Abstract
Background
Clinical practice guidelines have been developed aiming to improve the quality of care. The implementation of the computerized clinical guidelines (CCG) has been supported by the development of computerized clinical decision support systems.
This systematic review assesses the impact of CCG on the process of care compared with non-computerized clinical guidelines.
Methods
Specific features of CCG were studied through an extensive search of scientific literature, querying electronic databases: Pubmed/Medline, Embase and Cochrane Controlled Trials Register. A multivariable logistic regression was carried out to evaluate the association of CCG's features with positive effect on the process of care.
Results
Forty-five articles were selected. The logistic model showed that Automatic provision of recommendation in electronic version as part of clinician workflow (Odds Ratio [OR]= 17.5; 95% confidence interval [CI]: 1.6-193.7) and Publication Year (OR = 6.7; 95%CI: 1.3-34.3) were statistically significant predictors.
Conclusions
From the research that has been carried out, we can conclude that after implementation of CCG significant improvements in process of care are shown. Our findings also suggest clinicians, managers and other health care decision makers which features of CCG might improve the structure of computerized system.
Similar content being viewed by others
Background
Clinical practice guidelines have been developed to improve the quality of care, patient access, treatment outcomes, appropriateness of care and achieve cost containment by improving the cost benefit ratio [1–4].
At the same time many healthcare organizations have widely promoted the development of computerized clinical decision support systems (CDSS) with the aim of improving practitioners' performance [5–7].
According to the indications of regulatory systems, professional bodies and consumer organizations, CDSS can also support the implementation of the computerized clinical guidelines (CCG) [8].
An effective model of CCG consists of computer accessibility, patient-specific reminders in the clinician's workflow and its integration with medical records, as demonstrated by Wang et al. [9].
Even though different studies in literature are focused on demonstrating that CDSS can have an impact on physicians' behaviour regarding to patients' care [6, 10–12], there are very little evidence about the effectiveness of electronic guidelines [13–15] and impact of computerized support on implementing of clinical recommendations. In a qualitative systematic review, Shiffman et al. [13] highlighted higher effect of CCG versus non-electronic systems. Due to the lack of studies containing quantitative evaluation, research was focused on a systematic review of available literature about the impact of CCG upon the process of care compared with non-computerized clinical guidelines (NCCG) (such as paper guidelines, peer-to-peer consultation and previous experience.). Moreover, were analysed specific features of the computerized guidelines which are potentially linked with the improvement of the process of care.
Methods
Search strategy
An extensive search of scientific literature was carried out querying electronic databases to identify relevant studies: Pubmed/Medline, Embase and Cochrane Controlled Trials Register. The search covered the period from January 1992 to March 2006. The search of articles were carried out using the following key words, related to:
-
1.
Exposure variables: computerized clinical guidelines, computer-based guidelines, computerized clinical recommendations, computer decision support aids, software guidelines, computerized clinical pathways, computerized critical pathways, computer-based pathway*, electronic care map, electronic care pathways, electronic clinical pathways, electronic critical pathways, integrated care pathway, electronic clinical reminder, electronic clinical reminders, electronic reminder AND practice guidelines AND electronic medical record, computerized reminders AND guidelines;
-
2.
Effect variables: medical outcomes, organisation's outcomes, patients' outcomes; process of care
-
3.
Population variables: medical doctors, health personnel.
The search in grey literature was carried out using general purpose search engines (GOOGLE, VIVISIMO) in order to identify missing articles. Rest of the articles were identified through the analysis of bibliographic citations.
Inclusion and exclusion criteria
Considering study's design, only experimental or analytical studies were included while descriptive studies were excluded. The main exposure variable in our research was the comparison between CCG and NCCG (such as paper guidelines, peer-to-peer consultation and previous experience). Papers which did not contain comparison between CCG and NCCG were excluded from analysis. So, only the papers in which the guidelines were coming from a scientific society recommendations or approved by a National body, a scientific society, union or corporation of physicians or universities were included in this study. Articles not matching these criteria were excluded. Also, only articles focusing on adult patients (age ≥18 years) were taken into consideration. Studies involving children and adolescents (age <18 years) were excluded due to the fact that there are specific factors linked with the paediatricians adherence to guidelines in this specific age group [16–18].
