Abstract
Background
Depressive disorder is currently one of the most burdensome disorders worldwide. Evidence-based treatments for depressive disorder are already available, but these are used insufficiently, and with less positive results than possible. Earlier research in the USA has shown good results in the treatment of depressive disorder based on a collaborative care approach with Problem Solving Treatment and an antidepressant treatment algorithm, and research in the UK has also shown good results with Problem Solving Treatment. These treatment strategies may also work very well in the Netherlands too, even though health care systems differ between countries.
Methods/design
This study is a two-armed randomised clinical trial, with randomization on patient-level. The aim of the trial is to evaluate the treatment of depressive disorder in primary care in the Netherlands by means of an adapted collaborative care framework, including contracting and adherence-improving strategies, combined with Problem Solving Treatment and antidepressant medication according to a treatment algorithm. Forty general practices will be randomised to either the intervention group or the control group. Included will be patients who are diagnosed with moderate to severe depression, based on DSM-IV criteria, and stratified according to comorbid chronic physical illness. Patients in the intervention group will receive treatment based on the collaborative care approach, and patients in the control group will receive care as usual. Baseline measurements and follow up measures (3, 6, 9 and 12 months) are assessed using questionnaires and an interview. The primary outcome measure is severity of depressive symptoms, according to the PHQ9. Secondary outcome measures are remission as measured with the PHQ9 and the IDS-SR, and cost-effectiveness measured with the TiC-P, the EQ-5D and the SF-36.
Discussion
In this study, an American model to enhance care for patients with a depressive disorder, the collaborative care model, will be evaluated for effectiveness in the primary care setting. If effective across the Atlantic and across different health care systems, it is also likely to be an effective strategy to implement in the treatment of major depressive disorder in the Netherlands.
Similar content being viewed by others
Background
The burden of depressive disorder on society and on individual patients is enormous. The global burden of disease study reports that unipolar major depressive disorder is expected to be one of the top 2 leading causes of disability-adjusted life years in 2020 [1]. In primary care, 10% of the patients have a depressive disorder -although they may not explicitly seek help for this condition- [2], and when taken together with comorbid anxiety disorders, the community prevalence increases to an alarming 15–20% [2]. Moreover, up to 30% of the population will suffer once in their lifetime from depressive or anxiety symptoms [2, 3]. Depressive disorder has major consequences for the lives of patients, but is treatable. However, it is frequently under-diagnosed and under-treated in primary care [4]. Hence there is clearly room for improvement in the diagnosis and treatment of depressive disorder in primary care.
When looking at pitfalls in the efficient diagnosis and treatment of depressive disorder in primary care, diagnosis is paramount for the success of the treatment. However, several barriers hamper the diagnostic process. Patients often present themselves with several problems at the same time, and the general practitioner (GP) has to deal with 'competing demands', as described by Nutting [5]. In primary care a patient-led agenda is usually followed, and this reduces the chance of detection, because many depressed patients tend to avoid acknowledgement of their distress [5]. Moreover, a European study has shown that the length of the consultation increases drastically when psychosocial problems are detected by the GP [6]. Therefore, GPs do not always focus on the possibility of an underlying mental disorder such as depression.
Detection is further impaired, because 70% of depressed patients present themselves with physical symptoms and not with depressive symptoms [7]. In addition, the comorbidity between somatoform disorders and depression is high; earlier research shows a prevalence of 16.1% for somatoform disorders in primary care, and a 3.3 times greater likelihood of comorbid anxiety/depressive disorder than can be expected by chance [8]. Medically unexplained symptoms are thus, even though not by rule, at least a possible symptom of depressive disorder, and should therefore be addressed. Comorbid somatoform disorder influences the outcome of treatment; comorbid pain with depression, for example, predicts a longer time to remission [9].
Depressive disorder with comorbid physical chronic illness is highly prevalent in primary care [10–13] and it negatively influences (treatment of) the comorbid physical illness, and vice versa [14, 15]. For instance, the course of major depressive disorder in patients with diabetes tends to be more severe, with recurrences being the norm rather than the exception. However, even if these patients are treated successfully, approximately 80% will experience a recurrence [14]. Comorbid depressive disorder is associated with a lower quality of life [16, 17] poor adherence to (diabetic) treatment [14, 18] and also increased health care costs [19, 20]. Therefore, in the present study attention will be paid to comorbid somatoform disorder and physical chronic illness as factors in the accurate diagnosis and treatment of depressive disorder.
In primary care, evidence-based treatments for depressive disorder are available, but these are used insufficiently, and with miscellaneous results [4, 21]. Impeding factors are non-acceptance of the diagnosis, non-adherence of patients to the treatment, and non-adherence of GPs [4]. Earlier research has shown that interventions developed in the mental health setting can also be effective in primary care [22], but screening per se [23] and simple interventions [24] alone are not effective. Many single treatment modes -for instance, pharmacotherapy, psychotherapy or GP training- have been tried out in primary care, but with disappointing results; the treatment modes are, in fact efficacious, but their effect is limited [23]. The efficacy of a specific treatment mode is usually studied in a controlled clinical trial, but the implementation in daily practice under uncontrolled conditions can (and does) lead to different and sometimes worse outcomes [23, 25]. Schulberg therefore opts for ways to transfer efficacious treatments from research settings to routine primary care in a way that 'permits them to flourish', recommending various steps to execute this transfer effectively [25]. Multi-faceted, patient-tailored methods of treatment are needed, in combination with improvement of adherence, i.e. disease-management programmes such as collaborative care [24, 26–29]. Two recent meta-analyses have indeed shown the effectiveness of such collaborative care approaches in primary care [30, 31].
