Abstract
Background
By measuring the quality of the organisation of palliative care with process and structure quality indicators (QIs), patients, caregivers and policy makers are able to monitor to what extent recommendations are met, like those of the council of the WHO on palliative care and guidelines. This will support the implementation of public programmes, and will enable comparisons between organisations or countries.
Methods
As no European set of indicators for the organisation of palliative care existed, such a set of QIs was developed. An update of a previous systematic review was made and extended with more databases and grey literature. In two project meetings with practitioners and experts in palliative care the development process of a QI set was finalised and the QIs were categorized in a framework, covering the recommendations of the Council of Europe.
Results
The searches resulted in 151 structure and process indicators, which were discussed in steering group meetings. Of those QIs, 110 were eligible for the final framework.
Conclusions
We developed the first set of QIs for the organisation of palliative care. This article is the first step in a multi step project to identify, validate and pilot QIs.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Following the 2002 definition of the World Health Organisation (WHO), palliative care is no longer restricted to patients with cancer; it should be available for all patients with life-threatening diseases [1]. Furthermore, palliative care is applicable early in the course of the disease and can be delivered in conjunction with interventions that aim to prolong life. Palliative care needs a team approach in order to relieve not only pain and other somatic symptoms but also to provide multi-dimensional care including psychosocial and spiritual care and support for patients and their proxies. This wider definition implies an increase of the number of patients eligible for palliative care. Due to successful medical interventions, the aging population and improved survival of patients with chronic diseases or with cancer, the demand for palliative care will increase too [2, 3].
In 2003, the Council of Europe launched recommendations for the organisation of palliative care regarding settings and services, policy and organisation, quality improvement and research, education and training, family, communication with the patient and family, teams and bereavement. This included further cooperation between European countries [4]. As most scientific studies focus on clinical outcomes, it is unclear whether these recommendations and the WHO definition have been implemented in the organisation of palliative care in Europe. By measuring the quality of the organisation of palliative care, patients, caregivers and policy makers can monitor whether in their country, specific settings and networks for palliative care meet the recommendations of the council of Europe and of the WHO. This information would give better insight, which is needed for the measurement of the impact of palliative care programs [5].
A valid and reliable method for assessing the quality of the organisation of care is the use of structure and process quality indicators (QIs). QIs are ‘explicitly defined and measurable items referring to the outcomes, processes or structure of care’ [6, 7]. In a systematic review published in 2009, clinical indicators appeared to be widely overrepresented over indicators that assess organisational issues of palliative care, and most QIs were developed in and for one specific country or setting [8].
Therefore, we aimed to develop a scientifically sound European set of structure and process QIs, as a first step in quality measurement and improvement.
Methods
The study, undertaken by partners from seven collaborating countries (Belgium, United Kingdom, France, Germany, Netherlands, Poland and Spain), ran from October 2007 till September 2010 [9]. It was co-funded by the European Executive Agency for Health and Consumers (EAHC).
QI sets can be based on existing sets of QIs, recommendations from clinical guidelines, scientific literature, best practice or expert consensus [6]. We used a combination of these.
As palliative care, being a relatively young field within health care is changing rapidly. The initial phase of this project was an update and extension of a previous review aiming to find already existing QIs in literature or aspects of the organisation of the palliative care for which QIs would be useful [8]. QIs were operationalized as ‘measurable items referring to the outcomes, processes or structure of care’ [6, 7]. Organisation of palliative care was defined as ‘systems to enable the delivery of good quality in palliative care’, which made us focus on processes and structures [7]. Besides publications that describe the development or use of QIs for the organisation of palliative care, publications were used that describe the structure or process of good palliative care, in order to develop QIs if not available yet.
Main database search
As an update and extension of an existing systematic review, the following bibliographic databases were searched: Medline, Scopus, PsycINFO, Social Medicine, CINAHL, the Cochrane Database, Embase, SIGLE, ASCO, and Google Scholar by an existing search strategy (Additional file 1: Appendix A) [8]. If applicable, Mesh terms were changed, as these are database-specific.
Inclusion criteria were a publication period from December 2007 to May 2009, as the systematic review ran until December 2007 and containing information about the development or use of (sets of) QIs.
