Abstract
Background
Alternanthera sessilis is used by folk medicinal practitioners of Bangladesh for alleviation of severe pain. The objective of this study was to scientifically analyze the analgesic (non-narcotic) property of aerial parts of the plant along with antihyperglycemic activity.
Methods
Antihyperglycemic activity was measured by oral glucose tolerance tests. Analgesic (non-narcotic) activity was determined by observed decreases in abdominal writhings in intraperitoneally administered acetic acid-induced pain model in mice.
Results
Administration of methanol extract of aerial parts led to dose-dependent and significant reductions in blood glucose levels in glucose-loaded mice. At doses of 50, 100, 200 and 400 mg per kg body weight, the extract reduced blood sugar levels by 22.9, 30.7, 45.4 and 46.1%, respectively compared to control animals. By comparison, a standard antihyperglycemic drug, glibenclamide, when administered at a dose of 10 mg per kg body weight, reduced blood glucose level by 48.9%. In analgesic activity tests, the extract at the above four doses reduced the number of abdominal writhings by 27.6, 37.9, 41.4, and 44.8%, respectively. A standard analgesic drug, aspirin, reduced the number of writhings by 31.0 and 51.7%, respectively, when administered at doses of 200 and 400 mg per kg body weight.
Conclusion
The results validate the folk medicinal use of the plant to alleviate pain. At the same time, the antihyperglycemic activity result suggests that the plant may be a potential source for blood sugar lowering drug(s).
Similar content being viewed by others
Background
Alternanthera sessislis (L.) R. Br. (Amaranthaceae) is known in English as sessile joyweed or dwarf copperleaf and in Bangladesh as Chanchi shak. It is an aquatic plant and can be commonly observed in marshy areas and wetlands of Bangladesh. Folk medicinal practitioners of Bangladesh consider the plant to possess medicinal properties. In Noakhali district of Bangladesh, the plant is used to treat gonorrhea, low sperm count, and leucorrhea [1]. In several areas of Faridpur and Rajbari districts of Bangladesh, the plant is used by folk medicinal practitioners for treatment of severe pain [2]. The tribals of Bargarh district, India use the plant to treat blood dysentery [3]. Different communities of Uttara Kannada district of Karnataka, India use the plant for treatment of ulcers and cuts and wounds [4]. The plant is used by local tribals (Santals, Gonds, Kolha, Bathudi) and inhabitants of Kaptipada Forest Range in Orissa, India for treatment of fevers, ophthalmia, gonorrhea, and pruritis [5]. The local people of Amarkantak region, Madhya Pradesh India have multiple uses for the plant including treatment of burning sensations, diarrhea, skin diseases, dyspepsia, hemorrhoids, liver and spleen diseases, and fever [6]. The Irula tribals of Kalavai, Vellore district, Tamil Nadu, India, treat headache, hepatitis, and asthma with the plant [7].
Anti-bacterial activity and possible cytotoxicity as demonstrated by brine shrimp lethality assay has been reported for A. sessilis[8]. Ethyl acetate fraction of A. sessilis Red has been reported to reduce fasting blood glucose level, triglyceride level, and free fatty acid level when administered to obese type 2 diabetic rats induced by high fat diet and streptozotocin [9]. Anti-allergic effect of ethanolic extract of the plant has also been described [10].
Diabetes is a disease characterized by high blood glucose levels and is rapidly spreading throughout the world, possibly because of changes in lifestyle and dietary habits of people. The International Diabetes Federation (IDF) South East Asia (SEA) Region, which contains the countries of India, Sri Lanka, Bangladesh, Bhutan, Mauritius, and Maldives have a high prevalence of diabetes. It has been reported that there were more than 72 million adults with diabetes in 2013, a number which is expected to exceed 123 million by 2035. Nearly 95% people of the total diabetic patients have type 2 diabetes (T2DM). Moreover, another 24.3 million people have impaired glucose tolerance (IGT). Both rural and urban population has seen increases in the number of diabetic people [11]. In a cross-sectional survey of 402 people among the urban middle class in Bangladesh, it has been seen that 35% had T2DM and 45% had metabolic syndrome [12]. Diabetes can lead to other disorders like cardiovascular, kidney and eye disorders. In fact, a high prevalence of chronic kidney disease has been reported following a community survey of urban people of Bangladesh, which has been correlated with insulin resistance [13].
Pain is a feeling triggered in the nervous system and is a problem faced by people throughout the world on a daily basis. Pain can be acute (as caused through injury) or can be chronic (i.e. lasting for months or years, as is the case with patients suffering from rheumatoid arthritis, gout, or some forms of cancer). Over the counter (OTC) drugs like aspirin or paracetamol can cause gastric ulceration or hepatic damage from prolonged use or over-dosage.
