Abstract
Background
An international discussion about whether or not to legally permit euthanasia and (or) physician assisted suicide (EAS) is ongoing. Unbearable suffering in patients may result in a request for EAS. In the Netherlands EAS is legally permitted, and unbearable suffering is one of the central compulsory criteria. The majority of EAS is performed in cancer patients in the primary care practice. In around one in every seven end-of-life cancer patients dying in the primary care setting EAS is performed. The prevalence of unbearable symptoms and overall unbearable suffering in relationship to explicit requests for EAS was studied in a cohort of end-of-life cancer patients in primary care.
Methods
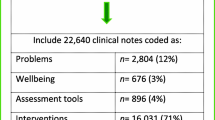
A prospective study in primary care cancer patients estimated to die within six months was performed. Every two months suffering was assessed with the State-of-Suffering V (SOS-V). The SOS-V is a comprehensive instrument for quantitative and qualitative assessment of unbearable suffering related to 69 physical, psychological and social symptoms in five domains.
Results
Out of 148 patients who were asked to participate 76 (51%) entered the study. The studied population were 64 patients who were followed up until death; 27% explicitly requested EAS, which was performed in 8% of the patients. The final interview per patient was analyzed; in four patients the SOS-V was missing. Unbearable symptoms were present in 94% of patients with an explicit request for EAS and in 87% of patients without an explicit request. No differences were found in the prevalence of unbearable suffering for physical, psychological, social and existential symptoms, nor for overall unbearable suffering, between patients who did or who did not explicitly request EAS.
Conclusions
In a population of end-of-life cancer patients cared for in primary care no differences in unbearable suffering were found between patients with and without explicit requests for EAS. The study raises the question whether unbearable suffering is the dominant motive to request for EAS. Most patients suffered from unbearable symptoms, indicating that the compulsory criterion of unbearable suffering may be met a priori in most end-of-life cancer patients dying at home, whether they request EAS or not.
Similar content being viewed by others
Background
Unbearable suffering is considered an important motive for patients requesting euthanasia and/or assisted suicide (EAS) [1]. Seven countries and states have legalized EAS, or permit EAS under existing law [2]. The presence of unbearable suffering, as assessed by a physician, is a central criterion for EAS in the Netherlands, Belgium and Luxembourg [3–6]. Further compulsory criteria to legally allow EAS include a voluntary and well considered request for EAS, prospect-less suffering, absence of reasonable treatment options and consultation with an independent physician [6, 7]. Terminal illness is not a compulsory criterion [6]. The legal model which applies in Switzerland, Oregon, Washington and Montana requires a voluntary and well considered request; unbearable suffering is not a compulsory criterion and only assisted suicide is allowed [2, 8, 9]. Terminal illness is a compulsory criterion in the U.S. states [2].
The Netherlands has a population of nearly seventeen million and 136.000 annual deaths. Annually some 40.000 patients die from cancer (28% of all deaths), 45% of whom die at home [10]. Primary care nationwide is provided by nearly 9.000 general practitioners (GPs), 57% of whom work part time [11]. A full time GP on average provides end-of-life care for a cancer patient nearly three times a year [12].
Performed euthanasia in the Netherlands has been studied in 5-year intervals since 1990 [13, 14]. In 2002 EAS was legalized. By 2005 the total number of explicit requests for EAS was 8400; 29% of all explicit requests for EAS were granted; 1.8% of all deaths were the result of EAS (n = 2410) [14, 15]. In 2010 the total number of explicit requests for EAS was 9100; 45% of all explicit requests for EAS were granted; 2.8% of all deaths were the result of EAS (n = 4050) [13, 16]. In the 2010 study 79% of all EAS patients has a cancer diagnosis. Eighty-eight percent of EAS cases were performed in primary care [13].