Papers describing QIs about palliative care for children, clinical outcome indicators, patient outcome and on treatment were excluded, as well as scientific papers that were not written in English.
The initial selection process was based on independent screening by three researchers of title and/or abstract, followed by a selection based on full text. Additionally, reference lists of obtained papers were studied and hand searches were performed (Current Opinion in Supportive and Palliative Care, Journal of Pain and Symptom Management, Palliative Medicine and Quality and Safety in Health Care Journal).
The QIs derived from the search were categorized in a framework. It was based on (1) a previously developed framework for evalution of the organisation of general practice and adapted for palliative care and (2) the recommendations of the Council of Europe [4, 10]. It contains the domains 1. Definition of a palliative care service, 2. Access to palliative care, 3. Infrastructure, 4. Assessment tools, 5. Personnel, 6. Documentation of clinical data, 7. Quality and safety issues, 8. Reporting clinical activity of palliative care, 9. Research and 10. Eduation.
Grey literature search
If a domain or subdomain of the framework was not covered with QIs found in the literature search, an additional grey literature search was performed. Grey literature was defined as ‘literature which has not been formally published in peer- reviewed literature’ [11]. Inclusion of grey literature was restricted to reports from government agencies or scientific research groups, white papers and websites from national organisations of the seven participating countries. Finally, the network of the Europall research group was used to identify relevant papers.
Methods of screening and article selection
The steering group of the Europall project planned two meetings in September and October 2009 with all project members (Additional file 1: Appendix B).
QI selection
The draft set of structure and process QIs was discussed during the first steering group meeting in September 2009. Academic experts from several disciplines in palliative care, all from one of the seven participating European countries were invited. Consensus was based on 1. whether it considered a process or structure QI 2. whether it overlapped with other proposed QIs, 3. to which domain of the framework (Table 1) it belonged [10] and 4. for which settings it was applicable. Based on the grey literature search, the project partners could suggest new QIs about aspects that were relevant but not yet operationalised as QIs.
-
3.
Based on this meeting, adaptations were made and a new draft QI set was presented in the second steering group meeting in October.
Results
Search flow
The literature search resulted in 541 papers, including a previous systematic review on quality indicators for palliative care [8]. Most of the papers came from the database search (n=527), followed by the hand search (n= 29) and least of grey literature search (n=14).
In the screening process 16 duplicates were identified, and titles and abstracts of 511 papers were searched. Of these, 389 documents were excluded, as they did not contain QIs. Full papers were obtained of 122 publications, from which 63 papers were included; 57 resulting from the database search [12–68] and another six papers from the additional hand searches (Figure 1) [69–74].
Results grey literature search
The grey literature search yielded seven papers, deriving from Belgium, the Netherlands and the UK [9, 75–80]. These sources included government sites, national health organisations and national institutes (Figure 1). This additional search resulted in the development of 53 QIs, divided over almost all domains (see Additional file 1).
QI development
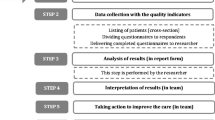
Sixhundred-thirtyfive QIs were derived from this literature review. After screening of duplicates, selecting process and structure QIs and combining QIs covering the same topic, the remaining 151 QIs were organised in the framework and discussed in the first steering group meeting. The two steering group meetings resulted in a reduction from 151 to 110 QIs (Additional file 1: Appendix C) (Figure 2). For instance the domain about finance QIs was excluded for the final set as the QIs were more useful on national level than in the setting specific palliative care institutions.
The rest of the QIs were distributed over the framework (Table 1) [10].
The majority of the 110 QIs were process QIs (n=76), the other structure QIs (n=34). Some of the QIs (n=24) were only applicable in specific settings; ten in primary care, thirteen in inpatient settings and one in home care. The others were meant for all settings that deliver palliative care.
Twenty-four QIs were developed based on organisational aspects found in literature (Table 1, QI 51). Finally, several QIs (n= 86), were changed in their presentation of text during the procedure. For example, originally developed QIs for other settings like the intensive care unit, were adapted to make them appropriate for palliative care settings.
Discussion
We were able to develop an international framework with 110 QIs to assess the organisation of palliative care in several kind of settings. To our knowledge, this study presents the first systematically developed international set of QIs on this topic. Part of the QIs are setting specific, whereas others will be applicable in all kind of settings that deliver palliative care.
