Abstract
Background
The development of resistant to current antimalarial drugs is a major challenge in achieving malaria elimination status in many countries. Therefore there is a need for new antimalarial drugs. Medicinal plants have always been the major source for the search of new antimalarial drugs. The aim of this study was to screen selected Malaysian medicinal plants for their antiplasmodial properties.
Methods
Each part of the plants were processed, defatted by hexane and sequentially extracted with dichloromethane, methanol and water. The antiplasmodial activities of 54 plant extracts from 14 species were determined by Plasmodium falciparum Histidine Rich Protein II ELISA technique. In order to determine the selectivity index (SI), all plant extracts demonstrating a good antiplasmodial activity were tested for their cytotoxicity activity against normal Madin-Darby Bovine Kidney (MDBK) cell lines by 3-(4, 5-Dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) assay.
Results
Twenty three extracts derived from Curcuma zedoaria (rhizome), Curcuma aeruginosa (rhizome), Alpinia galanga (rhizome), Morinda elliptica (leaf), Curcuma mangga (rhizome), Elephantopus scaber (leaf), Vitex negundo (leaf), Brucea javanica (leaf, root and seed), Annona muricata (leaf), Cinnamomun iners (leaf) and Vernonia amygdalina (leaf) showed promising antiplasmodial activities against the blood stage chloroquine resistant P. falciparum (EC50 < 10 μg/ml) with negligible toxicity effect to MDBK cells in vitro (SI ≥10).
Conclusion
The extracts belonging to eleven plant species were able to perturb the growth of chloroquine resistant P. falciparum effectively. The findings justified the bioassay guided fractionation on these plants for the search of potent antimalarial compounds or formulation of standardized extracts which may enhance the antimalarial effect in vitro and in vivo.
Similar content being viewed by others
Background
Malaria is one of the major public health problems in many tropical regions, including Malaysia. The resistance Plasmodium falciparum to common antimalarial drugs such as chloroquine, sulfadoxine-pyrimethamine [1–3] and artemisinin [4] have been reported. In response to this situation, as recommended by World Health Organization (WHO), Malaysian government has changed its first line antimalarial drug regimen to artemisinin-based combination therapy (ACT) such as the use of fixed dose artemether-lumefantrine combination (Riamet®) in the treatment of uncomplicated falciparum malaria (National Antibiotic Guideline 2008, Ministry of Health, Malaysia). However, the ability of the malaria parasite such as P. falciparum to develop and become resistant to ACT in the future cannot be denied [5–9]. Therefore, discovering new antimalarial drugs is a priority in the health sector. The challenges in malaria drug discovery are to find safe, cheap and effective antimalarial agents.
Plants have always been the main source for the search of new antimalarial drugs. Until the year of 2003, 1277 plant species from 160 families have been published by 33 tropical countries for their use in treatment of malaria and fevers [10]. In Peninsular Malaysia, about 21 plant species are used by the locals as traditional medicine for malaria treatment [11–13]. So, it is of pivotal to know the potential ingredients or candidates which play a major role in killing the malaria parasites. Thus, screening the plant extracts for antimalarial properties prior to bioassay guided fractionation and potent compound isolation is important.
Research on the effectiveness of medicinal plant extracts in inhibiting the growth of malaria parasite has been extensively studied worldwide. One good example is Artemisia annua where whole leaves extract of this plant has exhibited better antiplasmodial activity as compared to its isolated compound, artemisinin [14, 15]. This shows that there are other unidentified compounds still remain in this plant.
Many of medicinal plants which grow in Malaysian soil have been reported by the local scientists for their antiplasmodial activities in vitro and in vivo (Table 1). In this study, another 14 selected Malaysian medicinal plants (Table 2) with traditional claims were screened for their antiplasmodial activity against the malaria parasite, chloroquine (CQ) resistant P. falciparum (K1) in vitro by using P. falciparum Histidine Rich Protein II (HRP2) ELISA technique [16].
Methods
Plant collection and identification
All plant parts except Brucea javanica and Annona muricata were collected from the herbal garden of Herbal Medicine Research Centre (HMRC), Institute for Medical Research (IMR), Kuala Lumpur, Malaysia. Both B. javanica and A. muricata were collected from Northern part of Peninsular Malaysia, Tupah Village, Kedah andMalaysian Agricultural Research and Development Institute (MARDI), Kedah, respectively. All plants parts except B. javanica, Curcuma aeruginosa, C. mangga, C. phaeocaulis were identified and authenticated by Dr. Richard Chung Cheng Kong and deposited in the Herbarium of Forest Research Institute Malaysia (FRIM), Kepong, Kuala Lumpur. The B. javanica was identified and authenticated by Mr. Sani Miran and deposited in the Herbarium of the Universiti Kebangsaan Malaysia (UKM), Bangi, Selangor, Malaysia. The Curcuma species were identified and deposited in the Herbarium of Herbal Medicine Research Centre, Institute for Medical Research, Kuala Lumpur, Malaysia.
Plant extract preparation
The fresh plant materials (rhizome, leaf, root and seed) were cut into small pieces, dried and pulverized into powder before extraction with solvents in increasing polarity (Figure 1). The powdered materials were first defatted with hexane and sequentially extracted with dichloromethane (DCM), methanol (MeOH) and sterile deionised water (H2O) (80°C). Briefly, the resulting solutions from the first extraction using DCM were filtered through filter paper (Whatman No.1, England) to collect the supernatant from the residue. Organic supernatant were evaporated to dryness under reduced pressure with a rotary evaporator (Buchi Rotavapor R-200, Switzerland) at a temperature 40°C. The residue was further extracted by using MeOH similar to the procedure that carried out for the DCM. The resulting residue was air dried and used for further extraction with sterile H2O at 80°C. The aqueous supernatant were freeze-dried to obtain crude extracts (Figure 1). All crude extracts (DCM, MeOH and H2O) were stored at 4°C until used.
The mammalian cells and parasites
The CQ resistant P. falciparum strain, K1 was obtained from American Type Culture Collection (ATCC), The Malaria Research and Reference Reagent Resource Center (MR4). Madin-Darby Bovine Kidney (MDBK) cells were also obtained from ATCC. The cryopreserved parasites and cells were thawed and maintained in culture for further use in this study. Briefly, the cryopreserved parasites were thawed in waterbath at 37°C. The thawed parasites were transferred into 15 ml conical tubes and equal volume of 3.5% natrium chloride (NaCl) were added drop wise and swirled to mix. The mixtures were centrifuged at 500 × g for 5 minutes and the supernatants were discarded. These steps were repeated twice before adding the complete RPMI 1640 culture medium (Invitrogen, USA) containing 25 mM 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES), 0.2% sodium bicarbonate (NaHCO3), 0.02 mg/ml gentamycin supplemented with 10% AB+ human serum (Invitrogen, USA).