In end-of-life cancer patients dying in the primary care setting EAS is performed in around one in every seven patients [17]. EAS most frequently is performed in the estimated last two weeks of life [13]. Legal responsibility for EAS allotted to the medical profession changes the dynamics of interaction between patients and physicians [18]. Doctors face difficulties in assessing and responding to suffering and requests for EAS [1, 3, 19–23]. Patient directed research investigating unbearable suffering in relationship to whether an explicit request for EAS is made is scarce. In this study the presence and nature of unbearable suffering and its relationship to requests for euthanasia was investigated.
Methods
Design and population
The study was conducted in Utrecht, a city with about 235 000 people and 105 GPs. Those eligible for the study were terminal cancer patients expected to die within half a year and who were expected to live at home (most of the time) until death. They were cared for by a GP as the primary responsible physician. The GPs estimated survival, and clinical deterioration guided estimation of survival.
Forty-four GPs, representing 42% of the GPs in the city, 59% of whom worked part time, requested participation from eligible patients. A study coordinator organized the recruitment process, which included identifying all eligible patients in the care of GPs during the follow-up period. Baseline-characteristics of all eligible patients were registered. Within a week the baseline interview was administered to consenting patients. Follow-up interviews were administered every two months, or sooner based upon information by GPs that the condition of a patient had rapidly deteriorated. All interviews were at the patients’ residence. GPs were personally contacted every two months for follow-up data. When a patient died the treating physician was asked whether an explicit request for EAS had been made; a record of the date of the request was not part of the study design. Whether EAS actually was performed was not part of the initial physician-directed follow-up, because of the potential negative influence on recruitment related to enquiring about this sensitive subject. Transition to a hospice was not an exclusion criterion; in many Dutch hospices the GP remains responsible for palliative care. The interviewers were a physiotherapist (the study coordinator) and a GP (CR), both trained in interview techniques. The study protocol was approved by the Medical Ethics Committee at the VU University. Written informed consent was obtained from participants. The recruitment process is described in detail elsewhere [24].
Patient recruitment occurred from May 2003 until May 2006, follow-up continued until May 2007. There were 258 eligible patients. One hundred and ten patients were not requested to participate, in majority because their physical condition deteriorated so rapidly that their GP considered an interview too burdensome. Seventy-six out of 148 invited patients (51%) entered the interview study. Seventy-two patients refused to participate, in majority because of rapidly deteriorating physical condition and considering the interview too burdensome. In the 76 patients who entered the interview study the attrition rate was 8% (n = 6), caused by patients who stopped participating after one or more interviews. At the end of follow-up period 8% (n = 6) of the patients were alive, leaving 64 patients with follow up until death. In 60 patients at least one SOS-V interview was present; in four patients the interview was missing; the interviewer had considered the interview too burdensome and abandoned. In 33 patients the SOS-V was administered at least two times. Age, gender and type of cancer did not differ between the patients in and out of the interview sample. In January 2014 the GPs who had been addressed with a request for EAS were personally contacted to assess whether EAS had been performed. All GPs agreed to share this important information. Medical files were checked and dying trajectories were evaluated.
Issues concerning the investigation of unbearable suffering
Unbearable suffering was defined as a subjective experience of suffering that is so serious and uncontrollable that it overwhelms one’s bearing capacity [25]. Unbearable suffering is a relative experience, which may be more or less present. Quantitative investigation of unbearable suffering provides the opportunity to compare patient populations. The measure of unbearable suffering needs to be differentiated from the intensity of symptoms; symptoms may be intensely present yet bearable, and vice versa [17].
Evaluation of unbearable suffering in relationship to specific disease indicates a systematic investigation of whether disease specific symptoms are present [26–29], followed by an assessment of whether symptom related unbearable suffering occurs. Suffering caused by co-morbidities, particularly if these result in unbearable suffering, may confound study outcomes and needs to be assessed. Investigation of the various physiological systems whether symptoms caused by co-morbidity occur and whether these symptoms result in unbearable suffering is indicated. Suffering reaches further than biomedical symptoms, it includes the consequences and meaning of disease for the various domains of life. These domains include practical daily functioning (functional domain), the perspective of self (personal domain), functioning in relationship to others (domain of social environment) and perspective of the future (domain of future perspective). Suffering in these domains, related to disease as well as independent of disease, adds to suffering and needs to be investigated [30, 31]. The meaning of suffering [21, 30–36] cannot be fully understood by a study limited to providing scores. Assessment about the personal experience of the suffering is necessary.