Where Pasman et al. performed a systematic review on all kind of QIs for palliative care, and Pastrana et al. focused on outcome indicators for Germany, we focused on process and structure QIs [8, 81]. By using an international perspective and by not limiting the study to symptom control, our study follows the recommendations of Ostgathe et al. [82]. Our set also contains two QIs that are linked to the World Health Assembly’s proposed global health indicator ‘Access to palliative care assessed by morphine-equivalent consumption of strong opioid analgesia (excluding methadone) per death by cancer’, but without the restriction to patients with cancer [83].
Strength and limitations
We chose an approach with several consecutive methodological steps to develop a set of QIs. Of those aspects that were considered important for the organisation of palliative care but of which no QIs could be found, we developed QIs ourselves [84]. Of those QIs that were developed for a restricted group of patients or setting (e.g. ICU or vulnerable elderly) we checked whether we could rephrase them into QIs for more types of settings or palliative patients. Defining QIs in a consensus procedure is a good option if scientific literature is not yet available [7], particularly because it combines several methods to improve validity. Using a group approach has the advantage that participants can share their expertise and experience. Groups often make better decisions than individuals [85].
The naming of QIs as process or structure indicators can be discussed. Yet, this only influences the categorisation and not the content, importance or use of a QI.
Another strong aspect of our procedure is the inclusion of grey literature, which created the possibility to include documents from important although not scientific sources [86].
As the Europall project was a collaboration of seven European countries, only experts of these countries were represented in the steering group meetings. Other European countries, with different health care and financing systems, cultures and palliative care, were not involved at this stage.
This first step resulted in a set of structure and process QIs, that can help professionals or settings to measure the quality of care of their setting. In a next step, a subset will be developed of which each QI is applicable in the seven participating countries.
Based on a modified RAND Delphi method the following set will be interesting for international comparison. The advantage of this comprehensive set enables each country and each setting the opportunity to see all QIs that are available on this topic.
The last step will describe a pilot study to test the set of QIs on face-validity, applicability and discriminative power. This includes almost all (26) European countries. These studies will be published separately.
Further research
The final set can be used to provide feedback to settings or countries to reflect on their performance, for supporting quality improvement activities, accreditation, research, and enhancing transparency about quality. They can be used to evaluate the implementation of the WHO definition and the recommendations of the council of Europe [1, 4].
From 2011 to 2015, a follow-up project to Europall called IMPACT (funded by the EU 7th framework) will develop and test strategies to implement these QIs.
Conclusions
This review resulted in the first comprehensive framework of QIs for the organisation of palliative care.
References
WHO: Definition of Palliative Care. [http://www.who.int/cancer/palliative/definition/en/]
10 facts on ageing and the life course. [http://www.who.int/features/factfiles/ageing/en/index.html]
What are the public health implications of global ageing?. [http://www.who.int/features/qa/42/en/index.html]
Recommendation Rec (2003) 24 of the Committee of Ministers to member states on the organisation of palliative care. [http://www.coe.int/t/dg3/health/Source/Rec(2003)24_en.pdf]
Smith TJ, Hillner BE: Ensuring quality cancer care by the use of clinical practice guidelines and critical pathways. J Clin Oncol. 2001, 19: 2886-2897.
Campbell SM, Ludt S, Van Lieshout J, Boffin N, Wensing M, Petek D, Grol R, Roland MO: Quality indicators for the prevention and management of cardiovascular disease in primary care in nine European countries. Eur J Cardiovasc Prev Rehabil. 2008, 15: 509-515. 10.1097/HJR.0b013e328302f44d.
Campbell SM, Braspenning J, Hutchinson A, Marshall MN: Research methods used in developing and applying quality indicators in primary care. BMJ. 2003, 326: 816-819. 10.1136/bmj.326.7393.816.
Pasman HRW, Brandt HE, Deliens L, Francke AL: Quality indicators for palliative care: a systematic review. J Pain Symptom Manage. 2009, 38: 145-156. 10.1016/j.jpainsymman.2008.07.008.
