Abstract
Background
Regionalization of adult critical care services may improve outcomes for critically ill patients. We sought to develop a framework for understanding clinician attitudes toward regionalization and potential barriers to developing a tiered, regionalized system of care in the United States.
Methods
We performed a qualitative study using semi-structured interviews of critical care stakeholders in the United States, including physicians, nurses and hospital administrators. Stakeholders were identified from a stratified-random sample of United States general medical and surgical hospitals. Key barriers and potential solutions were identified by performing content analysis of the interview transcriptions.
Results
We interviewed 30 stakeholders from 24 different hospitals, representing a broad range of hospital locations and sizes. Key barriers to regionalization included personal and economic strain on families, loss of autonomy on the part of referring physicians and hospitals, loss of revenue on the part of referring physicians and hospitals, the potential to worsen outcomes at small hospitals by limiting services, and the potential to overwhelm large hospitals. Improving communication between destination and source hospitals, provider education, instituting voluntary objective criteria to become a designated referral center, and mechanisms to feed back patients and revenue to source hospitals were identified as potential solutions to some of these barriers.
Conclusion
Regionalization efforts will be met with significant conceptual and structural barriers. These data provide a foundation for future research and can be used to inform policy decisions regarding the design and implementation of a regionalized system of critical care.
Similar content being viewed by others
Background
The presence of a trained critical care physician and a multidisciplinary care team is associated with improved patient outcomes in the intensive care unit (ICU) [1–3]. Given the ortage of ICU clinicians, however, only a small minority of ICUs in the United States are organized in this manner [4]. The situation is expected to worsen as the population ages and demand for critical care rises [5]. To address this crisis some have called for a regionalized approach to critical care [6–8]. Under a regionalized scenario, high-risk patients would be routinely transferred to large regional care centers according to standardized triage criteria. Supporting this idea are several studies demonstrating lower risk-adjusted mortality in high volume hospitals and ICUs, indicating that the resources and experience of large hospitals may contribute to improved outcomes [9–12]. Recent population-based data indicate that transferring patients to high volume hospitals may significantly impact mortality for critically ill patients [13].
In order to research, design and implement a regionalized system of care, the active participation of all stakeholders will be essential. While there has been much written in support of regionalization by academics and opinion leaders, no information exists about the perceptions of front line critical care providers and hospital administrators regarding regionalization of care. Assessing the opinions of key stakeholders is a necessary step in implementing this type of large-scale organizational change [14]. Accordingly, the purpose of this study was to assess provider attitudes toward regionalization of adult critical care. We sought to determine not only the barriers to regionalization, but also potential solutions to those barriers. Because so little is known about the challenges to regionalization, including who would organize and implement such a system, we elected to use semi-structured interviews from a range of potential stakeholders in United States hospitals.
Methods
Study design and subjects
We performed a qualitative study using open-ended, semi-structured telephone interviews with potential stakeholders in critical care regionalization [15]. The interviews occurred between February and May, 2007. Stakeholders of interest included ICU physicians, ICU nurse managers, emergency department physicians, emergency department nurse managers, and hospital administrators/medical directors. These were identified as individuals who either routinely coordinate care for critically ill patients or may be involved in triage decisions under a regionalized scenario.
We obtained a stratified random sample of all non-federal, general care hospitals in the United States from the 2004 American Hospital Association Annual Survey. Hospitals were stratified by region (Northeast, Southeast, Midwest, and West), hospital size (<100 beds, 100 – 399 beds, and ≥400 beds) and size of metropolitan statistical area (<100,000, 100,000 – 1 million, and >1 million persons). The sampling frame was designed to ensure that we interviewed individuals representing a broad range of potential roles in a tiered, regionalized system of care. To account for the fact that many stakeholders either could not be reached or would decline to participate, three hospitals were selected from each strata. If fewer than three hospitals existed within a strata, all hospitals in the strata were selected.
Interviews
The interview guide consisted of a series of open-ended questions about regionalization and a list of potential barriers and solutions. The guide was developed with input from local care-givers experienced in regional care delivery and focused on three domains: (a) knowledge of and attitudes toward regionalization, (b) barriers to regionalizing care, and (c) potential solutions to those barriers. In order to ensure the broadest possible range of responses and solicit important viewpoints on novel barriers and solutions as they were uncovered, the guide expanded and evolved over time as additional interviews were conducted.
