Abstract
Background
An impairment of cardiovascular function in streptozotocin (STZ)-diabetic rats has been mentioned within 5 days-to-3 months of induction. ATP-sensitive potassium (KATP) channels are expressed on cardiac sarcolemmal membranes. It is highly responsive to metabolic fluctuations and can have effects on cardiac contractility. The present study attempted to clarify the changes of cardiac KATP channels in diabetic disorders.
Methods
Streptozotocin-induced diabetic rats and neonatal rat cardiomyocytes treated with a high concentration of glucose (a D-glucose concentration of 30 mM was used and cells were cultured for 24 hr) were used to examine the effect of hyperglycemia on cardiac function and the expression of KATP channels. KATP channels expression was found to be linked to cardiac tonic dysfunction, and we evaluated the expression levels of KATP channels by Western blot and Northern blot analysis.
Results
The result shows diazoxide produced a marked reduction of heart rate in control group. Furthermore, the methods of Northern blotting and Western blotting were employed to identify the gene expression of KATP channel. Two subunits of cardiac KATP channel (SUR2A and kir 6.2) were purchased as indicators and showed significantly decreased in both diabetic rats and high glucose treated rat cardiac myocytes. Correction of hyperglycemia by insulin or phlorizin restored the gene expression of cardiac KATP in these diabetic rats.
Conclusions
Both mRNA and protein expression of cardiac KATP channels are decreased in diabetic rats induced by STZ for 8 weeks. This phenomenon leads to result in desensitization of some KATP channel drugs.
Similar content being viewed by others
Background
Diabetes is a disease characterized by chronic hyperglycemia secondary to a reduction in the functional efficacy and/or a deficiency of insulin. In fact, patients with diabetes have a shorter life span and a lesser quality of life, mainly as a result of macrovascular and/or microvascular complications[1]. An impairment of cardiovascular function in streptozotocin (STZ)-diabetic rats has been mentioned within 5 days-to-3 months of induction [2].
ATP-sensitive potassium (KATP) channels are expressed on cardiac sarcolemmal membranes, and can have effects on cardiac repolarization and contraction during physiological and pathophysiological conditions [3–5]. Sarcolemmal KATP channels are composed of a pore-forming subunit (kir6.1 or kir6.2) and a sulfonylurea receptor (SUR1, SUR2A or SUR2B) [6]. Activation of KATP channels plays an important role of cardio-protection during myocardial ischemia and hypoxia [7–9].
In the cardiac muscular cells, KATP channel gating is highly responsive to metabolic fluctuations in the channel microenvironment[10]; the KATP could act as sensor of cell energy metabolism. KATP channel senses signals of cell energy metabolism in two ways. One is direct interactions between KATP and cell metabolites, which will produce immediate and temporal effects on channel activities[11]; the other is regulation of KATP genes expression by energy metabolism, this way can induce a delayed but much profound effect on channel quantity[12].
Cell energy metabolism regulates KATP genes expression; alternations in the metabolism will lead to changes of the KATP channel number[12]. High glucose leads to a marked decrease of kir6.2 mRNA level in isolated rat pancreatic islets as well as in the INS-1 beta cell line. This effect is reversed by exposure to low glucose[13]. Taken into together, investigation on the gene expression of cardiac KATP might clarify the cardiac dysfunction during diabetes development.
In order to demonstrate the changes of cardiac KATP channels in diabetic disorders, the present study employed the whole heart of diabetic rats induced by STZ injection for 8 weeks and neonatal rat cardiomyocytes. The alterations of cardiac KATP channels in the protein and mRNA levels were employed as indicators.
Methods
Animals
Three-month-old male Wistar rats were housed in a temperature controlled room (25°C) with a 12-h dark and 12-h light cycle. Food and water were available at its pleasure. Diabetic rats were prepared by giving an intravenous (IV) injection of 60 mg/kg streptozotocin (STZ) (Sigma-Aldrich, Inc., Saint Louis, Missouri, USA), into the fasting rats. Animals were considered to be diabetic if they had plasma glucose concentrations of 20 mmol/l or greater in addition to polyuria and other diabetic features. All studies were carried out 2 weeks after the injection of STZ. The concentration of plasma glucose was measured by the glucose oxidase method using an analyzer (Quik-Lab, Ames, Miles Inc., Elkhart, Indiana, USA). The animal experiment was approved and conducted in accordance with local institutional guidelines for the care and use of laboratory animals in the Chi-Mei Medical Center (No. 100052307) and conformed with the Guide for the Care and Use of Laboratory Animals (Kilkenny C et al. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol 2010, Jun 29;8(6):e1000412), as well as the guidelines of the Animal Welfare Act.
