Abstract
Background
Four single nucleotide polymorphisms (SNPs) (rs2237892, rs2237895, rs2237897, and rs2283228) in KCNQ1 are reported to be associated with type 2 diabetes mellitus (T2DM), possibly caused by a reduction in insulin secretion and higher fasting glucose, but the results are inconsistent. We investigated whether these 4 genetic markers are associated with serum lipid metabolism in a middle-aged Chinese Han population.
Methods
We enrolled 398 consecutive patients, including 180 with premature coronary artery disease (CAD) (male < 55 years, female < 65 years) and 218 controls without documented CAD. All subjects were genotyped for 4 SNPs by using the ligase detection reaction method. Fasting blood sugar (FBS) and plasma concentrations of total cholesterol, triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), apolipoprotein A1(apo A1), and apolipoprotein B (apo B) were determined by standard biochemical methods. Main anthropometric and metabolic characteristics are analyzed among 3 genotypes at rs2283228, rs2237895, rs2237897, or rs2237892 in KCNQ1.
Results
The 3 genotypes AA, AC, and CC were present in rs2283228 and rs2237895, and the 3 genotypes CC, CT, and TT were present in rs2237897 and rs2237892. The minor genotypes CC at rs2283228 and TT at rs2237892 were associated with higher levels of TG (P = 0.007 and 0.026, respectively). Furthermore, subjects with the CC genotype at rs2283228 had lower levels of HDL-C and apo A1 than in the other 2 genotype groups (P = 0.052 and 0.055, respectively). No other associations were detected between these 4 SNPs and FBS or other lipid parameters.
Conclusions
Our data suggest that rs2283228 and rs2237892 in KCNQ1 are associated with lipid metabolism in a middle-aged Chinese Han population.
Similar content being viewed by others
Background
KCNQ1, which is located at chromosome 11p15.5 and near a candidate region at 11p13-p12 and mainly encodes a protein for a voltage-gated potassium channel required for the repolarization phase of the cardiac action potential, has been proved to be associated with type 2 diabetes mellitus (T2DM). Studies done by different groups show that some common single nucleotide polymorphisms (SNPs) in KCNQ1, acting as T2DM susceptibility genes, exist in different ancestral groups including in the Asian populations of the Japanese, Korean, and Chinese in Hong Kong and Shanghai [1–5]. Among these are the 4 common SNPs rs2237892, rs2237895, rs2237897, and rs2283228 that were well replicated. However, controversies still exist in which these SNPs in KCNQ1 are not implicated as T2DM susceptibility genes in individuals of European descent [6, 7] or in a middle-aged population from East China [8].
Owing to the lack of consistent replication of these results in case-control studies in different study populations, it remains to be determined whether the results derived from Western societies are internationally applicable to East Asian races or specifically the Chinese Han population, or whether genetic background can cause different clinical phenotypes of the same disease as coronary artery disease (CAD) or T2DM.
Only recently have scholars demonstrated that the increased risk for T2DM linked to SNPs in KCNQ1 is likely to be caused by a reduction in insulin secretion, higher levels of fasting glucose or HbA1c [5, 9, 10], which implies that the KCNQ1 variants may play a major physiological role in the metabolism and dynamic balance of blood glucose. Furthermore, some other gene polymorphisms such as hepatocyte nuclear factor-1 homeobox A (HNF1A) gene polymorphisms [11], PPARgamma gene C161T polymorphism [12] and adiponectin receptor-2 gene variations [13] have also been proved to be connected with diabetes and cardiovascular disease.
Given that it is still unknown whether these 4 SNPs in KCNQ1 are associated with plasma lipid parameters besides their inconsistent association with T2DM [1–10], to fill this knowledge gap, we aimed to determine whether these 4 common SNPs at KCNQ1 loci would correlate with plasma lipid parameters in a middle-aged Chinese Han population living in East China. The results will help solve this apparent controversy and provide new evidence to elucidate the mechanism of KCNQ1 variants on the risk of T2DM and CAD.