A framework of categories of suffering may help to organize qualitative study outcomes of experiences of suffering. The qualitative descriptions may be attributed to a framework of biomedical, psychodynamic and emotional categories of suffering. An important psychodynamic perspective of suffering is the concept of loss, such as loss of meaning, loss of autonomy, loss of dignity or loss of hope [21, 31, 33, 34, 36, 37]. Emotional categorizations of suffering include depression, hopelessness, demoralization, anxiety, worrying and feeling tensed [31, 38–40]. Suffering is complex and there is no universal, clear-cut, comprehensive system of categorization of suffering [31, 41]. The frequently employed categorization in physical, psychological, social and existential suffering [32, 42–45] demonstrates overlap. This categorization may suggest that existential suffering is a separate entity. However, physical, psychological and social suffering may result in existential suffering, and existential suffering may be part of various categories of suffering [46]. For the purpose of analysis of qualitative data about suffering a considered choice may be made for categories relevant to the study perspective.
Measurement instrument: the State-of-Suffering V
To realize this study the State-of-Suffering V (SOS-V) was developed. The SOS-V is a structured, quantitative instrument for comprehensive assessment of unbearable suffering related to symptoms, with additional open ended questions to investigate the experience of suffering [17, 25]. “Symptoms” refers to physical, psychological, social and existential aspects of suffering; this extended interpretation of symptoms is not uncommon in psychosomatic research. Cancer is polysymptomatic [26] and systematic assessment of symptoms is indicated [27]. Based upon literature study a framework of domains in which suffering may occur was selected and symptoms relevant to end-of-life cancer populations were introduced. The SOS-V systematically addresses 69 symptoms in a framework of five domains: (I) medical symptoms; (II) loss of function; (III) personal aspects; (IV) environment and; (V) nature and prognosis of disease [25]. For every symptom two questions are asked. First, what is the intensity (or extent) of the symptom? Second, if the symptom is present, to what extent does the symptom cause unbearable suffering?
A uniform 5-point scoring scale with a description is employed for both questions: 1-not at all; 2-slightly; 3-moderately; 4-seriously; 5-very seriously, hardly could be worse. When a patient rates 4 or 5 for unbearable suffering, the experience is further explored through open ended questions. Answers are immediately written down as quoted phrases. After rating all 69 symptoms the interviewer asks whether individual aspects of suffering are missing, and if so documents and rates these as well. Reduction of symptoms investigated with the SOS-V was not striven for; suffering is multidimensional, the symptoms are clinically differentiable and it requires consideration that even one symptom may determine unbearability. The total number of symptoms which cause suffering does not automatically add up to an overall experience of suffering. The overall experience of suffering is assessed at the end of the interview; the patient is asked to consider all present symptoms and rate overall unbearable suffering (same scale). The two days before the interview were the reference period for assessment of suffering. The development of the instrument is described elsewhere [25]. Administration of the quantitative section of the SOS-V generally was possible within 15 to 20 minutes [12, 25].
Analysis
Only the final SOS-V interviews were analyzed as they were the interviews closest to death, taking in account that performing EAS in response to an explicit request in majority occurs in the final two weeks of life [13, 16]. The question about the intensity of symptoms was dichotomized into the symptom not at all being present (rating 1) versus the symptom being present (ratings 2–5). When a symptom was not at all present, it was assumed that the symptom did not lead to unbearable suffering, and a rating of 1 was given for unbearable suffering. After that the quantitative data about unbearable suffering were analyzed dichotomously. Ratings 1 (not at all), 2 (slightly) or 3 (moderately) for suffering were defined as bearable; ratings 4 (seriously) or 5 (very seriously, hardly could be worse) were defined as unbearable. Differences in prevalence of unbearable symptoms and overall unbearable suffering between patients who did and who did not request EAS were tested with a Fisher’s exact test for nominal variables and with a t-test for continuous variables; the p-level was 0,05. Additionally Bonferroni analysis for high numbers of independent tests was applied.