Rural people of Bangladesh suffer from lack of access to modern doctors and health-care facilities. Moreover, they cannot afford the price of allopathic medicines, whether be it anti-diabetic or analgesic. As such, scientific validation of traditional remedies or scientific validation of a previously not known plant for any given pharmacological effect offers the rural people (with ready accessibility to the plant) to get a desired medicinal effect at a much cheaper cost. Since diabetes and pain are common illnesses in Bangladesh, we had been screening various plants of Bangladesh for possible antihyperglycemic and analgesic effects [14–16]. A. sessilis is a common aquatic plant of Bangladesh and is readily available and frequently consumed by rural people as a vegetable. The objective of the present study was to evaluate the antihyperglycemic and analgesic potential of methanolic extract of aerial parts of A. sessilis through oral glucose tolerance tests and acetic acid-induced gastric pain model, respectively in mice.
Methods
Plant material collection
Aerial parts (leaves and stems) of A.sessilis were collected during March 2013 from Mirpur in Dhaka district, Bangladesh and taxonomically identified at the Bangladesh National Herbarium (Accession Number 38,593).
Preparation of methanolic extract of aerial parts
Aerial parts were cut into small pieces, air-dried in the shade, and 100 g of dried and powdered leaves and stems was extracted with methanol (w:v ratio of 1:6, final weight of the extract 8.03 g).
Chemicals and drugs
Glibenclamide, aspirin, and glucose were obtained from Square Pharmaceuticals Ltd., Bangladesh. All other chemicals were of analytical grade.
Animals
Swiss albino mice (male), which weighed between 15–19 g were used in the present study. The animals were obtained from International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR,B). The animals were acclimatized for three days prior to actual experiments. The study was conducted following approval by the Institutional Animal Ethical Committee of University of Development Alternative, Dhaka, Bangladesh.
Oral glucose tolerance tests for evaluation of antihyperglycemic activity
Oral glucose tolerance tests were carried out as per the procedure previously described by Joy and Kuttan (1999) [17] with minor modifications. Briefly, fasted mice were grouped into six groups of five mice each. The various groups received different treatments like Group 1 received vehicle (1% Tween 80 in water, 10 ml/kg body weight) and served as control, Group 2 received standard drug (glibenclamide, 10 mg/kg body weight). Groups 3–6 received extract (MEAAS) at doses of 50, 100, 200 and 400 mg per kg body weight. All substances were orally administered. Following a period of one hour, all mice were orally administered 2 g glucose/kg of body weight. Blood samples were collected 120 minutes after the glucose administration through puncturing heart. Blood glucose levels were measured by glucose oxidase method [18]. The percent lowering of blood glucose levels were calculated according to the formula described below.
where We and Wc represents the blood glucose concentration in glibenclamide or MEAAS administered mice (Groups 2–6), and control mice (Group 1), respectively.
Analgesic activity evaluation through abdominal writhing test
Analgesic activity of MEAAS was examined as previously described [19]. Briefly, mice were divided into seven groups of five mice each. Group 1 served as control and was administered vehicle only. Groups 2 and 3 were orally administered the standard non-narcotic analgesic drug aspirin at doses of 200 and 400 mg per kg body weight, respectively. Groups 4–7 were administered MEAAS at doses of 50, 100, 200 and 400 mg per kg body weight, respectively. Following a period of 60 minutes after oral administration of standard drug or MEAAS, all mice were intraperitoneally injected with 1% acetic acid at a dose of 10 ml per kg body weight. A period of 5 minutes was given to each animal to ensure onset of chemically induced irritation of acetic acid [20], following which period, the number of abdominal constrictions (writhings) was counted for 10 min. The percent inhibitions of abdominal writhings were calculated according to the formula given below.
where We and Wc represents the number of writhings in aspirin or MEAAS administered mice (Groups 2–7), and control mice (Group 1), respectively.
Acute toxicity test
Acute toxicity test was conducted as previously described [21]. Mice were divided into nine groups, each group consisting of six animals. Group 1 was given 1% Tween 80 in normal saline (2 ml per kg body weight). The other eight groups (Groups 2–9) were administered, respectively, 100, 200, 300, 600, 800, 1000, 2000 and 3000 mg of MEAAS per kg body weight. All animals were closely observed for the next 8 hours to notice any behavioral changes or mortality and were kept under close observation for the next two weeks.