Europall Project. [http://www.europall.eu/]
Engels Y, Campbell S, Dautzenberg M, van den Hombergh P, Brinkmann H, Szecsenyi J, Falcoff H, Seuntjens L, Kuenzi B, Grol R: Developing a framework of, and quality indicators for, general practice management in Europe. Fam Pract. 2005, 22: 215-222. 10.1093/fampra/cmi002.
Cook AM, Finlay IG, Edwards AG, Hood K, Higginson IJ, Goodwin DM, Normand CE, Douglas HR: Efficiency of searching the grey literature in palliative care Journal of Pain and Symptom Management. 2001, 22: 797-801.
Aa Petersen M, Pedersen L, Groenvold M: Does the agreement of patient and physician assessments of health related quality of life in palliative care depend on patient characteristics?. Palliat Med. 2007, 21: 289-294. 10.1177/0269216307077694.
ASCO-ESMO: Consensus statement on quality cancer care. J Clin Oncol. 2010, 24: 3498-3499.
Becker G, Sarhatlic R, Olschewski M, Xander C, Momm F, Blum HE: End-of-life care in hospital: current practice and potentials for improvement. J Pain Symptom Manage. 2007, 33: 711-719. 10.1016/j.jpainsymman.2006.09.030.
Bottomley A: The journey of health-related quality of life assessment. Lancet Oncol. 2008, 9: 906-10.1016/S1470-2045(08)70233-X.
Brumley R, Enguidanos S, Jamison P, Seitz R, Morgenstern N, Saito S, McIlwane J, Hillary K, Gonzalez J: Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc. 2007, 55: 993-1000. 10.1111/j.1532-5415.2007.01234.x.
Casarett D, Pickard A, Bailey FA, Ritchie C, Furman C, Rosenfeld K, Shreve S, Chen Z, Shea JA: Do palliative consultations improve patient outcomes?. J Am Geriatr Soc. 2008, 56: 593-599. 10.1111/j.1532-5415.2007.01610.x.
Delgado-Guay MO, Parsons HA, Li Z, Palmer LJ, Bruera E: Symptom distress, interventions, and outcomes of intensive care unit cancer patients referred to a palliative care consult team. Cancer. 2009, 115: 437-445. 10.1002/cncr.24017.
Demiris G, Oliver DP, Wittenberg-Lyles E: Assessing caregivers for team interventions (ACT): a new paradigm for comprehensive hospice quality care. Am J Hosp Palliat Care. 2009, 26: 128-134. 10.1177/1049909108328697.
Dixon BK: Quality measures crafted for palliative. Hospice Medicine. Family Practice News. 2007, 37: 6.
Dougherty E, Pierce B, Ma C, Panzarella T, Rodin G, Zimmermann C: Factors associated with work stress and professional satisfaction in oncology staff. Am J Hosp Palliat Care. 2009, 26: 105-111. 10.1177/1049909108330027.
Dy SM, Shugarman LR, Lorenz KA, Mularski RA, Lynn J, for the RAND—Southern California Evidence-Based Practice Center: A systematic review of satisfaction with care at the end of life. J Am Geriatr Soc. 2008, 56: 124-129. 10.1111/j.1532-5415.2007.01507.x.
Gelfman LP, Meier DE, Morrison RS: Does palliative care improve quality? A survey of bereaved family members. J Pain Symptom Manage. 2008, 36: 22-28. 10.1016/j.jpainsymman.2007.09.008.
Gomez-Batiste X, Fontanals MD, Roca J, Borras JM, Viladiu P, Stjernsward J, Rius E: Catalonia WHO demonstration project on palliative care implementation 1990–1995: results in 1995. J Pain Symptom Manage. 1996, 12: 73-78. 10.1016/0885-3924(96)00074-7.
Granda-Cameron C, Viola SR, Lynch MP, Polomano RC: Measuring patient-oriented outcomes in palliative care: functionality and quality of life. Clin J Oncol Nurs. 2008, 12: 65-77. 10.1188/08.CJON.65-77.
Gries CJ, Curtis JR, Wall RJ, Engelberg RA: Family member satisfaction with end-of-life decision making in the ICU. Chest. 2008, 133: 704-712. 10.1378/chest.07-1773.