For MDBK cells, the cryopreserved cells were thawed immediately in the waterbath at 37°C. The thawed cells were transferred in 15 ml conical tubes containing 1 ml of complete DMEM culture medium (Invitrogen, USA) containing 25 mM HEPES, 0.4% sodium bicarbonate (NaHCO3), 100U of Penstrep (100U penicillin and 100U streptomycin) supplemented with 10% fetal bovine serum (FBS). The mixtures were centrifuged at 1000 × g, 4°C for 5 minutes. The supernatants were discarded. The cell pellets were transferred into 25 cm2 culture flask containing 5 ml of complete DMEM culture medium. The suspension were mixed gently and incubated in 5% carbon dioxide (CO2) incubator at 37°C.
In vitro culture and synchronization of P. falciparum
The CQ resistant P. falciparum were grown by candle jar technique (3% CO2 and 17% O2) [37]. The culture was set up in a 25 cm3 culture flask with filtered vent and maintained in complete RPMI 1640 culture medium (Invitrogen, USA). The P. falciparum was grown in ‘O’ type fresh red blood cell (RBC) with the initial culture started with 1% parasitemia at 2.5% hematocrit. The parasite density was monitored daily by making thin blood smears stained with 10% Giemsa solution and observed under the microscope at 1000 times magnification. When the parasitemia of the parasite culture reached approximately 5 to 7%, the parasites were synchronized using 5% sorbitol [38] and cultured for one complete cycle prior to be used in in vitro P. falciparum HRP2 assay.
In vitro P. falciparum HRP2 assay
All crude extracts were evaluated in vitro for their antiplasmodial activities by HRP2 assay [16, 39]. The extracts were solubilised in 100% dimethyl sulphoxide (DMSO) or sterile H2O (H2O extracts only) to get 5 mg/ml stocks. In preparation of extract or drug stock plates, the extracts (5 mg/ml) were serially diluted (2 fold dilution) to 7 point concentrations (ranging from 5 to 0.08 mg/ml) in DMSO from well A1 to A7 in a 96 well plate. Fifteen microliters of serially diluted stock extracts were transferred correspondingly into watery plates containing 225 μl of sterile H2O. An aliquote of watery plates will be used in HRP2 assay.
Ring-infected RBCs with 5% parasitemia were adjusted to 0.05% parasitemia and 1.5% hematocrit. A total of 190 μl parasitized RBCs at 1.5% hematocrit were added into each well of the test plates. A total of 10 μl of serially diluted extracts from the watery plates prepared above were transferred into the test plates containing parasitized RBCs and incubated in a candle jar at 37°C for 72 hours. The final tested concentration ranging from 16 to 0.2 μg/ml. The final concentration of DMSO was 0.3%. Chloroquine (CQ) (Sigma, USA), quinine (Q) (Sigma, USA), mefloquine (Mef) (Sigma, USA) and artemisinine (Art) (Sigma, USA) were used as standard control to validate the test. The final tested concentration for standard control ranged from 1772.6 to 27.7 nM for CQ, 3495 to 54.6 nM for Q, 601.3 to 9.4 nM for Mef and 51.2 to 0.8 nM for Art. The negative control was the infected RBC without extracts or with sterile H2O only. After 72 hours of incubation, the test plates were kept in -80°C overnight. The plates were thawed at room temperature to lyse the infected RBCs. The activity of the parasite-extract exposure (end point) was measured by HRP2 assay. One day prior to the assay, 100 μl of immunoglobulin M (IgM) capture antibody (MPFM-55A, ICL, Inc, Newberg, OR, USA) specific for P. falciparum HRP2 (1 μg/ml in phosphate-buffered saline (PBS)) were added to each well of a 96-well ELISA plates (Microlon 600, Greiner, Germany). The plates were covered and incubated at 4°C overnight. Following incubation, the contents of the wells were removed and the plates were washed three times with 0.05% PBS-Tween 20 (PBST). The non-binding sites of the ELISA plates were blocked with 200 μl/well of 2% bovine serum albumin in PBS for 2 hours at room temperature. Following the blocking step, the ELISA plates were washed 3 times with 200 μl of 0.05% PBST. Hundred microliters of the P. falciparum infected RBC lysates (freeze thawed) were transferred from the test plates into ELISA plates and incubated in humidity chamber for 1 hour at room temperature. The ELISA plates were washed as described above. Hundred microliters of the detector antibody (MPFG-55P, ICL, Inc, Newberg, OR, USA) conjugated with horseradish peroxidase (0.2 μg/ml in PBS) were added to each well, and incubated in humid chamber for 1 hour at room temperature. Following a subsequent washing step similar to the above, 100 μl of 3,3’, 5,5;-tetramethylbenzidine (TMB) chromogen (Zymed Lab., Inc., San Francisco, CA, USA) was added to each well and incubated for 10 min in dark, followed by the addition of 50 μl of 1 M sulphuric acid. The absorbance was determined by using ELISA plate reader at a wavelength of 450 nm (FLUOstar Omega, Germany). The collected data were transferred to HN-nonLin software (malaria.farch.net) to get a 50% Effective Concentration (EC50) value directly from the graph.
In vitro cytotoxicity assay
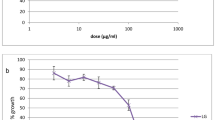
The MDBK cells were maintained in complete DMEM culture medium containing 25 mM HEPES, 0.4% sodium bicarbonate (NaHCO3), 100U of Penstrep (100U penicillin and 100U streptomycin) supplemented with 10% fetal bovine serum (FBS). The cytotoxicity of the extracts were measured by 3-(4, 5-Dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) assay [40]. Prior to the day of test, the stock plates were prepared by serially diluting (2 fold dilution) the stock extracts (5 mg/ml) to 7 point concentration (ranging from 5 to 0.16 mg/ml) with DMSO or sterile H2O (for H2O extracts only). Then, 6 μl of serially diluted stocks were transferred into 96 well plates containing 294 μl of complete DMEM media (Medium plates). On the day of the test, MDBK cells were harvested and adjusted to 1 × 104 cell per ml. A hundred microliter of cell suspension was seeded into each well of a 96-well plate and allowed to grow overnight. Then, 100 μl of test extracts taken from medium plate (as prepared above) were added to each well accordingly ranging final concentration of 0.8 to 50 μg/ml. The final concentration of DMSO in all test was less than 1%. All tests were performed in duplicate. The positive control for cell growth is the cell suspension without test substance while the negative control is the cell suspension with 0.05% Triton X 100. The culture was incubated at 37°C in 5% CO2 incubator for 72 hours. Fifty microliters of MTT solution (5 mg MTT in 1 ml PBS and 2.5 ml DMEM media) were added to each well. The plates were further incubated for 4 hours at 37°C in 5% CO2 incubator. The medium was removed and replaced with 200 μl of DMSO to solubilise the MTT formazan product. The solution was mixed for 15 min and once for 30 sec before measuring the absorbance at 540 nm with a micro plate reader (FLUOstar Omega, Germany). The percentage of growth inhibition and the EC50 were estimated from a dose response curve.