Methods
Study population samples
The study population has been previously described [8]. Briefly, from January 2003 to August 2008, 398 patients undergoing coronary angiography (CAG) for chest discomfort or suspected CAD were enrolled in this study, including 180 patients (men age 32-54 years and women age 39-64 years) with documented premature CAD [14] and 218 subjects without coronary stenosis, acting as controls. CAD was defined as a significant coronary stenosis (≥ 50%) in at least one of the 3 main coronary arteries or their major branches (branch diameter ≥ 2 mm) assessed by CAG or having experienced a myocardial infarction (MI) defined according to World Health Organization criteria. All patients with type 1 diabetes mellitus, congenital heart disease, syndrome X, severe liver or kidney disease, or noncoronary artery thrombotic disease were excluded from this study. The study was approved by the Medical Ethics Committee of the Affiliated ZhongDa Hospital of Southeast University. Before enrollment, the trial information was explained carefully to each patient, and subsequently written informed consent was obtained from all participants.
Coronary angiography
All participants underwent CAG during hospitalization. The grade of the coronary stenosis and CAD diagnosis were judged by 2 cardiologists unaware of this study.
Determination of parameters and risk factors
At the time of enrollment, background data, such as sex, age, height, body weight, and risk factors including hypertension, T2DM, family history of CAD, and smoking status were collected from each subject. Anthropometric measurements and blood pressure determination were performed according to standard protocols. Blood was collected and plasma concentrations of total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) were analyzed as previously described [15]. Levels of apolipoprotein A1 (apo A1), apolipoprotein B (apo B), fasting blood sugar (FBS), and insulin were determined by standard biochemical methods using a chemistry analyzer (Beckman Coulter Synchron clinical system LX20). Insulin resistance was calculated from fasting insulin and glucose by using the homeostasis model assessment method [16].
Determination of hypertension, T2DM, family history of CAD, and smoking status has been previously described [8]. Body weight and height were measured with individuals wearing light clothing, and body mass index (BMI) is expressed as weight in kilograms divided by the square of the height in meters.
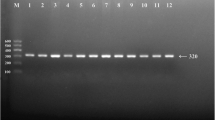
DNA extraction and genotyping
Genomic DNA extraction and genotyping of 4 SNPs in intron 15 of KCNQ1 have been described previously [8]. Genotype distributions obeyed the Hardy-Weinberg equilibrium (P > 0.05).
Statistical analyses
Statistical analyses were conducted using SPSS 15.0 software. Continuous data are expressed as mean ± SD, and categorical variables are expressed as frequencies. Analyses of continuous data and categorical variables among 3 different groups according to the genotypes of these 4 SNPs at KCNQ1 were determined by one-way ANOVA or chi-square test. Two-tailed P- values < 0.05 were considered as significant.
Results
Analysis of baseline characteristics in patients among 3 different genotypic groups (Table 1 and Table 2)
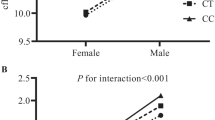
The 3 genotypes AA, AC, and CC are in rs2283228 and rs2237895, and the 3 genotypes CC, CT, and TT are in rs2237897 and rs2237892. When all study subjects were divided into 3 groups as the AA, AC, and CC group in rs2283228 and rs2237895, or the CC, CT, and TT group in rs2237897 and rs2237892, we found that 3 groups were well matched for mean age and gender composition. Subjects with the CC genotype in rs2283228 and TT genotype in rs2237892 had significantly higher levels of TG compared with the other 2 groups (P < 0.05), but this was not the case in subjects with the CC genotype in rs2237895 or TT genotype in rs2237897 (data not shown).