Cell cultures
Primary cultures of neonatal rat cardiomyocytes were prepared by modification of a previously described method [14]. Briefly, under anaesthesia with pentobarbital (30 mg/Kg), the heart tissue from a 1- to 2-day-old Wistar rat was excised then cut into 1-2 mm pieces and predigested with trypsin to remove red blood cells. The heart tissue was then digested with 0.25% trypsin and 0.05% collagenase. The dissociated cells were placed in uncoated 100 mm dishes and incubated at 37°C in a 5% CO2 incubator for at least 1 h to remove the non-myocytic cells. This procedure caused fibroblasts to predominantly attach to the dishes while most of the cardiomyocytes remained unattached. The population of cells enriched in cardiomyocytes was collected and counted. The cells were cultured in Dulbecco/Vogt modified Eagle's minimal essential medium (DMEM) with 1 mmol/L pyruvate, 10% foetal bovine serum (FBS), 100 units/mL penicillin, and 100 units/mL streptomycin. Using this protocol, > 95% of the cells were deemed cardiomyocytes as judged by sarcomeric myosin content. On the second day after plating, medium was replaced. Three to 4 days after plating, the cells were exposed to hyperglycaemic conditions. The high glucose-treated cardiomyocytes were generated by treating the cells with 30 mmol/L glucose for 24 h [15]. This animal experiment was also approved and conducted in accordance with local institutional guidelines for the care and use of laboratory animals in the Chi-Mei Medical Center (No. 100052307) and followed the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996), as well as the guidelines of the Animal Welfare Act.
Blood pressure measurement
The systolic blood pressure (SBP) was monitored in rats with diabetes 8 weeks after induction. The blood pressure measurements in age-matched normal rats were designated as controls. The blood pressure of the tail artery was measured non-invasively with a photoelectric volume oscillometer (UR-5000, Ueda, Japan) by placing the tail cuff device around the tail of the rat. The measurements for SBP were recorded in quadruplicate for each rat and the average blood pressure was calculated.
The effect of diazoxide (DZ) on heart rate on diabetic rats 8 weeks after induction
DZ (Sigma-Aldrich, Inc.), the well-known opener of KATP channels[16], was iv injected at 0.5, 1, 2 mg/kg for diabetic rats and 3, 5, 8 mg/kg for normal rats. The changes in heart rates were recorded at 5 minutes interval for 30 minutes.
The effects of insulin and phlorizin on diabetic rats 8 weeks after induction
Normalization of hyperglycemia was achieved per a previous protocol [17] in rats with diabetes for 8 weeks, using treatment either with 1 mg/kg of phlorizin dehydrate (Fluka Chemie, Buchs, Switzerland) or 0.5 IU of insulin (Novo Nordisk, Bagsvaerd, Denmark) by ip injection every 8 h for 4 days. Fluctuations in blood glucose levels were not observed in rats during repeated injections of insulin or phlorizin. Upon completion of treatment, the rats were sacrificed and their hearts were immediately removed, frozen in liquid nitrogen, and stored at -70°C until analysis was performed. The SUR-2A and Kir6.2 protein and mRNA concentrations in the heart tissue were measured by Western immunoblotting and Northern blotting, respectively. Blood samples were also collected from the femoral vein of the rats prior to sacrifice to estimate alterations in plasma glucose.
Preparation of heart membrane fraction
The preparation of membrane fraction from whole heart was performed on ice. The isolated heart tissue was lysed in 10 ml of pH 7.4 Tris/EDTA buffer at 4°C and homogenized for 15 s. The membrane fraction was obtained by centrifugation at 20,000 g for 15 min.