The collaborative care framework used in the present study is based on enhancing active collaboration of the patient with the providers of the treatment, and active collaboration between primary care and mental health care [26, 32]. Within this collaborative care framework the following interventions are implemented: care-management [32, 33], contracting [29] (the care manager explains the nature of the symptoms as part of a depressive disorder, mentions several evidence and guideline-based treatment options, and formulates a treatment plan, together with the patient and the GP in accordance with the preferences of the patient), adherence-enhancing techniques, manual-guided self-help and/or lifestyle changes, Problem Solving Treatment (PST) [34–36] and antidepressant medication according to a treatment algorithm. Psychiatric consultation is one of the adherence-enhancing techniques in the stepped care protocol. Depending on the patients preferences in the contracting phase, the collaborative care treatment plan contains (one of) these modules. Contracting and self help are novel within this collaborative care approach. Contracting is included because it has been proven to be an effective way to enhance adherence [29], and self-help because this strategy has a long history of positive results in the Netherlands [37–40]. In Wagner's chronic care model, self-help has always been a major aspect of good chronic illness care, and in the IMPACT study [27, 32] self-help was also included and referred to as education for self management. In the present study this aspect is emphasized even more. This will be described in more detail in another publication [41].
One of the elements in the collaborative care treatment model is a type of evidence-based psychotherapy for depression that is feasible in primary care. An option that meets these requirements is PST, a brief psychological intervention that is based on problem solving therapy from the behavioural perspective, but is less time-consuming [36, 42]. Research in the UK has recently shown that PST provided by suitably trained practice nurses is effective in the treatment of depressive disorder in primary care patients [34, 35]. The IMPACT study in the USA also successfully implemented PST within a collaborative care approach in the treatment of depressive disorder in primary care patients [32].
Algorithms describing the stepped use of antidepressant medication already exist, but are mainly used in secondary care [43–45]. Antidepressant medication is effective in the treatment of major depressive disorder in primary care [46], but current practice can be further improved by adherence-enhancing strategies according to an algorithm that has been specifically developed for the primary care setting. Elements of the present treatment algorithm are specific decision points for stepped care and recommendations for the choice of medication and daily dosages, implemented by the GP and reinforced by a consultant psychiatrist.
The aim of the current randomised clinical trial (RCT) is to study the effectiveness of treatment for depressive disorder in primary care in the Netherlands based on a collaborative care framework, and including care management, contracting, adherence-improving strategies, manual-guided self help and lifestyle interventions, PST, and an antidepressant treatment algorithm, in which the treatment plan is based on patient preferences, and compared with well-documented care as usual (CAU) as provided by the GP.
The interventions included in the collaborative care package are all evidence-based, and the trial will test the whole package for effectiveness in primary care (compared to care as usual). This study is therefore a pragmatic trial, not an efficacy trial, because it is not the intention to evaluate new interventions [47]. Economic analyses will be performed to assess whether collaborative care is not only effective in terms of response and remission to treatment, but also effective in terms of (health care) costs.
Methods/design
Objectives
The primary aim of the current study is to evaluate the effectiveness of a collaborative care approach, including contracting, PST and an antidepressant treatment algorithm in the treatment of major depressive disorder in primary care. Secondary aims are to assess remission, and to estimate the cost-effectiveness of the intervention.
Study design
The study design is a two-armed randomised pragmatic clinical trial, stratified according to physical chronic illness.
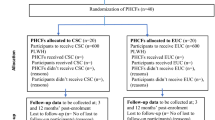
Subjects are randomised and allocated to the intervention (collaborative care) or the control group (CAU). See Figure 1 for flowchart of participants.
Recruitment of GPs
The study is designed in cooperation with the Department of General Practice at the VU Medical Centre in Amsterdam. From the group of general practices connected to this department, as well as from general practices connected to a regional support structure for primary care in two other regions in the Netherlands, practices will be recruited.
Recruitment of patients
The aim is to include patients with a diagnosis of major depressive disorder and who dysfunction due to this depressive disorder (i.e. by the loss of role-functioning in daily life).
All patients who visited the participating practices within the previous 6 months will be selected from the files. These patients will receive a letter describing the purpose of the study, together with an informed consent form for the screening procedure, the Patient Health Questionnaire depression sub-scale (PHQ9) [48] that is used as a screener for depressive disorder, and baseline questionnaires. Any other patients that the GPs recommend for participation will also receive the informed consent letter, the PHQ9 and the baseline questionnaires.
Patients will be included if they reach the cut-off score of 15 for moderate to severe depressive disorder on the PHQ9 and also give informed consent [48]. Subsequently, the Mini-International Neuropsychiatric Interview (MINI [49, 50] will be administered for the classification of symptoms and the diagnosis of major depressive disorder. In the same interview the patients will be asked if they have had the symptoms for at least 6 weeks, and if their dysfunctioning leads to serious problems in at least one of the following roles: work, household activities or relationship.
In the intervention group, the patients will be invited for a consultation with their GP; in the control group, the patients will receive CAU.
Patient exclusion criteria
Patients will be excluded from the study if they are suicidal, psychotic, or suffering from dementia, have insufficient knowledge of the Dutch language to fill in the questionnaires, are addicted to drugs or alcohol, are already receiving psychiatric treatment and/or are under 18 years of age.
Intervention
Training
Since the treatment includes a collaborative care intervention, the participating GPs and care managers will receive training in collaborative care, including contracting and the antidepressant treatment algorithm. The practice nurses will also be trained in care management and will be trained in PST.
The training will be given by the research group. All members of the research group had received training from the IMPACT research group in Seattle [32], the developers of the collaborative care model.
Treatment in the intervention group
1. Collaborative care
The care provided in the intervention group follows a collaborative care approach: patient-tailored care executed, in the current study, within a team of the GP, the patient, the care manager and the consultant psychiatrist. Within this team the need for and the specific requirements for treatment are assessed, and a treatment plan is developed by the GP, the care manager and the patient. Subsequently, the care manager coordinates the care and evaluates each step. If necessary, each treatment step is followed up by a next step to improve the outcome according to the principles of stepped care [51]. The care manager consults the psychiatrist at set points in time, and if there are any difficulties. Subsequently, the care manager advises the GP when necessary.
2. Contracting
During the initial visit, the care manager informs the patient about depressive disorder, and discusses treatment options with the patient. The patient is then offered the choice between several types of treatment (PST and antidepressant medication if desired) and, according to the patient's preferences, a treatment plan is jointly formulated by the care manager, the patient and the GP together.
Initially, the progress of the patient according to the treatment plan is monitored by the care manager, weekly or fortnightly, by telephone or during visits to the clinic. The PHQ9 is filled in, and the results are discussed. When the symptoms are in remission, a relapse prevention plan is formulated by the care manager and the patient together (e.g. defining alarming symptoms and maintenance of antidepressant medication) and follow-up becomes less frequent.