Study selection
Titles and abstracts of the selected studies were reviewed independently by two authors (C.S.C and A.R.) and were rated as "potentially relevant" or "not relevant" using search strategies based on study design, subjects and type of intervention. If one of the reviewers considered a reference potentially relevant, full-text articles were retrieved and examined independently, using the full set of inclusion and exclusion criteria to select the final number of studies for research. Disagreements between reviewers were resolved by discussion or by third author (G.D.).
Data extraction
Two reviewers (C.S.C. and A.R.) assessed whether the use of computerized guidelines was going to improve the process of care and evaluated the positive or negative impact of computerized guidelines on the process of care.
Afterwards, the outcomes were distributed in two groups: favouring CCG and favouring NCCG based on evaluation of results of inference analysis. Then, the effect of computerized guidelines was defined as positive when reported improvement was more than 50% of the outcomes. Effect was defined as negative when the improvement was equal or less than 50% of the outcomes. Positive or negative effects of computerized guidelines were confirmed according to the authors' judgment in the conclusions' section of each single paper. Finally, were analysed the variables potentially linked to positive effect on the process of care. Some variables were not included in the analysis because it was not possible to obtain them from most studies (patients' age, health care givers' age, health care providers' degree, duration of observation). The analysed system's features were identified referring to Kawamoto [12] or they were extracted by the authors from the studies. So, 21 features related to the following categories were analysed:
-
General system features;
-
Clinician-system interaction features;
-
Communication content features;
-
Auxiliary features;
-
Guidelines features.
The description of each feature is reported in Table 1.
Quality assessment
The methodology of each study was assessed independently by two authors (C.S. and A.R.) according to a score assessing five potential sources of study bias [10, 19–21]. Disagreements were solved by consulting the third author (G.D.) or according to a consensus. The studies were evaluated using following system:
-
allocation to study groups (random, 2; quasi-random, 1; selected concurrent controls, 0);
-
data analysis and presentation of results (appropriate statistical analysis and clear presentation of results, 2; inappropriate statistical analysis or unclear presentation of results, 1; inappropriate statistical analysis and unclear presentation of results, 0);
-
presence of baseline differences between the groups that were potentially linked to study outcomes (no baseline differences present or appropriate statistical adjustments made for differences, 2; baseline differences present and no statistical adjustments made, 1; baseline characteristics not reported, 0);
-
objectivity of the outcome (objective outcomes or subjective outcomes with blinded assessment, 2; subjective outcomes with no blinding but clearly defined assessment criteria, 1; subjective outcomes with no blinding and poorly defined, 0);
-
completeness of follow-up for the appropriate unit of analysis (> 90%, 2; from 80% to 90%, 1; < 80% or not described, 0).
The cut-off value for including an article in our paper was 5/10.
The quality assessment of each study is reported in Table 2.
Statistical Analysis
Each study, comparing the impact of CCG versus NCCG, was considered as a unit of analysis.
We estimated, within 95% confidence interval:
-
Positive Effect Prevalence, calculated as the proportion of studies showing a positive effect of CCG on the total of selected studies.
-
Negative Effect Prevalence, calculated as the proportion of studies not showing any or negative effect of CCG on the total of selected studies.
Chi-square test was performed in order to identify whether the differences between the proportions of the studies' positive and negative effects were statistically significant. The significance level was set at 5% (α = 0.05).
The effect of each specific feature on the process of care was also analysed in a backward logistic regression analysis which was carried out to evaluate the association of features with the positive effect of CCG, adjusting for the following variables:
-
publication year, using 1999 (after publication of Shifman's article) as a cut-off year (1994-1999; 2000-2006);
-
design of the study: observational and experimental studies;
-
quality of the study, using 7 as cut-off score (5-7; 8-10)
Hosmer-Lemeshow test was applied to evaluate the goodness of fit of model. All analyses were carried out using SPSS package, version 13.0.
Results
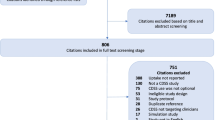
A total number of 2,996 articles out of 3,502 was excluded because of the title and the content of abstract. Then, 191 out of 506 studies met the inclusion criteria. Forty-five articles were included in the final selection [14, 15, 22–64]. (Figure 1). Some of the articles included in Garg's and Kawamoto reviews [6, 12] were excluded by our selection [see Additional file 1]. The characteristics of selected studies are shown in Table 3.
