Abstract
Background
No consistent relationship exists between pre-treatment expectations and therapeutic benefit from various complementary and alternative medicine (CAM) therapies in clinical trials. However, many different expectancy measures have been used in those studies, with no validated questionnaires clearly focused on CAM and pain. We undertook cognitive interviews as part of a process to develop and validate such a questionnaire.
Methods
We reviewed questions about expectations of benefits of acupuncture, chiropractic, massage, or yoga for pain. Components of the questions – verbs, nouns, response options, terms and phrases describing back pain – were identified. Using seven different cognitive interview scripts, we conducted 39 interviews to evaluate how individuals with chronic low back pain understood these individual components in the context of expectancy questions for a therapy they had not yet received. Chosen items were those with the greatest agreement and least confusion among participants, and were closest to the meanings intended by the investigators.
Results
The questionnaire drafted for psychometric evaluation had 18 items covering various domains of expectancy. “Back pain” was the most consistently interpreted descriptor for this condition. The most understandable response options were 0-10 scales, a structure used throughout the questionnaire, with 0 always indicating no change, and 10 anchored with an absolute descriptor such as “complete relief”. The use of words to describe midpoints was found to be confusing. The word “expect” held different and shifting meanings for participants. Thus paired items comparing “hope” and “realistically expect” were chosen to evaluate 5 different aspects of treatment expectations (back pain; back dysfunction and global effects; impact of back pain on specific areas of life; sleep, mood, and energy; coping). “Impact of back pain” on various areas of life was found to be a consistently meaningful concept, and more global than “interference”.
Conclusions
Cognitive interviews identified wordings with considerable agreement among both participants and investigators. Some items widely used in clinical studies had different meanings to participants than investigators, or were confusing to participants. The final 18-item questionnaire is undergoing psychometric evaluation with goals of streamlining as well as identifying best items for use when questionnaire length is constrained.
Similar content being viewed by others
Background
Patient expectations of therapeutic benefit are widely thought to be important determinants of treatment outcomes [1–3]. Some studies have suggested that patient expectations of treatment outcomes are one of the most important prognostic factors for patients with back pain [4–6]. However, results from trials of various complementary and alternative medical (CAM) therapies have not consistently supported this belief for musculoskeletal pain [7–10]. The lack of a comprehensive theoretical framework for understanding patient expectations [11] and the paucity of measuring instruments that have been evaluated in relation to participant comprehension and interpretation, reproducibility, and construct validity [3] have impeded progress in understanding how expectations may impact treatment outcomes.
There is disagreement in how best to identify, monitor, and classify patients’ expectations [11, 12]. Literature reviews of expectations have reported that when and how expectations are elicited matters [12]. Other studies have reported the importance of distinguishing between “probability expectations” (rational projections) and idealized expectations (hopes) [11]. Cognitive interviews have not been used when developing previously validated questionnaires of treatment expectations [13–15], even though cognitive interviews have been used when developing other questionnaires designed to assess patient reported outcomes [16, 17]. A recent document from the United States Food and Drug Administration (FDA) recommends cognitive interviews be conducted when developing patient reported outcomes [18].
Here we report our efforts to develop and validate a comprehensive questionnaire for measuring patient expectations of four CAM treatments commonly used for back pain. We chose to focus on back pain because it is the most common musculoskeletal pain condition and the most common pain condition for which people use CAM care [19]. However, we believe that our questionnaire could be modified slightly to capture expectations for other pain conditions.
After reviewing relevant literature and surveying CAM researchers to identify questions that have been used to assess patient expectations of treatments for back pain, we conducted cognitive interviews with low back pain patients to develop and refine questions and identify issues in measurement of patient expectations. Here we describe the content, structure, and meaning of questions and issues identified in cognitive interviews.
Methods
Selection of categories and domains for testing
We used two strategies to identify key components of questions for cognitive testing. First, we conducted qualitative interviews with CAM practitioners regarding their experience with and management of patient expectations [20] and with patients seeking CAM about their treatment expectations. Second, KJS and JT collected extant questions related to participant expectations through two mechanisms: literature searches for published questionnaires on patient expectations; and email queries to acupuncture, chiropractic, massage, and yoga researchers in January of 2010 asking for copies of the questions they used to measure expectations in their trials. (See Additional file 1: Appendix A for researchers contacted, and a representative list of their publications).
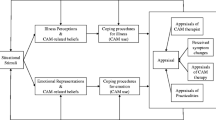
Our patient interviews included questions about back pain history, changes they hoped to see as a result of treatment, expectations they had for the treatments and whether these differed from their hopes. During data analyses, we extracted themes related to expectations and outcomes from the treatment, including the desire for diminished pain and better ability to engage in meaningful activities. We then compared themes from interviews with those from existing questionnaires and from a literature review and a drafted a conceptual model of patient expectations [20]. We thereby identified areas of importance not addressed by existing questions. Once relevant themes were elucidated, KJS reviewed the original battery of questionnaires from CAM researchers and published questionnaires and created a document with potentially relevant questions. CR and KJS then reviewed these questions and compared them with themes from the interviews. They found all of the extant questions contained potential ambiguities that required evaluation by cognitive interviews to elucidate participant understanding. We therefore deconstructed the questions and responses into components so we could test terms and phrases related to expectations, outcome domains, timeframes for improvement, and response options. Additional file 1: Appendix A contains a list of researchers who provided us with copies of expectancy-related questions they had used in prior studies. Additional file 1: Appendix B contains a list of representative citations for researchers listed in Additional file 1: Appendix A.