Overall in the study population, no significant differences were detected in the prevalences of hypertension, T2DM, family history of CAD, smoking, and average values of BMI, FBS, insulin, TC, LDL-C, and homeostasis model assessment of insulin resistance (HOMA-IR) among 3 groups according to 3 different genotypes at 4 SNPs in KCNQ1 (all P > 0.05).
Despite the lack of association between genotypes and TC, LDL-C, and apo B, concentrations of HDL-C and apo A1 in the CC group in rs2283228 were lower at the borderline significance level compared with the other 2 groups (P = 0.052 and 0.055, respectively). No other associations were detected between concentrations of HDL-C, apo A1, and apo B and SNPs at rs2237892, rs2237895, or rs2237897 (all P > 0.05).
Discussion
In the present study, for the first time, we report a strong association between rs2283228 and rs2237892 in KCNQ1 and lipid metabolism in a middle-aged Chinese Han population, which adds new data to this study issue.
Better understanding and preventive strategies for the morbidity and mortality related to T2DM are compelling. Recently, some susceptibility genes for T2DM have been reported [1–4], and potential mechanisms have also been elucidated [5, 9, 10]. However, inconsistent results still exist [6–8], and other mechanisms could not be fully excluded.
In the study by Tan JT et al [9], a total of 3 734 participants (2 520 Chinese, 693 Malay, and 521 Asian Indians) living in Singapore were enrolled, among which 1 881 Chinese subjects with normal glucose tolerance served as controls, and the reference population had an age range from 18 to 69 years. In the study by Liu Y et al [5], there were more women in both T2DM cases (women, 1 127; men, 785) and controls (women, 1 406; men, 635) and higher average age [(63.9 ± 9.5) years vs. (58.1 ± 9.4) years] than in our study. For the present study, all participants were aged 32 to 64 years and were hospitalized for CAD screening, among which 14.3% of subjects were diagnosed with T2DM, 180 subjects (45.2%) had CAD, and 218 subjects (54.8%) were non-CAD controls [8]. Young CAD patients usually have a different profile of major coronary risk factors [17]. Obviously, the differences in enrollment criteria and population characteristics account for the discrepancies between these studies. Meanwhile, differences in genetic inheritance among the races, lifestyles, public health insurance, and a system of free access to hospitals might contribute to the available subjects enrolled in our study.
In the current study, subjects in 3 groups according to different genotypes at rs2283228, rs2237895, rs2237897, and rs2237892 were well matched for mean age and gender composition, and no significant differences were detected in the prevalences of hypertension, T2DM, family history of CAD, smoking and values of BMI, FBS, insulin, TC, LDL-C, and HOMA-IR.
More recently, emerging evidence supports TG as a risk factor for CAD [18, 19]. Patients with T2DM are more likely to have higher levels of TG and lower levels of HDL-C. Our study thus furthermore helps settle the issue of whether the variants in KCNQ1 are related to lipid metabolism. In the present study, we demonstrated that an association exists between CC genotype in rs2283228 and TT genotype in rs2237892 and higher levels of TG. Further fine mapping of SNPs in KCNQ1, especially within the LD block containing rs2283228 or rs2237892, may allow the eventual identification of the causal variant. Meanwhile, in the study by Giuffrida et al, though HNF1A I27L polymorphism did not differ significantly among late-onset autosomal dominant diabetes mellitus, classical T2DM and normoglycemic controls, it was found to be associated with risk of hypertriglyceridemia [11]. In patients with CAD combined with T2DM, P PARgamma C161 > T genotypes are associated with levels of TG and apo B but not glucose metabolism, with CC homozygote carriers having significantly higher levels of TG and apo B than those in T allele carriers [12]. Large prospective studies have identified HDL-C as a strong, independent, inverse predictor of risk of CAD [20, 21]. Patients with higher levels of HDL-C and CAD had a similar or lower prevalence of traditional CAD risk factors compared with patients with normal HDL-C levels and CAD [22]. In our study, subjects with CC genotype in rs2283228 had lower levels of HDL-C and apo A1.
