Abstract
Background
It has been proposed that greater availability of primary medical care practitioners (GPs) contributes to better population health. We evaluated whether measures of the supply and structure of primary medical services are associated with health and health care indicators after adjusting for confounding.
Methods
Data for the supply and structure of primary medical services and the characteristics of registered patients were analysed for 99 health authorities in England in 1999. Health and health care indicators as dependent variables included standardised mortality ratios (SMR), standardised hospital admission rates, and conceptions under the age of 18 years. Linear regression analyses were adjusted for Townsend score, proportion of ethnic minorities and proportion of social class IV/ V.
Results
Higher proportions of registered rural patients and patients ≥ 75 years were associated with lower Townsend deprivation scores, with larger partnership sizes and with better health outcomes. A unit increase in partnership size was associated with a 4.2 (95% confidence interval 1.7 to 6.7) unit decrease in SMR for all-cause mortality at 15–64 years (P = 0.001). A 10% increase in single-handed practices was associated with a 1.5 (0.2 to 2.9) unit increase in SMR (P = 0.027). After additional adjustment for percent of rural and elderly patients, partnership size and proportion of single-handed practices, GP supply was not associated with SMR (-2.8, -6.9 to 1.3, P = 0.183).
Conclusions
After adjusting for confounding with health needs of populations, mortality is weakly associated with the degree of organisation of practices as represented by the partnership size but not with the supply of GPs.
Similar content being viewed by others
Background
In 1971 Tudor Hart described what he termed the 'inverse care law' which stated that 'the availability of good medical care tends to vary inversely with the need for it in the population served' [1]. Deprived areas with worse health have fewer general practitioners[2] (GPs), and general practices in these areas tend to be less well organised, offering fewer services[3], giving shorter consultation times [4], and perhaps providing lower quality care).)[5]. Recent policies for the allocation of health care resources in the NHS, and for the contractual arrangements for GPs have attempted to redress some of these inequalities in order to promote equity in access to primary care.
Similar inequalities in the availability of primary medical care have also been reported in the US literature. Shi and colleagues [6, 7] found that states with fewer primary care doctors had higher mortality, even after adjusting for income inequality and smoking as socio-economic influences on health. They argued that better access to primary medical care might lead to improved health status and reduced socio-economic inequalities in health. In their analyses, population health indicators were viewed, not as measures of health care need as has generally been the case in the English literature, but as measures of health care outcome. Under this interpretation, investment in primary care is viewed as a route to achieving equity in health.
We recently reported the results of analyses[8] which aimed to replicate the models of Shi et al [6, 7] in an English context. The results were obtained from an ecological study of data for 99 health authorities in England in 1999. In order to allow for variations in the socio-economic conditions of different areas, we adjusted for Townsend deprivation score, the proportion of the population in social classes IV and V and the proportion of ethnic minorities. In these analyses, each unit increase in the supply of general practitioners per 10,000 population was associated with a 5.2 unit (95% confidence interval 2.0 to 8.3, P = 0.002) decrease in the standardised mortality ratio for all cause mortality at ages 15 to 64 years[8]. Since adjustment for variations in health need associated with socio-economic inequality might be incomplete, we additionally adjusted for the proportion of the population with limiting long term illness; the association between GP supply and mortality was then attenuated (mean difference -3.3, -6.7 to 0.1, P = 0.060). Pereira Gray[9] criticised our interpretation, arguing that the proportion of the population with limiting long term illness can be regarded as one of the outcomes of primary medical care, and also part of the causal pathway linking primary medical care and mortality. In his view, the analyses provided convincing evidence that better access to primary care contributes to improved health outcomes[9]. This debate is reflected in the English Department of Health's recent choice of an indicator of access to primary care, the number of primary care professionals per 100,000 population, as one of 12 headline indicators for its strategy on addressing inequalities in health[10].