If the patient does not respond (or responds only partially) to the initial treatment, and/or if a patient is not satisfied with the chosen treatment, another form of treatment will be contracted. Subsequent steps are again based on the patient's preferences, and follow the principle of stepped care supervised by the consultant psychiatrist.
3. Improving adherence
The adherence of GPs has been found to be enhanced by a combination of phone calls, written instructions and reminders; an approach that is feasible and effective [24, 27, 52]. The care manager is likewise closely monitored via a net-based tracking system, with set evaluation points every six weeks under the supervision of the consultant psychiatrist. There will be PST supervision, and monthly meetings with other care managers will be held to improve performance as well as adherence.
Patient adherence is improved by contracting and providing written instructions for the patient [24, 53] and the care manager, who monitors the patient meticulously [32].
4. Manual-guided self-help
One of the core symptoms of depression is the loss of interest in (nearly) all activities during the best part of the day, almost every day [54]. In order to relieve these symptoms, a self-help manual has been developed, activating the patients step-by-step as they read each chapter. Initially, the patients are encouraged to participate in low-level behavioural activation, depending on their capability. Attention is paid to restoring the sleep-wake-rhythm [55], self-relaxation-techniques [37, 56] and diet [40, 57]. As the patient improves, there are options for running-therapy, [37, 58] which has recently been proved to be helpful in the treatment of (minor) depressive disorder, and promoting return to work. Two-thirds of the costs involved in the treatment of depressive disorder are accounted for by absence from work through illness, as Bosmans recently pointed out [59].
5. Treatment algorithm for antidepressant medication
To enhance the effectiveness of and adherence to antidepressant medication, the GPs are provided with a protocol of instructions to optimize the prescription of antidepressants. The protocol includes time to titrate to daily dosages (2 weeks), time to respond (partially or remission, another 4 weeks), and well-defined step up criteria and methods (for example 'partial response: increase dose', 'no response: switch medication'). Progress (i.e. (partial) response) is measured with the PHQ9, and results and adverse effects are discussed with the care manager. Subsequently, the care manager advises the GP to step up the treatment (if necessary, after consulting a psychiatrist) if the results are not satisfactory and/or adverse effects are intolerable.
6. Problem solving treatment
PST is provided by the care manager in a course of 6–12 sessions, depending on the progress on the PHQ9 scale. The problem solving approach consists of 7 stages, and is based on the concept that emotional problems are often induced by problems in daily life [35]. The focus lies on regaining control over symptoms by doing something about these problems. The first session lasts for one hour, during which, based on the patient's current problems a clear focus of the treatment is established. Follow-up sessions last for 30 minutes.
Stepped care is realized by evaluation points at 6 weeks and 12 weeks at which it is decided if one or two antidepressants, and 6 sessions or 12 sessions of PST will be sufficient treatment, depending on the improvement according to the PHQ9. It is possible to switch between the two options (e.g. due to disappointing results, or adverse effects) or, if the patients prefers this, to receive a combination of the two treatment options. Either way, the total intervention will last for 18 weeks. This is the maximum duration of the studied intervention.
Treatment in the control group
Half of the general practices function as a control group, and in these practices the patients receive CAU. The actual content of the CAU treatment (e.g. medication, number of contacts in primary care, and referral policy) will be assessed with the Scale for Medical Utilisation of Health Services [53].
Outcome-parameters
1. Primary outcome measure
Response
The severity of the depressive symptoms is measured with the Patient Health Questionnaire depression sub-scale, [48] a brief but valid instrument that scores each of the DSM-IV criteria for major depressive disorder. Response is defined as a 50% reduction of symptoms [48].
2. Secondary outcome measures
Remission of depressive symptoms
Remission -reduction of DSM-IV criteria below the threshold for a diagnosis of depressive disorder- [54] is measured with the PHQ9 [48]. As in previous studies [32, 48, 60], remission is defined as a score between 0 and 4 on the PHQ9.
Cost utility
In addition to the improvement in the severity of symptoms, the cost utility of collaborative care compared to CAU is also assessed. Therefore, the direct medical costs and the costs due to production losses (productivity costs) will be estimated. The relevant data will be collected by means of the Trimbos/iMTA questionnaire for Costs associated with Psychiatric Illness (TiC-P) [61, 62]. Quality of life is assessed with the EuroQol (EQ-5D) [63] and the Short Form-36 (SF-36) [64], which are validated tools for measuring general health-related quality of life.
The EQ-5D descriptive system consists of five dimensions (Mobility, Self Care, Usual Activities, Pain/Discomfort and Anxiety/Depression) each with three levels (no problems, some problems and extreme problems), thus defining 243 (35) distinct health states. Recently, a study in the Netherlands measured and valuated the EQ-5D in a national setting, resulting in the 'Dutch EQ-5D tariff'. The resulting tariff is used to calculate utilities for EQ-5D health states for cost-utility analyses ofDutchhealth care programmes and treatments.
The cost utility is evaluated by relating the difference in direct medical costs per patient receiving collaborative care or CAU to the difference in terms of Quality Adjusted Life Years gained (QALY), which yields a cost per QALY estimate. Furthermore, an attempt will be made to estimate the cost per QALY, including the productivity costs.
3. Effect modifiers and additional outcome measures
Effect of physical illness. Physical comorbidity is measured by means of a questionnaire developed by the Dutch Central Bureau for Statistics (the CBS list). The list contains 28 chronic conditions (e.g. diabetes type II and Multiple Sclerosis). Physical illness is thought to be the key effect modifier.
Somatoform disorder, as measured with the Lichamelijke Klachten Vragenlijst: Bodily Complaints Questionnaire (LKV; assessing the number and intensity of functional somatic complaints a patient is experiencing) [65], the Screening for Somatoform Symptoms-7 (SOMS-7; measuring possible comorbid somatoform disorder) [66], the Illness Attitude Scale (IAS; measuring concern about disease) [67] and the Whitely Index (measuring Hypochondriasis) [67].