Some limitations of the present study need to be acknowledged. First, our study population comprised only those who have been admitted to the hospital for CAD screening and diagnosis, so it's more representative of patients in a cardiac center and might not be representative of the general population. Additionally, our study sample is predominantly yellow; thus, the results may not be generalizable to other ethnic groups in which disparities in population composition, geographical, and ethnic backgrounds may exist. It is well known that significant differences exist in the frequencies of some genetic variations among different ethnic groups and geographical regions. The fact is that these novel observations have not been previously found in other ethnic groups.
Conclusion
Our novel findings that the risk alleles of rs2283228 and rs2237892 within the KCNQ1 gene are associated with levels of TG, HDL-C and apo A1 in a middle-aged Chinese Han population are encouraging. Though the causal effects of four common SNPs (rs2237892, rs2237895, rs2237897, and rs2283228) in KCNQ1 on T2DM are controversial, our present study, for the first time, provide new evidence that these variants have an effect on lipid metabolism. Further studies are needed to firmly replicate these promising findings in other populations and to fully delineate the role of KCNQ1 and its related pathways in the pathogenesis of T2DM and CAD.
Author information
1Department of Cardiology, the Affiliated ZhongDa Hospital and Institute of Cardiovascular Disease of Southeast University, NO.87 Dingjiaqiao, Nanjing 210009, P.R.China
2Department of Cardiology, the Affiliated Jiangyin Hospital of Southeast University, Jiangyin 214400, P.R.China
Abbreviations
- Apo A1:
-
apolipoprotein A1
- Apo B:
-
apolipoprotein B
- BMI:
-
body mass index
- CAD:
-
coronary artery disease
- CAG:
-
coronary angiography
- FBS:
-
fasting blood sugar
- HDL-C:
-
high-density lipoprotein cholesterol
- HNF1A:
-
hepatocyte nuclear factor-1 homeobox A
- HOMA-IR:
-
homeostasis model assessment-insulin resistance
- LDL-C:
-
low-density lipoprotein cholesterol
- SNPs:
-
single nucleotide polymorphisms
- TC:
-
total cholesterol
- TG:
-
triglyceride
- T2DM:
-
type 2 diabetes mellitus.
References
Mori Y, Otabe S, Dina C, Yasuda K, Populaire C, Lecoeur C, Vatin V, Durand E, Hara K, Okada T, Tobe K, Boutin P, Kadowaki T, Froguel P: Genome-wide search for type 2 diabetes in Japanese affected sib-pairs confirms susceptibility genes on 3q, 15q, and 20q and identifies two new candidate loci on 7p and 11p. Diabetes. 2002, 51: 1247-1255. 10.2337/diabetes.51.4.1247.
Nawata H, Shirasawa S, Nakashima N, Araki E, Hashiguchi J, Miyake S, Yamauchi T, Hamaguchi K, Yoshimatsu H, Takeda H, Fukushima H, Sasahara T, Yamaguchi K, Sonoda N, Sonoda T, Matsumoto M, Tanaka Y, Sugimoto H, Tsubouchi H, Inoguchi T, Yanase T, Wake N, Narazaki K, Eto T, Umeda F, Nakazaki M, Ono J, Asano T, Ito Y, Akazawa S: Genome-wide linkage analysis of type 2 diabetes mellitus reconfirms the susceptibility locus on 11p13-p12 in Japanese. J Hum Genet. 2004, 49: 629-634. 10.1007/s10038-004-0199-3.
Unoki H, Takahashi A, Kawaguchi T, Hara K, Horikoshi M, Andersen G, Ng DP, Holmkvist J, Borch-Johnsen K, Jørgensen T, Sandbaek A, Lauritzen T, Hansen T, Nurbaya S, Tsunoda T, Kubo M, Babazono T, Hirose H, Hayashi M, Iwamoto Y, Kashiwagi A, Kaku K, Kawamori R, Tai ES, Pedersen O, Kamatani N, Kadowaki T, Kikkawa R, Nakamura Y, Maeda S: SNPs in KCNQ1 are associated with susceptibility to type 2 diabetes in East Asian and European populations. Nat Genet. 2008, 40: 1098-1102. 10.1038/ng.208.