Cognitive interview methodology
Cognitive interviewing, a prominent method in questionnaire development, is used to detect potential problems with survey questions prior to their widespread use [21–24]. Cognitive interview participants are asked to verbally articulate their thought processes related to selection of responses during or immediately after answering specific questionnaire items [17, 21, 23]. There are two distinct cognitive interviewing paradigms [22, 25]. The “Think-aloud” method requires participants to verbalize their thought process in “real time” as they answer a set of sample survey questions. Retrospective probing or “respondent debriefing” [16] requires participants to complete a set of sample survey questions and immediately respond to detailed probes about the questions.
Because researchers disagree about which method is best [21, 23, 24], we used a combination [25]. For our initial round of interviews, we used retrospective probes to reduce participant burden and to approximate a real experience of responding to actual survey questions. Once we began to finalize terms, response options and question formats, we asked participants to think-aloud as they responded in order to identify additional problems that might not have arisen with our targeted probes. Interviews were conducted via telephone and lasted between 30 and 60 minutes. Each interview contained between 12 and 27 questions, with additional probes depending on the responses.
To refine components of questions into testable questionnaire items, we completed seven rounds of cognitive interviews, each round being concluded when sufficient agreement or disagreement among participants led to adjustments of both items and probes. Within each round, we made minor revisions to address emergent problems and gain additional insight into the reason for a particular problem (e.g. adding a probe to learn why participant definitions of a particular term were inconsistent). Each round included 4 to 11 interviews. Interview guides were prepared in advance and interviewers were instructed to follow scripted probes carefully in order to facilitate analysis and comparability [26]. Where unanticipated concerns were elicited, interviewers were instructed to add probes as appropriate [23].
Table 1 lists all specific terms tested in any of the seven rounds of interviews, and their sources. Initially, we asked participants to define terms related to expectations and back pain. Terms included in the first interview guide can be found in Table 1: Terms and phrases describing expectations (with the exception of think is likely to occur which was added later); back pain; and back dysfunction and global effects. We asked participants to define new terms throughout the seven rounds of interviews. Later rounds combined terms, contrasted them with one another, and tested complete questions with response sets in varying combinations and orders. Interview guides typically contained 10-12 sample questions and 4-6 probes for each sample question. To create clear questions for our domains of interest, we tested a variety of combinations of terms and phrases describing expectations, back pain, and our response options.
Table 2 lists terms tested in each round of interviews. Underlined terms were ultimately selected for use in our draft questionnaire. Italicized terms were eliminated in that round of testing. We typically tested each term in multiple rounds of interviews.
Additional tables provide quotations illustrating findings reported in the main text. For most findings, one quotation was selected that best represented overall findings. In situations where we found inconsistent definitions, multiple quotes are often included to illustrate conflicting views.
The following situations raised concerns about specific questionnaire items: (a) inconsistent responses among participants; (b) responses that differed from our a priori expectations; (c) participants reluctant to answer questions or confused about how to do so; or (d) terms or phrases that our participants found to be ambiguous. We continued to test items in cognitive interviews until a satisfactory level of category saturation [27] was reached. Some items were eliminated quickly, but others required multiple adjustments and rounds of questioning before they were either eliminated or included in the final questionnaire. No items were accepted without being tested in at least two rounds of questioning and in varying order within the questionnaire.
Cognitive interviewing is not intended to yield the best possible question, but rather to provide information to facilitate the design of clear and logical questions [21]. After five rounds of interviews, we sought feedback on a draft questionnaire from seven colleagues with expertise in survey design, CAM research, research on chronic pain, and/or patient expectations. After receiving their feedback, we modified the questionnaire and conducted two additional rounds of cognitive interviews (Table 2). We then drafted a cognitively-informed questionnaire that we will test psychometrically.
Interviewers and training
All four cognitive interviewers had considerable experience in qualitative interviewing and were familiar with the goals of the study. CR had previous experience conducting and analyzing cognitive interviews for questionnaire development [17] and designed and conducted a cognitive interviewer training. Digital recordings were quickly transcribed for immediate review by cognitive interview team members. Rapid turn-around on transcription provided opportunities for assuring comparable interview approach and probing. Weekly teleconference team meetings were the venue for assessing the results of that week’s interviews, modifying the interview process as needed in real time, and making prompt decisions for next steps. The high level of interaction among interviewers and investigators assured comparability across interviewers and sites.
Participant recruitment
We recruited a convenience sample of 39 adults (22 from Arizona, 17 from Washington State) with chronic back pain through recommendations from CAM providers, fliers posted in the community, word of mouth, and internet advertising. Eligibility criteria included: ages 20 to 64; back pain lasting at least 3 months; and no experience with at least one of the four therapies of interest (acupuncture, massage, chiropractic, yoga classes). Participants were not required to be starting a new therapy, but only to express interest in trying one of the four target therapies and to be naïve to that therapy. These inclusion criteria were useful for finding participants who would resemble patients willing to enroll in a clinical trial of CAM. Both the Group Health and University of Arizona Institutional Review Boards determined that these cognitive interviews were “not Human Subjects Research” because the questions were non-sensitive, hypothetical and used for questionnaire development and therefore did not require that we provide formal informed consent. However, prospective participants who responded were provided with a brief description of the study and screened for eligibility. Eligible participants were provided with complete study description, an explanation of cognitive interviews, and information about privacy and protection of the data collected.