Concomitant symptoms of comorbid chronic illness, measured with the Multidimensional Fatigue Inventory (MFI) [68, 69], and the World Health Organization Disability Assessment Survey II (WHO-DAS-II) [70].
Depressive symptoms are assessed as well with the 30-item Inventory for Depressive Symptomatology Self-Report (IDS-SR) [71]. The IDS-SR measures all DSM-IV criteria for the diagnosis of major depressive disorder, as well as the symptoms that are most frequently associated with major depressive disorder (e.g. melancholic symptoms and anxiety) [72].
Preference and adherence. Possible patient preference is based on the preferences of patients in the intervention group, patient adherence is assessed with a qualitative questionnaire, and the patient-doctor working relationship (from the perspective of the patient) is assessed with the Patient Doctor Relationship Questionnaire (PDRQ-9) [73]. The attitude of the GP towards the treatment of depressive disorder is measured with the Depression Attitude Questionnaire (DAQ) [74].
Life-events and social support are measured according to the Social Readjustment Rating Scale [75] and two items of the SF-36 [64], respectively.
Personality is assessed with the Neuroticism extraversion openness-five factor inventory (NEO-FFI; sub-scales 'extraversion' and 'neuroticism') [76, 77].
Treatment in the CAU group is assessed with the Contact between Patients and Practitioners Questionnaire (filled in by the patient) and the Questionnaire Medical Consumption (filled in by the GP) [53].
Baseline measurements take place before inclusion (T0), and follow-up measurements take place after 3 months (T1), 6 months (T2), 9 months (T3) and 12 months (T4).
Sample size
The primary outcome measure is response (a 50% reduction in depressive symptoms). Based on previous work [27] the expected response rate is 14,76% in the CAU group and 31,8% in the intervention group. Given these estimates of the effect of the intervention, and using conventional values for α (0.05) and β (0.80), and two-tailed tests with equal groups, the sample size aimed for in the current study is 94 patients per arm. To compensate for an estimated 26% loss to follow up, 120 patients per arm will be included. (See Figure 1 for flowchart participants.
Analysis
Intention-to-treat analysis will be performed with t-tests, Chi-square tests (dichotomous variables), and General Linear Model (GLM) repeated measurements (continuous variables). The effect size will be estimated by Chi-square tests, and described in Cohen's d. Time to remission will be analysed using survival analysis, and Cox regression models for multivariate analyses will be used for possible effect modifiers (e.g. physical chronic illness and somatoform disorder). Possible confounders such as age, gender, immigrant status, level of education, history of treatment and life events will also be included as variables in these analyses.
Economic evaluation
The aim of the economic evaluation is to assess the cost-effectiveness of collaborative care of the treatment of depressive disorders in primary care. A cost-utility analysis (CUA) will be applied, and the results will be expressed as cost per QALY. The economic evaluation will be undertaken from a societal perspective. Hence, all relevant effects and costs due to resource utilisation within the health care system (direct medical costs) and costs due to production losses (productivity costs) will be included.
Since the collaborative care intervention used in this study is a new intervention, a unit price per session is not known yet. To determine a reference price, a detailed cost-price study will be performed. Therefore, we will perform measurements of time for face-to-face contacts as well as indirect time per contact (e.g. consultations of other specialists) for a total of 20 sessions. Furthermore, we will estimate overhead costs based on the information of the financial department of the hospital. This will result in an estimate of the actual costs per contact. The unit cost estimate per contact will be used as a reference price per contact for the collaborative care intervention.
The TiC-P [61] will be used to assess the costs. The TiC-P is commonly applied in the economic evaluation of treatment in mental health care. For instance, the TiC-P was recently used in a large naturalistic trial on the cost utility of brief psychological treatment for depression and anxiety [62].
To calculate the total direct medical costs, the total number of medical contacts (outpatient visits, length of stay in hospital, use of medication, etc will be multiplied by unit costs of the corresponding health care services. Reference unit prices of health care services will be applied, and adjusted to the year of this study according to the consumer price index [78].
In the second part of the TiC-P a short form of the Health and Labour questionnaire (HLQ) will be used to collect data on productivity losses [79]. The Short-Form HLQ (SF-HLQ) consists of three modules that measure productivity losses: absence from work, reduced efficiency at work and difficulties with job performance [80]. The number of days absent from work and the actual cost of hours missed at work due to health-related problems are calculated from the average value added per worker according to age and gender per day and per hour, respectively. If respondents indicate that they have been absent from work for the entire recall period, data will be collected as from the date when the period of long-term absence started. This additional information will be used to calculate the production losses according to the friction cost method [81, 82]. The friction cost method takes into account the economic circumstances that limit the losses of productivity to society, which is related to the fact that a formerly unemployed person may replace a person who becomes disabled [81].
For the economic evaluation, the effects will be measured by calculating utility scores. In addition to the clinical outcome parameters, utility scores will supply additional information about the impact of collaborative care on the treatment of depressive disorder, compared to CAU on the general health-related quality of life. Furthermore, the results can be compared to a broad range of other health care interventions, also outside the mental health care setting.
The cost utility will be evaluated by relating the difference in direct medical costs per patient receiving collaborative care or CAU to the difference in terms of QALYs gained, which yields a cost per QALY estimate. Furthermore, the cost per QALY, including the productivity costs, will be estimated.
In the case of missing data on costs and/or effects, and the additional uncertainty this introduces, multiple imputation will be used [83]. The Monte Carlo Markov Chain (MCMC) approach will be used to impute the missing values. The uncertainty will be assessed using bootstrapping, and the results will be presented in acceptability curves [84].
Time-frame of the study
The preparatory period is 6 months. Subsequent to the approval of the Medical Ethical Board, general practices will be recruited and the GPs and care managers will be trained. The inclusion and intervention phase will take 22 months. The follow-up phase will be 6 months, and the data-analyses will last for 6 months. The entire study period will last for 4 years.
Ethical principles
The study has been designed, and will be executed in accordance with the principles laid down in the Helsinki Declaration (Edinburgh, Scotland amendment, October 2000).
Participation in the study is voluntary, and written informed consent will be obtained. The patients will be explicitly informed of the fact that they can withdraw their consent to participate at any time, without specification of reasons and with no negative consequences with regard to their future medical treatment. Patients who wish to withdraw from the study will receive care as usual.
