reiffers J, Saglio G, Shepherd J, Simonsson B, Gratwohl A, Goldman JM, Kantarjian H, Taylor K, Verhoef G, Bolton AE, Capdeville R, Druker BJ: Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2003, 348: 994-1004. 10.1056/NEJMoa022457.
Branford S, Hughes TP, Rudzki Z: Monitoring chronic myeloid leukaemia therapy by real-time quantitative PCR in blood is a reliable alternative to bone marrow cytogenetics. Br J Haematol. 1999, 107: 587-599. 10.1046/j.1365-2141.1999.01749.x.
Berman DM, Karhadkar SS, Hallahan AR, Pritchard JI, Eberhart CG, Watkins DN, Chen JK, Cooper MK, Taipale J, Olson JM, Beachy PA: Medulloblastoma growth inhibition by hedgehog pathway blockade. Science. 2002, 297: 1559-1561. 10.1126/science.1073733.
Beachy PA, Karhadkar SS, Berman DM: Tissue repair and stem cell renewal in carcinogenesis. Nature. 2004, 432: 324-331. 10.1038/nature03100.
Oehler VG, Radich JP, Storer B, Blume KG, Chauncey T, Clift R, Snyder DS, Forman SJ, Flowers ME, Martin P, Guthrie KA, Negrin RS, Appelbaum FR, Bensinger W: Randomized trial of allogeneic related bone marrow transplantation versus peripheral blood stem cell transplantation for chronic myeloid leukemia. Biol Blood Marrow Transplant. 2005, 11: 85-92. 10.1016/j.bbmt.2004.09.010.
Heldal D, Brinch L, Tjonnfjord G, Solheim BG, Egeland T, Albrechtsen D, Aamodt G, Evensen SA: Fewer relapses and increased chronic GVHD in patients transplanted with blood stem cells: a 5-year follow-up in a single centre study. Bone Marrow Transplant. 2003, 32: 257-264. 10.1038/sj.bmt.1704127.
Nucci M, Andrade F, Vigorito A, Trabasso P, Aranha JF, Maiolino A, De Souza CA: Infectious complications in patients randomized to receive allogeneic bone marrow or peripheral blood transplantation. Transpl Infect Dis. 2003, 5: 167-173. 10.1111/j.1399-3062.2003.00033.x.
Powles R, Mehta J, Kulkarni S, Treleaven J, Millar B, Marsden J, Shepherd V, Rowland A, Sirohi B, Tait D, Horton C, Long S, Singhal S: Allogeneic blood and bone-marrow stem-cell transplantation in haematological malignant diseases: a randomised trial. Lancet. 2000, 355: 1231-1237. 10.1016/S0140-6736(00)02090-0.
Mahmoud H, Fahmy O, Kamel A, Kamel M, El Haddad A, El Kadi D: Peripheral blood vs bone marrow as a source for allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 1999, 24: 355-358. 10.1038/sj.bmt.1701906.
Barbui AM, Galli M, Dotti G, Belli N, Borleri G, Gritti G, Bellavita P, Viero P, Comotti B, Barbui T, Rambaldi A: Negative selection of peripheral blood stem cells to support a tandem autologous transplantation programme in multiple myeloma. Br J Haematol. 2002, 116: 202-210. 10.1046/j.0007-1048.2001.03189.x.
Stewart AK, Vescio R, Schiller G, Ballester O, Noga S, Rugo H, Freytes C, Stadtmauer E, Tarantolo S, Sahebi F, Stiff P, Meharchard J, Schlossman R, Brown R, Tully H, Benyunes M, Jacobs C, Berenson R, White M, DiPersio J, Anderson KC, Berenson J: Purging of autologous peripheral-blood stem cells using CD34 selection does not improve overall or progression-free survival after high-dose chemotherapy for multiple myeloma: results of a multicenter randomized controlled trial. J Clin Oncol. 2001, 19: 3771-3779.
Vescio R, Schiller G, Stewart AK, Ballester O, Noga S, Rugo H, Freytes C, Stadtmauer E, Tarantolo S, Sahebi F, Stiff P, Meharchard J, Schlossman R, Brown R, Tully H, Benyunes M, Jacobs C, Berenson R, DiPersio J, Anderson K, Berenson J: Multicenter phase III trial to evaluate CD34(+) selected versus unselected autologous peripheral blood progenitor cell transplantation in multiple myeloma. Blood. 1999, 93: 1858-1868.
Shpall EJ, Stemmer SM, Bearman SI, Myers S, Purdy M, Jones RB: New strategies in marrow purging for breast cancer patients receiving high-dose chemotherapy with autologous bone marrow transplantation. Breast Cancer Res Treat. 1993, 26 Suppl: S19-S23. 10.1007/BF00668356.
Huang Y, Yang J, Wang XB, Becker FF, Gascoyne PR: The removal of human breast cancer cells from hematopoietic CD34+ stem cells by dielectrophoretic field-flow-fractionation. J Hematother Stem Cell Res. 1999, 8: 481-490. 10.1089/152581699319939.
Borbolla-Escoboza JR, Leon MI, Collados MT, Baez E, Baltasar S, Hernandez R, Rojas JC: Induction of apoptosis and effect on CD20+ using rituximab on autologous peripheral blood stem cell harvests from patients with B cell lymphomas. Stem Cells Dev. 2004, 13: 193-196. 10.1089/154732804323046792.
Craiu A, Saito Y, Limon A, Eppich HM, Olson DP, Rodrigues N, Adams GB, Dombkowski D, Richardson P, Schlossman R, Choi PS, Grogins J, O'Connor PG, Cohen K, Attar EC, Freshman J, Rich R, Mangano JA, Gribben JG, Anderson KC, Scadden DT: Flowing cells through pulsed electric fields efficiently purges stem cell preparations of contaminating myeloma cells while preserving stem cell function. Blood. 2005, 105: 2235-2238. 10.1182/blood-2003-12-4399.
Wierenga PK, Setroikromo R, Kamps G, Kampinga HH, Vellenga E: Differences in heat sensitivity between normal and acute myeloid leukemic stem cells: feasibility of hyperthermic purging of leukemic cells from autologous stem cell grafts. Exp Hematol. 2003, 31: 421-427. 10.1016/S0301-472X(03)00049-3.
Author information
Authors and Affiliations
Corresponding author
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Sagar, J., Chaib, B., Sales, K. et al. Role of stem cells in cancer therapy and cancer stem cells: a review. Cancer Cell Int 7, 9 (2007). https://doi.org/10.1186/1475-2867-7-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2867-7-9