Data analysis
Cognitive interviews were audio-recorded and transcribed verbatim. Interview transcripts were later coded using qualitative data analysis software (ATLAS.ti, Version 6.0 [28]) by EE, an interviewer experienced in coding and analyzing qualitative data. Coding was helpful for confirming or refuting initial impressions and for organizing the data for presentation to the study team.
Because interviewers had been instructed to use scripted probes and improvised only to elicit additional data, coding was simple and typically aligned with pre-determined domains and areas of interest. 86 codes covered the terms tested (e.g. terms about expectation, response anchors), outcome domains (e.g. back pain, sleep, mood, energy, coping), timeframe and response options (e.g. 0-10 scale, percentage scale, participant defined scale), and comments pertaining to a specific question (e.g. questions originally used by DC and KJS or specific questions created based on participant comments).
Results
Components of the questions
Terms and phrases describing expectations
We tested numerous terms to see how useful they were in eliciting meaningful responses related to expectancy (Table 1). In the first round of interviews, we asked participants to define each term and tell us which they preferred. In later rounds of interviews we continued to clarify which terms were most consistently defined and most meaningful to participants. Table 3 provides relevant quotes for each term.
Originally, we anticipated the term expect, which participants consistently defined as what people think will happen as a result of treatment, would be the best way to ask about this belief. However, after several rounds of cognitive testing, we learned that expect was not actually used consistently when participants responded to sample questions containing the term (Table 3). Some participants answered based on their hopes while others considered both their hopes and expectations. Participants initially defined the terms expect and realistically expect similarly. However when probed, they described realistically expect as more narrowly focused on what one really thinks will happen without consideration of one’s hopes (Table 3). Some participants said the word “realistically” made them think about what they really thought would occur.
In cognitive interviews, participants defined hope as what they wished for or wanted to occur at the highest levels of aspiration, unconstrained by reality, prior knowledge or experience (Table 3). Some participants said hope includes emotional aspects of what is expected. By contrast, the term expect is more realistic. Based on these findings, we chose to pair questions about hope with questions about realistically expect in our questionnaire in order to tease apart blind hopes from more realistic beliefs.
One of our expert reviewers recommended we use the phrase think is likely to occur (Table 3) instead of realistically expect. Our participants defined these two phrases similarly. When we compared numerical responses to both survey items, however, we found that participants typically used the same numerical rating for think is likely to occur as they used for the question immediately preceding it (e.g. a high number if it followed a question containing hope; a low number if it followed a question containing realistically expect). In contrast, responses to realistically expect and hope were consistently divided and did not seem to fluctuate with question order. We therefore eliminated think is likely to occur from further consideration.
Other terms tested
Think, feel, and believe (Table 3) were tested as ways to ask participants about their expectations for treatment outcome (e.g. How successful do you feel the treatment will be in relieving your back pain?). We eliminated them because, compared to realistically expect and hope, they did not elicit consistent responses about participant expectations and anticipated outcomes.
Participants found personally expect redundant, since they assumed all questions were about their beliefs. We eliminated really think because participants described feeling as though this questioned their honesty, which this had a negative connotation.
We eliminated helpful, successful, confident, and hopeful because participants defined them inconsistently or we found them less useful in capturing expectations (Table 3). Helpful was defined by some as steps toward relieving pain, and by others as related to consequences of improvement in pain. Successful was defined by some participants as a marked improvement, while others thought this meant that the treatment worked as expected. Success seemed focused on the end of the treatment period and did not imply long-term improvement. Confident was not consistently defined (Table 3). Hopeful was distinct from hope (described above) and was consistently defined as a broadly wishful or optimistic approach. Hopeful is less goal-oriented than hope and we therefore chose to use the term hope in our draft questionnaire due to its association with more specific outcomes.
Domains of outcome expectations
Back pain
In order to assess the usefulness and meaningfulness of different terms used to describe back pain, we cognitively tested several terms or phrases used by past researchers, including: back condition; back pain; and back pain problems (Table 4). In the first round of interviews, participants were asked to describe the meaning of each term or phrase independently, and then to compare them to one another.
Of the three terms describing pain, participants understood back pain most clearly. They consistently defined back pain as the physical experience of pain, while back condition was described as a more anatomical or diagnostic term that some participants did not believe was relevant to their symptom experience. Back pain problems was slightly more ambiguous, referring to the physical problems associated with back pain according to some respondents, and to how back pain interferes with life for others.
Back pain: average/current/worst
We also tested the value of specifically asking about average pain, worst pain, and current pain (Table 4). When asking participants whether they had described their average pain, current pain or worst pain, most (6 of 7) said they had described average pain. While they preferred average pain to the other terms, they preferred to think about areas of highest importance for them, or to answer based on a broader average. Participants had trouble compartmentalizing pain into these categories. They reported it was easier to respond if they could consider both the severity of acute episodes and the constant presence of low or mid-level pain. They did not believe that the term average pain captured these considerations. Based on these findings, we elected to use back pain in our draft questionnaire without additional qualification.