Griffin JP, Koch KA, Nelson JE, Cooley ME: Palliative care consultation, quality-of-life measurements, and bereavement for end-of-life care in patients with lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 2007, 132: 404S-422S. 10.1378/chest.07-1392.
Grunfeld E, Lethbridge L, Dewar R, Lawson B, Paszat LF, Johnston G, Burge F, McIntyre P, Earle CC: Towards using administrative databases to measure population-based indicators of quality of end-of-life care: testing the methodology. Palliat Med. 2006, 20: 769-777. 10.1177/0269216306072553.
Hanratty B, Holland P, Jacoby A, Whitehead M: Financial stress and strain associated with terminal cancer–a review of the evidence. Palliat Med. 2007, 21: 595-607. 10.1177/0269216307082476.
Hicks F, Rees E: A ‘pain-free‘ death. Br Med Bull. 2008, 88: 23-41. 10.1093/bmb/ldn043.
Irwin SA, Zurhellen CH, Diamond LC, Dunn LB, Palmer BW, Jeste DV, Twamley EW: Unrecognised cognitive impairment in hospice patients: a pilot study. Palliat Med. 2008, 22: 842-847. 10.1177/0269216308096907.
Jarabek BR, Jama AA, Cha SS, Ruegg SR, Moynihan TJ, McDonald FS: Use of a palliative care order set to improve resident comfort with symptom management in palliative care. Palliat Med. 2008, 22: 343-349. 10.1177/0269216308090169.
Jordhoy MS, Inger Ringdal G, Helbostad JL, Oldervoll L, Loge JH, Kaasa S: Assessing physical functioning: a systematic review of quality of life measures developed for use in palliative care. Palliat Med. 2007, 21: 673-682. 10.1177/0269216307083386.
Jünger S, Pestinger M, Elsner F, Krumm N, Radbruch L: Criteria for successful multiprofessional cooperation in palliative care teams. Palliat Med. 2007, 21: 347-354. 10.1177/0269216307078505.
Kairuz TE, Gargiulo D, Bunt C, Garg S: Quality, safety and efficacy in the ‘off-label‘ use of medicines. Curr Drug Saf. 2007, 2: 89-95. 10.2174/157488607779315471.
Kapo J, Morrison LJ, Liao S: Palliative care for the older adult. J Palliat Med. 2007, 10: 185-209. 10.1089/jpm.2006.9989.
Kim Y, Given BA: Quality of life of family caregivers of cancer survivors: across the trajectory of the illness. Cancer. 2008, 112: 2556-2568. 10.1002/cncr.23449.
Le BHC, Ashby MA: Audit of deaths and palliative care referrals in a large Australian teaching hospital. J Palliat Med. 2007, 10: 835-836. 10.1089/jpm.2007.0034.
Leonard M, Agar M, Mason C, Lawlor P: Delirium issues in palliative care settings. J Psychosom Res. 2008, 65: 289-298. 10.1016/j.jpsychores.2008.05.018.
Lorenz K: Progress in measuring and improving palliative and end-of-life quality. J Palliat Med. 2008, 11: 682-684. 10.1089/jpm.2008.9906.
Mayadev AS, Weiss MD, Distad BJ, Krivickas LS, Carter GT: The amyotrophic lateral sclerosis center: a model of multidisciplinary management. Phys Med Rehabil Clin N Am. 2008, 19: 619-631. 10.1016/j.pmr.2008.04.004.
McNiff KK, Neuss MN, Jacobson JO, Eisenberg PD, Kadlubek P, Simone JV: Measuring supportive care in medical oncology practice: lessons learned from the quality oncology practice initiative. J Clin Oncol. 2008, 26: 3832-3837. 10.1200/JCO.2008.16.8674.
Meraviglia M, Sutter R, Gaskamp CD: Providing spiritual care to terminally ill older adults. J Gerontol Nurs. 2008, 34: 8-14.
Miller SC, Kiely DK, Teno JM, Connor SR, Mitchell SL: Hospice care for patients with dementia: does volume make a difference?. J Pain Symptom Manage. 2008, 35: 283-291. 10.1016/j.jpainsymman.2007.12.001.
Miyashita M, Nakamura A, Morita T, Bito S: Identification of quality indicators of end-of-life cancer care from medical chart review using a modified Delphi method in Japan. Am J Hosp Palliat Care. 2008, 25: 33-38. 10.1177/1049909107307376.