The association of general practitioner supply with health measures might be explained by confounding in several ways. There may be residual confounding with population characteristics even after adjustment for Townsend score, social class and ethnicity. The supply of GPs might be confounded with other aspects of the structure and functioning of primary care services such as the number of partners in a practice or the types of services offered. Finally, there may also be confounding with access to other services such as the availability of hospital services. Further insights into these relationships may be obtained by exploring the relationships between a wider range of characteristics of primary medical services and population health indicators and measures of health service utilisation. A key question concerns whether the relationship between primary care access and mortality is more strongly associated with the services provided by practices or with the characteristics of populations registered with practices. This paper therefore presents results of analyses which aimed to determine how different primary medical services access variables were associated with population health indicators and measures of health service utilisation after adjusting for socio-economic deprivation. Indicators included measures both of the supply of primary medical services, including the structure of general practices and the types of services offered, and the socio-demographic characteristics of registered populations.
Methods
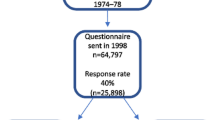
Data for the 99 health authorities in England in 1999 were obtained from the English Department of Health's statistical publications[11, 12] and from the National Database for Primary Care Groups and Trusts developed by the National Primary Care Research and Development Centre in Manchester [13]. We obtained data for six population health and health service indicators including the standardised mortality ratio (SMR) for all-cause mortality at ages 15 to 64 years, the SMR for acute myocardial infarction at 35 to 64 years, the SMR for avoidable mortality [14], standardised hospital emergency admission rates per 100,000 for acute conditions (infections of the ears, nose and throat, or kidneys and urinary tract and heart failure) and chronic conditions (diabetes and asthma), and the conception rate per 1,000 in women less than 18 years of age. Comprehensive definitions of these indicators are provided in relevant publications [11–13]. Hospital admission rates provide measures of health care utilisation but may also be viewed as measures of the effective delivery of primary care when hospital admissions are considered, as here, to be either preventable or amenable to effective care in primary settings. The conception rate in women less than 18 years is considered in the English Department of Health's dataset to be an indicator of 'health improvement'; that is, an indicator which may be influenced by multi-sectoral activities aimed at improving health.
Primary medical services indicators included the number of whole time equivalent GPs per 10,000 weighted population. In Department of Health indicator datasets the estimated denominator populations for this indicator are weighted for need [2, 11]. The socio-demographic characteristics of the registered populations were the percent of rural patients and the percent of patients aged ≥ 75 years. 'Rural' patients are patients who are registered with a practice but reside more than three miles from a practice. The structure of services was measured in terms of the mean partnership size, the proportion of single-handed practices (a special case of the partnership size), the proportion of GPs aged ≥ 61 years and the proportion of practices with a female GP. The types of services were measured in terms of the proportion of practices with services for diabetes, child health surveillance or contraception (for any patient).
The association of population health measures with primary medical services indicators were evaluated using multiple linear regression with observations weighted for health authority population size. In initial analyses, we explored the relationship between primary care measures and outcomes after adjusting for confounders. These were the Townsend deprivation score (an index of deprivation based on census-derived data for unemployment, housing tenure, overcrowding and car ownership), the proportion in social class IV and V, and the proportion in households headed by persons born in the New Commonwealth as a measure of the proportion of ethnic minorities. In the next stage of the analysis, we included additionally all explanatory variables which were consistently associated with outcomes. This model included adjustment for Townsend score, social class, ethnic group, proportion of rural patients, proportion of patients ≥ 75 years, the supply of GPs, the partnership size and the proportion of single handed practices. This approach was preferred to a stepwise elimination from all candidate variables because the latter led to different models for each outcome, and because confounders may be important even when they do not yield statistically significant associations.