Determination of a selectivity index
A selectivity index (SI), corresponding to the ratio between antiplasmodial and cytotoxic activities was calculated according to the following formula:
Results
Antiplasmodial activity against CQ resistant P. falciparum, K1 strain
A total of 54 extracts from different parts of 14 plant species (Table 2) were tested for antiplasmodial activity against chloroquine resistant P. falciparum by using HRP2 assay in vitro. Each part of the plants was extracted by 3 different solvents with increasing polarity (DCM-MeOH-H2O). The discrimination of active extracts is based on ranked levels of antiplasmodial activity proposed by Rasoanaivo et al. [41]. The score for the test is classified as extracts with EC50 value less than 0.1 μg/ml is considered to be very good, 0.1 to 1.0 μg/ml is good, 1.1 to 10 μg/ml is good to moderate, 11 to 25 μg/ml is weak, 26 to 50 μg/ml is very weak while more than 100 μg/ml is considered inactive [41]. So, any extracts which exhibit an EC50 value less than 10 μg/ml (EC50 ≤ 10 μg/ml) is considered to have potential or promising antiplasmodial activity. The antiplasmodial HRP2 assay on the plant extracts were performed in parallel with the standard antimalarial drugs such as CQ, Q, Mef and Art which act as a control for the validity of the assay (Table 3). Briefly, the results of each assay were validated by determination of EC50 values produced by the standard antimalarial drugs against CQ resistant P. falciparum. In this study, the assay is considered valid when the EC50 value of CQ is more than 100 nM [42].
The DCM, MeOH and H2O extracts from 14 plants species showed wide range of antiplasmodial activities (Table 4). Overall 41 extracts (76%) from 13 plant species showed promising antiplasmodial activity (EC50 < 10 μg/ml) (Table 5). In detail, there are 11 extracts from 5 plant species fall within a good level of antiplasmodial activity (EC50 < 1 μg/ml) (Table 5). Good to moderate antiplasmodial activities (EC50 = 1.1-10 μg/ml) were detected in 30 extracts from 12 plant species (Table 5). Thirteen extracts from 6 plant species were considered weak or inactive as these extracts exhibited EC50 values of more than 10 μg/ml or less than 50% parasite inhibition at the highest tested concentration (EC50 > 15.7 μg/ml) (Table 5). Overall, DCM and MeOH extracts were more active against CQ resistant P. falciparum with good level of antiplasmodial activity (Table 5).
Cytotoxicity activity to mammalian MDBK cell line
Forty one extracts from 13 different plant species with promising antiplasmodial activity (EC50 < 10.0 μg/ml), were subjected to MTT cytotoxicity assay and tested against the MDBK cell lines (Table 4). In fact, the pharmacological efficacy of the extracts is considered selective and nontoxic when SI is ≥10 [43]. Twenty three of antiplasmodial plant extracts (DCM, MeOH or H2O) from 11 plant species showed a specific selectivity (SI >10) towards chloroquine resistant P. falciparum, K1 rather than MDBK cells with SI ranging from 10.46 to 756.14 (Table 4). The extract from B. javanica green seed was not tested for MTT assay and has been excluded from this experiment.
Discussion
The present study has identified the antiplasmodial activity in selected plant extracts by HRP2-based assay or HRP2 ELISA technique. There are other reports on antiplasmodial studies using different screening methods such as WHO schizont maturation test [44], isotopic assay [45], pLDH enzymatic assay [46, 47], SYBR Green I assay [48–50] or fluocytometric assay [51]. Briefly, the HRP2-based assay is a very sensitive and specific measures of P. falciparum growth by quantifying parasite specific biomolecule, HRP2. The suitability, reproducibility and sensitivity of HRP2-based assay in antimalarial drug screening is well documented since year 2002 [16, 39, 52–55]. The HRP2-based assay is comparable with other techniques because the result produced by this assay has been previously shown to be closely parallel those obtained from the isotopic assay, traditional WHO schizont maturation tests [54] and SYBR green I assay [56].
Eleven plants (79%) were identified to possess promising antimalarial properties in at least one of their extracts (DCM, MeOH or H2O). These findings are based on their potent antiplasmodial activities (EC50 ≤ 10 μg/ml) and high preferences in killing the malaria parasite rather than mammalian cell line (SI ≥10) (Table 4). Most of the potential antiplasmodial activity were exhibited by DCM and MeOH extracts which may be related to the presence of alkaloids, terpenoids and flavonoids [57, 58]. Theoretically, the purpose of using this extraction technique is to extract specific classes of phytochemical constituents from non-polar compounds to polar compounds [59]. The crude extract of DCM usually contains intermediate polarity of compounds such as alkaloids, steroids and terpenoids [59–61]. These classes of compounds especially alkaloids are well known as active constituents against antiplasmodial activity. In fact, one of the oldest and most known antimalarial drug, quinine belongs to this class of compounds. In addition, an example of common terpenoids is artemisinin, the most potent antimalarial to date [58]. Extraction with methanol will extract more polar compounds such as flavonoid glycosides, saponin, tannins and anthocyanins [59–61]. The antimalarial activity from these classes of compounds especially flavonoids have been described earlier [57]. Further extraction with water will extract high polarity of compounds such as phenolic acids, sugars and glycosides [59–61].
In another point of view, majority of these plants also possessed at least 1% of CQ antiplasmodial activity indicating the potential of these plants to be the source of antimalarial candidates. For example, the ethanolic extract of Artemisia annua Linn leaves (the source of artemisinin) inhibited the growth of CQ resistant (K1) and CQ sensitive (3D7) strains of P. falciparum with IC50 of 10.4 μg/ml and 21.8 μg/ml, respectively [49]. So, even the plant like A. annua with weak antiplasmodial activity (only 0.007% and 0.004% of artesunate activity against P. falciparum K1 and 3D7, respectively) contains the most potent antimalarial compound to date. This phenomenon may also apply to the plants extracted in this study.
In this study, A. galanga (rhizome), C. iners (leaf), C. zedoaria (rhizome), E. scaber (leaf), C. mangga (rhizome) and M. elliptica (leaf) were for the first time reported for their good level of antiplasmodial activities in vitro. Other potent antiplasmodial plants such as C. aeruginosa (rhizome) [62], V. negundo (leaf) [46], B. javanica (leaf and root) [45, 51, 62], A. muricata (leaf) [63] and V. amygdalina (leaf) [44, 64–68] have been widely studied and were further discussed in this section.
A. galanga
The A. galanga has been identified as one of the plants traditionally used in some part of Peninsular Malaysia [11]. The in vitro antiplasmodial data of A. galanga rhizome extracts (EC50 < 10 μg/ml) reported by present study is complementing the in vivo study conducted by Al-Adhroey et al. [11]. The MeOH extract of the rhizome exhibited a significant suppressive, curative and prophylactic activities on P. berghei infected mice. The antimalarial properties of MeOH extract of A. galanga rhizome could be governed by its active constituents such as flavonoids and terpenoids [18]. In addition, both terpenoids and flavonoids related compounds have been previously shown to exhibit antiplasmodial activities against several P. falciparum strains [57].