Yasuda K, Miyake K, Horikawa Y, Hara K, Osawa H, Furuta H, Hirota Y, Mori H, Jonsson A, Sato Y, Yamagata K, Hinokio Y, Wang HY, Tanahashi T, Nakamura N, Oka Y, Iwasaki N, Iwamoto Y, Yamada Y, Seino Y, Maegawa H, Kashiwagi A, Takeda J, Maeda E, Shin HD, Cho YM, Park KS, Lee HK, Ng MC, Ma RC: Variants in KCNQ1 are associated with susceptibility to type 2 diabetes mellitus. Nat Genet. 2008, 40: 1092-1097. 10.1038/ng.207.
Liu Y, Zhou DZ, Zhang D, Chen Z, Zhao T, Zhang Z, Ning M, Hu X, Yang YF, Zhang ZF, Yu L, He L, Xu H: Variants in KCNQ1 are associated with susceptibility to type 2 diabetes in the population of mainland China. Diabetologia. 2009, 52: 1315-1321. 10.1007/s00125-009-1375-y.
Diabetes Genetics Initiative of Broad Institute of Harvard and MIT Lund University, and Novartis Institutes of BioMedical Research, Saxena R, Voight BF, Lyssenko V, Burtt NP, de Bakker PI, Chen H, Roix JJ, Kathiresan S, Hirschhorn JN, Daly MJ, Hughes TE, Groop L, Altshuler D, Almgren P, Florez JC, Meyer J, Ardlie K, Bengtsson Boström K, Isomaa B, Lettre G, Lindblad U, Lyon HN, Melander O, Newton-Cheh C, Nilsson P, Orho-Melander M, Råstam L, Speliotes EK, Taskinen MR, Tuomi T: Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science. 2007, 316: 1331-1336. 10.1126/science.1142358.
Zeggini E, Weedon MN, Lindgren CM, Frayling TM, Elliott KS, Lango H, Timpson NJ, Perry JR, Rayner NW, Freathy RM, Barrett JC, Shields B, Morris AP, Ellard S, Groves CJ, Harries LW, Marchini JL, Owen KR, Knight B, Cardon LR, Walker M, Hitman GA, Morris AD, Doney AS, Wellcome Trust Case Control Consortium (WTCCC), McCarthy MI, Hattersley AT: Replication of genome-wide association signals in U.K. samples reveals risk loci for type 2 diabetes. Science. 2007, 316: 1336-1341. 10.1126/science.1142364.
Chen Z, Zhang X, Ma G, Qian Q, Yao Y: Association study of four variants in KCNQ1 with type 2 diabetes mellitus and premature coronary artery disease in a Chinese population. Mol Biol Rep. 2010, 37: 207-212. 10.1007/s11033-009-9597-0.
Tan JT, Nurbaya S, Gardner D, Ye S, Tai ES, Ng DP: Genetic variation in KCNQ1 associates with fasting glucose and beta-cell function: a study of 3,734 subjects comprising three ethnicities living in Singapore. Diabetes. 2009, 58: 1445-1449. 10.2337/db08-1138.
Hu C, Wang C, Zhang R, Ma X, Wang J, Lu J, Qin W, Bao Y, Xiang K, Jia W: Variations in KCNQ1 are associated with type 2 diabetes and beta cell function in a Chinese population. Diabetologia. 2009, 52: 1322-1325. 10.1007/s00125-009-1335-6.