Measurement of KATP channel protein
After homogenization, the protein content was determined by BioRad protein dye binding assay (Bio-Rad Laboratories, Richmond, CA, USA). Protein samples (9 μg) were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (10% acrylamide gel) using Bio-Rad Mini-Protein II system (Laemmli 1970). The separated proteins were blotted onto nitrocellulose. After treating with SUR-2A and Kir6.2 antibody (Affinity Bioreagents, Inc., Colorado, USA). Immunostaining was performed for peroxidase activity by incubation in Tris-buffer (10 mmol/l). The intensity of the blot incubated with goat polyclonal antibody (1:1000) to bind actin (Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA) was used to ensure that the amount of protein loaded into each lane of the gel was constant. Autoradiography was developed using an enhanced chemiluminescence development system (Amersham International, Buckinghamshire, UK). The resulting immunoblots were quantified by a scanning densitometer (Hoefer, San Francisco, CA, USA).
Measurement of KATP channel mRNA
Total RNA was extracted from heart using Ultraspec™-II RNA extraction system (Bioteck, Houston, TX, USA) as indication of the manufacturer. RNA (20 μg) was denatured and aliquots of total RNA were then size-fractionated in a 1.2% agarose/formaldehyde gel. The RNA was transferred to a Hybond-N membrane (Amersham International). SUR-2A and Kir6.2 mRNA levels were detected using prime-labeled full-length cDNA under stringent hybridization conditions [18]. Intensity of the mRNA blot was quantified by scanning densitometry (Hoefer, San Francisco, CA, USA). The response of β-actin was used as internal standard.
Statistical analysis
Statistical analysis was carried out using ANOVA analysis and Newman-Keuls post-hoc analysis. Statistical significance was set as p < 0.05. Results were expressed as mean ± SE of each group from various samples (n).
Results
Changes of plasma glucose and systolic blood pressure in rats with diabetes for 8 weeks
The fasting plasma glucose levels of STZ-diabetic rats were significantly higher than those of untreated rats (Table 1). Additionally, the plasma insulin mean level in diabetic rats induced by STZ for 8 weeks was 13.4 ± 2.7 μU/ml (n = 8), markedly lower than the insulin level in control rats (58.3 ± 6.4 μU/ml; n = 8). Moreover, the plasma glucose levels in rats with diabetes for 8 weeks were markedly reversed by treatment with either insulin or phlorizin for 4 days, as compared to untreated diabetic rats (Table 1).
The SBP in diabetic rats induced by STZ for 8 weeks was significantly lower than that in age-matched normal rats. Injection of diabetic rats with 0.5 IU/kg insulin, three times daily for 4 days, restored the SBP to a level approaching normal control (Table 1). Similarly, treatment with phlorizin for 4 days elevated the SBP in rats with diabetes for 8 weeks to 118.4 ± 2.9 mmHg, which was not statistically different from the control rats (Table 1).
The body weight of STZ-diabetic rats was markedly less than that of normal control (Table 1). There was no difference in the body weight of diabetic rats between the vehicle- and insulin-treated groups throughout the 4-day study (Table 1). Also, phlorizin did not influence the body weight in STZ-diabetic rats throughout the 4-day treatment (Table 1).
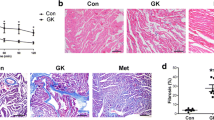
Effect of diazoxide (DZ) on the heart rate of rats
Figure 1 showed that DZ reduced the heart rates in both STZ-diabetic and control rats. Also, heart rate decreased in STZ-diabetic rats (11.8 ± 2.4%) by DZ at the low dose of 0.5 mg/kg was more pronounced than that (2.6 ± 1.2%) in normal rats responding to 3 mg/kg DZ.
Effects of K ATP channel opener, diazoxide (DZ), on the heart rates in STZ-diabetic rats with 8 weeks of diabetes (closed circles) and Wistar rats (open circles). Diabetic rats were iv injected with DZ at 0.5, 1 or 2 mg/kg. Wistar rats were received same treatment with DZ at 3, 5 or 8 mg/kg. The results are expressed as the mean ± SE obtained from each group of 7 animals. * P < 0.05 and ** P < 0.01 for comparisons of the post-injection heart rates with the pre-injection baseline heart rate (0) in each group.