E. scaber
In this study, the good level of antiplasmodial activity showed by the MeOH extract of E. scaber leaf (EC50 = 0.27 μg/ml) was contradictory to the study reported by Kantamreddi and Wright [46]. According to Kantamreddi and Wright [46], the MeOH extract of the leaves of this plant was considered inactive (IC50 = 133.8 μg/ml) against CQ resistant P. falciparum (K1) [46]. The possible reason for the contradictory results could be due to the differences in the duration of incubation in antiplasmodial assay. The incubation period for the present study is longer (72 hours) than the Kantamreddi and Wright [46] study (48 hours). The 72 hours incubation period allows the activity of the substance to affect the merozoite reinvasion process whereas the 48 hours incubation period will only affect the intraerythrocytic growth of the malaria parasites. In this case, the MeOH extract of this plant might not so effective against the ring to schizont intraerythrocytic stages of P. falciparum. Other species of Elephantopus such as E. mollis have been shown to possess potential antiplasmodial activity (IC50 = 2.2 μg/ml) against CQ resistant P. falciparum (K1) [69].
M. elliptica
To our knowledge, this plant had not yet been investigated for the in vitro antiplasmodial activity. However other species of Morinda, M. morindoides has been shown to exhibit a pronounced antiplasmodial activity [64].
C. iners
The only antiplasmodial study on C. iners was previously reported for its roots extract. However, the MeOH extract of C. iners roots exhibited weak antiplasmodial activity (IC50 = 12.7 μg/ml) against CQ resistant P. falciparum (FCR-3) [21]. In contrast, the leaves extract (MeOH) of this plant which was prepared by present study exhibited a good antiplasmodial activity (EC50 = 0.63 μg/ml) (Table 4). In addition, other Cinnamomun species, C. griffithii has been reported to elicit a promising antiplasmodial activity (IC50 < 10 μg/ml) against both CQ sensitive and resistant P. falciparum strains [70]. To our knowledge, there is no compound related to this plant reported for antiplasmodial activity.
Curcuma sp
The member of the Curcuma plant species such as C. zedoaria, C. mangga, C. aeruginosa and others were well studied for their antiparasiticidal properties [71]. The H2O extracts of C. xanthorriza and C. aeruginosa were previously found to be effective in inhibiting P. falciparum in vitro (40% and 90% inhibition, respectively). However the concentration of the extracts used (1 mg/ml) was too high [62]. Moreover, the major antiplasmodial compounds like curcumin and its derivatives such as demethoxycurcumin and bis-demethoxycurcumin isolated from C. longa exhibited high IC50 value (IC50 > 5 μM) [72]. In contrast, by different technique of plant extraction, the present study showed a promising antiplasmodial activity (EC50 < 10 μg/ml) of C. zedoaria (DCM extract), C. aeruginosa (H2O extract) and C. mangga (MeOH and H2O extracts) with negligible toxic effect on normal cell line (SI >10) (Table 4 and 5). Although the antiplasmodial activity of Curcuma sp isolated compound such as curcumin is considered weak, it was found to be very effective in antimalarial drug combination study [15, 73–75].
V. amygdalina
The V. amygdalina plant is also found in African countries and is widely used traditionally in treating fever, malaria, measles, diabetes, worms, hypertension and others [76, 77]. The ethanol, petroleum ether, methylene chloride and MeOH extracts of V. amygdalina leaf have been previously reported to elicit IC50 values of less than 10 μg/ml against P. falciparum[64, 65]. Both ethanolic and H2O extracts of V. amygdalina leaf has also been shown to inhibit schizont maturation of fresh P. falciparum isolates from patients with negligible toxicity in rats [44]. In addition, the in vivo antimalarial activity of this plant has also been reported [66–68]. In in vivo drug combination experiment, the decoction of V. amygdalina leaves has the ability to enhance the CQ activity in P. berghei infected mice [68]. Furthermore, the infusion of V. amygdalina leaves has been clinically tested against the uncomplicated malaria where the parasite clearance has been documented [78]. So, it is not surprising to see a promising antiplasmodial activity of V. amygdalina leaf extracts (DCM, MeOH and H2O extracts) as showed by the present study (EC50 < 10 μg/ml) (Table 4). The antimalarial property of this plant could be due to the presence of its active constituents, sesquiterpene lactones such as vernolepin, vernolin, vernolide, vernodalin and hydroxyvernodalin [79].
B. javanica
The B. javanica grows in Asia Pacific region including China, Indonesia, Malaysia and Thailand [45]. Different parts of this plant such as fruit, roots, seeds, stems and bark are traditionally used in treating variety of diseases including babesiosis, malaria and cancer. The H2O extract of B. javanica leaves, fruits and bark have been shown to possess a strong antiplasmodial activity against P. falciparum[62]. In the present study, the DCM and MeOH extracts of B. javanica leaves and roots showed good (EC50 < 1 μg/ml) to good to moderate (EC50 = 1.1 to 10 μg/ml) level of antiplasmodial activities against CQ resistant P. falciparum, K1 (Table 4). By similar extraction procedure, the DCM, MeOH and H2O extracts B. javanica roots have also been previously reported to possess a good to moderate level antiplasmodial activity against another CQ resistant P. falciparum strain, W2 with IC50 ranging from 1.0 to 2.0 μg/ml [51]. The antiplasmodial activity showed by this plant might be governed by its active constituents such as quassinoids, alkaloids (bruceacanthinoside) and triterpenoids (Bruceajavanin A and dihydrobruceajavanin A) [80, 81]. Other plant from the same family (Simaroubaceae) like E. longifolia also exhibited an antiplasmodial activity ruled by its quassinoids and alkaloids contents [25, 82]. In addition, the present study has identified the antiplasmodial activity from seeds of this plant (MeOH and H2O extracts). However, the DCM extract of the seeds seem to have weak or no antiplasmodial activity (EC50 > 15.7 μg/ml) (Table 4). In another study with different extraction procedure, the extracts of B. javanica fruits (ethanol, MeOH-ethanol, aqueous-MeOH residue, ethyl acetate and ethyl alcohol extracts) have been shown to have a promising antiplasmodial activity against P. falciparum K1 strain (IC50 < 10 μg/ml). In contrast, the H2O extract of the fruits showed weak antiplasmodial activity (IC50 > 10 μg/ml) [45].