Back dysfunction and global effects
To evaluate appropriate terms for describing “back dysfunction” [29] and “global improvement” [30] we tested: limitations due to back pain; impact of back pain on your life; and how back pain interferes with your life (Table 4). Participants said both limitations due to back pain and how back pain interferes with your life referred specifically to physical limitations. Limitations and interference were consistently understood to mean physical inability to complete specific tasks. However, the impact of back pain on participants’ lives was consistently defined more broadly. It included less tangible aspects of life such as irritability, mood, energy, sleep, and “lightness of being”. All of these domains were explicitly not considered to be “interference” and respondents did not include them when answering sample questions about interference. For example, some participants with back pain who continued to do their normal activities reported no interference. However, the same participants reported that the back pain impacted them by increasing irritability, decreasing their enjoyment or “ease and joy” in completing tasks and therefore had a significant impact on their life.
Impacts of back pain on specific areas of life
We included some questions about expectations related to specific areas of life that back pain could affect but that participants might not have routinely considered as part of general questions about expectations of treatment (Table 4).
Specifically, we tested questions about: (a) impact of back pain on work, including housework; (b) impact of back pain on social and recreational activities; (c) impact of back pain on daily activities; and (e) impact of back pain on relationships with family and friends. Impact of back pain on work was important to include because some participants felt was the most important area of impact while others said they tended to power through pain while at work in ways they could not in other circumstances. Many participants had eliminated sports or other leisure activities from their lives, and did not always consider these activities when responding to general questions about impact of back pain on life. Daily activities were defined by participants as a focus on active times or things that needed attention on a daily basis, rather than on an impact in general. Relationships with family and friends was the domain in which many participants said they were most likely to be impacted by their pain. Families were impacted by negative moods stemming from pain, although this was rarely mentioned in responses to more general questions.
Sleep, mood, and energy
Poor sleep is a known consequence of back pain for many patients [31]. We used the phrase back-related sleep problems since some participants said they reported sleep problems unrelated to pain (Table 4).
We decided to include questions about mood and energy[30] as some participants reported difficulties in these areas as consequences of back pain (Table 4) [32]. Participants’ found these terms straightforward. For these two domains, participants reported they might expect treatment to have benefits not directly correlated to reduction in pain.
Coping
We included coping as a domain of experience because improvement in coping was distinct from improvement in pain (Table 4). Our participants defined coping as the mental ability to carry on in spite of pain. Participants distinguished between coping and self-care very consistently in our interviews. While coping was the ability to handle pain, self-care referred to one’s ability to employ various strategies aimed at decreasing or preventing pain.
Timeframe for improvement
We wanted to assess participants’ short-term and long-term expectations. We tried several terms, including end of the treatment period and one year from now. Participants thought the term at the end of the treatment period typically referred to a period between 6 weeks and 6 months, with most (7 of 10) thinking this was 10 weeks to 3 months.
Given the high degree of agreement, we left the end of the treatment period open, though it could be clarified for future studies if needed. To ask about expectations of long-term outcomes, we tested multiple versions of a question about expectations for one year from now. Simply asking what participants expected one year from now was confusing because some participants could not predict long-term outcomes in the absence of knowing the short-term results. Other participants did not know whether they should include other treatments they might do during the year. We therefore explained that participants should include the current course of treatment they are seeking, plus any self-care or other health care they anticipated completing during that time period. By including this domain in our questionnaire, we can test whether participants expect their treatments would have short term benefits for back pain or would have more lasting benefits.
Components of the responses
Response options
Overall, we found participants preferred response options that were consistent throughout the questionnaire, that numerical options elicited more consistently meaningful responses than word sets, and that numerical rating scales were the most intuitive for participants because they were typically asked about pain on a similar scale in health care settings.
Word sets
We tested several types of word sets as potential response options (Table 5). Although some participants said they preferred word options, many reported difficulty in remembering the words during their telephone interview. In addition, the meanings of some words differed among participants, and having words define each option made the scales appear non-linear to participants. Finally, participants found it easier to be asked questions using the same scale throughout the interview.
We tested Likert scales reflecting degree of endorsement. Responses included: strongly disagree; moderately disagree; a little disagree; neither agree nor disagree; a little agree; moderately agree; strongly agree (used by [33, 34] and more recently by Younger et al. [15]. To test this set of responses, we adapted four items from Mao’s validated “Acupuncture Expectancy Scale” expectations of acupuncture [35, 36] (Mao)a: 1) “my pain will improve a lot”; 2) “I will be better able to cope with my pain”; 3) “my pain will go away”; and 4) “my energy level will improve”. We discovered that participants were confused about the use of these response options (Table 5 for examples on items 1, 2 and 4). Respondents reported different interpretations of these questions when telling us how they answered these questions. They had trouble reconciling the value judgment in the stem (improve, get better) with a value judgment in the response category (moderately, strongly). Furthermore, when given hypothetical scenarios respondents did not consistently select the same response category.