Changes in mRNA levels of cardiac KATP channels in rats with diabetes for 8 weeks
The mRNA levels of cardiac SUR-2A and Kir6.2 were significantly decreased in diabetic rats that received STZ for 8 weeks as compared to the age-matched normal rats (Figure 2). This decrease in cardiac SUR-2A and Kir6.2 mRNA levels of rats with diabetes for 8 weeks was reversed after 4 days of insulin treatment to approximately the same level which existed in control rats. Treatment of these diabetic rats with 4 days of phlorizin also reversed the mRNA levels of SUR-2A and Kir6.2 in cardiac tissue to approximately 67% of the level compared with vehicle-treated diabetic rats (Figure 2).
Effects of insulin or phlorizin on the gene expression of cardiac K ATP channels in STZ-treated rats with 8 weeks of diabetes. The upper panel is the autoradiograph resulting from Northern blotting of the cardiac SUR-2A (A), Kir6.2 (B) mRNA or β-actin in hearts isolated from these diabetic rats treated with insulin (0.5 IU) or phlorizin (1 mg/kg) three times daily for 4 days. The vehicle used to dissolve the test medications was given in the same volume. Similar results were obtained with an additional 5 replications. Quantification of mRNA levels using SUR-2A or Kir6.2/β-actin, expressed as mean with SE (n = 6 per group) in each column, is indicated in the lower panel. * P < 0.05, ** P < 0.01 and *** P < 0.001 vs. control.
Changes in protein and mRNA levels of cardiac KATP channels in rats with diabetes for 8 weeks
The protein levels of cardiac SUR-2A and Kir6.2 in rats 8 weeks after STZ injection were markedly decreased to nearly 2-fold the levels in aged-matched controls (Figure 3). After 4 days of insulin injections, the cardiac SUR-2A and Kir6.2 protein levels in these diabetic rats were approximately 60% reversed than that in vehicle-treated diabetic rats (Figure 3). A marked recovery in the protein level of SUR-2A and Kir6.2 was also observed in the cardiac tissues of rats with diabetes for 8 weeks after a 4-day treatment of phlorizin, which was 64% of the level measured in the vehicle-treated diabetic rats (Figure 3).
Effects of insulin or phlorizin on the protein levels of cardiac K ATP channels in STZ-treated rats with 8 weeks of diabetes. Upper panel depicts the Western blot analysis of representative protein levels for SUR-2A or Kir6.2, actin in hearts isolated from these diabetic rats treated in same manner. Quantification of protein levels using SUR-2A or Kir6.2/actin, expressed as mean with SE (n = 6 per group) in each column, is indicated in the lower panel. * P < 0.05, ** P < 0.01 and *** P < 0.001 vs. control.
Decrease of KATP channels expression levels by glucose in neonatal rat cardiac myocytes
Effects of hyperglycemia on SUR-2A and Kir6.2 expression levels were further characterized by exposing cultured neonatal rat cardiac myocytes to various concentrations of glucose in vitro. The SUR-2A and Kir6.2 expression levels in neonatal rat cardiac myocytes were reduced in a concentration-dependent manner when cultured in media containing glucose after 24 hr incubation. The lack of change in SUR-2A and Kir6.2 expression levels in mannitol treated neonatal rat cardiac myocytes showed that protein expression levels were not affected by hyperosmolarity. Thus, we identified that expression levels of SUR-2A and Kir6.2 are decreased by high glucose in neonatal rat cardiac myocytes, similar to the changes observed in heart of diabetic rats (Figure 4).
Changes in expression of K ATP channels in neonatal rat cardiac myocytes after exposure to high concentrations of glucose. Cultured neonatal rat cardiac myocytes exposed to glucose at final concentrations of 10 mM, 20 mM and 30 mM were used to compare with the control, which was incubated with 5.5 mM glucose. Cells were also exposed to 24.5 mM mannitol to produce the same osmolarity (317 mOsmol/L) as that produced when using the highest concentration of glucose (30 mM). After 24 hours of incubation, cells were prepared for Western blot analysis. Quantification of protein levels using SUR-2A or Kir6.2 over β-actin indicated as means with SE (n = 4 per group) in each column are presented in the lower panel. *P < 0.05, **P < 0.001 compared to control.