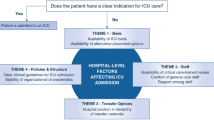
At the beginning of each interview we explicitly defined regionalization by making the following statement: "In a regionalized system, all US hospitals would be categorized into tiers according to the level of ICU acuity they can provide. The criteria for each tier would be set by a multidisciplinary panel and monitored by existing accreditation organizations. Selected patients in lower level ICUs would then be routinely transferred to higher level, regional care centers."
Each hospital was called in random order, and hospital operators were used to identify potential stakeholders. We did not fix the total number of interviews in the study a priori. Rather, we conducted interviews until one of two pre-specified conditions was met: (a) we interviewed at least one of all five stakeholders in each strata of the sampling frame, or (b) we reached thematic saturation (i.e. no new barriers or solutions obtained in ten consecutive interviews). All participants gave oral informed consent. This research was approved by the University of Pennsylvania Institutional Review Board.
Analysis
Interviews were recorded and transcribed. A framework for understanding regionalization was developed through directed content analysis of the interview responses [16]. Two investigators trained in qualitative data analysis (JMK, RJA) met regularly to identify key concepts and code the responses. Codes were tabulated, grouped into categories according to the developed framework, and reviewed with the other investigators [15]. Results are presented as a list of potential barriers and solutions, grouped by category, with representative quotes selected from the transcriptions used to illustrate each viewpoint [17].
Results
The final sample contained 104 hospitals. Thematic saturation was achieved after conducting 30 stakeholder interviews at 24 hospitals. Hospitals with a participating stakeholder varied in size and location (Table 1). We interviewed eight hospital administrators (27 percent), seven ICU nurse managers (23 percent), five emergency department nurse managers (17 percent), seven ICU physicians (23 percent), and three emergency department physicians (10 percent).
Respondents had diverse opinions on how regionalization would affect patient care. Some respondents felt that regionalization would have a small impact on patient outcomes. This view was expressed by stakeholders who thought that critical care in their area was already regionalized under an ad hoc system ("In our community we actually function that way – our center is the destination spot for anyone who becomes critically ill beyond a certain level."), or those at hospitals that already receive a large number of referral patients ("we already have a high volume and state-of-the-art facility"). Respondents who felt regionalization would improve quality generally noted the concentration of resources for critically ill patients at high volume centers (" [patients] would be in a facility that would be able to offer the care that they needed, so would imagine their outcomes would be better"). Respondents also noted the potential for adverse outcomes, either by restricting patient market freedoms ("I think it would remove choice and negatively impact patient care"), by overcrowding large centers ("What do we do in the ER with our ICU patients?"), by reducing services at small-volume hospitals ("we would lose all of our skills and capabilities"), or through the direct risks of inter-hospital transfer ("if you are transferring someone who is critically ill there's always a risk").
Respondents expressed the idea that regionalization could potentially be very costly, noting that it would create the added expense of routine inter-hospital transfer, and that large hospitals would see an increase in complex cases. Respondents also noted ways in which regionalization could reduce the cost of care through economies of scale. Regional referral centers, which are predominantly staffed by intensivists, might provide complex care more efficiently ("you will have a higher level of expertise"). Concentrating critical services might also reduce duplication of services and increase efficiency through economies of scale (" [regionalization could] lower cost by focusing complex care in places that do it regularly"). Many stakeholders expressed uncertainty in this area, citing the need for cost-effectiveness studies prior to instituting a regionalized system. A few stakeholders framed the issue of costs in terms of reimbursement and net revenue for hospitals, noting that the overall financial impact is dependent on payer mix ("It depends on what we send – if we send no-pay patients, they'll lose money and we'll do okay".)
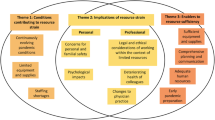
All respondents identified potential barriers to regionalization (Table 2). We categorized the reported barriers to regionalization into those concerning patients and families, clinicians, source hospitals, destination hospitals, and system design. Key concepts included financial and personal strain on families, lack of physician agreement to participate, the need for demonstrated effectiveness, and the possibility that regionalization would overwhelm the resources at destination hospitals. Respondents also noted the concern that regionalization could negatively impact resources and clinical skills at source hospitals, which may in turn lower the quality of care for patients left behind.
Potential solutions to these barriers were grouped into four domains: communication, education, system design, and reimbursement (Table 3). Key concepts included maintaining continuity of care, developing an evidence base, and educating clinicians. Some stakeholders conceived of a system where all the hospitals in a regional referral hospital shared a common information technology platform, which would facilitate communication and allow rapid transfer of health information between sites. Many stakeholders indicated that the criteria to become a regional referral center should be internal and voluntary – i.e., any hospital should have the potential to become a high level critical care center by meeting a set of objective criteria. Stakeholders also felt that a regionalized system should allow for some return of reimbursement and ultimately patient care to the source hospitals as a way to overcome losses of patients and revenue.