The study protocol has been approved by the Medical Ethics Committee of the VU Medical Centre.
Discussion
The aim of this study is to investigate the effectiveness of an American model of collaborative care for the treatment of depression, implemented in the Netherlands. The emphasis lies on collaboration with a care manager, team effort and stepped care. Trials on such disease management programmes have so far shown promising results in the USA and the UK respectively [23, 33, 85–87], and are also likely to show the same results in the Netherlands. The focus hereby lies on major depressive disorder, since disease management programmes are developed to treat chronic diseases [32, 88], and major depressive disorder closely resembles a chronic disease in terms of difficulty to treat, impact on daily life, duration, and chance of relapse [2].
Strengths and limitations
Critics may raise concern about whether collaborative care -as designed in the USA- can be effectively implemented in the Netherlands, since the health care systems differ between the two countries. The American health care system is based on the comparatively rare private enterprise health care system (i.e. decentralized payment) whereas in the Netherlands there is a public insurance system (i.e. centralized payment). Primary care in the Netherlands is, in the majority of cases, provided in very small practices (1–2 GPs), and is in many ways less organized and less centralized than thelarger group practices in the USA. This could present a challenge in the implementation of a team-based approach with a care manager, because it is not likely that a solo general practice can really afford to have a full-time care manager, so the care managers will probably also have several other practice tasks. However, the collaborative care approach has been implemented in several settings, with different health care providers and different levels of CAU [32], and in each setting significant improvement has been reported for the collaborative care approach compared to CAU [27, 30, 31, 89]. One can therefore expect to find the same improvement when the collaborative care approach is carefully implemented in the Netherlands.
A possible limitation of the study might also be that we are adding two elements, i.e. self-care (a self-help manual has been developed for this trial, enhancing patient empowerment) and contracting, in which the weighing of patient preferences for a given treatment is crucial. This might make the intervention stronger, but it might also make implementation more strenuous. Therefore, specific emphasis will be laid on adherence to these two additional aspects of the model.
Due to randomisation at patient level, one can argue that contamination of effect could occur: GPs and care managers might transfer their knowledge of the intervention to the control group. The risk of dilution of effect however, is expected to be very small. The positive effect of the intervention can only be reached by implementing the whole package, including the care manager who plays the most significant role within the model, and patients receiving care as usual are not involved with a care manager. The antidepressant treatment algorithm will be carried out by the GPs and not the care manager, but under strict supervision of the consultant psychiatrist, so dilution of effect in the control group, when medication is concerned, is also expected to be small.
A characteristic of collaborative care is the fact that the offered treatments are all evidence-based; efficacy thus has previously been proved. Effectiveness trials and reviews have already shown mixed but positive results concerning the optional treatment modes: short-term psychotherapy and antidepressant medication if desired. Either no significant difference is found between the effectiveness of antidepressant medication and psychotherapy [90–92] or, a combination of antidepressant medication and some form of psychotherapy is most effective [91, 93]. A strong aspect of this design is the fact that we are offering both evidence-based treatment modes in a package.
Strengths and limitations taken into account, at the very least patients make a significant contribution to (the choice of) the treatment in this design. Aiming, above all else, to relieve patients of the burden of depressive disorder, this seems a particularly valuable contribution to the design.
References
Murray CJ, Lopez AD: Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet. 1997, 349: 1498-1504. 10.1016/S0140-6736(96)07492-2.
Bijl RV, Ravelli A, van Zessen G: Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS). Soc Psychiatry Psychiatr Epidemiol. 1998, 33: 587-595. 10.1007/s001270050098.
De Graaf R, Bijl RV, Spijker J, Beekman ATF, Vollebergh WA: Temporal sequencing of lifetime mood disorders in relation to comorbid anxiety and substance use disorders – findings from the Netherlands Mental Health Survey and Incidence Study. Soc Psychiatry Psychiatr Epidemiol. 2003, 38: 1-11. 10.1007/s00127-003-0597-4.
Ormel J, Bartel M, Nolen WA: [Undertreatment of depression; causes and recommendations. In Dutch]. Ned Tijdschr Geneeskd. 2003, 147: 1005-1009.
Nutting PA, Rost K, Smith J, Werner JJ, Elliot C: Competing demands from physical problems: effect on initiating and completing depression care over 6 months. Arch Fam Med. 2000, 9: 1059-1064. 10.1001/archfami.9.10.1059.
Deveugele M, Derese A, Brink-Muinen A, Bensing J, de Maeseneer J: Consultation length in general practice: cross sectional study in six European countries. BMJ. 2002, 325: 472-10.1136/bmj.325.7362.472.
Simon GE, Von Korff M, Piccinelli M, Fullerton C, Ormel J: An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999, 341: 1329-1335. 10.1056/NEJM199910283411801.
De Waal MW, Arnold IA, Eekhof JA, van Hemert AM: Somatoform disorders in general practice: prevalence, functional impairment and comorbidity with anxiety and depressive disorders. Br J Psychiatry. 2004, 184: 470-476. 10.1192/bjp.184.6.470.
Karp JF, Scott J, Houck P, Reynolds CF, Kupfer DJ, Frank E: Pain predicts longer time to remission during treatment of recurrent depression. J Clin Psychiatry. 2005, 66: 591-597.
Kathol RG, Petty F: Relationship of depression to medical illness. A critical review. J Affect Disord. 1981, 3: 111-121. 10.1016/0165-0327(81)90036-7.
Wittchen HU, Lieb R, Wunderlich U, Schuster P: Comorbidity in primary care: presentation and consequences. J Clin Psychiatry. 1999, 60 (Suppl 7): 29-36.
Mergl R, Seidscheck I, Allgaier AK, Moller HJ, Hegerl U, Henkel V: Depressive, anxiety, and somatoform disorders in primary care: prevalence and recognition. Depress Anxiety. 2006.
Nuyen J, Schellevis FG, Satariano WA, Spreeuwenberg PM, Birkner MD, van den Bos GAM, Groenewegen PP: Comorbidity associated with neurologic and psychiatric diseases: A general practice-based controlled study. J of Clin Epidemiol.