Norton SA, Hogan LA, Holloway RG, Temkin-Greener H, Buckley MJ, Quill TE: Proactive palliative care in the medical intensive care unit: effects on length of stay for selected high-risk patients. Crit Care Med. 2007, 35: 1530-1535. 10.1097/01.CCM.0000266533.06543.0C.
van der Ploeg E, Depla MFIA, Shekelle P, Rigter H, Mackenbach JP: Developing quality indicators for general practice care for vulnerable elders; transfer from US to The Netherlands. Qual Saf Health Care. 2008, 17: 291-295. 10.1136/qshc.2007.023226.
Pronost A, Le Gouge ALD: The effects of various features of haematology-oncology services using the palliative approach and the socio-demographic characteristics of healthcare providers on health indicators: social support, perceived stress, coping strategies, quality of life at work. Oncology. 2008, 10: 125-134. 10.1007/s10269-007-0775-1.
Quill TE: Is length of stay on hospice a critical quality of care indicator?. J Palliat Med. 2007, 10: 290-292. 10.1089/jpm.2006.9984.
Ripamonti CI: Malignant bowel obstruction: tailoring treatment to individual patients. J Support Oncol. 2008, 6: 114-115.
Robinson C, Pesut B, Bottorff J, Mowry A, Broughton S, Fyles G: Rural palliative care: a comprehensive review. J Palliat Med. 2009, 12: 253-258. 10.1089/jpm.2008.0228.
Rokoske FS, Schenck AHL: Developing Quality Measures for Hospice and Palliative Care. Gerontologist. 2008, 48: 691.
Sampson EL, Thune-Boyle I, Kukkastenvehmas R, Jones L, Tookman A, King M, Blanchard MR: Palliative care in advanced dementia; A mixed methods approach for the development of a complex intervention. BMC Palliat Care. 2008, 7: 8-10.1186/1472-684X-7-8.
Sato K, Miyashita M, Morita T, Sanjo M, Shima Y, Uchitomi Y: Reliability assessment and findings of a newly developed quality measurement instrument: quality indicators of end-of-life cancer care from medical chart review at a Japanese regional cancer center. J Palliat Med. 2008, 11: 729-737. 10.1089/jpm.2007.0227.
Sela RA: Screening for depression in palliative cancer patients attending a pain and symptom control clinic. Palliat Support Care. 2007, 5: 207-217.
Slaven M, Wylie N, Fitzgerald B, Henderson N, Taylor S: Who needs a palliative care consult?: the Hamilton Chart Audit tool. J Palliat Med. 2007, 10: 304-307. 10.1089/jpm.2006.0237.
Smith AK, McCarthy EP, Paulk E, Balboni TA, Maciejewski PK, Block SD, Prigerson HG: Racial and ethnic differences in advance care planning among patients with cancer: impact of terminal illness acknowledgment, religiousness, and treatment preferences. J Clin Oncol. 2008, 26: 4131-4137. 10.1200/JCO.2007.14.8452.
van der Steen JT, Mitchell SL, Frijters DHM, Kruse RL, Ribbe MW: Prediction of 6-month mortality in nursing home residents with advanced dementia: validity of a risk score. J Am Med Dir Assoc. 2007, 8: 464-468. 10.1016/j.jamda.2007.05.004.
Tei Y, Morita T, Nakaho T, Takigawa C, Higuchi A, Suga A, Tajima T, Ikenaga M, Higuchi H, Shimoyama N, Fujimoto M: Treatment efficacy of neural blockade in specialized palliative care services in Japan: a multicenter audit survey. J Pain Symptom Manage. 2008, 36: 461-467. 10.1016/j.jpainsymman.2007.11.009.
Teno JM, Connor SR: Referring a patient and family to high-quality palliative care at the close of “life: “We met a new personality… with this level of compassion and empathy“. JAMA. 2009, 301: 651-659. 10.1001/jama.2009.109.
Teunissen SCCM, Verhagen EH, Brink M, van der Linden BA, Voest EE, de Graeff A: Telephone consultation in palliative care for cancer patients: 5 years of experience in The Netherlands. Support Care Cancer. 2007, 15: 577-582. 10.1007/s00520-006-0202-y.