Giuffrida FM, Furuzawa GK, Kasamatsu TS, Oliveira MM, Reis AF, Dib SA: HNF1A gene polymorphisms and cardiovascular risk factors in individuals with late-onset autosomal dominant diabetes: a cross-sectional study. Cardiovasc Diabetol. 2009, 8: 28-10.1186/1475-2840-8-28.
Wan J, Xiong S, Chao S, Xiao J, Ma Y, Wang J, Roy S: PPARgamma gene C161T substitution alters lipid profile in Chinese patients with coronary artery disease and type 2 diabetes mellitus. Cardiovasc Diabetol. 2010, 9: 13-10.1186/1475-2840-9-13.
Halvatsiotis I, Tsiotra PC, Ikonomidis I, Kollias A, Mitrou P, Maratou E, Boutati E, Lekakis J, Dimitriadis G, Economopoulos T, Kremastinos DT, Raptis SA: Genetic variation in the adiponectin receptor 2 (ADIPOR2) gene is associated with coronary artery disease and increased ADIPOR2 expression in peripheral monocytes. Cardiovasc Diabetol. 2010, 9: 10-10.1186/1475-2840-9-10.
Kareinen A, Viitanen L, Halonen P, Lehto S, Laakso M: Cardiovascular risk factors associated with insulin resistance cluster in families with early-onset coronary artery disease. Arterioscler Thromb Vasc Biol. 2001, 21: 1346-1352. 10.1161/hq0801.093655.
Chen Z, Ma G, Zhang X, Wang J: Lipoprotein lipase and premature coronary artery disease. Acta Cardiol. 2009, 64: 379-383. 10.2143/AC.64.3.2038025.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC: Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985, 28: 412-419. 10.1007/BF00280883.
Yasar AS, Turhan H, Basar N, Metin F, Erbay AR, Ilkay E, Sabah I: Comparison of major coronary risk factors in female and male patients with premature coronary artery disease. Acta Cardiol. 2008, 63: 19-25. 10.2143/AC.63.1.2025327.
Hopkins PN, Wu LL, Hunt SC, Brinton EA: Plasma triglycerides and type III hyperlipidemia are independently associated with premature familial coronary artery disease. J Am Coll Cardiol. 2005, 45: 1003-1012. 10.1016/j.jacc.2004.11.062.
Chen CY, Hwu CM, Lin MW, Tsai CH, Yeh HI: High triglyceride level is associated with severe coronary artery disease in hypertensive subjects. Scand Cardiovasc J. 2008, 42: 146-152. 10.1080/14017430701840325.
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR: High density lipoprotein as a protective factor against coronary heart disease: the Framingham study. Am J Med. 1977, 62: 707-714. 10.1016/0002-9343(77)90874-9.
Assmann G, Schulte H, von Eckardstein A, Huang Y: High-density lipoprotein cholesterol as a predictor of coronary heart disease risk: the PROCAM experience and pathophysiological implications for reverse cholesterol transport. Atherosclerosis. 1996, 124 (suppl): S11-20. 10.1016/0021-9150(96)05852-2.
DeFaria Yeh D, Freeman MW, Meigs JB, Grant RW: Risk factors for coronary artery disease in patients with elevated high-density lipoprotein cholesterol. Am J Cardiol. 2007, 99: 1-4. 10.1016/j.amjcard.2006.07.053.
Acknowledgements
We are grateful to Xiaoli Zhang and Jiahong Wang for their efforts on data collection.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
ZC conceived the study, designed and performed the study experiments, analyzed the data and interpreted the results and wrote the manuscript. QZY, GSM and QQ interpreted the results, participated in the writing of the manuscript. All authors read and approved the final manuscript.
Zhong Chen, Quanzhong Yin contributed equally to this work.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Chen, Z., Yin, Q., Ma, G. et al. KCNQ1 gene polymorphisms are associated with lipid parameters in a Chinese Han population. Cardiovasc Diabetol 9, 35 (2010). https://doi.org/10.1186/1475-2840-9-35
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2840-9-35