Discussion
This study demonstrates that front-line critical care stakeholders in the United States hold diverse opinions about the benefit of regionalization and potential barriers to implementing a regionalized system. Many stakeholders felt that regionalization had the potential to significantly improve outcomes for critically ill patients in small hospitals, while others expressed concerns that regionalization could negatively impact care for some patients. Costs, personal and family strain, loss of revenue and loss of autonomy were seen as important barriers to implementing a regionalized system. Potential solutions to these barriers included improving communication between hospitals, developing common information technology platforms, and revenue sharing between hospitals within a system.
The framework developed in this study provides an foundation for future research and development of a regionalized system of critical care. Formal regionalization of adult critical care in the United States has been under study since at least 1994, when a taskforce of the American College of Critical Care concluded that regionalizing critical care is likely to improve patient outcomes and called for more research in the area [6]. More recently, a position paper of the critical care professional societies highlighted regionalization as a potentially important way expand access to intensivist-led, multidisciplinary care [7]. This report led to the Prioritizing the Organization and Management of Intensive Care Services (PrOMIS) conference, a multi-disciplinary taskforce consisting of critical care practitioners, non-critical care clinicians, payer groups, government and regulatory agencies, and patients [8]. PrOMIS participants concluded that variation in the delivery of critical care results in avoidable mortality and morbidity, and directly called for the creation of a tiered, regionalized system of care in the United States. Ultimately, the PrOMIS conference will lead to continued discussions about the regionalization of critical care, however formal regionalization efforts on a national scale are not yet underway. Much health policy in the United States is formed by subtle government regulation of open market processes, and it is likely that regionalization will proceed in this manner as well.
The present study adds to the regionalization debate by providing the views of a broader constituency of clinicians and administrators. Whereas opinion-leaders and researchers appear to be very supportive of regionalization, there is no such consensus among providers on the ground.
Many stakeholders worried that regionalization could disrupt existing patient-clinician relationships, create undue personal and financial hardships on families, limit the ability of small hospitals to provide necessary acute care, reduce revenue to small hospitals, and burden large hospitals with excess case-load. Still, other stakeholders expressed the core concept in support of regionalization: the notion that concentrating limited resources in a few selected large hospitals could improve both quality and efficiency for patients with critical illness.
Stakeholders also identified several key unknowns that can define a research agenda to be addressed prior to implementation. Many were unwilling to consider implementing a regionalized system without additional investigations into the effectiveness of such a system. Data are also needed as to how regionalization would affect case-load at referral hospitals. Even at large hospitals, existing ICU staffing and infrastructure are limited [18–20]. It is possible that the number of patients transferred to large hospital would overload existing resources. Similarly, we do not know how regionalization would affect small hospitals, where there is concern that regionalization might reduce their ability to care for acutely ill patients. Critical care is tightly tied to other hospital services such as cardiac, cancer and neurological care [21–24]. If hospitals are asked to scale back critical care services, they might need to scale back these services as well, potentially resulting in significant revenue loss and loss of community access to care. Finally, stakeholders expressed concern about the personal and financial hardships patients and families might face in travel to regional centers.
Stakeholders also suggested ways to overcome the barriers they perceive. To overcome financial barriers, it might be possible to return revenue to source hospitals. To overcome concerns about loss of continuity, information systems could be used facilitate communication across care sites. To address concerns about hospital and physician autonomy, all hospitals could be invited to become regional referral centers based on pre-defined objective criteria. Although some very small hospitals might not plausibly be able to compete for participation, hospitals are much more likely to participate if every hospital is given the opportunity to fulfill the criteria to accept high acuity patients in transfer. Indeed, this type of participation scheme was integral to trauma system development [25].
We interviewed only critical care stakeholders in the United States – these results may not directly apply to other countries with different approaches to the organization and management of critical care [26]. Countries with single-payor health systems like Canada and the United Kingdom may experience unique challenges should they attempt to regionalize critical care. Unlike the United States, closed ICUs staffed by trained intensivists are extremely common. Although research demonstrates volume-outcome relationships exist in Europe just as in the United States, the potential benefits may be lessened in the setting of universal intensivist staffing [12].