Lustman PJ, Griffith LS, Clouse RE: Depression in Adults with Diabetes. Semin Clin Neuropsychiatry. 1997, 2: 15-23.
Katon WJ: Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003, 54: 216-226. 10.1016/S0006-3223(03)00273-7.
Goldney RD, Phillips PJ, Fisher LJ, Wilson DH: Diabetes, depression, and quality of life: a population study. Diabetes Care. 2004, 27: 1066-1070. 10.2337/diacare.27.5.1066.
Cully JA, Graham DP, Stanley MA, Ferguson CJ, Sharafkhaneh A, Souchek J, Kunik ME: Quality of life in patients with chronic obstructive pulmonary disease and comorbid anxiety or depression. Psychosomatics. 2006, 47: 312-319. 10.1176/appi.psy.47.4.312.
Gehi A, Haas D, Pipkin S, Whooley MA: Depression and medication adherence in outpatients with coronary heart disease: findings from the Heart and Soul Study. Arch Intern Med. 2005, 165: 2508-2513. 10.1001/archinte.165.21.2508.
Ciechanowski PS, Katon WJ, Russo JE: Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000, 160: 3278-3285. 10.1001/archinte.160.21.3278.
Katon WJ, Lin EH, Russo JE, Unutzer J: Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psychiatry. 2003, 60: 897-903. 10.1001/archpsyc.60.9.897.
Bodenheimer T: Helping patients improve their health-related behaviors: what system changes do we need?. Dis Manag. 2005, 8: 319-330. 10.1089/dis.2005.8.319.
Schulberg HC, Katon WJ, Simon GE, Rush AJ: Treating major depression in primary care practice: an update of the Agency for Health Care Policy and Research Practice Guidelines. Arch Gen Psychiatry. 1998, 55: 1121-1127. 10.1001/archpsyc.55.12.1121.
Bijl D, van Marwijk HWJ, de Haan M, van Tilburg W, Beekman ATF: Effectiveness of disease management programmes for recognition, diagnosis and treatment of depression in primary care. Eur J Gen Pract. 2004, 10: 6-12.
Van der Feltz-Cornelis CM, van Oppen P, Adèr H, van Dyck R: Randomised Controlled Trial of a Collaborative Care Model with Psychiatric Consultation for Persistent Medically Unexplained Symptoms in General Practice. Psychother Psychosom. 2006, 75: 282-289. 10.1159/000093949.
Schulberg HC: Treating depression in primary care practice: applications of research findings. J Fam Pract. 2001, 50: 535-537.
Katon WJ, Von Korff M, Lin EH, Simon GE, Walker EA, Unutzer J, Bush T, Russo J, Ludman E: Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiatry. 1999, 56: 1109-1115. 10.1001/archpsyc.56.12.1109.
Unutzer J, Katon WJ, Callahan CM, Williams JW, Hunkeler EM, Harpole L, Hoffing M, Della Penna RD, Hitchcock Noël P, Lin EHB, Areán PA, Hegel MT, Tang L, Belin TR, Oishi SM, Langston CA: Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002, 288: 2836-2845. 10.1001/jama.288.22.2836.
Katon WJ, Russo JE, Von Korff M, Lin EH, Simon GE, Bush T, Ludman E, Walker E: Long-term effects of a collaborative care intervention in persistently depressed primary care patients. J Gen Intern Med. 2002, 17: 741-748. 10.1046/j.1525-1497.2002.11051.x.
Van der Feltz-Cornelis CM, van Oppen P, Adèr H, van Dyck R: [Collaborative care for physically unexplained symptoms in primary care. Results and profits for general practitioners. In Dutch]. Huisarts & Wetenschap. 2006, 49: 342-347.
Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ: Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006, 166: 2314-2321. 10.1001/archinte.166.21.2314.
Bower P, Gilbody S, Richards D, Fletcher J, Sutton A: Collaborative care for depression in primary care: Making sense of a complex intervention: systematic review and meta-regression. Br J Psychiatry. 2006, 189: 484-493. 10.1192/bjp.bp.106.023655.
Unutzer J, Katon WJ, Williams JW, Callahan CM, Harpole L, Hunkeler EM, Hoffing M, Areán PA, Hegel MT, Schoenbaum M, Oishi SM, Langston CA: Improving primary care for depression in late life: the design of a multicenter randomized trial. Med Care. 2001, 39: 785-799. 10.1097/00005650-200108000-00005.
Gensichen J, Beyer M, Muth C, Gerlach FM, Von Korff M, Ormel J: Case management to improve major depression in primary health care: a systematic review. Psychol Med. 2006, 36: 7-14. 10.1017/S0033291705005568.
Mynors-Wallis LM, Gath DH, Day A, Baker F: Randomised controlled trial of problem solving treatment, antidepressant medication, and combined treatment for major depression in primary care. BMJ. 2000, 320: 26-30. 10.1136/bmj.320.7226.26.
Mynors-Wallis LM, Davies I, Gray A, Barbour F, Gath DH: A randomised controlled trial and cost analysis of problem-solving treatment for emotional disorders given by community nurses in primary care. Br J Psychiatry. 1997, 170: 113-119.
Mynors-Wallis LM, Gath DH, Lloyd-Thomas AR, Tomlinson D: Randomised controlled trial comparing problem solving treatment with amitriptyline and placebo for major depression in primary care. BMJ. 1995, 310: 441-445.
CBO, Trimbos-instituut: Multidisciplinairy Guideline Depressive disorder [Multidisciplinaire Richtlijn Depressie. In Dutch]. 2005, Utrecht: Trimbos-insituut
Cuijpers P: [In de put, uit de put. Zelf depressiviteit overwinnen. In Dutch]. 2003, Baarn: HB Uitgevers
Cuijpers P, Buijssen H: [Ik zie het weer zitten. Omgaan met depressiviteit/Control your depression. In Dutch]. 1997, Utrecht: Teleac/NOT
Willemse GR, Smit F, Cuijpers P, Tiemens BG: Minimal-contact psychotherapy for sub-threshold depression in primary care. Randomised trial. Br J Psychiatry. 2004, 185: 416-421. 10.1192/bjp.185.5.416.