Automatic provision of recommendation in electronic version as part of clinician workflow (proportion = 0.82) and Degree of automation (proportion = 0.80) were the most frequent features used in the CCG software described in the selected articles. On the contrary, the least frequent features were Recommendation executed by noting agreement, Provision of a recommendation not just an assessment, Promotion of action rather than inaction (proportion = 0.11) as shown in Table 1.
Proportions of studies with Positive and Negative Effect of CCG versus NCCG are shown in Figure 2. In the selected 45 articles the positive effect proportion of CCG was 0.64 (p = 0.053) [see Additional file 2].
The multivariable analysis highlighted two variables as statistically significant predictors of CCG positive impact on the process of care: Automatic provision of recommendation in electronic version as part of clinician workflow (Odds Ratio [OR]= 17.5; 95% confidence interval [CI]: 1.6-193.7) and Publication Year (OR = 6.7; 95%CI: 1.3-34.3). Besides, the feature Justification of recommendation via provision of reasoning (OR = 14.8; 95%CI: 0.9-224.2) resulted marginally significant in logistic analysis.
The goodness of fit of the logistic model was confirmed in the Hosmer-Lemeshow test (p = 0.905).
Discussion
Previous researches [6, 10, 11] reviewed controlled clinical trials classified within different categories (e.g. drug dose determination, diagnosis, prevention) in order to assess the effects of CDSS on physician's performance and patient's outcomes. Enhancements on clinical performance were reported after the use of these tools. Furthermore, role of specific features of CDSS affecting clinical practice were identified by Kawamoto et al [12].
Our study instead focused on the effectiveness of CCG (a group of CDSS strictly related to the medical decision making). The functionality and the effectiveness of CCG until 1998 had been studied by Shiffman et al. [13]. They reviewed the literature showing that CCG delivered positive effect, but no quantitative and synthetic analysis were carried out. Our contribution provides an updated, systematic and quantitative analysis aiming to understand the design factors which are responsible for the success or the failure of computer-based guidelines compared with NCCG.
The resulting evidence showed that the use of CCG seems to have a significant impact on the process of care. In addition to qualitative evidence reported by Shiffman [13], the multivariable analysis highlighted the positive effect of the presence of an operating CCG system, characterized by the automatic provision of recommendation in electronic form as part of clinician workflow. This system is designed for providing automatic support to clinicians so that they don't need to look for computer advices. The system automatically provides support on clinical or administrative task and recommends execution or avoiding of it during the clinical process, (e.g. automatic recommendation of executing prophylaxis in patients at risk of deep-vein thrombosis [48]), and in decisions, such as the selection from a set of potential alternatives based on predefined criteria (e.g. automatic prompt of further assessment for potential Latent Tuberculosis Infection in patients selected according to specific criteria [38]) [65].
The positive effect might be related to time saving for clinicians, facilitation of the information retrieval and integration among different users.
The evidence of increased probability of positive effect for CCG, showed after 1999, might suggest that the improvement of the process of care may be related to the development of more automated CCG systems [66, 67].
The physicians' involvement in decisions regarding clinical recommendations, even though marginally significant in the multivariable analysis, might be a key element for the effective organization of the whole process of care, relating to the improvement of the adherence of physicians to guidelines. This aspect is coherent to the active roles that physicians should play in Clinical Governance context [68, 69].
Some limits of our study might be related to the lack of quantitative estimate of specific outcomes linked to clinical conditions. However, the evaluation of synthetic quantitative measures of CCG effect was unfeasible because of the high heterogeneity of analysed guidelines, population and outcomes. However, our work presents the synthetic result on the effectiveness of CCG, providing a quantitative and reproducible evaluation.
Conclusions
Findings of this paper suggest clinicians, managers and other health care decision makers which features of CCG might improve the structure of an electronic system in health care settings. At the same time, the implementation of CCG may be integrated with more training and investment in user friendly hardware and software. Therefore, specific studies should be carried out to evaluate the cost-effectiveness of implementing CCG systems.
Abbreviations
- CCG:
-
computerized clinical guidelines
- CDSSs:
-
computerized clinical decision support systems
- NCCG:
-
non-computerized clinical guidelines.