Results
The independent associations of the standardised mortality ratio for all-cause mortality at ages 15 to 64 years with deprivation and general practitioner supply are shown in Table 1, using the Townsend score as the primary measure of deprivation. The mean SMR increased with increasing deprivation tertile but within each deprivation tertile, mortality declined with increasing GP supply tertile. There was no evidence for an interaction between Townsend score and GP supply (P = 0.832). In the least deprived tertile there were no health authorities with the lowest level of GP supply.
The distributions of primary medical services indicators are shown in Table 2. Inspection of the correlation coefficients reveals that the GP supply was greater where there was a high proportion of rural patients. There was a positive association between GP supply and both partnership size and proportion of female GPs. The proportion of single-handed practices, and of GPs older than sixty, was lower where the GP supply was high. Provision of specific services for diabetes or for contraception was greater when the GP supply was higher. Higher Townsend scores, indicating greater deprivation, were associated with lower proportions of older or rural patients. High Townsend scores were also associated with lower supply of GPs, a greater frequency of single-handed practices, more older doctors, fewer female GPs, and lower provision of specific services.
In these analyses (Tables 3 and 4), after adjusting for deprivation, social class and ethnicity, a higher supply of GPs was associated with lower mortality, lower hospital utilisation and lower rates of teenage conceptions as reported previously[8]. The socio-demographic characteristics of the populations registered with practices were strongly associated with each of the population health measures. Health authorities with a high proportion of rural patients registered with their practices had more favourable values for each of the measures of population health or health service utilisation. The proportion of registered patients aged 75 years or over, was associated generally with lower values for the health indicators although conventional levels of statistical significance were not reached for mortality from acute myocardial infarction or hospital admissions for chronic conditions. Note that each of the population health measures was either standardised or stratified for age. When the association of GP supply and all cause mortality SMR was adjusted for percent of rural patients and percent of registered patients ≥ 75 years, as well as Townsend score, social class and ethnicity, the coefficient was reduced to -3.7 (-7.2 to -0.2, P = 0.036).
Health authorities where general practices had more partners had consistently lower values for population health measures (Tables 3 and 4). The proportions of single-handed practices, GPs older than sixty, or practices with female partners, were strongly associated with patterns of emergency hospital utilisation but only weakly or not associated with mortality or the proportion of teenage conceptions. In general the availability of services for diabetes or child health surveillance was not associated with outcome measures. The provision of contraceptive services was associated with reduced hospital utilisation but not with teenage conceptions.
In the next stage of analysis, we evaluated the independent associations of the variables included in Tables 3 and 4. Since the types of services were generally not associated with outcome measures, these were excluded. The proportions of GPs aged ≥ 61 years and the proportion of female GPs were also excluded because they were not associated with mortality indicators. This final model therefore included the Townsend score, proportion in social class IV/V, proportion of ethnic minorities, proportions of rural patients and patients aged ≥ 75 years as confounders. The GP supply, the mean partnership size and proportion of single-handed practices were included as primary care indicators. Coefficients obtained for each outcome measure from these models are shown in Table 5. In this model, the GP supply was not associated with mortality indicators, only weakly associated with hospital utilisation for acute and chronic conditions and was associated with teenage conceptions. The partnership size, and the proportion of single-handed practices were associated with all-cause mortality and more strongly with avoidable mortality. The partnership size but not the proportion of single-handed practices was associated with myocardial infarction mortality. The partnership size and the proportion of single handed practices were not associated with hospital utilisation or teenage conceptions.
Discussion
The supply of GPs is associated with variations in the characteristics of primary medical care services including the partnership size, the characteristics of the practitioner including age and gender, the services provided by a practice, as well as with the socio-demographic characteristics of the patients registered with practices. Many of these characteristics of primary medical services are also associated with socio-economic deprivation in accordance with the 'inverse care law'. After adjusting for deprivation, social class and ethnicity, mortality indicators were strongly associated with the sociodemographic characteristics of registered populations but were less consistently associated with the characteristics of primary care services. We first describe the limitations of the study, and then discuss the interpretation of these findings.