V. negundo
The V. negundo has been traditionally used in India as antiseptic, anti-inflammatory, antipyretic, treating enlargement of spleen and others [83]. The present study has highlighted the potential antiplasmodial activity of DCM (EC50 = 1.1 μg/ml) and MeOH (EC50 = 2.17 μg/ml) extracts of V. negundo leaves against the CQ resistant P. falciparum. The MeOH extracts of V. negundo leaf has been previously shown to exhibit a promising antiplasmodial activity against CQ sensitive (IC50 = 9.5 μg/ml) P. falciparum but not to CQ resistant P. falciparum strain (IC50 = 19.8 μg/ml). In similar study, the MeOH extract of the flower of this plant also exhibited a promising antiplasmodial activity with IC50 value of against CQ sensitive (IC50 = 2.8 μg/ml) but not to CQ resistant P. falciparum (IC50 = 17.8 μg/ml) [46].
A. muricata
As reported by Osorio et al. [63], the hexane, ethyl acetate and MeOH extract of A. muricata leaf exhibited good to moderate level of antiplasmodial activities against CQ sensitive P. falciparum strain F32 (IC50 ranging from 7.2 to 9.2 μg/ml) but not to CQ resistant strain W2 (IC50 ranging from 10.4 to 38.6 μg/ml) [63]. However, the most potent ethyl acetate extracts of this plant is considered toxic to U-937 cells (human monocytes) (SI = 1.1 and 0.2 for F32 and W2 P. falciparum strains, respectively). On the other hand, with different extraction approach, the present study not only showing the promising antiplasmodial activity of A. muricata leaves extracts (DCM, MeOH and H2O extracts) (EC50 < 10 μg/ml), but also the non-toxic activity of the extract to MDBK cells (SI = 66-756) (Table 4 and 5).
Conclusions
Twenty three extracts derived from C. zedoaria (rhizome), C. aeruginosa (rhizome), A. galanga (rhizome), V. negundo (leaf), M. elliptica (leaf), C. mangga (rhizome), E. scaber (leaf), B. javanica (leaf and root), A. muricata (leaf), C. iners (leaf) and V. amygdalina (leaf) showed the best antiplasmodial activities against the blood stage chloroquine resistant P. falciparum with no toxic effects on MDBK cells (SI ≥ 10). The present study has also scientifically supported the efficacy of B. javanica and A. galanga which are used traditionally to treat malaria in Peninsular Malaysia. Although these plant extracts were able to kill the P. falciparum in vitro, further in vivo evaluation is needed to demonstrate their efficacy in treating mammalian malaria model. Furthermore, the bioassay guided fractionation is a way forward for determination of bioactive compounds which will lead to the formulation of new antimalarial drugs or standardized antimalarial extracts.
Authors’ information
All the authors are researchers from Bioassay and Phytochemistry Units of Herbal Medicine Research Centre, Institute for Medical Research, Kuala Lumpur, Malaysia.
References
Abdullah NR, Norahmad NA, Jelip J, Sulaiman LH, Mohd Sidek H, Ismail Z, Noedl H: High prevalence of mutation in the Plasmodium falciparum dhfr and dhps genes in field isolates from Sabah, Northern Borneo. Malar J. 2013, 12 (1): 198-10.1186/1475-2875-12-198.
Norahmad NA, Abdullah NR, Yaccob N, Jelip J, Dony JF, Ruslan KF, Sulaiman LH, Sidek HM, Noedl H, Ismail Z: High prevalence of pfcrt K76t mutants among Plasmodium falciparum isolates from Sabah, Malaysia. Southeast Asian J Trop Med Public Health. 2011, 42 (6): 1322-1326.
Lokman Hakim S, Sharifah Roohi SW, Zurkurnai Y, Noor Rain A, Mansor SM, Palmer K, Navaratnam V, Mak JW: Plasmodium falciparum: increased proportion of severe resistance (RII and RIII) to chloroquine and high rate of resistance to sulfadoxine-pyrimethamine in Peninsular Malaysia after two decades. Trans R Soc Trop Med Hyg. 1996, 90 (3): 294-297. 10.1016/S0035-9203(96)90258-8.
Phyo AP, Nkhoma S, Stepniewska K, Ashley EA, Nair S, McGready R, ler Moo C, Al-Saai S, Dondorp AM, Lwin KM, Singhasivanon P, Day NP, White NJ, Anderson TJ, Nosten F: Emergence of artemisinin-resistant malaria on the western border of Thailand: a longitudinal study. Lancet. 2012, 379 (9830): 1960-1966. 10.1016/S0140-6736(12)60484-X.
Baliraine FN, Rosenthal PJ: Prolonged selection of pfmdr1 polymorphisms after treatment of falciparum malaria with artemether-lumefantrine in Uganda. J Infect Dis. 2011, 204 (7): 1120-1124. 10.1093/infdis/jir486.
Farnert A, Ursing J, Tolfvenstam T, Rono J, Karlsson L, Sparrelid E, Lindegardh N: Artemether-lumefantrine treatment failure despite adequate lumefantrine day 7 concentration in a traveller with Plasmodium falciparum malaria after returning from Tanzania. Malar J. 2012, 11: 176-10.1186/1475-2875-11-176.
Wongsrichanalai C, Sibley CH: Fighting drug-resistant Plasmodium falciparum: the challenge of artemisinin resistance. Clin Microbiol Infect. 2013, 19 (10): 908-916. 10.1111/1469-0691.12316.
Wongsrichanalai C: Artemisinin resistance or artemisinin-based combination therapy resistance?. Lancet Infect Dis. 2013, 13 (2): 114-115. 10.1016/S1473-3099(12)70349-3.
Na-Bangchang K, Muhamad P, Ruaengweerayut R, Chaijaroenkul W, Karbwang J: Identification of resistance of Plasmodium falciparum to artesunate-mefloquine combination in an area along the Thai-Myanmar border: integration of clinico-parasitological response, systemic drug exposure, and in vitro parasite sensitivity. Malar J. 2013, 12: 263-10.1186/1475-2875-12-263.
Willcox M, Burford G, Bodeker G: An overview of ethnobotanical studies on plants used for the treatment of malaria. Traditional Medicinal Plant and Malaria. Edited by: Willcox M, Bodeker G, Rasoanaivo P. 2004, Florida: CRC Press, 187-197.
Al-Adhroey AH, Nor ZM, Al-Mekhlafi HM, Mahmud R: Ethnobotanical study on some Malaysian anti-malarial plants: a community based survey. J Ethnopharmacol. 2010, 132 (1): 362-364. 10.1016/j.jep.2010.08.006.
Ong HC, Chua S, Milow P: Ethno-medicinal plants used by the Temuan villagers in Kampung Jeram Kedah, Negeri Sembilan, Malaysia. Ethno Med. 2011, 5 (2): 95-100.
Ong HC, Nordiana M: Malay ethno-medico botany in Machang, Kelantan, Malaysia. Fitoterapia. 1999, 70: 502-513. 10.1016/S0367-326X(99)00077-5.
Elfawal MA, Towler MJ, Reich NG, Golenbock D, Weathers PJ, Rich SM: Dried whole plant Artemisia annua as an antimalarial therapy. PLoS One. 2012, 7 (12): e52746-10.1371/journal.pone.0052746.