References
Field MJ, Lohr KN, eds: Clinical practice guidelines: directions for a new program. 1990, Washington, DC: National Academy Press
Shekelle P, Eccles MP, Grimshaw JM, Woolf SH: When should clinical guidelines be updated?. BMJ. 2001, 323 (7305): 155-7. 10.1136/bmj.323.7305.155.
Shekelle PG, Woolf SH, Eccles M, Grimshaw J: Clinical guidelines: developing guidelines. BMJ. 1999, 318 (7183): 593-6.
Steinbrook R: Guidance for guidelines. N Engl J Med. 2007, 356 (4): 331-3. 10.1056/NEJMp068282.
Wyatt J, Spiegelhalter D: Field trials of medical decision-aids: potential problems and solutions. Proceedings of the Annual Symposium on Computer Application in Medical Care: 17-20 November 1991; Washington. Edited by: Clayton P. 1991, 3-7.
Garg AX, Adhikari NKJ, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, Sam J, Haynes B: Effects of Computerized Clinical Decision Support Systems on practitioner performance and patient outcomes. JAMA. 2005, 293: 1223-1238. 10.1001/jama.293.10.1223.
Shortliffe EH: Computer programs to support clinical decision making. JAMA. 1987, 258 (1): 61-6. 10.1001/jama.258.1.61.
Waitman LR, Miller RA: Pragmatics of implementing guidelines on the front lines. J Am Med Inform Assoc. 2004, 11 (5): 436-8. 10.1197/jamia.M1621.
Wang D, Peleg M, Tu SW, Shortliffe EH, Greenes RA: Representation of clinical practice guidelines for computer-based implementations. Stud Health Technol Inform. 2001, 84 (Pt 1): 285-9.
Hunt DL, Haynes RB, Hanna SE, Smith K: Effects of computer-based clinical decision support systems on physicians performance and patient outcomes. J Am Med Assoc. 1998, 280: 1339-1346. 10.1001/jama.280.15.1339.
Johnston ME, Langton KB, Haynes RB, Mathieu A: Effects of computer-based clinical decision support systems on clinician performance and patient outcome. A critical appraisal of research. Ann Intern Med. 1994, 120 (2): 135-42.
Kawamoto K, Houlihan CA, Balas EA, Lobach DF: Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005, 330: 765-773. 10.1136/bmj.38398.500764.8F.
Shiffman RN, Liaw Y, Brandt CA, Corb GJ: Computer-based guideline implementation system: a systematic review of functionality and effectiveness. JAMIA. 1999, 6: 104-114.
Overhage JM, Tierney WM, McDonald CJ: Computer reminders to implement preventive care guidelines for hospitalized patients. Arch Intern Med. 1996, 156: 1551-1556. 10.1001/archinte.156.14.1551.
Raebel MA, Lyons EE, Chester EA, Bodily MA, Kelleher JA, Long CL, Miller C, Magid DJ: Improving laboratory monitoring at initiation of drug therapy in ambulatory care. Arch Intern Med. 2005, 165: 2395-2401. 10.1001/archinte.165.20.2395.
Cabana MD, Rand CS, Becher OJ, Rubin HR: Reasons for pediatrician nonadherence to asthma guidelines. Arch Pediatr Adolesc Med. 2001, 155 (9): 1057-62.
Cabana MD, Ebel BE, Cooper-Patrick L, Powe NR, Rubin HR, Rand CS: Barriers pediatricians face when using asthma practice guidelines. Arch Pediatr Adolesc Med. 2000, 54 (7): 685-93.
Weinberger M: Seventeen Years of Asthma Guidelines: why Hasn't the Outcome Improved for Children?. J Pediatr. 2009, 54 (6): 786-8.
Haynes RB, Walker C: Computer-aided quality assurance. Arch Intern Med. 1987, 147: 1297-1301. 10.1001/archinte.147.7.1297.
Damiani G, Pinnarelli L, Sammarco A, Sommella L, Francucci M, Ricciardi W: Postoperative Pulmonary Function inOpen versus Laparoscopic Cholecystectomy: A Meta-Analysis of the Tiffenau Index Dig. Surg. 2008, 25: 1-7.
Chalmers TC, Smith H, Blackburn B, Silverman B, Schroeder B, Reitman D, Ambroz : A method for assessing the quality of a randomized control trial. A Control Clin Trials. 1981, 2 (1): 31-49. 10.1016/0197-2456(81)90056-8.