The study has several limitations. First, the data represent routinely collected administrative data. The census derived data for deprivation, social class and proportion of ethnic minorities were collected in 1991 (data from the 2001 census not yet being available) and may not accurately reflect the true position in 1999. The same is true for the population denominators which were estimated from the 1991 census returns using well-established methods. When registered populations are considered, list inflation represents a further difficulty. The resulting misclassification may vary between areas, since deprived urban areas tend to have more mobile populations and to change in character more rapidly than stable rural areas. The general effect of this misclassification will be to reduce the magnitude of associations, but where confounders are misclassified the effect may not be readily predicted. Secondly, the analysis is ecological and the associations identified can only be expected to hold at the population level. Differing conclusions might result if the relationship between access to primary care and health were studied at the individual level. Thirdly, the data are cross-sectional and this makes the assessment of temporality impossible and possible causal relationships will be difficult to evaluate. A related problem is that reverse causality may be present, health may influence the distribution of primary care in addition to a potential effect of primary care on health. This problem can potentially be addressed through techniques such as instrumental variables regression which require a two stage model. 'Primary care' would be specified in the first stage and then used as a predictor in the second stage. However, this approach was considered to be beyond the scope of this analysis. Fourthly, as we have acknowledged in the Introduction, the problem of residual confounding may exist. This may be a particular problem in respect of the relationship between primary and secondary care. Better GP supply might be associated with better supply of hospital services. This possibility deserves further investigation but it is not clear what aspect of hospital supply might be important. For example, distinctions should be made between the availability of acute or elective care, and access to either public or privately provided care. However, primary care services appeared to be better organised in rural areas where geographical accessibility to hospital services may be less.
The relationships between socio-economic deprivation and health[15, 16]).) on the one hand, and socio-economic deprivation and supply and structure of primary medical services[2, 17] on the other, have been well documented. A possible relationship between access to primary medical services and population health has been less well investigated. After adjusting for socio-economic variables, the supply of primary care services is associated with population health indicators[8]. These associations might be explained either in terms of residual confounding with deprivation, or in terms of an effect of access to primary health care on population health. Gravelle and Sutton[2] note that the former explanation is likely to be important because general practitioners' decisions about location may be very sensitive to the quality of amenities in an area. In cross-sectional data, health measures may be viewed either as measures of need or outcome, and neither of the two alternative explanations can be ruled out. However, the nature of the associations identified offer some clues.
It was clear that the socio-demographic characteristics of patients registered with practices in an area were strongly associated with health measures. Areas where practices had more registered rural or older patients had better health after standardising for age. These areas are typically more affluent than urban areas with more youthful populations. The coefficient for the association between GP supply and all-cause mortality was reduced after additionally adjusting for the population socio-demographic variables. This finding suggests that the association between primary care access and health outcomes might be accounted for in terms of residual confounding with population health needs consequent on deprivation, because it can be anticipated that unmeasured confounders would also have an important effect. In contrast, the types of services provided by practices were generally not associated with population health measures. In particular, provision of diabetes services was not associated with hospital utilisation for chronic conditions, and provision of contraceptive services was not associated with teenage conceptions. However, these findings might be explained by the generally high levels of provision of these services (see Table 2). Baker and Hann[18], using PCG level data, found that services for diabetes and asthma were widely available. Variations in provision were not associated with an index of population need based on the Jarman score. Instead, there were geographical variations in provision, with the London region having lower coverage.
Our findings are generally consistent with Tudor Hart's 'inverse care law'. The strong associations between the socio-demographic characteristics of registered populations and mortality, and the lack of consistency or specificity in associations with the structure of primary care services suggest that residual confounding with wider socio-economic influences on health may be important. There is generally stronger evidence that better supply of general practice services is associated with altered patterns of emergency hospital utilisation, as has been noted by other authors [19, 20].