Restored of K ATP channels expression levels in high-glucose treated neonatal rat cardiac myocytes by free radicals scavenger
Free radicals (ROS) are excessively produced in the pathogenesis of acute and diseases[19]. Present studies have demonstrated that cardiac dysfunction is caused by increasing of ROS production in hyperclycemic rats and high-glucose treated cardiac myocytes. To investigate the effect of hyperglycemia on SUR-2A and Kir6.2 expression, we treated neonatal rat cardiac myocytes with high concentrations of glucose (30 mmol/l; HG) in medium with and without 100 nmol of tiron, a superoxide anion scavenger[20] and after incubation we examined the effects on SUR-2A and Kir6.2 expression using western blot analysis (Figure 5). We observed that the decreased SUR-2A and Kir6.2 protein expressions in neonatal rat cardiac myocytes caused by high glucose concentrations were reversed by tiron treatment (Figure 5); these are consistent with our previous observations of SUR-2A and Kir6.2.
Effects of tiron on the protein levels of cardiac K ATP channels in high-glucose treated neonatal rat cardiac myocytes. Cultured neonatal rat cardiac myocytes exposed to glucose at final concentrations of 30 mM were used to compare with the control, which was incubated with 5.5 mM menitol. Cells were also exposed to 100 nM tiron as radical scavenger. After 24 hours of incubation, cells were prepared for Western blot analysis. Quantification of protein levels using SUR-2A or Kir6.2 over β-actin indicated as means with SE (n = 4 per group) in each column are presented in the lower panel. *P < 0.05, **P < 0.001 compared to control.
Discussion
Due to the difference between human and animal and/or the stage of diabetes, the response of blood pressure is varied; changes of blood pressure in diabetic complications seem not so simple. Numerous evidences suggest that diabetic heart is characterized by compromised ventricular contraction and prolonged relaxation attributable to multiple causative factors including calcium accumulation, oxidative stress and apoptosis. Previous study have demonstrated that blocking the calcium channel and oxidative stress could have advantage in diabetic heart [21]. Another study also showed that hyperglycemia can cause systolic dysfunction and a higher expression of cTnI in cardiomyocytes through ROS, enhancing MEK/ERK-induced GATA-4 phosphorylation and accumulation in the cell nucleus [22]. Although chronic diabetes is commonly linked to hypertension[23], hypotension has been ubiquitously described in early stage of diabetes[24, 25]. In the present study, cardiac dysfunction as evidenced by bradycardia and hypotension has been observed early in the course of diabetic rats receiving STZ for 8 weeks. Similar cardiac pathology in spontaneously diabetic Bio-Breeding rats has also been reported; specifically, the heart rate and heart rate variability were significantly lower than the control rats [26].
We showed that the mRNA level of cardiac KATP channels in rats with diabetes for 8 weeks duration was markedly lower than in non-diabetic rats. Also, changes in the protein level of cardiac KATP channels were associated with steady-state levels of mRNA encoding this receptor. A decrease of cardiac KATP gene expression was observed during the early stage of type-1 like diabetes. It is well known that the most prominent role of KATP channels in cardiovascular system is that opening of this channel can protect cardiac myocytes against ischemic injuries [27]. Actually, the effect of diazoxide (DZ) through opening of KATP channels was also decreased in rats with diabetes for 8 weeks duration. Therefore, decreased expression of cardiac KATP channel is one of the mechanisms accounting for cardiac dysfunction in the early stage of diabetes.
Several mechanisms have been proposed to explain the pathogenesis of diabetic complications, and hyperglycemia is always implicated [28]. Abnormal sympathetic nervous system and β-adrenoceptor (β-AR) signaling is associated with diabetes. β-AR have been found reduced the expression under Hyperglycemia [29]. In an attempt to know the role of hyperglycemia and/or hypoinsulinemia in the changes of cardiac KATP channels in insulin-deficient diabetic rats, exogenous insulin was administrated for 4 days into the diabetic rats, 8 weeks following induction with STZ. We found that insulin treatment of diabetic rats reversed the blood pressure reduction. In addition, normalization of plasma glucose level with insulin had a tendency to reverse the lower expression of cardiac KATP channels in 8 weeks diabetic rats. Phlorizin is an inhibitor of the renal tubular reabsorption of glucose and it has been widely used to distinguish the role of hyperglycemia in STZ-diabetic rats [30]. The reductions in blood pressure as well as the lowerer gene expression of cardiac KATP in these diabetic rats were also reversed by the reduction of hyperglycemia from phlorizin injection. Therefore, hyperglycemia is related to the down-regulation of cardiac KATP channels during the early stage of diabetes. In the present study, similar changes of KATP channels were observed on the whole heart of experimental diabetes, instead of limiting to atria or ventricles. Hyperglycemia could be considered a key in cardiac alteration that was associated with the decrease in cardiac KATP channels gene expression, leading to result in hypotension observed in 8 weeks type-1 diabetic rats.