Rasoanaivo P, Wright CW, Willcox ML, Gilbert B: Whole plant extracts versus single compounds for the treatment of malaria: synergy and positive interactions. Malar J. 2011, Suppl 1: S4-
Noedl H, Wernsdorfer WH, Miller RS, Wongsrichanalai C: Histidine-rich protein II: a novel approach to malaria drug sensitivity testing. Antimicrob Agents Chemother. 2002, 46 (6): 1658-1664. 10.1128/AAC.46.6.1658-1664.2002.
Noor Rain A, Khozirah S, Mohd Ridzuan MA, Ong BK, Rohaya C, Rosilawati M, Hamdino I, Badrul A, Zakiah I: Antiplasmodial properties of some Malaysian medicinal plants. Trop Biomed. 2007, 24 (1): 29-35.
Al-Adhroey AH, Nor ZM, Al-Mekhlafi HM, Mahmud R: Median lethal dose, antimalarial activity, phytochemical screening and radical scavenging of methanolic Languas galanga rhizome extract. Molecules. 2010, 15 (11): 8366-8376. 10.3390/molecules15118366.
Wong SK, Lim YY, Abdullah NR, Nordin FJ: Assessment of antiproliferative and antiplasmodial activities of five selected Apocynaceae species. BMC Complement Altern Med. 2011, 11: 3-10.1186/1472-6882-11-3.
Basir R, Chan KL, Yam MF, Othman F, Abdullah WO, Mohd Moklas MA, Abdul Rahim AS, Ismail IS, Hidayat MT, Mat Taib CN, Mahmud R: Antimalarial activity of selected Malaysian medicinal plants. Phytopharmacology. 2012, 3 (1): 82-92.
Wan Omar A, Ngah ZU, Zaridah MZ, Noor Rain A: In vitro and in vivo antiplasmodial properties of some Malaysian plants used in traditional medicine. Infect Dis J Pakistan. 2007, 16 (4): 97-101.
Siti Najila MJ, Noor Rain A, Mohamad Kamel AG, Syed Zahir SI, Khozirah S, Lokman Hakim S, Zakiah I, Azizol AK: The screening of extracts from Goniothalamus scortechinii, Aralidium pinnatifidum and Andrographis paniculata for anti-malarial activity using the lactate dehydrogenase assay. J Ethnopharmacol. 2002, 82 (2–3): 239-242.
Al-Adhroey AH, Nor ZM, Al-Mekhlafi HM, Amran AA, Mahmud R: Evaluation of the use of Cocos nucifera as antimalarial remedy in Malaysian folk medicine. J Ethnopharmacol. 2011, 134 (3): 988-991. 10.1016/j.jep.2011.01.026.
Nasrullah AA, Zahari A, Mohamad J, Awang K: Antiplasmodial alkaloids from the bark of Cryptocarya nigra (Lauraceae). Molecules. 2013, 18 (7): 8009-8017. 10.3390/molecules18078009.
Chan KL, Choo CY, Abdullah NR, Ismail Z: Antiplasmodial studies of Eurycoma longifolia Jack using the lactate dehydrogenase assay of Plasmodium falciparum. J Ethnopharmacol. 2004, 92 (2–3): 223-227.
Ang HH, Chan KL, Mak JW: In vitro antimalarial activity of quassinoids from Eurycoma longifolia against Malaysian chloroquine-resistant Plasmodium falciparum isolates. Planta Med. 1995, 61 (2): 177-178. 10.1055/s-2006-958042.
Chan KL, Choo CY, Abdullah NR: Semisynthetic 15-O-acyl- and 1,15-di-O-acyleurycomanones from Eurycoma longifolia as potential antimalarials. Planta Med. 2005, 71 (10): 967-969. 10.1055/s-2005-864188.
Vejanan V, Latip J, Chin LP, Embi N, Sidek HM: In vitro and in vivo anti-plasmodial activities of Gynura procumbens. Sains Malaysiana. 2012, 41 (12): 1535-1542.
Yapp DT, Yap SY: Lansium domesticum: skin and leaf extracts of this fruit tree interrupt the lifecycle of Plasmodium falciparum, and are active towards a chloroquine-resistant strain of the parasite (T9) in vitro. J Ethnopharmacol. 2003, 85 (1): 145-150. 10.1016/S0378-8741(02)00375-6.
Faridahanim MJ, Abdul Hamid AH, Khalijah A, Nor Hadiani I, Noor Rain A: The screening of the extract from Leuconotis eugenifolius for antimalarial activity using the lactate dehydrogenase assay. Malaysian Medicinal Plants: Chemistry and Biological Activity. Edited by: Ahmad F, Assim Z, Din L, Said IM. 2006, Sarawak, Malaysia: UNIMAS and Malaysian Natural Products Society, 23-26. 1
Zakaria I, Ahmat N, Jaafar FM, Widyawaruyanti A: Flavonoids with antiplasmodial and cytotoxic activities of Macaranga triloba. Fitoterapia. 2012, 83 (5): 968-972. 10.1016/j.fitote.2012.04.020.
Awang K, Mukhtar MR, Hadi AH, Litaudon M, Latip J, Abdullah NR: New alkaloids from Phoebe grandis (Nees) Merr. Nat Prod Res. 2006, 20 (6): 567-572. 10.1080/14786410500183944.
Al-Adhroey AH, Nor ZM, Al-Mekhlafi HM, Amran AA, Mahmud R: Antimalarial activity of methanolic leaf extract of Piper betle L. Molecules. 2011, 16 (1): 107-118.
Najib Nik ARN, Furuta T, Kojima S, Takane K, Ali Mohd M: Antimalarial activity of extracts of Malaysian medicinal plants. J Ethnopharmacol. 1999, 64 (3): 249-254. 10.1016/S0378-8741(98)00135-4.
Osman CP, Ismail NH, Ahmad R, Ahmat N, Awang K, Jaafar FM: Anthraquinones with antiplasmodial activity from the roots of Rennellia elliptica Korth. (Rubiaceae). Molecules. 2010, 15 (10): 7218-7226. 10.3390/molecules15107218.
Burkill IH: A Dictionary of the Economic Products of the Malay Peninsula, Volume I and II. 1966, Ministry of Agriculture Malaysia: Kuala Lumpur, Malaysia
Trager W, Jensen JB: Cultivation of erythrocytic stages. Bull World Health Organ. 1977, 55 (2–3): 363-365.
Lambros C, Vanderberg JP: Synchronization of Plasmodium falciparum erythrocytic stages in culture. J Parasitol. 1979, 65 (3): 418-420. 10.2307/3280287.
Noedl H, Bronnert J, Yingyuen K, Attlmayr B, Kollaritsch H, Fukuda M: Simple histidine-rich protein 2 double-site sandwich enzyme-linked immunosorbent assay for use in malaria drug sensitivity testing. Antimicrob Agents Chemother. 2005, 49 (8): 3575-3577. 10.1128/AAC.49.8.3575-3577.2005.