Torres-Vigil I, Aday LA: Health care providers‘ assessments of the quality of advanced-cancer care in Latin American medical institutions: a comparison of predictors in five countries: Argentina, Brazil, Cuba, Mexico, and Peru. J Pain Palliat Care Pharmacother. 2008, 22: 7-20. 10.1080/15360280801989195.
Tsai LY, Li IF, Liu CP, Su WH, Change TY: Application of quality audit tools to evaluate care quality received by terminal cancer patients admitted to a palliative care unit. Support Care Cancer. 2008, 16: 1067-1074. 10.1007/s00520-007-0365-1.
Tuffrey-Wijn I, Hogg JCL: End-of-life and palliative care for people with intellectual disabilities who have cancer or other life-limiting illness: a review of the literature and available resources. J Appl Res Intellect Disabil. 2007, 20: 331-344. 10.1111/j.1468-3148.2006.00350.x.
Walling A, Lorenz KA, Dy SM, Naeim A, Sanati H, Asch SM, Wenger NS: Evidence-based recommendations for information and care planning in cancer care. J Clin Oncol. 2008, 26: 3896-3902. 10.1200/JCO.2007.15.9509.
Wenig LC, Huang HL, Wilkie DJ, Hoenig NA, Suarez ML, Marschke M, Durham J: Predicting survival with the palliative performance scale in a minority-serving hospice and palliative care program. J Pain Symptom Manage. 2009, 37: 642-648. 10.1016/j.jpainsymman.2008.03.023.
Yao CA, Hu WY, Lai YF, Cheng SY, Chen CY, Chiu TY: Does dying at home influence the good death of terminal cancer patients?. J Pain Symptom Manage. 2007, 34: 497-504. 10.1016/j.jpainsymman.2007.01.004.
Zib M, Saul P: A pilot audit of the process of end-of-life decision-making in the intensive care unit. Crit Care Resusc. 2007, 9: 213-218.
Costantini M: Editorial: place of death. It is time for a change of gear. Palliat Med. 2008, 22: 785-786. 10.1177/0269216308096424.
Dudgeon DJ, Knott C, Eichholz M, Gerlach JL, Chapman C, Viola R, Van Dijk J, Preston S, Batchelor D, Bartfay E: Palliative Care Integration Project (PCIP) quality improvement strategy evaluation. J Pain Symptom Manage. 2008, 35: 573-582. 10.1016/j.jpainsymman.2007.07.013.
Glasgow JL, McLennan SR, High KJ, Celi LAG: Quality of dying in a New Zealand teaching hospital. Qual Saf Health Care. 2008, 17: 244-248. 10.1136/qshc.2007.024745.
Luthy C, Cedraschi C, Pautex S, Rentsch D, Piguet V, Allaz AF: Difficulties of residents in training in end-of-life care. A qualitative study. Palliat Med. 2009, 23: 59-65.
Rayner L, Loge JH, Wasteson E, Higginson IJ: The detection of depression in palliative care. Curr Opin Support Palliat Care. 2009, 3: 55-60. 10.1097/SPC.0b013e328326b59b.
Zaider T, Kissane D: The assessment and management of family distress during palliative care. Curr Opin Support Palliat Care. 2009, 3: 67-71. 10.1097/SPC.0b013e328325a5ab.
Externe indicatoren voor pijn bij kanker. [http://www.zichtbarezorg.nl/mailings/FILES/htmlcontent/Ziekenhuizen/New%202e%20tranche/Pijn%20bij%20kanker%20defnew%20incl%20wijzigingen%20nav%20autorisatie.pdf]
Klinische kwaliteitsindicatoren. Objective Elements - Communication (OEC). Brussel: Federaal Kenniscentrum voor de gezondheidszorg (KCE). [https://kce.fgov.be/sites/default/files/page_documents/d20061027343.pdf]
Improving Supportive and Palliative Care for Adults National Institute for Clinical Excellence with Cancer. [http://www.nice.org.uk/nicemedia/live/10893/28816/28816.pdf]
Plan van Aanpak Palliatieve Zorg. 2008, [http://www.palliatief.nl/LinkClick.aspx?fileticket=yX68iRdBUjw%3d&tabid=3997&mid=10542] –2010
Quality and outcomes framework. [http://www.paymodernisation.scot.nhs.uk/gms/quality/docs/QualOutFrame0804.pdf]
Studie inzake de ontwikkeling van een registratie-instrument voor palliatieve zorg. [http://www.palliatief.be/accounts/143/attachments/Research/studie_registratie-instrument_pz_def.versie.pdf]
Pastrana T, Radbruch L, Nauck F, Hover G, Fegg M, Pestinger M, Ross J, Krumm N, Ostgathe C: Outcome indicators in palliative care–how to assess quality and success. Focus group and nominal group technique in Germany. Support Care Cancer. 2010, 18: 859-868. 10.1007/s00520-009-0721-4.