For example, responses to item 2 (ability to cope) revealed general issues with agree/disagree responses as demonstrated by responses to two scenarios. Scenario (1): Participants were asked, “If you thought your pain would be completely gone, how would you answer this question?” All three participants said they would strongly agree. Scenario (2): participants were asked “If you thought your pain would stay the same but you would have new tools for dealing with it, how would you answer this question?” In response, all three participants also said they would strongly agree. In this example, two different situations elicited the same response. These responses would be hard to interpret if researchers could not distinguish whether a response of “strongly agree” meant a participant expected little relief from pain, but better coping, or significant relief from pain.
Numerical response options
When asked to define their own scales in response to questions about outcome expectations, all participants selected a numerical scale with the smallest number (0 or 1) representing no change and the largest (5 or 10) representing the best possible outcome (Table 5). No participants preferred a 0-100 scale because the large number of choices was too great for general questions about expectations. Some participants conflated percentage with a 100-point scale. Ultimately, we eliminated percentages in order to use a consistent format for all response options. The 0-10 scale was preferred by most participants, being described as more intuitive, more familiar, and allowing them to communicate their anticipated improvement with a reasonable amount of precision.
Anchors
After determining that participants preferred a 0 to 10 scale, we tested several possible phrases for the upper and lower anchors as well as a possible midpoint (Table 5). Participants preferred word anchors that described absolute amounts of improvement (e.g., “no change” or “complete relief”) as opposed to relative improvement (e.g., “worst pain imaginable”). Our anchors were tested and modified over several rounds of interviews to determine the best fit for each question and to elicit the most consistent responses.
We eliminated midpoint anchors because participants often did not agree on the definition of the word and relied too heavily on the midpoint anchor rather than choosing an answer based on their own expectations. One participant changed her answer when a midpoint was used because she perceived that definition was below her idea of the midpoint. For most of our questions, the lower anchor “no change/worse” was clearly understood and elicited the most consistent and meaningful responses. Upper anchors were tailored to specific questions. For back pain related questions, the upper anchor “complete relief” was found to be most clear and consistent. For questions related to limitations due to back pain, we chose “limitations completely resolved” and for questions related to impact of back pain on life we chose “back pain no longer impacts my life”. When asking about specific items, we adjusted this anchor to “back pain no longer impacts my: sleep, energy, work, etc”. For our coping question (#8 in draft questionnaire, Additional file 1: Appendix C), “no improvement” to “extreme improvement” was found to be the most meaningful anchor pair after testing several questions and anchor sets.b
Overall structure of questions
In the course of our cognitive interviews, we found that respondents had difficulty specifying the likelihood of a specific outcome (e.g., cure, substantial improvement, better coping). Rather, they wanted to tell us how much improvement they expected. For example, one participant responded to the item, “my pain will improve a lot” by saying that she was “making in [her] mind [her] own rating system which these [response options] represent” (SEA-416) to allow her to communicate how much improvement she expected. Rather than use the response options as intended, she described changing the scale in a way that enabled her to convey the meaning she intended to convey. Another participant, when asked how likely the treatment was to substantially reduce back pain, said “I know that the question was slightly different [from how much improvement do you expect], but … I think I kind of was answering it the same way. … In the back of my mind I was thinking about what I expected in terms of relief from pain [rather than speculating on the likelihood of the statement provided].” (AZ-511).
This pattern of participant comments and responses led us to think that the ideal question structure would be: “how much change do you [realistically expect] in your [outcome of interest, e.g. back pain]?” where the bracketed ([ ]) terms could vary. The best response options associated with these questions is a scale of zero to ten where zero is “no change or worse” and ten is “[customized version of relief of the problem, e.g. complete relief]”. For example: “On a scale of zero to ten, where zero is no change or worse and ten is complete relief, how much change do you realistically expect in your back pain?”
Discussion
We have presented findings from the cognitive interviewing phase of our study aimed at creating a questionnaire for more accurately measuring patient expectations of CAM therapies. Through these interviews, we gained insight into a number of key problems that might arise with existing questions now used to assess patient expectations in clinical trials. These key difficulties would not have emerged without cognitive interviewing. Key findings from these interviews included: (1) participants used the term expect in an ambiguous way, encompassing both hopes and realistic expectations; (2) participants had difficulty in determining their “average” or “current” pain, in contrast to their lack of difficulty thinking about their back pain in more general terms, i.e. “your back pain”; (3) participants reported a difference between physical limitations and impact of back pain on life and tended not to report important aspects of impact on life when asked only about limitations; (4) participants did not consider some specific areas of impact unless asked directly (e.g. leisure activities); (5) participants identified sleep, mood, and energy as important areas of potential improvement, independent of pain; (6) participants were confused about the meaning of “improvement in coping” (wondering whether “better coping” did or did not imply a decrease in pain); (7) participants had trouble assessing long-term expectations, which were contingent on a number of lifestyle and other factors; (8) participants adapted some categories of response options to convey what they wanted to communicate with researchers rather than providing the information the question was intended to elicit; (9) participants had problems with response options based on word (as opposed to numeric) descriptors both in relation to ability to recall them (in telephone interviews) and to varying interpretations of word meanings; (10) participants preferred anchors that specified absolute amounts of improvement; and (11) participants desired to communicate how much improvement they expected rather than their speculations on the likelihood of specific outcomes. In order to elicit meaningful, consistent responses, questions need to be framed to take these issues into account.