We also demonstrated that expression levels of SUR-2A and Kir6.2 are decreased by high glucose in neonatal rat cardiac myocytes, similar to the changes observed in heart of diabetic rats. Furthermore, in cultured neonatal rat cardiac myocytes, the reduced expressions of SUR-2A and Kir6.2 caused by high concentrations of glucose were also reversed by the antioxidant tiron.
Clinically, heart disease is one of the major causes of death in diabetic patients, due in part to the accumulation of advanced glycation end products (AGE) resulting from chronic hyperglycemia [31]. AGE is known to produce from various pathways such as lipid peroxidation or oxidative stress, in addition to the underlying glycemia and accumulation in blood and tissues at an extremely accelerated rate, which is correlated with the time course of diabetes [32]. It has been suggested that suitable glycemic control in patients with diabetes for 8 years does not lead to an effective reduction in AGE levels, illustrating the negative correlation between hyperglycemia and the advanced diabetic complications that occur in chronic diabetes[32]. It appears that hyperglycemia may decrease cardiac KATP channels gene expression to account for the changes of cardiovascular function during the early stage of diabetes [28]. Thus, more studies are necessary to clarify the detailed mechanism(s) in the near future. The current study supports the recommendations for glycemic control of diabetes at early stage to lower complications.
Conclusions
We have demonstrated that both mRNA and protein expression of cardiac KATP channels are decreased in diabetic rats induced by STZ for 8 weeks. This phenomenon leads to reduction of blood pressure. Correction of hyperglycemia by insulin or phlorizin restored the gene expression of cardiac KATP in these diabetic rats. These data suggest that an increase of plasma glucose may enhance cardiac KATP channels gene expression to result in cardiac dysfunction observed in diabetic rats.
Abbreviations
- KATP:
-
ATP-sensitive potassium channels
- HR:
-
heart rate
- STZ:
-
streptozotoxin
- CO:
-
cardiac output
- i.p.:
-
intraperitoneal
- HG:
-
high glucose
- PBS:
-
phosphate-buffered saline
- BSA:
-
bovine serum albumin
- RIPA:
-
radioimmunoprecipitation assay
- SDS-PAGE:
-
sodium dodecyl sulfate polyacry lamide gel electrophoresis
- SBP:
-
systolic blood pressure
- SD:
-
standard deviation
- SEM:
-
standard error of mean
- DZ:
-
Diazoxide
- SUR2A:
-
sulfonylurea receptors2A
- kir 6.2:
-
inward-rectifier potassium ion channels 6.2
- IV:
-
intravenous
- FBS:
-
foetal bovine serum
- ROS:
-
reactive oxygen species.
References
Sobel BE, Schneider DJ: Cardiovascular complications in diabetes mellitus. Curr Opin Pharmacol. 2005, 5: 143-148. 10.1016/j.coph.2005.01.002.
De Angelis K, Schaan BD, Maeda CY, Dall'Ago P, Wichi RB, Irigoyen MC: Cardiovascular control in experimental diabetes. Braz J Med Biol Res. 2002, 35: 1091-1100. 10.1590/S0100-879X2002000900010.
Noma A: ATP-regulated K+ channels in cardiac muscle. Nature. 1983, 305: 147-148. 10.1038/305147a0.
Wilde AA, Escande D, Schumacher CA, Thuringer D, Mestre M, Fiolet JW, Janse MJ: Potassium accumulation in the globally ischemic mammalian heart. A role for the ATP-sensitive potassium channel. Circ Res. 1990, 67: 835-843.