To organize the qualitative descriptions of the experiences of suffering, related to symptoms for which the patients rated 4 or 5 for unbearable suffering, a categorization schedule was composed of senses of suffering which are relevant in patients at the end of life (Table 1) [17]. Existential suffering, an important construct of suffering, was not separately identified, from the perspective that other identifiable senses of suffering all may potentially contribute to existential suffering [21, 26–30, 32–36, 38, 41–43, 46–48]. Two raters, a GP (CR) and an external clinical psychologist, independently rated the descriptions of the experiences of unbearable suffering according to the categorization schedule. One rating per unbearable description was permitted. The raters then deliberated about the ratings which were not identically attributed and provided identical rating, if possible, after discussion. Only identically attributed ratings were used to analyze differences between patients who did and who did not request EAS. Consensus between the raters occurred in 86% of the analyzed qualitative descriptions. T-test for mean prevalence were used for statistical analysis. The rating process is described in more detail elsewhere [17].
Results
The studied sample consisted of the 64 patients who died during follow-up; 46 patients died within six months after inclusion. The average age was 70 years (range 38–86), 52% were female, all patients were Caucasian. Lung cancer (27%) and gastro-intestinal cancer (25%) were most prevalent. An explicit request for EAS occurred in 27% (17 patients); EAS was performed in 8% (5 patients). A part of the study design was to obtain information from GPs that the condition of a patient had rapidly deteriorated, so that additional interviews could be planned close to death. This rarely occurred. The final interview was on average 30 days before death (SD 17 days); in 23% the interview was administered within two weeks prior to death. An advance euthanasia directive (77% versus 9%) and higher education (defined as any further education after high school) (35% versus 13%) were significantly more frequent in the group of patients with an explicit request; for the other demographic characteristics no differences occurred (Table 2). The prevalence of explicit requests for EAS was 15% (16 out of 110 patients) in the sample which was not invited to participate, and 10% (7 out of 72 patients) in the sample which declined participation.
Unbearable symptoms were present in 88% (n = 53) of the 60 patients studied with the SOS-V. No significant differences in prevalence of unbearable symptoms occurred between patients with and without an explicit request for EAS (Tables 3 and 4). “Needing help with housekeeping” was unbearable more frequently in patients with an explicit request for euthanasia (65% versus 33%), however after application of the Bonferroni correction no significant differences remained. No differences occurred between patients with and without an explicit EAS request for mean total of unbearable symptoms (mean 11.6 ± SD 8.6 unbearable symptoms versus mean 10.3 ± SD 9.3 unbearable symptoms) and for prevalence of overall unbearable suffering (33% versus 28%). Unbearable symptoms were present in 94% of patients with an explicit request for EAS and in 87% of patients without an explicit request. There were no differences in numbers of unbearable symptoms per domain.
The qualitative analysis demonstrated no significant differences in senses of unbearable suffering between patients with and without an explicit request for euthanasia (Table 5). Examples of attributions of qualitative data to categories are additionally provided in Table 1. Additional information about the trajectory of patients with an explicit request for EAS is provided in Table 6.
Two of the patients withdrew their request for EAS. Reasons why EAS was not performed could not be retrieved from the medical files in the other patients. No conflicts between patients and GPs about whether or not to perform EAS were identified; in one case a conflict with the family occurred because EAS was not performed. Referral to other physicians, because GPs did not agree with performing EAS, did not occur.