Other researchers have distinguished between “probability expectations” (what participants think is likely to happen) and “value expectations” (what participants want, feel they need, feel they are due, or what they hope for) [11, 12]. While we did not base our cognitive interview questions on these distinctions, they are useful for explaining the reasoning behind our inclusion of both hope and realistically expect in our questionnaire items. Since participants seemed compelled to disclose their hopes along with any admission of “realistic” expectations, it was important to ask about both, even if we were primarily interested in the latter. In interviews with individuals beginning a new CAM therapy in an earlier phase of this study, we found that participants often described both their hopes and what they really thought would happen when they were asked what they expected from treatment. Eaves et al. [37] provide a framework for distinguishing between different kinds of hope and show how hope is tightly bound to individuals’ assessments of their expectations, experiences, and outcomes of a treatment.
Our findings indicate that cognitive interviews serve an important purpose in survey design. Many questions initially favored by members of the research team and suggested by other experts turned out to present unforeseen interpretation challenges to participants. Our findings are an important reminder to researchers intending to create new questions: researchers’ understandings and usages of words and phrases may differ from those of study participants. Cognitive interviews are instrumental for learning how participants will interpret questions and what meanings participants are attempting to convey with their responses. The latter issue is important not only to ensure validity and consistency of responses, but also to ensure that questions capture what is most important to participants.
Our findings have implications for selecting outcome measures for clinical trials evaluating treatments for back pain, especially treatments utilizing novel therapies. They suggest that some standard questions used in back pain research to measure expectations are more challenging for patients to answer and may need to be reconsidered. If corroborated in other patient populations, our findings strongly suggest that some question structures (such as endorsement of the likelihood of particular outcomes) are problematic regardless of whether they have been validated.
Cognitive interviews add unique insights that complement other tools we have for survey development such as open-ended qualitative interviewing and conceptual analysis or quantitative psychometric analysis of survey responses. Cognitive interviews allow for the blending of quantitative and pattern analysis of numerical rating as well as the qualitative aspects of participants’ discussions of the meaning of those ratings. For example, we found that asking participants what they thought was “likely to occur” as a result of treatment was problematic. The weakness of this term in eliciting the desired information was revealed only when the numerical responses chosen by participants were compared to their descriptions of their intended response and the changes in descriptions and responses when the order of questions was adjusted. Although some researchers may have little experience with this technique and it seems to be infrequently reported, Cognitive Interviewing has been recommended by the Food and Drug Administration (FDA) as part of the development of Patient Reported Outcome (PRO) measures as it is key in ensuring understanding and completeness of conceptual content of questions [18].
In addition to our specific findings, we offer the following insights to researchers planning to conduct cognitive interviews: (1) employing both retrospective probing and “think-aloud” cognitive interviews may elicit a range of issues and help to clarify questions; (2) attention to both participants’ descriptions of their response choices and intended meaning as well as to numerical patterns in their responses is key to understanding data after it has been collected; and (3) gaining an understanding of what participants’ want researchers to learn, and creating questions that elicit that information, leads to more consistent and meaningful responses.
Limitations
While we anticipate that our results are broadly applicable among English-speaking North Americans, due to cultural differences in health care and social discourse on pain these results should probably be confirmed in local pilot studies prior to use in other English-speaking countries. Translation into other languages will necessitate additional work using standard protocols for survey translation.
Conclusions
Our goal of creating a standard questionnaire to measure expectations at the beginning of clinical trials is intended to contribute to understanding the complex relationships of patient expectations and treatment outcomes. The cognitive interview phase of our project has added a level of clarity to our questions that we hope will assist our final questionnaire in eliciting information that is not only meaningful to research participants, but also better suited to provide clear data on the links (if, in fact, there are any) between participant expectations and treatment outcomes.
The final steps in our research include: (1) psychometric evaluation of our draft questionnaire in both clinical and clinical trial populations and (2) analysis of outcomes data collected in clinical trials administering the questionnaire. Once these additional steps have been completed, we will provide the research community with a questionnaire on expectations developed specifically for use in CAM settings that they may choose to use in their own future research.
Endnotes
aMao’s original scale contains the following responses: “not at all agree; a little agree; moderately agree; mostly agree; completely agree”, the study team elected to use “strongly disagree; moderately disagree; slightly disagree; neither agree nor disagree; slightly agree; moderately agree; strongly agree”.
bWe recognize that “extreme improvement” does not fit with our finding that the upper anchor should communicate an absolute amount of improvement. However, as described in relation to Mao’s coping question [35] above, improvement in coping is not necessarily correlated to improvements in pain and is therefore problematic. We chose to include this domain, but found that the word anchors that best described this question differed from those in other questions.
Abbreviations
- CAM:
-
Complementary and alternative medicine
- FDA:
-
Food and drug administration
- PRO:
-
Patient reported outcome.
References
Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H: The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review. Health Technol Assess. 1999, 3: 1-96.
Constantino MJ, Arnkoff DB, Glass CR, Ametrano RM, Smith JZ: Expectations. J Clin Psychol. 2011, 67: 184-192. 10.1002/jclp.20754.
van Hartingsveld F, Ostelo RWJG, Cuijpers P, de Vos R, Riphagen II, de Vet HCW: Treatment-related and patient-related expectations of patients with musculoskeletal disorders: a systematic review of published measurement tools. Clin J Pain. 2010, 26: 470-488. 10.1097/AJP.0b013e3181e0ffd3.