Statistical analysis
Experimental values are expressed as mean ± SEM. Independent Sample t-test was carried out for statistical comparison. Statistical significance was considered to be indicated by a p value < 0.05 in all cases [20].
Preliminary phytochemical screening
Preliminary phytochemical analysis of MEAAS for presence of saponins, tannins, alkaloids, and flavonoids were conducted as described before [22].
Results
Preliminary screening of phytochemicals
Various tests conducted for presence of phytochemicals in MEAAS indicated the presence of tannins, alkaloids, and flavonoids.
Toxicity evaluation
The crude extract did not show any toxicity in mice even at the highest dose tested.
Antihyperglycemic activity evaluation results
MEAAS, when administered at doses of 50, 100, 200 and 400 mg per kg body weight, dose-dependently and significantly reduced the concentration of blood glucose in glucose-loaded mice by 22.9, 30.7, 45.4, and 46.1% respectively. By comparison, a standard antihyperglycemic drug, glibenclamide, when administered to mice at a dose of 10 mg per kg body weight, reduced blood glucose level by 48.9%. The results are shown in Table 1 and indicate that at the highest dose of 400 mg, the antihyperglycemic activity of MEAAS was comparable to that of glibenclamide.
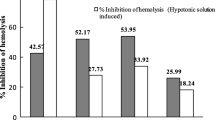
Analgesic activity evaluation results
Dose-dependent and significant reductions in the number of abdominal writhings induced by intraperitoneal administration of acetic acid were observed with MEAAS. At doses of 50, 100, 200 and 400 mg per kg body weight, MEAAS reduced the number of writhings, respectively, by 27.6, 37.9, 41.4, and 44.8%. A standard non-narcotic analgesic drug, aspirin, when administered to experimental animals at doses of 200 and 400 mg per kg body weight, reduced the number of writhings by 31.0 and 51.7%, respectively. Thus the three higher doses of MEAAS exhibited greater analgesic activity than aspirin when administered at a dose of 200 mg per kg body weight. The results are shown in Table 2.
Discussion
The observed decrease in blood glucose levels by MEAAS can be possibly through potentiating pancreatic insulin secretion or by increasing glucose uptake. Such mechanisms have been proposed before for extracts of Picrorrhiza kurroa[17] and Helicteres isora[23]. Although identification of phytochemicals was not conducted in this preliminary study, flavonoids or alkaloids present in MEAAS can account for the observed antihyperglycemic effect. Free radical scavenging activity as well as antihyperglycemic and antihypertensive effects has been reported for flavonoid-rich fractions from Trichilia emetica and Opilia amentacea in animal model of type II diabetes mellitus [24]. Hypoglycaemic and tissue-protective effects of the aqueous extract of Persea americana seeds on alloxan-induced albino rats has been reported; alkaloids and flavonoids were present among the extract [25].
Intraperitoneal administration of acetic acid can lead to pain (with consequent abdominal writhings) by inducing the release of mediators like prostaglandin E2, as well as lipooxygenase products [26]. Prostaglandins [mainly prostacyclines (PGI2) and prostaglandin- (PG-E)], in turn, has been shown to be responsible for excitation of Aδ-nerve fibers, leading to the sensation of pain [27, 28]. Thus the observed non-narcotic analgesic activity of MEAAS can be due to its ability to block prostaglandin synthesis through inhibition of lipooxygenase and/or cyclooxygenase activities. A similar mechanism has been proposed before for analgesic activity of Ficus deltoidea aqueous extract in acetic acid-induced pain model [26]. Flavonoids, alkaloids and tannins present in MEAAS can be responsible for the analgesic effect. Flavonoids, alkaloids and tannins have been shown to be present in methanol extract of Muntingia calabura leaves demonstrating analgesic activity [29, 30].
The present study validates the folk medicinal use of A. sessilis in Bangladesh for treatment of severe pain, and further suggests that the aerial parts of the plant can be a potential mean for lowering blood glucose levels. Since the plant is widely available in Bangladesh, it can prove beneficial in being a source of a cheap and effective medication for persons with high blood glucose levels and persons suffering from chronic pain in cases like rheumatoid arthritis. Notably, the plant is consumed by the people of Bangladesh as a vegetable. Further studies are underway in our laboratory as to whether cooking destroys the antihyperglycemic and analgesic principles or the principles still remain active.
Conclusion
The results validate the folk medicinal use of stems of A. sessilis to reduce high blood glucose levels in diabetic patients and to alleviate pain. From that view point, the extract merits further scientific attention for further isolation and identification of the responsible bioactive component(s).