Zhang H, Flagg TP, Nichols CG: Cardiac sarcolemmal K(ATP) channels: Latest twists in a questing tale!. J Mol Cell Cardiol. 2010, 48: 71-75. 10.1016/j.yjmcc.2009.07.002.
Chan KW, Wheeler A, Csanady L: Sulfonylurea receptors type 1 and 2A randomly assemble to form heteromeric KATP channels of mixed subunit composition. J Gen Physiol. 2008, 131: 43-58.
Venkatesh N, Lamp ST, Weiss JN: Sulfonylureas, ATP-sensitive K+ channels, and cellular K+ loss during hypoxia, ischemia, and metabolic inhibition in mammalian ventricle. Circ Res. 1991, 69: 623-637.
Cole WC, McPherson CD, Sontag D: ATP-regulated K+ channels protect the myocardium against ischemia/reperfusion damage. Circ Res. 1991, 69: 571-581.
Lee TM, Lin MS, Chang NC: Effect of ATP-sensitive potassium channel agonists on ventricular remodeling in healed rat infarcts. J Am Coll Cardiol. 2008, 51: 1309-1318. 10.1016/j.jacc.2007.11.067.
O'Rourke B, Ramza BM, Marban E: Oscillations of membrane current and excitability driven by metabolic oscillations in heart cells. Science. 1994, 265: 962-966. 10.1126/science.8052856.
Philip-Couderc P, Tavares NI, Roatti A, Lerch R, Montessuit C, Baertschi AJ: Forkhead transcription factors coordinate expression of myocardial KATP channel subunits and energy metabolism. Circ Res. 2008, 102: e20-35. 10.1161/CIRCRESAHA.107.166744.
Santos RM, Barbosa RM, Antunes CM, Silva AM, Salgado AP, Abrunhosa AJ, Pereira FC, Seica RM, Rosario LM: Bursting electrical activity generated in the presence of KATP channel blockers. Pharmacology, sensitivity to intracellular pH and modulation by glucose metabolism. Adv Exp Med Biol. 1997, 426: 33-41.
Moritz W, Leech CA, Ferrer J, Habener JF: Regulated expression of adenosine triphosphate-sensitive potassium channel subunits in pancreatic beta-cells. Endocrinology. 2001, 142: 129-138. 10.1210/en.142.1.129.
Simpson P, McGrath A, Savion S: Myocyte hypertrophy in neonatal rat heart cultures and its regulation by serum and by catecholamines. Circ Res. 1982, 51: 787-801.
Kannel WB, Hjortland M, Castelli WP: Role of diabetes in congestive heart failure: the Framingham study. Am J Cardiol. 1974, 34: 29-34. 10.1016/0002-9149(74)90089-7.
Suzuki M, Saito T, Sato T, Tamagawa M, Miki T, Seino S, Nakaya H: Cardioprotective effect of diazoxide is mediated by activation of sarcolemmal but not mitochondrial ATP-sensitive potassium channels in mice. Circulation. 2003, 107: 682-685. 10.1161/01.CIR.0000055187.67365.81.
Liu IM, Tzeng TF, Tsai CC, Lai TY, Chang CT, Cheng JT: Increase in adenosine A1 receptor gene expression in the liver of streptozotocin-induced diabetic rats. Diabetes Metab Res Rev. 2003, 19: 209-215. 10.1002/dmrr.369.
Tong YC, Chin WT, Cheng JT: Alterations in urinary bladder M2-muscarinic receptor protein and mRNA in 2-week streptozotocin-induced diabetic rats. Neurosci Lett. 1999, 277: 173-176. 10.1016/S0304-3940(99)00871-X.
Iglesias-De La Cruz MC, Ruiz-Torres P, Alcami J, Diez-Marques L, Ortega-Velazquez R, Chen S, Rodriguez-Puyol M, Ziyadeh FN, Rodriguez-Puyol D: Hydrogen peroxide increases extracellular matrix mRNA through TGF-beta in human mesangial cells. Kidney Int. 2001, 59: 87-95. 10.1046/j.1523-1755.2001.00469.x.
Cheng JT, Huang CC, Liu IM, Tzeng TF, Chang CJ: Novel mechanism for plasma glucose-lowering action of metformin in streptozotocin-induced diabetic rats. Diabetes. 2006, 55: 819-825. 10.2337/diabetes.55.03.06.db05-0934.