Bialosky JE, Bishop MD, Cleland JA: Individual expectation: an overlooked, but pertinent, factor in the treatment of individuals experiencing musculoskeletal pain. Phys Ther. 2010, 90: 1345-1355. 10.2522/ptj.20090306.
Bishop MD, Bialosky JE, Cleland JA: Patient expectations of benefit from common interventions for low back pain and effects on outcome: secondary analysis of a clinical trial of manual therapy interventions. J Man Manip Ther. 2011, 19: 20-25. 10.1179/106698110X12804993426929.
Iles R, Davidson M, Taylor N, O’Halloran P: Systematic review of the ability of recovery expectations to predict outcomes in Non-chronic Non-specific Low back pain. J Occup Rehabil. 2009, 19: 25-40. 10.1007/s10926-008-9161-0.
Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA: Lessons from a trial of acupuncture and massage for Low back pain: patient expectations and treatment effects. Spine. 2001, 26: 1418-1424. 10.1097/00007632-200107010-00005.
Linde K, Witt CM, Streng A, Weidenhammer W, Wagenpfeil S, Brinkhaus B, Willich SN, Melchart D: The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain. 2007, 128: 264-271. 10.1016/j.pain.2006.12.006.
Sherman KJ, Cherkin DC, Ichikawa L, Avins AL, Delaney K, Barlow WE, Khalsa PS, Deyo RA: Treatment expectations and preferences as predictors of outcome of acupuncture for chronic back pain. Spine. 2010, 35: 1471-1477.
Thomas KJ, MacPherson H, Thorpe L, Brazier J, Fitter M, Campbell MJ, Roman M, Walters SJ, Nicholl J: Randomised controlled trial of a short course of traditional acupuncture compared with usual care for persistent non-specific low back pain. BMJ. 2006, 333: 623-10.1136/bmj.38878.907361.7C.
Haanstra TM, Hanson L, Evans R, Nes FA, Vet HCW, Cuijpers P, Ostelo RWJG: How do low back pain patients conceptualize their expectations regarding treatment? Content analysis of interviews. Eur Spine J. 2013, 22: 1986-1995. 10.1007/s00586-013-2803-8.
Kravitz RL: Measuring Patients' expectations and requests. Ann Intern Med. 2001, 134: 881-888. 10.7326/0003-4819-134-9_Part_2-200105011-00012.
Borkovec TD, Nau SD: Credibility of analogue therapy rationales. J Behav Ther Exp Psychiatry. 1972, 3: 257-260. 10.1016/0005-7916(72)90045-6.
Mao J, Armstrong K, Farrar J, Bowman M: Acupuncture expectancy scale: development and preliminary validation in China. EXPLORE. 2007, 3: 372-377. 10.1016/j.explore.2006.12.003.
Younger J, Gandhi V, Hubbard E, Mackey S: Development of the Stanford Expectations of Treatment Scale (SETS): a tool for measuring patient outcome expectancy in clinical trials. Clin Trials. 2012, 9: 767-776. 10.1177/1740774512465064.
Irwin DE, Varni JW, Yeatts K, DeWalt DA: Cognitive interviewing methodology in the development of a pediatric item bank: a patient reported outcomes measurement information system (PROMIS) study. Health Qual Life Outcomes. 2009, 7: 1-10. 10.1186/1477-7525-7-1.
Thompson JJ, Kelly KL, Ritenbaugh C, Hopkins AL, Sims CM, Coons SJ: Developing a patient-centered outcome measure for complementary and alternative medicine therapies II: refining content validity through cognitive interviews. BMC Complement Altern Med. 2011, 11: 136-153. 10.1186/1472-6882-11-136.
Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Book Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. 2006, City: FDA Center for Drug Evaluation and Research; FDA Center for Biologics Evaluation and Research; FDA Center for Devices and Radiological Health, 4: 79-
Barnes PM, Bloom B, Nahin RL: Complementary and Alternative Medicine Use Among Adults and Children: United States, 2007. Book Complementary and Alternative Medicine Use Among Adults and Children: United States. 2007, City, 12: 2008-
Schafer LM, Hsu C, Eaves ER, Ritenbaugh C, Turner J, Cherkin DC, Sims CM, Sherman KJ: Complementary and alternative medicine (CAM) providers’ views of chronic low back pain patients’ expectations of CAM therapies: a qualitative study. BMC Complement Altern Med. 2012, 12: 234-10.1186/1472-6882-12-234.
Beatty PC, Willis GB: Research synthesis: the practice of cognitive interviewing. Pub Opin Q. 2007, 71: 287-311. 10.1093/poq/nfm006.
Drennan J: Cognitive interviewing: verbal data in the design and pretesting of questionnaires. J Adv Nurs. 2003, 42: 57-63. 10.1046/j.1365-2648.2003.02579.x.
Willis GB: Cognitive Interviewing: A Tool for Improving Questionnaire Design. 2005, Thousands Oaks: Sage Publications
Conrad F, Blair J, Tracy E: Verbal reports are data! A theoretical approach to cognitive interviews. Proceedings of the 1999 Federal Committee on Statistical Methodology Research Conference. 1999, Washington, DC: Office of Management and Budget
Renberg T, Kettis Lindblad Å, Tully MP: Testing the validity of a translated pharmaceutical therapy-related quality of life instrument, using qualitative ‘think aloud’ methodology. J Clin Pharm Ther. 2008, 33: 279-287. 10.1111/j.1365-2710.2008.00921.x.