Following the work of McKeown[21], it is widely appreciated that medical care is a relatively weak influence on population health. Thus the Independent Inquiry into Inequalities in Health[15] made its major recommendations in respect of wider socio-economic and environmental influences on health including income, education, employment, housing, transport and nutrition rather than the organisation of health services. The immediate rationale for improving primary medical care in deprived areas is one of achieving equity of access to health care[22]. Improving health is only one objective, and arguably not the main objective, in providing access to health care. Nevertheless, modern medicine has become increasingly effective, and several authors have estimated that significant gains in life expectancy could be expected if known effective treatments were more widely applied [23, 24]. Uptake of effective interventions is less for lower socio-economic groups which have worse health outcomes in treatable conditions like acute myocardial infarction [25] or cancer [26]. There is therefore a convergence between the objectives of achieving equity of access and equity in health.
This model requires that the concept of 'access' is extended to include the relevance and effectiveness of services [27]. Indicators of primary care access which are based only on the supply and utilisation of services will be inadequate. Information about the coverage of the population at risk by effective interventions is also required. Some studies suggest that larger practices provide better quality care [28] and that this may be associated with reduced hospital utilisation [29] and better health outcomes. This might explain why the partnership size and proportion of single-handed practices were associated with health outcomes. However, other studies have suggested that single-handed practices provide satisfactory standards of care[30]. In order to answer the questions raised by this and other studies, future analyses should link data for the supply and utilisation of primary care services to individual-level data describing levels of risk and delivery of interventions in the form of effective treatment.
References
Hart JT: The inverse care law. Lancet. 1971, 1: 405-412.
Gravelle H, Sutton M: Inequality in the geographical distribution of general practitioners in England and Wales 1974–1995. J Health Serv Res Policy. 2001, 6: 6-13. 10.1258/1355819011927143.
Leese B, Bosanquet N: Change in general practice and its effects on service provision in areas with different socioeconomic characteristics. BMJ. 1995, 311: 546-550.
Stirling AM, Wilson P, McConnachie A: Deprivation, psychological distress, and consultation length in general practice. Br J Gen Pract. 2001, 51: 456-460.
Campbell SM, Hann M, Hacker J, Burns C, Oliver D, Thapar A, Mead N, Safran DG, Roland MO: Identifying predictors of high quality care in English general practice: observational study. BMJ. 2001, 323: 784-787. 10.1136/bmj.323.7316.784.
Shi L, Starfield B, Kennedy B, Kawachi I: Income inequality, primary care, and health indicators. J Fam Pract. 1999, 48: 275-284.
Shi L, Starfield B: The effect of primary care physician supply and income inequality on mortality among blacks and whites in US metropolitan areas. Am J Public Health. 2001, 91: 1246-1250.
Gulliford MC: Availability of primary care doctors and population health in England: is there an association?. J Public Health Med. 2002, 24: 252-254. 10.1093/pubmed/24.4.252.
Pereira Gray D: Primary care doctors and population health. J Public Health Medicine. 2003, 25: 272.
Department of Health: Tackling health inequalities: a programme for action. 2003, London, Department of Health
Department of Health: Quality and Performance in the NHS: High Level Performance and Clinical Indicators. 2001, London: Department of Health, accessed September 24th 2001, [http://www.performance.doh.gov.uk/nhsperformanceindicators/hlpi2000/arealist_h.html]
Department of Health: Compendium of clinical and health indicators 2000. Data definitions and user guide for computer files. September 2001 version. 2003, London: Department of Health and London School of Hygiene and Tropical Medicine
National Primary Care Research and Development Centre: The National Database for Primary Care Groups and Trusts. 2003, Manchester: National Primary Care Research and Development Centre, accessed 21st July 2003, [http://www.primary-care-db.org.uk/]
Charlton JR, Bauer R, Lakhani A: Outcome measures for district and regional health care planners. Community Med. 1984, 6: 306-315.