Ostgathe C, Voltz R: Quality indicators in end-of-life care. Curr Opin Support Palliat Care. 2010, 4: 170-173. 10.1097/SPC.0b013e32833add10.
Payne S, Leget C, Peruselli C, Radbruch L: Quality indicators for palliative care: debates and dilemmas. Palliat Med. 2012, 26: 679-680. 10.1177/0269216312450123.
Claessen S, Francke A, Belarbi H, Pasman H, van der Putten M, Deliens L: A new set of quality indicators for palliative care: process and results of the development trajectory. J Pain Symptom Manage. 2011, 42: 169-182. 10.1016/j.jpainsymman.2010.10.267.
Mrowietz U, Kragballe K, Reich K, Spuls P, Griffiths C, Nast A, Franke J, Antoniou C, Arenberger P, Balieva F, Bylaite M, Correia O, Dauden E, Gisondi P, Iversen L, Kemeny L, Lahfa M, Nijsten T, Rantanen T, Reich A, Rosenbach T, Segaert S, Smith C, Talme T, Volc-Platzer B, Yawalkar N: Definition of treatment goals for moderate to severe psoriasis: a European consensus. Arch Dermatol Res. 2010, 303: 1-10.
Genet N, Boerma WG, Kringos DS, Bouman A, Francke AL, Fagerstrom C, Melchiorre MG, Greco C, Deville W: Home care in Europe: a systematic literature review. BMC Health Service Research. 2011, 11: 207-10.1186/1472-6963-11-207.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6963/12/381/prepub
Acknowledgements
The authors are grateful to the EAHC (Executive Agency for Health and Consumers) for funding the Europall project. We would like to thank Hristina Mileva from EAHC specifically for her help and support. Further our thanks also go to the many individuals and organisations in the seven countries that contributed information to the project. We are especially grateful to all those who shared their views with us.
Belgium: Johan Menten
England: Sam Ahmedzai, Bill Noble
France: Jean-Christophe Mino
Germany: Eberhard Klaschik, Birgit Jaspers
Poland: Wojciech Leppert, Sylwia Dziegielewska
Spain: Xavier Gomez Batiste Alentorn, Silvia Paz, Marisa Martinez Munoz
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interest
This work was partly funded by EAHC (Executive Agency for Health and Consumers, grant: 2006111 PPP ‘Best practices in palliative care’). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors have no financial disclosures.
Authors' contributions
KvB participated in the literature search, design of the study and drafted the manuscript. NA participated in the literature search, design of the study and drafted the manuscript. JH participated in the literature search, design of the study and drafted the manuscript. JMM was actively involved in the selection and developmental process of the QI. She attended the expert meeting. IC was actively involved in the selection and developmental process of the QI. She attended the expert meeting. LR and helped to draft the manuscript and had an advisory role. KV conceived of the study and participated in its design and coordination and helped to draft the manuscript. YE conceived of the study and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
12913_2011_2333_MOESM1_ESM.doc
Additional file 1: Supplementary online content. Development of a set of process and structure indicators for palliative care: the Europall project. Appendix A- Search strategies for databases. Appendix B- Project partners. Appendix C- Indicators set for the organisation of palliative care. (DOC 252 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Woitha, K., Van Beek, K., Ahmed, N. et al. Development of a set of process and structure indicators for palliative care: the Europall project. BMC Health Serv Res 12, 381 (2012). https://doi.org/10.1186/1472-6963-12-381
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6963-12-381