Vlasveld M, Beekman ATF, Hakkaart-van Roijen L, Hoedeman R, van Marwijk HWJ, van der Feltz-Cornelis CM: The cost-effectiveness of Collaborative Care for Depressive Disorder in the Occupational Health Setting; study protocol of a randomised controlled trial. BMC, article under construction.
Mynors-Wallis LM: Problem-solving treatment in general psychiatric practice. Adv Psych Treatment. 2001, 7: 417-425. 10.1192/apt.7.6.417.
Adli M, Berghofer A, Linden M, Helmchen H, Muller-Oerlinghausen B, Mackert A, Stamm T, Bauer M: Effectiveness and feasibility of a standardized stepwise drug treatment regimen algorithm for inpatients with depressive disorders: results of a 2-year observational algorithm study. J Clin Psychiatry. 2002, 63: 782-790.
Bondolfi G, Aubry JM, Golaz J, Gex-Fabry M, Gervasoni N, Bertschy G: A stepwise drug treatment algorithm to obtain complete remission in depression: a Geneva study. Swiss Med Wkly. 2006, 136: 78-85.
Trivedi MH, Rush AJ, Crismon ML, Kashner TM, Toprac MG, Carmody TJ, Key T, Biggs MM, Shores-Wilson K, Witte B, Suppes T, Miller AL, Altshuler KZ, Shon SP: Clinical results for patients with major depressive disorder in the Texas Medication Algorithm Project. Arch Gen Psychiatry. 2004, 61: 669-680. 10.1001/archpsyc.61.7.669.
Arroll B, Macgillivray S, Ogston S, Reid I, Sullivan F, Williams B, Crombie I: Efficacy and tolerability of tricyclic antidepressants and SSRIs compared with placebo for treatment of depression in primary care: a meta-analysis. Ann Fam Med. 2005, 3: 449-456. 10.1370/afm.349.
Feinstein AR: Clinical epidemiology: the architecture of clinical research. 1985, Philadelphia: WB Saunders, First
Kroenke K, Spitzer RL, Williams JB: The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001, 16: 606-613. 10.1046/j.1525-1497.2001.016009606.x.
Van Vliet IM, Leroy H, van Megen HJM: [The MINI-International neuropsychiatric interview: a short, structured, diagnostic interview for DSM-IV and ICD-10 psychiatric disorders. In Dutch]. 2000, Leiden: LUMC
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC: The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998, 59 (Suppl 20): 22-33.
Meeuwissen JAC, Donker MCH: [Less is more. Stepped care in mental health care. In Dutch]. Maandblad Geestelijke Volksgezondheid. 2004, 59: 904-915.
Bettinger TL, Crismon ML, Trivedi MH, Grannemann B, Shon SP: Clinicians' adherence to an algorithm for pharmacotherapy of depression in the Texas public mental health sector. Psychiatr Serv. 2004, 55: 703-705. 10.1176/appi.ps.55.6.703.
Van der Feltz-Cornelis CM: Psychiatric consultation for patients with somatoform disorder in general practice. PhD-thesis. 2002, VU Amsterdam
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders (4th ed. TR). 2000, Washington DC
Oosterhuis A, Klip EC: The treatment of insomnia through mass media, the results of a televised behavioral training programme. Soc Sci Med. 1997, 45: 1223-1229. 10.1016/S0277-9536(97)00041-5.
Jorm AF, Christensen H, Griffiths KM, Rodgers B: Effectiveness of complementary and self-help treatments for depression. Med J Aust. 2002, 176 (Suppl): S84-S96.
Sontrop J, Campbell MK: Omega-3 polyunsaturated fatty acids and depression: a review of the evidence and a methodological critique. Prev Med. 2006, 42: 4-13. 10.1016/j.ypmed.2005.11.005.
Bosscher RJ: [Runningtherapy in the treatment of Depressive disorder. In Dutch]. PhD-thesis. 1991, VU Amsterdam
Bosmans JE: Cost-effectiveness of treatment of depression in primary care. PhD-thesis. 2006, VU Amsterdam
Lowe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K: Monitoring depression treatment outcomes with the patient health questionnaire-9. Med Care. 2004, 42: 1194-1201. 10.1097/00005650-200412000-00006.
Hakkaart-van Roijen L: [Manual Trimbos/iMTA questionnaire for costs associated with psychiatric illness. In Dutch]. 2002, Rotterdam: Institute for Medical Technology Assessment
Hakkaart-van Roijen L, Straten van A, Al MJ, Rutten F, Donker M: Cost-utility of brief psychological treatment for depression and anxiety. Br J Psychiatry. 2006, 323-329. 10.1192/bjp.188.4.323.
Euroqol group: Eq-5D user guide. 1995, Rotterdam: Sanders instituut, eur
Ware JE, Sherbourne CD: The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992, 30: 473-483. 10.1097/00005650-199206000-00002.
Hemert AM: [Bodily Complaints Questionnaire. In Dutch]. 2003, Leiden: Leids Universitair Medisch Centrum
Rief W, Hiller W: A new approach to the assessment of the treatment effects of somatoform disorders. Psychosomatics. 2003, 44: 492-498. 10.1176/appi.psy.44.6.492.
Speckens AE, Spinhoven P, Sloekers PP, Bolk JH, van Hemert AM: A validation study of the Whitely Index, the Illness Attitude Scales, and the Somatosensory Amplification Scale in general medical and general practice patients. J Psychosom Res. 1996, 40: 95-104. 10.1016/0022-3999(95)00561-7.
Smets EM, Garssen B, Bonke B, de Haes JC: The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995, 39: 315-325. 10.1016/0022-3999(94)00125-O.
Schneider RA: Reliability and validity of the Multidimensional Fatigue Inventory (MFI-20) and the Rhoten Fatigue Scale among rural cancer outpatients. Cancer Nurs. 1998, 21: 370-373. 10.1097/00002820-199810000-00009.
WHO: Disability Assessment Schedule II (WHO-DAS-II), brief version pilot, interviewer's manual. 1998, Geneva: WHO
Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH: The Inventory of Depressive Symptomatology (IDS): psychometric properties. Psychol Med. 1996, 26: 477-486.
Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T, Crismon ML, Shores-Wilson K, Toprac MG, Dennehy EB, Witte B, Kashner TM: The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychol Med. 2004, 34: 73-82. 10.1017/S0033291703001107.
Van der Feltz-Cornelis CM, van Oppen P, van Marwijk HWJ, de Beurs E, van Dyck R: A patient-doctor relationship questionnaire (PDRQ-9) in primary care: development and psychometric evaluation. Gen Hosp Psychiatry. 2004, 26: 115-120. 10.1016/j.genhosppsych.2003.08.010.
Botega N, Blizard R, Wilkinson DG, Mann A: General practitioners and depression first use of the depression attitude questionnaire. International Journal of Methods for Psychiatric Research. 1992, 4: 169-180.
Holmes TH, Rahe RH: The Social Readjustment Rating Scale. J Psychosom Res. 1967, 11: 213-218. 10.1016/0022-3999(67)90010-4.
Hoekstra HA, de Fruyt F: [NEO-PI-R and NEO-FFI: Big Five Personality-questionnaires: Manual. In Dutch]. 1996, Lisse: Swets & Zeitlinger
Duggan C, Sham P, Lee A, Minne C, Murray R: Neuroticism: a vulnerability marker for depression evidence from a family study. J Affect Disord. 1995, 35: 139-143. 10.1016/0165-0327(95)00062-3.
Oostenbrink JB, Bouwmans CAM, Koopmanschap MA, Rutten FF: [Handleiding voor kostenonderzoek, methoden en standaardkostprijzen voor economische evaluaties in de gezondheidszorg. In Dutch]. 2004, College voor zorgverzekeringen
Van Roijen L, Essink-Bot ML, Koopmanschap MA, Bonsel G, Rutten FF: Labor and health status in economic evaluation of health care. The Health and Labor Questionnaire. Int J Technol Assess Health Care. 1996, 12: 405-415.
Van Dam QD, Spijker A, Arends LR: [Costeffectiveness of psychotherapy: A feasiblity study. In Dutch]. J of Pychotherapy. 1998, 24: 5-22.
Koopmanschap MA, Rutten FF: A practical guide for calculating indirect costs of disease. Pharmacoeconomics. 1996, 10: 460-466.
Koopmanschap MA, Rutten FF, van Ineveld BM, van Roijen L: The friction cost method for measuring indirect costs of disease. J Health Econ. 1995, 14: 171-189. 10.1016/0167-6296(94)00044-5.
Rubin DB: Multiple imputation after 18+ years. J Am Stat Assoc. 1996, 91: 473-489. 10.2307/2291635.
Van Hout BA, Al MJ, Gordon GS, Rutten FF: Costs, effects and C/E-ratios alongside a clinical trial. Health Econ. 1994, 3: 309-319.
Adli M, Bauer M, Rush AJ: Algorithms and collaborative-care systems for depression: are they effective and why? A systematic review. Biol Psychiatry. 2006, 59: 1029-1038. 10.1016/j.biopsych.2006.05.010.
Badamgarav E, Weingarten SR, Henning JM, Knight K, Hasselblad V, Gano A, Ofman JJ: Effectiveness of disease management programs in depression: a systematic review. Am J Psychiatry. 2003, 160: 2080-2090. 10.1176/appi.ajp.160.12.2080.
Neumeyer-Gromen A, Lampert T, Stark K, Kallischnigg G: Disease management programs for depression: a systematic review and meta-analysis of randomized controlled trials. Med Care. 2004, 42: 1211-1221. 10.1097/00005650-200412000-00008.
Schrijvers G: Disease management programs in the USA and Europe are comparable (yet?) different. Int J Integr Care. 2006, 6: e13.
Unutzer J, Powers D, Katon WJ, Langston CA: From establishing an evidence-based practice to implementation in real-world settings: IMPACT as a case study. Psychiatr Clin North Am. 2005, 28: 1079-1092. 10.1016/j.psc.2005.09.001.
DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, O'Reardon JP, Lovett ML, Gladis MM, Brown LL, Gallop R: Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatry. 2005, 62: 409-416. 10.1001/archpsyc.62.4.409.
Hollon SD, Jarrett RB, Nierenberg AA, Thase ME, Trivedi MH, Rush AJ: Psychotherapy and medication in the treatment of adult and geriatric depression: which monotherapy or combined treatment?. J Clin Psychiatry. 2005, 66: 455-468.
Hollon SD, DeRubeis RJ, Shelton RC, Amsterdam JD, Salomon RM, O'Reardon JP, Lovett ML, Young PR, Haman KL, Freeman BB, Gallop S: Prevention of relapse following cognitive therapy vs medications in moderate to severe depression. Arch Gen Psychiatry. 2005, 62: 417-422. 10.1001/archpsyc.62.4.417.
Pampallona S, Bollini P, Tibaldi G, Kupelnick B, Munizza C: Combined pharmacotherapy and psychological treatment for depression: a systematic review. Arch Gen Psychiatry. 2004, 61: 714-719. 10.1001/archpsyc.61.7.714.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6963/7/34/prepub
Acknowledgements
The Foundation Central Funds RVVZ (Reserves Formally Voluntary National Health Service insurances) in the Netherlands funds this project.
We would also like to thank Giel Nijpels, connected to the VU Medical Centre for his contribution to the design-discussions; and Diane Powers and Rita Haverkamp, connected to the IMPACT research group, for their training and advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
CFC is principle investigator, daily supervisor and consultant psychiatrist in the trial. HvM is daily mentor and AB is monthly supervisor. LHR will be supervising the cost-effectiveness part of the trial and FR contributed to the design. JU is principle investigator of the IMPACT trial in the USA and international advisor on the design. KH will be executing the trial together with MIJ. All participants have contributed their part of expertise and read and approved the latest version of the article.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
IJff, M.A., Huijbregts, K.M., van Marwijk, H.W. et al. Cost-effectiveness of collaborative care including PST and an antidepressant treatment algorithm for the treatment of major depressive disorder in primary care; a randomised clinical trial. BMC Health Serv Res 7, 34 (2007). https://doi.org/10.1186/1472-6963-7-34
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6963-7-34