Acheson ED: Independent inquiry into inequalities in health. 1998, London: The Stationery Office
Townsend P, Whitehead M, Davidson N: Inequalities in health: the Black report and the health divide. 1992, London: Penguin Books
Tudor HJ: Commentary: three decades of the inverse care law. BMJ. 2000, 320: 18-19.
Baker D, Hann M: General practitioner services in primary care groups in England: is there inequity between service availability and population need?. Health Place. 2001, 7: 67-74. 10.1016/S1353-8292(00)00041-1.
Carlisle R, Groom LM, Avery AJ, Boot D, Earwicker S: Relation of out of hours activity by general practice and accident and emergency services with deprivation in Nottingham: longitudinal survey. BMJ. 1998, 316: 520-523.
Jarman B, Gault S, Alves B, Hider A, Dolan S, Cook A, Hurwitz B, Iezzoni LI: Explaining differences in English hospital death rates using routinely collected data. BMJ. 1999, 318: 1515.
Mckeown T: The role of medicine. 1979, Oxford: Blackwell
Gulliford MC: Equity and access to health care. In Access to health care. Edited by: Gulliford MC, Morgan M. 2003, London: Routledge, 36-60.
Bunker JP, Frazier HS, Mosteller F: Improving health: measuring effects of medical care. Milbank Q. 1994, 72: 225-258.
Wald NJ, Law MR: A strategy to reduce cardiovascular disease by more than 80%. BMJ. 2003, 326: 1419-10.1136/bmj.326.7404.1419.
Morrison C, Woodward M, Leslie W, Tunstall-Pedoe H: Effect of socioeconomic group on incidence of, management of, and survival after myocardial infarction and coronary death: analysis of community coronary event register. BMJ. 1997, 314: 541.
Coleman MP, Babb P, Sloggett A, Quinn M, De Stavola B: Socioeconomic inequalities in cancer survival in England and Wales. Cancer. 2001, 91 (1 Suppl): 208-16. 10.1002/1097-0142(20010101)91:1+<208::AID-CNCR6>3.0.CO;2-E.
Gulliford M, Figueroa-Munoz J, Morgan M, Hughes D, Gibson D, Beech R, Hudson M: What does 'access to health care' mean?. J Health Serv Res Policy. 2002, 7: 186-188. 10.1258/135581902760082517.
Campbell SM, Hann M, Hacker J, Burns C, Oliver D, Thapar D, Mead N, Safran DG, Roland MO: Identifying predictors of high quality care in English general practice: observational study. BMJ. 2001, 323: 784-787. 10.1136/bmj.323.7316.784.
Griffiths C, Sturdy P, Naish J, Omar R, Dolan S, Feder G: Hospital admissions for asthma in East London: associations with characteristics of local general practices, prescribing and population. BMJ. 1997, 314: 482-486.
Hippisley-Cox J, Pringle M, Coupland C, Hammersley V, Wilson A: Do single handed practices offer poorer care? Cross sectional survey of processes and outcomes. BMJ. 2001, 323: 320-323. 10.1136/bmj.323.7308.320.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6963/4/12/prepub
Acknowledgement
The National Database for Primary Care Groups and Trusts is a product of the National Primary Care Research and Development Centre at the University of Manchester. It was devised by Dr Deborah Baker, who is the database director. The database was constructed by Justin Hayes at the Regional Research Laboratory, School of Geography, University of Manchester (Director: Dr Robert Barr); SEE IT consultancy designed and built the map interface. We are grateful to Andrew Wagner, Mark Hann and David Reeves (NPCRDC) for their considerable hard work in cleaning and validating the data sets. Andrew Wagner is the database manager (a.wagner@man.ac.uk).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Gulliford, M.C., Jack, R.H., Adams, G. et al. Availability and structure of primary medical care services and population health and health care indicators in England. BMC Health Serv Res 4, 12 (2004). https://doi.org/10.1186/1472-6963-4-12
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6963-4-12