References
Rahmatullah M, Mahmud AA, Rahman MA, Uddin MF, Hasan M, Khatun MA, Bashar ABMA, Ahsan S, Mou SM, Begum R, Jahan R: An ethnomedicinal survey conducted amongst folk medicinal practitioners in the two southern districts of Noakhali and Feni, Bangladesh. Am-Eur J Sustain Agric. 2011, 5: 115-131.
Mukti M, Ahmed A, Chowdhury S, Khatun Z, Bhuiyan P, Debnath K, Rahmatullah M: Medicinal plant formulations of Kavirajes in several areas of Faridpur and Rajbari districts, Bangladesh. Am-Eur J Sustain Agric. 2012, 6: 234-247.
Sen SK, Behera LM: Ethnomedicinal plants used by the tribals of Bargarh district to cure diarrhoea and dysentery. Indian J Tradit Knowl. 2008, 7: 425-428.
Bhat P, Hegde G, Hegde GR: Ethnomedicinal practices in different communities of Uttara Kannada district of Karnataka for treatment of wounds. J Ethnopharmacol. 2012, 143: 501-514. 10.1016/j.jep.2012.07.003.
Behera KK, Mishra NM, Rout GR: Potential ethnomedicinal plants at Kaptipada Forest Range Orissa, India and their uses. J Econ Taxon Bot. 2008, 32: 194-202.
Srivastava A, Patel SP, Mishra RK, Vasishtha RK, Singh A, Puskar AK: Ethnomedicinal importance of the plants of Amarkantak Region, Madhya Pradesh, India. Int J Med Arom Plants. 2012, 2: 53-59.
Natarajan A, Leelavinodh KS, Jayavelu A, Devi K, Kumar BS: A study on ethnomedicinal plants of Kalavai, Vellore district, Tamil Nadu, India. J Appl Pharmaceut Sci. 2013, 3: 99-102.
Ullah MO, Haque M, Urmi KF, Zulfiker AH, Anita ES, Begum M, Hamid K, Uddin SJ: Anti-bacterial activity and brine shrimp lethality bioassay of methanolic extracts of fourteen different edible vegetables from Bangladesh. Asian Pac J Trop Biomed. 2013, 3: 1-7.
Tan KK, Kim KH: Alternanthera sessilis Red ethyl acetate fraction exhibits antidiabetic potential on obese type 2 diabetic rats. Evid Based Complement Alternat Med. 2013, 2013: 845172-doi:10.1155/2013/845172
Rayees S, Kumar A, Rasool S, Kaiser P, Satti NK, Sangwan PL, Singh S, Johri RK, Singh G: Ethanolic extract of Alternanthera sessilis (AS-1) inhibits IgE-mediated allergic response in RBL-2H3 cells. Immunol Invest. 2013, 42: 470-480. 10.3109/08820139.2013.789909.
Ramachandran A, Snehalatha C, Ma RC: Diabetes in South-East Asia: an update. Diabetes Res Clin Pract. 2014, 103: 231-237. 10.1016/j.diabres.2013.11.011.
Saquib N, Khanam MA, Saquib J, Anand S, Chertow GM, Barry M, Ahmed T, Cullen MR: High prevalence of type 2 diabetes among the urban middle class in Bangladesh. BMC Public Health. 2013, 13: 1032-10.1186/1471-2458-13-1032. doi:10.1186/1471-2458-13-1032
Anand S, Khanam MA, Saquib J, Saquib N, Ahmed T, Alam DS, Cullen MR, Barry M, Chertow GM: High prevalence of chronic kidney disease in a community survey of urban Bangladeshis: a cross-sectional study. Global Health. 2014, 10: 9-10.1186/1744-8603-10-9. doi:10.1186/1744-8603-10-9
Haque ME, Rahman S, Rahmatullah M, Jahan R: Evaluation of antihyperglycemic and antinociceptive activity of Xanthium indicum stem extract in Swiss albino mice. BMC Complement Altern Med. 2013, 13: 296-10.1186/1472-6882-13-296. doi:10.1186/1472-6882-13-296
Rahmatullah M, Hossain M, Mahmud A, Sultana N, Rahman SM, Islam MR, Khatoon MS, Jahan S, Islam F: Antihyperglycemic and antinociceptive activity evaluation of 'khoyer’ prepared from boiling the wood of Acacia catechu in water. Afr J Tradit Complement Altern Med. 2013, 10: 1-5. 10.1625/jcam.10.1.
Khatun F, Zaman F, Mosaiab T, Mostafa F, Zaman M, Rehana F, Nasrin D, Jamal F, Nahar N, Rahmatullah M: Evaluation of antinociceptive and antihyperglycemic activities in methanol extracts of whole plants of Alternanthera philoxeroides (Mart.) Griseb. (Amaranthaceae) in mice. Pak J Pharm Sci. 2012, 25: 583-587.