Conrad F, Blair J: Data Quality in Cognitive Interviews: The Case of Verbal Reports. Methods for Testing and Evaluating Survey Questions. Edited by: Presser S, Rothgeb JM, Couper MP, Lessler JT, Martin E, Martin J, Singer E. 2004, John Wiley & Sons, Inc
Strauss AL, Corbin JM: Basics of Qualitative Research: grounded theory procedures and techniques. 1990, Newbury Park, California: Sage Publications
Muhr T: ATLASti Qualitative Data Analysis Program. Book ATLASti Qualitative Data Analysis Program. 2011, City: ATLAS.ti Scientific Software Development GmbH, 60
Bombardier C: Outcome assessments in the evaluation of treatment of spinal disorders: summary and general recommendations. Spine. 2000, 25: 3100-3103. 10.1097/00007632-200012150-00003.
Turk DC, Dworkin RH, Allen RR, Bellamy N, Brandenburg N, Carr DB, Cleeland C, Dionne R, Farrar JT, Galer BS: Core outcome domains for chronic pain clinical trials: IMMPACT recommendations. Pain. 2003, 106: 337-345. 10.1016/j.pain.2003.08.001.
van de Water A, Eadie J, Hurley DA: Investigation of sleep disturbance in chronic low back pain: an age-and gender-matched case-control study over a 7-night period. Man Ther. 2011, 16: 550-556. 10.1016/j.math.2011.05.004.
White P, Lewith G, Hopwood V, Prescott P: The placebo needle, is it a valid and convincing placebo for use in acupuncture trials? A randomised, single-blind, cross-over pilot trial. Pain. 2003, 106: 401-409. 10.1016/j.pain.2003.08.013.
Pariente J, White P, Frackowiak RS, Lewith G: Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. Neuroimage. 2005, 25: 1161-1167. 10.1016/j.neuroimage.2005.01.016.
Moyer CA, Rounds J: The Attitudes toward Massage (ATOM) scale: reliability, validity, and associated findings. J Bodyw Mov Ther. 2009, 13: 22-33. 10.1016/j.jbmt.2008.01.002.
Mao J, Armstrong K, Farrar J, Bowman M: Acupuncture expectancy scale: development and preliminary validation in China. EXPLORE (NY). 2007, 3: 372-377. 10.1016/j.explore.2006.12.003.
Mao J: Validation of acupuncture expectancy scale in cancer patients. Book Validation of acupuncture expectancy scale in cancer patients. 2009, City
Eaves ER, Ritenbaugh C, Nichter M, Hopkins AL, Sherman KJ: Modes of hoping: understanding hope and expectation in the context of a clinical trial of complementary and alternative medicine for chronic pain. EXPLORE (NY). In press
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6882/14/39/prepub
Acknowledgements
The authors would like to thank Rene Hawkes and Melissa Parsons for serving as interviewers and offering their experience in survey creation for this phase of the study. We would also like to thank the participants who completed these very tedious cognitive interviews. We thank the 23 researchers who responded to our request for copies of their questions related to expectations. We thank Carol Greco, Roni Evans, Mark Jensen, Ted Kaptchuk, George Lewith, Charlotte Paterson and Kevin Ulrich for helpful comments on a draft of the survey. This research was funded by the National Center for Complementary and Alternative Medicine (NCCAM) of the National Institutes of Health (R01AT005809). The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare they have no competing interests.
Authors’ contributions
KJS is the Principal Investigator; she conceived of and designed the overall study, participated in a review of the literature and contacting CAM researchers for copies of the questions on expectancy they had used in prior studies, participated in creating and revising interview guides, analyzing data, compiling a draft questionnaire, contacting content experts to review the draft questionnaire, and drafting and revising the manuscript. ERE participated in creating and revising the interview guides, interviewing participants, coding and analyzing data, and drafting and revising the manuscript. CR participated in design and conceptualization of the overall study and the cognitive interviewing phase of the study, creating and revising interview guides, training cognitive interviewers, coding and analyzing data, compiling a draft questionnaire, and drafting and revising the manuscript. CH participated in creating and revising interview guides, interviewing participants, compiling a draft questionnaire, and provided important intellectual insight and revision of the manuscript. DC participated in the design of the overall study, contributed important intellectual insight and revisions to the manuscript. JT participated in the design of the overall study, reviewing the literature, contacting content experts to review the draft questionnaire, compiling a draft questionnaire, and contributed important intellectual insight and revisions to the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
12906_2013_1639_MOESM1_ESM.docx
Additional file 1: Appendix A. List of researchers responding to requests for contributions of expectancy-related questions used in their clinical trials. Appendix B. Representative citations for authors contributing questionnaire items or with published questionnaires of interest. Appendix C. Draft EXPECT Questionnaire (after Cognitive Testing). (DOCX 40 KB)
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Sherman, K.J., Eaves, E.R., Ritenbaugh, C. et al. Cognitive interviews guide design of a new CAM patient expectations questionnaire. BMC Complement Altern Med 14, 39 (2014). https://doi.org/10.1186/1472-6882-14-39
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6882-14-39