Jousimaa J, Makela M, Kunnamo I, MacLennan G, Grimsha JM: Primary care guidelines on consultation practices: the effectiveness of computerized versus paper-based versions. Int J Technol Assess Health Care. 2002, 18: 586-596.
Rood E, Bossman RJ, Spoel Van Der JI, Taylor P, Zandstra DF: Use of a computerized guideline for glucose regulation in the intensive care unit improved both guideline adherence and glucose regulation. JAMIA. 2005, 12: 172-180.
Butzlaff M, Vollmar HC, Floer B, Koneczny N, Isfort J, Lange S: Learning with computerized guidelines in general practice? A randomized controlled trial. Fam Pract. 2003, 21: 183-188. 10.1093/fampra/cmh214.
Medow MA, Wilt TJ, Dysken S, Hillson SD, Woods S, Borowsky SJ: Effect of written and computerized decision support aids for the U.S. Agency for Health Care Policy and Research depression guidelines on the evaluation of hypothetical clinical scenarious. Med Decis Making. 2001, 21: 344-356.
Durieux P, Nizard R, Ravaud P, Mounier N, Lepage E: A Clinical Decision Support System for prevention of venous thromboembolism. Effect on physician behaviour. JAMA. 2000, 283: 2816-2821. 10.1001/jama.283.21.2816.
Rossi RA, Every NR: A computerized intervention to decrease the use of calcium channel blockers in hypertension. J Gen Intern Med. 1997, 12: 672-678. 10.1046/j.1525-1497.1997.07140.x.
Safran C, Rind DM, Davis RB, Ives D, Sands DZ, Currier J, Slack WV, Makadon HJ, Cotton DJ: Guidelines for management of HIV infection with compute-based patient's record. Lancet. 1995, 346: 341-346. 10.1016/S0140-6736(95)92226-1.
Dexter PR, Perkins S, Overhage M, Maharry K, Kohler RB, McDonald CJ: A computerized reminder system to increase the use of preventive care for hospitalized patients. N Engl J Med. 2001, 345: 965-970. 10.1056/NEJMsa010181.
Mosen D, Elliott CG, Egger MJ, Mundorff M, Hopkins J, Patterson R, Gardner RM: The effect of a computerized reminder system on the prevention of postoperative venous thromboembolism. Chest. 2004, 125: 1635-1641. 10.1378/chest.125.5.1635.
Shojania KG, Yokoe D, Platt R, Fiskio J, Ma'luf N, Bates DW: Reducing vancomycin use utilizing a computer guideline: results of a randomized controlled trial. JAMIA. 1998, 5: 554-562.
Schriger DL, Baraff LJ, Rogers WH, Cretin S: Implementing of clinical guidelines using a computer charting system. Effect on the initial care of health care workers exposed to body fluids. JAMA. 1997, 278: 1585-1590. 10.1001/jama.278.19.1585.
Thomas KW, Dayton CS, Peterson MW: Evaluation of internet-based clinical decision support systems. JMIR. 1999, 1: 6-36.
Carton M, Auvert B, Guerini H, Boulard JC, Heautot JF, Landre MF, Beauchet A, Sznajderi M, Brun-Ney D, Chagnon S: Assessment of radiological referral practice and effect of computer-based guidelines on radiological requests in two emergency departments. Clin Radiol. 2002, 57: 123-128. 10.1053/crad.2001.0827.
Lobach DF, Hammond WE: Computerized decision support based on a clinical practice guideline improves compliance with care standards. Am J Med. 1997, 102: 89-98. 10.1016/S0002-9343(96)00382-8.
Tierney WM, Overhage JM, Murray MD, Harris LE, Zhou XH, Eckert GJ, Smith FE, Nienaber N, McDonald CJ, Wolinsky FD: Effects of computerized guidelines for managing heart disease in primary care. J Gen Intern Med. 2003, 18: 967-976. 10.1111/j.1525-1497.2003.30635.x.
McMullin ST, Lonergan TP, Rynearson CS, Doerr TD, Veregge PA, Scanlan ES: Impact of an evidence-based computerized decision support system on primary care prescription costs. Ann Fam Med. 2004, 2: 494-498. 10.1370/afm.233.
Steele AW, Eisert S, Davidson A, Sandison T, Lyons P, Garrett N, Gabow P, Ortiz E: Using computerized clinical decision support for latent tuberculosis infection screening. Am J Prev Med. 2005, 28: 281-284. 10.1016/j.amepre.2004.12.012.