Our study has several additional limitations. First, we did not interview all potential stakeholders, such as respiratory therapists, pharmacists, primary care physicians, surgeons, or representatives from payer groups and regulatory agencies. We did not interview surgeons because regionalization for high-risk surgery is currently being advocated separately from critical care [27]. Others were not interviewed because we wanted to interview only those individuals who would be directly involved in the triage of critically ill patients under a regionalized system. The goal of this study was to give voice to those immediate, but otherwise under-represented, stakeholders. Second, our study was limited to stakeholders' perceptions of the barriers to regionalization. This study design may not reveal some important types of barriers, for example, socioeconomic, racial or professional status barriers which may be less well perceived by stakeholders or may be less socially acceptable to reveal. Nonetheless, an understanding of the perceptions of key stakeholders is an essential first step toward implementing a major organizational change such as regionalization. Third, we performed only 30 interviews, creating the possibility that some viewpoints were missed. We stopped after 30 interviews because we reached thematic saturation – additional interviews would be very unlikely to solicit new viewpoints. Fourth, stakeholder opinions are likely to vary across different regions and health systems – efforts to design a regionalized system based upon this research should be customized for local health care environments. Finally, although we sought to identify opinions and barriers to regionalization, we did not seek to quantify their absolute or relative importance, or determine the differences in perception of regionalization across stakeholder groups. These analyses are better suited to quantitative research methods. Instead, we took advantage of qualitative methodology to solicit the broadest possible viewpoints on regionalization. Future work should be directed at a quantitative examination of the perceptions of critical care stakeholders using survey methodology based upon these findings [28].
Conclusion
Using open-ended interviews with key stakeholders, we have identified diverse opinions about the potential benefits of regionalization and the barriers to implementing a regionalized system. These results provide a roadmap for future research toward a more effective system of critical care.
References
Young MP, Birkmeyer JD: Potential reduction in mortality rates using an intensivist model to manage intensive care units. Eff Clin Pract. 2000, 3: 284-289.
Randolph AG, Pronovost P: Reorganizing the delivery of intensive care could improve efficiency and save lives. J Eval Clin Pract. 2002, 8: 1-8. 10.1046/j.1365-2753.2002.00321.x.
Durbin CG: Team model: advocating for the optimal method of care delivery in the intensive care unit. Crit Care Med. 2006, 34: S12-17. 10.1097/01.CCM.0000199985.72497.D1.
Angus DC, Shorr AF, White A, Dremsizov TT, Schmitz RJ, Kelley MA: Critical care delivery in the United States: Distribution of services and compliance with Leapfrog recommendations. Crit Care Med. 2006, 34: 1016-1024. 10.1097/01.CCM.0000206105.05626.15.
Angus DC, Kelley MA, Schmitz RJ, White A, Popovich J: Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population?. JAMA. 2000, 284: 2762-2770. 10.1001/jama.284.21.2762.
Thompson DR, Clemmer TP, Applefeld JJ, Crippen DW, Jastremski MS, Lucas CE, Pollack MM, Wedel SK: Regionalization of critical care medicine: task force report of the American College of Critical Care Medicine. Crit Care Med. 1994, 22: 1306-1313. 10.1097/00003246-199408000-00015.
Ewart GW, Marcus L, Gaba MM, Bradner RH, Medina JL, Chandler EB: The critical care medicine crisis: a call for federal action: a white paper from the critical care professional societies. Chest. 2004, 125: 1518-1521. 10.1378/chest.125.4.1518.
Barnato AE, Kahn JM, Rubenfeld GD, McCauley K, Fontaine D, Frassica JJ, Hubmayr R, Jacobi J, Brower RG, Chalfin D, et al: Prioritizing the organization and management of intensive care services in the United States: the PrOMIS Conference. Crit Care Med. 2007, 35: 1003-1011. 10.1097/01.CCM.0000259535.06205.B4.
Durairaj L, Torner JC, Chrischilles EA, Vaughan Sarrazin MS, Yankey J, Rosenthal GE: Hospital Volume-Outcome Relationships Among Medical Admissions to ICUs. Chest. 2005, 128: 1682-1689. 10.1378/chest.128.3.1682.
Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O'Brien CR, Rubenfeld GD: Hospital volume and the outcomes of mechanical ventilation. N Engl J Med. 2006, 355: 41-50. 10.1056/NEJMsa053993.
Glance LG, Li Y, Osler TM, Dick A, Mukamel DB: Impact of patient volume on the mortality rate of adult intensive care unit patients. Crit Care Med. 2006, 34: 1925-1934. 10.1097/01.CCM.0000226415.93237.84.