Kain V, Kumar S, Sitasawad S: Azelnidipine prevents cardiac dysfunction in streptozotocin-diabetic rats by reducing intracellular calcium accumulation, oxidative stress and apoptosis. Cardiovasc Diabetol. 2011, 10: 97-10.1186/1475-2840-10-97.
Ku PM, Chen LJ, Liang JR, Cheng KC, Li YX, Cheng JT: Molecular role of GATA binding protein 4 (GATA-4) in hyperglycemia-induced reduction of cardiac contractility. Cardiovasc Diabetol. 2011, 10: 57-10.1186/1475-2840-10-57.
Eppens MC, Craig ME, Cusumano J, Hing S, Chan AK, Howard NJ, Silink M, Donaghue KC: Prevalence of diabetes complications in adolescents with type 2 compared with type 1 diabetes. Diabetes Care. 2006, 29: 1300-1306. 10.2337/dc05-2470.
Gando S, Hattori Y, Akaishi Y, Nishihira J, Kanno M: Impaired contractile response to beta adrenoceptor stimulation in diabetic rat hearts: alterations in beta adrenoceptors-G protein-adenylate cyclase system and phospholamban phosphorylation. J Pharmacol Exp Ther. 1997, 282: 475-484.
Maeda CY, Fernandes TG, Timm HB, Irigoyen MC: Autonomic dysfunction in short-term experimental diabetes. Hypertension. 1995, 26: 1100-1104.
Sanyal SN, Arita M, Ono K: Inhomogeneous derangement of cardiac autonomic nerve control in diabetic rats. Circ J. 2002, 66: 283-288. 10.1253/circj.66.283.
Gross GJ, Fryer RM: Sarcolemmal versus mitochondrial ATP-sensitive K+ channels and myocardial preconditioning. Circ Res. 1999, 84: 973-979.
Koya D: [Molecular understanding of adverse effects of hyperglycemia in diabetic nephropathy]. Nippon Jinzo Gakkai Shi. 2007, 49: 470-473.
Thackeray JT, Parsa-Nezhad M, Kenk M, Thorn SL, Kolajova M, Beanlands RS, DaSilva JN: Reduced CGP12177 binding to cardiac beta-adrenoceptors in hyperglycemic high-fat-diet-fed, streptozotocin-induced diabetic rats. Nucl Med Biol. 2011, 38: 1059-1066. 10.1016/j.nucmedbio.2011.04.002.
Bucking C, Wood CM: Renal regulation of plasma glucose in the freshwater rainbow trout. J Exp Biol. 2005, 208: 2731-2739. 10.1242/jeb.01668.
Cooper ME: Importance of advanced glycation end products in diabetes-associated cardiovascular and renal disease. Am J Hypertens. 2004, 17: 31S-38S. 10.1016/j.amjhyper.2004.08.021.
Mentink CJ, Kilhovd BK, Rondas-Colbers GJ, Torjesen PA, Wolffenbuttel BH: Time course of specific AGEs during optimised glycaemic control in type 2 diabetes. Neth J Med. 2006, 64: 10-16.
Acknowledgements
We appreciate Dr. Hsien-Hui Chung for kind help in the measurement of blood pressures and Miss Pei-Lin Chou for research assistance of experiment of blotting. The present study was supported by a grant (CMFHR9848) from Chi-Mei Medical Center, Tainan City, Taiwan in addition to a grant (NSC99-2628-B309-001-MY3) from the National Science Council of R.O.C.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
JTC, LJC and KCC carried out the molecular studies and drafted the manuscript. YZC and YXL were involved in the interpretation of the results. ZCC and JTC conceived the study and participated in its design, interpretation and coordination, and drafted and approved the manuscript. All authors have read and approved the final manuscript. Also, all authors contributed significantly to and are in agreement with the content of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Chen, ZC., Cheng, YZ., Chen, LJ. et al. Increase of ATP-sensitive potassium (KATP) channels in the heart of type-1 diabetic rats. Cardiovasc Diabetol 11, 8 (2012). https://doi.org/10.1186/1475-2840-11-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2840-11-8