Joy KL, Kuttan RJ: Anti-diabetic activity of Picrorrhiza kurroa extract. J Ethnopharmacol. 1999, 67: 143-148. 10.1016/S0378-8741(98)00243-8.
Nyunai N, Njikam N, Addennebi EH, Mbaford JT, Lamnaouer D: Hypoglycaemic and antihyperglycaemic activity of Ageratum conyzoides L. in rats. Afr J Tradit Complement Altern Med. 2009, 6: 123-130. 10.1625/jcam.6.123.
Shanmugasundaram P, Venkataraman S: Anti-nociceptive activity of Hygrophilous auriculata (Schum) Heine. Afr J Tradit Complement Altern Med. 2005, 2: 62-69.
Rahman MM, Hasan MN, Das AK, Hossain MT, Jahan R, Khatun MA, Rahmatullah M: Effect of Delonix regia leaf extract on glucose tolerance in glucose-induced hyperglycemic mice. Afr J Tradit Complement Altern Med. 2011, 8: 34-36.
Ganapaty S, Dash GK, Subburaju T, Suresh P: Diuretic, laxative and toxicity studies of Cocculus hirsutus aerial parts. Fitoterapia. 2002, 71: 28-31.
Kumar C, Kumar R, Nehar S: Phytochemical properties, total antioxidant status of acetone and methanol extract of Terminalia arjuna Roxb. bark and its hypoglycemic effect on Type-II diabetic albino rats. J Pharmacogn Phytochem. 2013, 2: 199-208.
Venkatesh S, Reddy GD, Reddy YSR, Sathyavathy D, Reddy BM: Effect of Helicteres isora root extracts on glucose tolerance in glucose-induced hyperglycemic rats. Fitoterapia. 2004, 75: 364-367. 10.1016/j.fitote.2003.12.025.
Konaté K, Yomalan K, Sytar O, Zerbo P, Brestic M, Patrick VD, Gagniuc P, Barro N: Free radicals scavenging capacity, antidiabetic and antihypertensive activities of flavonoid-rich fractions from leaves of Trichilia emetica and Opilia amentacea in an animal model of type 2 diabetes mellitus. Evid Based Complement Alternat Med. 2014, 2014: 867075-doi:10.1155/2014/867075
Ezejiofor AN, Okorie A, Orisakwe OE: Hypoglycaemic and tissue-protective effects of the aqueous extract of Persea americana seeds on alloxan-induced albino rats. Malays J Med Sci. 2013, 20: 31-39.
Sulaiman MR, Hussain MK, Zakaria ZA, Somchit MN, Moin S, Mohamad AS, Israf DA: Evaluation of the antinociceptive activity of Ficus deltoidea aqueous extract. Fitoterapia. 2008, 2008 (79): 557-561.
Rang HP, Dale MM, Ritter JM, Moore PK: Pharmacology. 2003, London, UK: Churchill Livingstone, 562-563. 5
Reynolds JEF: Martindale: The Extra Pharmacopoeia. 1982, London, UK: The Pharmaceutical Press, 245-28
Mohamad Yusof MI, Salleh MZ, Lay Kek T, Ahmat N, Nik Azmin NF, Zakaria ZA: Activity-guided isolation of bioactive constituents with antinociceptive activity from Muntingia calabura L. leaves using the formalin test. Evid Based Complement Alternat Med. 2013, 2013: 715074-doi:10.1155/2013/715074
Zakaria ZA, Sani MH, Cheema MS, Kader AA, Kek TL, Salleh MZ: Antinociceptive activity of methanolic extract of Muntingia calabura leaves: further elucidation of the possible mechanisms. BMC Complement Altern Med. 2014, 14: 63-10.1186/1472-6882-14-63. doi:10.1186/1472-6882-14-63
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6882/14/169/prepub
Acknowledgements
This work was funded through internal funding of the University of Development Alternative.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors’ contributions
AIH, MF and SR collected the plant, did the extraction, and performed the experiments under the supervision of RJ and MR. MR wrote the manuscript draft, which was read and edited by all authors. All authors read and approved the final version of the manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hossain, A.I., Faisal, M., Rahman, S. et al. A preliminary evaluation of antihyperglycemic and analgesic activity of Alternanthera sessilis aerial parts. BMC Complement Altern Med 14, 169 (2014). https://doi.org/10.1186/1472-6882-14-169
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6882-14-169