Discussion
The present study touches on fundamental questions about suffering, autonomy and the tasks of the medical profession concerning life and death. We have not identified prior patient directed studies which prospectively investigated unbearable suffering in relationship to requests for EAS in a cohort of patients. EAS in one out of three patients with an explicit request for euthanasia is comparable to findings in other studies in the Dutch setting [13, 14, 49, 50].
No differences occurred in prevalence of unbearable symptoms, or in prevalence of overall unbearable suffering, between patients with and without an explicit request for EAS. Frequently mentioned motives for requesting EAS are loss of control, loss of autonomy, loss of dignity, not wanting to be a burden to others and fear of the future [8, 32, 51–55]. The prevalences of these motives, from the perspective of unbearable suffering, were not different for patients with and without a request for EAS. Loss of control, isolation, hopelessness, burden on others and fear about the future, which in research were found indicative of existential issues [46], were not different for patients with and without unbearable suffering. These findings may indicate that unbearable suffering is not the dominant motive to request EAS.
Unbearable symptoms occurred in 88% of this primary care population of end-of-life cancer patients in the period around one month before death. This indicates that the criterion of unbearable suffering, also when not being the decisive motive to request EAS, may be met in the majority of end-of-life cancer patients cared for in primary care when initiating the procedure of compulsory criteria assessment to evaluate whether EAS is permitted. How to interpret this finding as part of the process in which physicians respond to requests for EAS is unclear. Identified causes for not granting requests for EAS included death of the patient before performance of EAS (20%; percentage of total of ungranted requests), death of the patient before finalization of decision making (20%), withdrawal of the request by the patient (20%) and refusal of the physician to comply to the request of the patient (18%) [49].
Motives to request EAS may need to be interpreted from a different perspective. A desire to control the circumstances of one’s death, rather than unbearable suffering due to loss of control, may determine the request for EAS. Another driver of requests for EAS may be loss of the will to continue living [56–58], caused by loss of positive feelings towards life and (or) loss of connectedness with life [32, 36, 38, 47, 53, 57]. Loss of energy and exhaustion, related to tiredness and weakness which are prevalent among end-of-life cancer patients [29], may contribute to loss of the desire to continue living. Depression and related suicidality in cancer patients are possible causes of a request for EAS [59–61]. The prevalent role of depression related to requesting for EAS has not been assessed in research [62, 63]. Another perspective is that a genuine desire to die is absent in patients who express a wish to hasten death [22, 64]. The underlying message of a request for EAS might be a cry for help [22], a request to be given a reason to live [37, 64], or an expression of feelings [65]. None of these has been sufficiently recognized or addressed. Finally societal influences need to be considered. Individual choice is an important societal driver of Western society [66]. Practices which enhance autonomous choice in health care, e.g. physician initiated discussions of the subject of EAS at an early stage [67], or granting the wish of the patients as the motive to provide EAS [13], may influence direction and outcomes of provision of care [3, 19, 66, 68, 69]. The presence of an advance pro-euthanasia directive and higher education, which occurred more frequently in patients with an explicit request, may be in line with the perspective of control and with the perspective of choice.
Patients depend upon responses of physicians. In responding to patients with a request for EAS it needs to be realized that dying cancer patients perceive that they cannot feel completely independent, which affects true autonomous decision making [70, 71]. Additionally, processes of transference may influence the communication between patient and physician. Awareness of such processes is important when responding to patients with a request for EAS [70, 72, 73]. Physician factors in response to the suffering of patients include attitude and quality of provided palliative care [18, 23, 72, 74]. Palliative interventions to reduce suffering in end-of-life cancer patients include symptom reduction [28], psycho-oncologic interventions [32, 33, 36, 47, 75, 76], spiritual care [77, 78] and palliative sedation [79, 80]. A tradition of research investigating effectiveness of palliative interventions in primary care populations does not exist. Therefore little is known about the effectiveness of interventions to reduce the suffering of end-of-life cancer patients in this setting. Even less is known about the question of which interventions may reduce the prevalence of requests for EAS, or performance of EAS. A remarkable quote in a Dutch qualitative study was that some GPs, since adopting a more caring attitude, found they no longer had to perform euthanasia [74].