Mosmann T: Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods. 1983, 65 (1–2): 55-63.
Rasoanaivo P, Ramanitrahasimbola D, Rafatro H, Rakotondramanana D, Robijaona B, Rakotozafy A, Ratsimamanga-Urverg S, Labaied M, Grellier P, Allorge L, Mambu L, Frappier F: Screening extracts of Madagascan plants in search of antiplasmodial compounds. Phytother Res. 2004, 18 (9): 742-747. 10.1002/ptr.1533.
Sidhu AB, Verdier-Pinard D, Fidock DA: Chloroquine resistance in Plasmodium falciparum malaria parasites conferred by pfcrt mutations. Science. 2002, 298 (5591): 210-213. 10.1126/science.1074045.
Weniger B, Robledo S, Arango GJ, Deharo E, Aragon R, Munoz V, Callapa J, Lobstein A, Anton R: Antiprotozoal activities of Colombian plants. J Ethnopharmacol. 2001, 78 (2–3): 193-200.
Sha'a KK, Oguche S, Watila IM, Ikpa TF: In vitro antimalarial activity of the extracts of Vernonia amygdalina commonly used in traditional medicine in Nigeria. Sci World J. 2011, 6 (2): 5-9.
Sriwilaijaroen N, Kondo S, Nanthasri P, Auparakkitanon S, Suzuki Y, Wilairat P: Antiplasmodial effects of Brucea javanica (L.) Merr. and Eurycoma longifolia Jack extracts and their cobination with chloroquine and quinine on Plasmodium falciparum in culture. Trop Med Health. 2010, 38 (2): 61-68. 10.2149/tmh.2009-11.
Kantamreddi VS, Wright CW: Screening Indian plant species for antiplasmodial properties–ethnopharmacological compared with random selection. Phytother Res. 2012, 26 (12): 1793-1799. 10.1002/ptr.4651.
Ondo JP, Lekana-Douki JB, Bongui JB, Zang Edou ES, Zatra R, Toure-Ndouo FS, Elomri A, Lebibi J, Seguin E: In vitro antiplasmodial activity and cytotoxicity of extracts and fractions of Vitex madiensis, medicinal plant of Gabon. Trop Med Int Health. 2012, 17 (3): 316-321.
Bagavan A, Rahuman AA, Kaushik NK, Sahal D: In vitro antimalarial activity of medicinal plant extracts against Plasmodium falciparum. Parasitol Res. 2011, 108 (1): 15-22. 10.1007/s00436-010-2034-4.
Thiengsusuk A, Chaijaroenkul W, Na-Bangchang K: Antimalarial activities of medicinal plants and herbal formulations used in Thai traditional medicine. Parasitol Res. 2013, 112 (4): 1475-1481. 10.1007/s00436-013-3294-6.
Kamaraj C, Kaushik NK, Rahuman AA, Mohanakrishnan D, Bagavan A, Elango G, Zahir AA, Santhoshkumar T, Marimuthu S, Jayaseelan C, Kirthi AV, Rajakumar G, Velayutham K, Sahal D: Antimalarial activities of medicinal plants traditionally used in the villages of Dharmapuri regions of South India. J Ethnopharmacol. 2012, 141 (3): 796-802. 10.1016/j.jep.2012.03.003.
Hout S, Chea A, Bun SS, Elias R, Gasquet M, Timon-David P, Balansard G, Azas N: Screening of selected indigenous plants of Cambodia for antiplasmodial activity. J Ethnopharmacol. 2006, 107 (1): 12-18. 10.1016/j.jep.2006.01.028.
Noedl H, Yingyuen K, Laoboonchai A, Fukuda M, Sirichaisinthop J, Miller RS: Sensitivity and specificity of an antigen detection ELISA for malaria diagnosis. Am J Trop Med Hyg. 2006, 75 (6): 1205-1208.
Noedl H, Attlmayr B, Wernsdorfer WH, Kollaritsch H, Miller RS: A histidine-rich protein 2-based malaria drug sensitivity assay for field use. Am J Trop Med Hyg. 2004, 71 (6): 711-714.
Noedl H, Wernsdorfer WH, Kollaritsch H, Looareesuwan S, Miller RS, Wongsrichanalai C: Malaria drug-susceptibility testing. HRP2-based assays: current data, future perspectives. Wien Klin Wochenschr. 2003, 115 (Suppl 3): 23-27.
Noedl H, Wongsrichanalai C, Miller RS, Myint KS, Looareesuwan S, Sukthana Y, Wongchotigul V, Kollaritsch H, Wiedermann G, Wernsdorfer WH: Plasmodium falciparum: effect of anti-malarial drugs on the production and secretion characteristics of histidine-rich protein II. Exp Parasitol. 2002, 102 (3–4): 157-163.
Bacon DJ, Latour C, Lucas C, Colina O, Ringwald P, Picot S: Comparison of a SYBR green I-based assay with a histidine-rich protein II enzyme-linked immunosorbent assay for in vitro antimalarial drug efficacy testing and application to clinical isolates. Antimicrob Agents Chemother. 2007, 51 (4): 1172-1178. 10.1128/AAC.01313-06.
Batista R, Silva Ade J, de Oliveira AB: Plant-derived antimalarial agents: new leads and efficient phytomedicines. Part II. Non-alkaloidal natural products. Molecules. 2009, 14 (8): 3037-3072. 10.3390/molecules14083037.
Oliveira AB, Dolabela MF, Braga FC, Jacome RL, Varotti FP, Povoa MM: Plant-derived antimalarial agents: new leads and efficient phythomedicines. Part I. Alkaloids. An Acad Bras Cienc. 2009, 81 (4): 715-740. 10.1590/S0001-37652009000400011.
Houghton PJ, Raman A: Laboratory Handbook for the Fractionation of Natural Extracts. 1998, London: Chapman & Hall, 1
Tiwari P, Kumar B, Kaur M, Kaur G, Kaur K: Phytochemical screening and extraction: A review. Internationale Pharmaceutica Sciencia. 2011, 1 (1): 98-106.
Cowan MM: Plant products as antimicrobial agents. Clin Microbiol Rev. 1999, 12 (4): 564-582.
Murnigsih T, Subeki , Matsuura H, Takahashi K, Yamasaki M, Yamato O, Maede Y, Katakura K, Suzuki M, Kobayashi S, Chairul , Yoshihara T: Evaluation of the inhibitory activities of the extracts of Indonesian traditional medicinal plants against Plasmodium falciparum and Babesia gibsoni. J Vet Med Sci. 2005, 67 (8): 829-831. 10.1292/jvms.67.829.
Osorio E, Arango GJ, Jimenez N, Alzate F, Ruiz G, Gutierrez D, Paco MA, Gimenez A, Robledo S: Antiprotozoal and cytotoxic activities in vitro of Colombian Annonaceae. J Ethnopharmacol. 2007, 111 (3): 630-635. 10.1016/j.jep.2007.01.015.