Peelen L, De Keizer NF, Peek N, Scheffer GJ, Voort Van der PH, De Jonge E: The influence of volume and ICU organization on hospital mortality in patients admitted with severe sepsis: a retrospective multicenter cohort study. Crit Care. 2007, 11: R40-10.1186/cc5727.
Kahn JM, Linde-Zwirble WT, Wunsch H, Barnato AE, Iwashyna TJ, Roberts MS, Lave JR, Angus DC: Potential value of regionalized intensive care for mechanically ventilated medical patients. Am J Respir Crit Care Med. 2007.
Connor PE, Lake LK, Stackman RW: Managing organizational change. 2003, Westport, CT: Prager Paperback, 3
Russell BH: Social research methods : qualitative and quantitative approaches. 2000, Thousand Oaks: Sage Publications
Hsieh HF, Shannon SE: Three approaches to qualitative content analysis. Qual Health Res. 2005, 15: 1277-1288. 10.1177/1049732305276687.
Kvale S: Interviews : an introduction to qualitative research interviewing. 1996, Thousand Oaks: Sage Publications
Sprung CL, Geber D, Eidelman LA, Baras M, Pizov R, Nimrod A, Oppenheim A, Epstein L, Cotev S: Evaluation of triage decisions for intensive care admission. Crit Care Med. 1999, 27: 1073-1079. 10.1097/00003246-199906000-00021.
Truog RD, Brock DW, Cook DJ, Danis M, Luce JM, Rubenfeld GD, Levy MM: Rationing in the intensive care unit. Crit Care Med. 2006, 34: 958-963. 10.1097/01.CCM.0000206116.10417.D9.
Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP: Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007, 35: 1477-1476. 10.1097/01.CCM.0000266585.74905.5A.
Chalfin DB, Carlon GC: Age and utilization of intensive care unit resources of critically ill cancer patients. Crit Care Med. 1990, 18: 694-698. 10.1097/00003246-199007000-00002.
Paz HL, Garland A, Weinar M, Crilley P, Brodsky I: Effect of clinical outcomes data on intensive care unit utilization by bone marrow transplant patients. Crit Care Med. 1998, 26: 66-70. 10.1097/00003246-199801000-00018.
Rundek T, Nielsen K, Phillips S, Johnston KC, Hux M, Watson D: Health care resource use after acute stroke in the Glycine Antagonist in Neuroprotection (GAIN) Americas trial. Stroke; a journal of cerebral circulation. 2004, 35: 1368-1374.
Hein OV, Birnbaum J, Wernecke K, England M, Konertz W, Spies C: Prolonged intensive care unit stay in cardiac surgery: risk factors and long-term-survival. Ann Thorac Surg. 2006, 81: 880-885. 10.1016/j.athoracsur.2005.09.077.
American College of Surgeons Committee on Trauma: Optimal hospital resources for care of the seriously injured. Bull Am Coll Surg. 1976, 61 (9): 15-22.
Wunsch H, Rowan KM, Angus DC: International comparisons in critical care: a necessity and challenge. Curr Opin Crit Care. 2007, 13: 725-731.
Birkmeyer JD, Finlayson EV, Birkmeyer CM: Volume standards for high-risk surgical procedures: potential benefits of the Leapfrog initiative. Surgery. 2001, 130: 415-422. 10.1067/msy.2001.117139.
Sudman S, Bradburn NM, Schwarz N: Thinking about answers: the application of cognitive processes to survey methodology. 2005, San Francisco: Jossey Bass
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6963/8/239/prepub
Acknowledgements
This work was supported by the University of Pennsylvania Leschly Fund. Dr. Kahn is supported by a career development award from the United States National Institutes of Health (K23 HL082650). The funding source had no role in the design, implementation, analysis or decision to publish this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
JMK contributed to study conception and design, analyzed the qualitative data, interpreted the results, and drafted the manuscript. RJA performed and transcribed the interviews, analyzed the qualitative data, and critically revised the manuscript for important content. TJI contributed to study conception and design, interpreted the results, and critically revised the manuscript for important content. GDR contributed to study conception and design, interpreted the results, and critically revised the manuscript for important content. DCA contributed to study conception and design, interpreted the results, and critically revised the manuscript for important content. DAA contributed to study conception and design, interpreted the results, and critically revised the manuscript for important content.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kahn, J.M., Asch, R.J., Iwashyna, T.J. et al. Perceived barriers to the regionalization of adult critical care in the United States: a qualitative preliminary study. BMC Health Serv Res 8, 239 (2008). https://doi.org/10.1186/1472-6963-8-239
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6963-8-239