Dayton CS, Ferguson S, Hornick DB, Peterson MW: Evaluation of an internet-based decision-support system for applying the ATS/CDC guidelines for tuberculosis preventive therapy. Med Decis Making. 2000, 20: 1-6. 10.1177/0272989X0002000101.
Overhage JM, Tierney WM, Zhou XA, McDonald CJ: A randomized trial of "corollary orders" to prevent errors of omission. JAMIA. 1997, 4: 364-375.
Filippi A, Sabatini A, Badioli L, Samani F, Mazzaglia G, Catapano A, Cricelli C: Effects of an automated electronic reminder in changing the antiplatelet drug-prescribing behavior among italian general practitioners in diabetic patients. Diabetes Care. 2003, 26: 1497-1500. 10.2337/diacare.26.5.1497.
Turner RC, Peden JG, O'Brien K: Patient-carried card prompts vs computer-generated prompts to remind private practice physicians to perform health maintenance measures. Arch Intern Med. 1994, 154: 1957-1960. 10.1001/archinte.154.17.1957.
Burack RC, Phyllis AG: Promoting screening mammography in inner-city settings. The sustained effectiveness of computerized reminders in a randomized controlled trial. Med Care. 1997, 35: 921-931. 10.1097/00005650-199709000-00005.
Burack RC, Phyllis AG, George J, Stengle W, Warbasse L, Moncrease A: Promoting screening mammography in inner-city settings: a randomized controlled trial of computerized reminders as a component of a program to facilitate mammography. Med Care. 1994, 32: 609-624. 10.1097/00005650-199406000-00006.
Sequist TD, Gandhi TK, Karson AS, Fiskio JM, Bugbee D, Sperling M, Cook EF, Orav EJ, Fairchild DJ, Bates DW: A randomized trial of electronic clinical reminders to improve quality of care for diabetes and coronary artery disease. JAMIA. 2005, 12: 431-437.
Derose SF, Dudl JR, Benson VM, Contreas R, Nakahiro RK, Ziel FH: Point-of-service reminders for prescribing cardiovascular medications. Am J Manag Care. 2005, 11: 298-304.
Kitahata MM, Dillingham PW, Chaiyakunapruk N, Buskin SE, Jones JL, Harrington RD, Hooton TM, Holmes KK: Electronic human immunodeficiency virus (HIV) clinical reminder system improves adherence to practice guidelines among the University of Washington HIV study cohort. Clin Infect Dis. 2003, 36: 803-811. 10.1086/368085.
Kucher N, Koo S, Quiroz R, Cooper JM, Paterno MD, Soukonnikov B, Goldhaber SZ: Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med. 2005, 352: 969-977. 10.1056/NEJMoa041533.
Feldman PH, Murtaugh CM, Pezzin LE, McDonald MV, Peng TR: Just-in-time evidence-based e-mail "reminders" in home health care: impact on patient outcomes. Health Serv Res. 2005, 40: 865-885. 10.1111/j.1475-6773.2005.00389.x.
Frank O, Litt J, Beilby J: Opportunistic electronic reminders. Aust Fam Physician. 2004, 33: 87-90.
Feldstein A, Elmer PJ, Smith DH, Herson M, Orwoll E, Chen C, Aickin M, Swain MC: Electronic medical record reminder improves osteoporosis management after a fracture: a randomized, controlled trial. J Am Geriatr Soc. 2006, 54: 450-457. 10.1111/j.1532-5415.2005.00618.x.
Williams RB, Boles M, Johnson RE: A patient-initiated system for preventive health care. Arch Fam Med. 1998, 7: 338-345. 10.1001/archfami.7.4.338.
Zanetti G, Flanagan HL, Cohn LH, Giardina R, Platt R: Improvement of intraoperative antibiotic prophylaxis in prolonged cardiac surgery by automated alerts in the operating room. Infect Control Hosp Epidemiol. 2003, 24: 13-16. 10.1086/502109.
Demakis JG, Beauchamp C, Cull WL, Denwood R, Eisen SA, Lofgren R, Nichol K, Woolliscroft J, Henderson WG: Improving residents' compliance with standards of ambulatory care. JAMA. 2000, 284: 1411-1416. 10.1001/jama.284.11.1411.