Tona L, Cimanga RK, Mesia K, Musuamba CT, De Bruyne T, Apers S, Hernans N, Van Miert S, Pieters L, Totte J, Vlietinck AJ: In vitro antiplasmodial activity of extracts and fractions from seven medicinal plants used in the Democratic Republic of Congo. J Ethnopharmacol. 2004, 93 (1): 27-32. 10.1016/j.jep.2004.02.022.
Zofou D, Tene M, Ngemenya MN, Tane P, Titanji VP: In vitro antiplasmodial activity and cytotoxicity of extracts of selected medicinal plants used by traditional healers of Western cameroon. Malar Res Treat. 2011, 2011: 561342-
Abosi AO, Raseroka BH: In vivo antimalarial activity of Vernonia amygdalina. Br J Biomed Sci. 2003, 60 (2): 89-91.
Njan AA, Adzu B, Agaba AG, Byarugaba D, Diaz-Llera S, Bangsberg DR: The analgesic and antiplasmodial activities and toxicology of Vernonia amygdalina. J Med Food. 2008, 11 (3): 574-581. 10.1089/jmf.2007.0511.
Iwalokun BA: Enhanced antimalarial effects of chloroquine by aqueous Vernonia amygdalina leaf extract in mice infected with chloroquine resistant and sensitive Plasmodium berghei strains. Afr Health Sci. 2008, 8 (1): 25-35.
Gachet MS, Lecaro JS, Kaiser M, Brun R, Navarrete H, Munoz RA, Bauer R, Schuhly W: Assessment of anti-protozoal activity of plants traditionally used in Ecuador in the treatment of leishmaniasis. J Ethnopharmacol. 2010, 128 (1): 184-197. 10.1016/j.jep.2010.01.007.
Horgen FD, Edrada RA, de los Reyes G, Agcaoili F, Madulid DA, Wongpanich V, Angerhofer CK, Pezzuto JM, Soejarto DD, Farnsworth NR: Biological screening of rain forest plot trees from Palawan Island (Philippines). Phytomedicine. 2001, 8 (1): 71-81. 10.1078/0944-7113-00019.
Haddad M, Sauvain M, Deharo E: Curcuma as a parasiticidal agent: a review. Planta Med. 2011, 77 (6): 672-678. 10.1055/s-0030-1250549.
Rasmussen HB, Christensen SB, Kvist LP, Karazmi A: A simple and efficient separation of the curcumins, the antiprotozoal constituents of Curcuma longa. Planta Med. 2000, 66 (4): 396-398. 10.1055/s-2000-8533.
Nandakumar DN, Nagaraj VA, Vathsala PG, Rangarajan P, Padmanaban G: Curcumin-artemisinin combination therapy for malaria. Antimicrob Agents Chemother. 2006, 50 (5): 1859-1860. 10.1128/AAC.50.5.1859-1860.2006.
Aditya NP, Chimote G, Gunalan K, Banerjee R, Patankar S, Madhusudhan B: Curcuminoids-loaded liposomes in combination with arteether protects against Plasmodium berghei infection in mice. Exp Parasitol. 2012, 131 (3): 292-299. 10.1016/j.exppara.2012.04.010.
Mishra K, Dash AP, Swain BK, Dey N: Anti-malarial activities of Andrographis paniculata and Hedyotis corymbosa extracts and their combination with curcumin. Malar J. 2009, 8: 26-10.1186/1475-2875-8-26.
Toyang NJ, Verpoorte R: A review of the medicinal potentials of plants of the genus Vernonia (Asteraceae). J Ethnopharmacol. 2013, 146 (3): 681-723. 10.1016/j.jep.2013.01.040.
Tabuti JR: Herbal medicines used in the treatment of malaria in Budiope county, Uganda. J Ethnopharmacol. 2008, 116 (1): 33-42. 10.1016/j.jep.2007.10.036.
Challand S, Willcox M: A clinical trial of the traditional medicine Vernonia amygdalina in the treatment of uncomplicated malaria. J Altern Complement Med. 2009, 15 (11): 1231-1237. 10.1089/acm.2009.0098.
Phillipson JD, Wright CW, Kirby GC, Warhurst DC: Phytochemistry of some plants used in traditional medicine for the treatment of protozoal diseases. International Symposium of the Phytochemical Society of Europe. 1993, Lausanne, Switzerland: University of Lausanne, 3-
Kitagawa I, Mahmud T, Simanjuntak P, Hori K, Uji T, Shibuya H: Indonesian medicinal plants. VIII. Chemical structures of three new triterpenoids, bruceajavanin A, dihydrobruceajavanin A, and bruceajavanin B, and a new alkaloidal glycoside, bruceacanthinoside, from the stems of Brucea javanica (Simaroubaceae). Chem Pharm Bull (Tokyo). 1994, 42 (7): 1416-1421. 10.1248/cpb.42.1416.
O'Neill MJ, Bray DH, Boardman P, Chan KL, Phillipson JD, Warhurst DC, Peters W: Plants as sources of antimalarial drugs, Part 4: Activity of Brucea javanica fruits against chloroquine-resistant Plasmodium falciparum in vitro and against Plasmodium berghei in vivo. J Nat Prod. 1987, 50 (1): 41-48. 10.1021/np50049a007.
Kuo PC, Shi LS, Damu AG, Su CR, Huang CH, Ke CH, Wu JB, Lin AJ, Bastow KF, Lee KH, Wu TS: Cytotoxic and antimalarial beta-carboline alkaloids from the roots of Eurycoma longifolia. J Nat Prod. 2003, 66 (10): 1324-1327. 10.1021/np030277n.
Tandon VR: Medicinal uses and biological activities of Vitex negundo. Natural Product Radiance. 2005, 4 (3): 162-165.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6882/14/492/prepub
Acknowledgements
The authors would like to thank the Director General of Health Malaysia for the permission to publish this paper. We thank the Director for the Institute for Medical Research (IMR), Kuala Lumpur for her critical review and support in publishing this paper. The authors also wish to thank the staff of Phytochemistry and Information Units, Herbal Medicine Research Centre, IMR, Kuala Lumpur who has contributed in this study. This study, NMRR-13-424-16108 was supported by the National Institute of Health, Ministry of Health Malaysia.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MRMAR involves manuscript preparation, data interpretation and analysis. AA and RA carried out the plant extraction and cytotoxicity test. NFAJ involves in antiplasmodial screening of plant extracts and data analysis. MIW involves in consultation of plant extraction procedure. SHSZ involves in the preparation of plant specimens for species identification. NRA contributes in overall project design and concept. ZI involves in revising and giving the final approval of the version to be published. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mohd Abd Razak, M.R., Afzan, A., Ali, R. et al. Effect of selected local medicinal plants on the asexual blood stage of chloroquine resistant Plasmodium falciparum . BMC Complement Altern Med 14, 492 (2014). https://doi.org/10.1186/1472-6882-14-492
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6882-14-492