Hetlevik I, Holmen J, Kruger O: Implementing clinical guidelines in the treatment of hypertension in general practice. Scand J Prim Health Care. 1999, 17: 35-40. 10.1080/028134399750002872.
Hetlevik I, Holmen J, Kruger O, Kristensen P, Iversen H, Furuseth K: Implementing clinical guidelines in the treatment of diabetes mellitus in general practice. Int J Technol Assess Health Care. 2000, 16: 210-227. 10.1017/S0266462300161185.
Murtaugh CM, Pezzin LE, McDonald MV, Feldman PH, Peng TR: Just-in-time evidence-based e-mail "reminders" in home health care: impact on nurse practices. Health Serv Res. 2005, 40: 849-864. 10.1111/j.1475-6773.2005.00388.x.
Lafata JE, Baker AM, Divine GW, McCarthy BD, Xi H: The use of computerized birthday greeting reminders in the management of diabetes. J Gen Intern Med. 2002, 17: 521-530. 10.1046/j.1525-1497.2002.10901.x.
Fitzmaurice DA, Hobbs FDR, Murray ET, Holder RL, Allan TF, Rose PE: Oral anticoagulation management in primary care with the use of computerized decision support and near-patient testing. Arch Intern Med. 2000, 160: 2343-2348. 10.1001/archinte.160.15.2343.
Poller L, Wright D, Rowlands M: rospective comparative study of computer programs used for management of warfarin. J Clin Pathol. 1993, 46: 299-303. 10.1136/jcp.46.4.299.
Meigs JB, Cagliero E, Dubey A, Murphy-Sheehy P, Gildesgame C, Chueh H, Barry M, Singer DE, Nathan MD: A controlled trial of web-based diabetes disease management. Diabetes Care. 2003, 26: 750-757. 10.2337/diacare.26.3.750.
Montgomery AA, Fahey T, Peters TJ, MacIntosh C, Sharp DJ: Evaluation of computer based clinical decision support system and risk chart for management of hypertension in primary care: randomised controlled trial. BMJ. 2000, 320: 686-690. 10.1136/bmj.320.7236.686.
Cannon DS, Allen SN: A comparison of the effects of computer and manual reminders on compliance with a mental health clinical practice guideline. JAMIA. 2000, 7: 196-203.
McCowan C, Neville RG, Ricketts W, Warner FC, Hoskins G, Thomas GE: Lessons from a randomized controlled trial designed to evaluate computer decision support software to improve the management of asthma. Med Inform. 2001, 26 (3): 191-201. 10.1080/14639230110067890.
Wang D, Peleg M, Tu SW, Boxwala AA, Greenes RA, Patel VL, Shortliffe EH: Representation primitives, process models and patient data in computer-interpretable clinical practice guidelines: a literature review of guideline representation models. Int J Med Inform. 2002, 68 (1-3): 59-70. 10.1016/S1386-5056(02)00065-5.
Isern D, Moreno A: Computer-based execution of clinical guidelines: a review. Int J Med Inform. 2008, 77 (12): 787-808. 10.1016/j.ijmedinf.2008.05.010.
Goldstein MK: Using health information technology to improve hypertension management. Curr Hypertens Rep. 2008, 10 (3): 201-7. 10.1007/s11906-008-0038-6.
Scally G, Donaldson LJ: Clinical governance and the drive for quality improvement in the new NHS in England. BMJ. 1998, 317: 61-65.
Halligan A, Donaldson LJ: Implementing clinical governance: turning vision into reality. BMJ. 2001, 322: 1413-1417. 10.1136/bmj.322.7299.1413.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6963/10/2/prepub
Acknowledgements
Funding for this project "Development, application and effectiveness valuation of an informative system to support the clinical research" was provided by the Italian Ministry of Health.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
GD, LP and WR contributed to the conception of this paper; GD, LP RG, LoS designed the study. SCC and RA selected articles that met the inclusion criteria and extracted data. LS, LP conducted the statistical analysis. All authors made substantial contributions to the interpretation of results and have seen and approved the final version.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Damiani, G., Pinnarelli, L., Colosimo, S.C. et al. The effectiveness of computerized clinical guidelines in the process of care: a systematic review. BMC Health Serv Res 10, 2 (2010). https://doi.org/10.1186/1472-6963-10-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6963-10-2