The present study has some limitations. The first is the limited number of patients, which limits statistical power. We cannot rule out the possibility of differences in unbearable suffering between patients with and without an explicit request that we did not find. Interviews with most patients were not in the final days of life; unbearable suffering may have progressed, or may have been adequately treated. Furthermore, for the patients who explicitly requested euthanasia, the interview was not administered at the time of the request. The sample concerns a Western population in primary care in a context of legally permitted EAS, which limits generalizability.
Conclusions
We conclude that in a population of end-of-life cancer patients cared for in primary care no differences in unbearable suffering were found between patients with and without explicit requests for EAS. The study raises the question of whether unbearable suffering is the dominant motive to request for EAS. Another outcome was that most patients suffered from unbearable symptoms, indicating that the compulsory criterion of unbearable suffering, part of the criteria which permit performing EAS, may be met a priori in most end-of-life cancer patients dying at home, whether they request EAS or not.
Ethical approval
The study protocol was approved by the Medical Ethics Committee at the VU University Medical Center (METC VUmc No. 2002/79).
References
Emanuel EJ: Depression, euthanasia and improving end-of-life care. J Clin Oncol. 2005, 23: 6456-6458. 10.1200/JCO.2005.06.001.
Steck N, Egger M, Maessen M, Reisch T, Zwahlen M: Euthanasia and assisted suicide in selected European countries and US States. Systematic literature review. Med Care. 2013, 51: 938-944. 10.1097/MLR.0b013e3182a0f427.
Gorsuch NM: The right to assisted suicide and euthanasia. Harv J Law Public Policy. 2000, 23: 599-710.
Royal Dutch Medical Association (KNMG): In Dutch. Position of Federation Committee KNMG Concerning Euthanasia 2003. 2003, Utrecht: KNMG
Emanuel EJ: Euthanasia: Historical, ethical, and empiric perspectives. Arch Int Med. 1994, 154: 1890-1901. 10.1001/archinte.1994.00420170022003.
Rietjens JAC, van Tol DG, van der Heide A: Judgement of suffering in the case of a euthanasia request in The Netherlands. J Med Ethics. 2009, 35: 502-507. 10.1136/jme.2008.028779.
Van Tol DG, Rietjens JAC, van der Heide A: Empathy and the application of the “unbearable suffering” criterion in Dutch euthanasia practice. Health Policy. 2012, 105: 296-302. 10.1016/j.healthpol.2012.01.014.
Ganzini L, Goy ER, Dobscha SK: Oregonians’ reasons for requesting physician aid in dying. Arch Int Med. 2009, 169: 489-492. 10.1001/archinternmed.2008.579.
Hedberg K, Hopkins D, Leman R, Kohn M: The 10-year experience of Oregon’s death with dignity act: 1998–2007. J Clin Ethics. 2009, 20: 124-132.
Cohen J, Houttekier D, Onwuteaka-Philipsen B, Miccenesi G, Addington-Hall J, Kaasa S, Bilsen J, Deliens L: Which patients with cancer die at home? A study of six European countries using death certificate data. J Clin Oncol. 2010, 28: 2267-2273. 10.1200/JCO.2009.23.2850.
Institute for Health Services Research: Figures from the Registration of General Practitioners; Estimates. 2008, Netherlands (In Dutch)
Ruijs CDM, Kerkhof AJFM, van der Wal G, Onwuteaka-Philipsen BD: The broad spectrum of unbearable suffering in end-of-life cancer studied in Dutch primary care. BMC Palliative Care. 2012, 11: 12-10.1186/1472-684X-11-12.
Onwuteaka-Philipsen BD, Brinkman-Stoppelenburg A, Penning C, de Jong-Krul GJF, van Delden JJM, van der Heide A: Trends in end-of-life practices before and after the enactment of the euthanasia law in the Netherlands from 1990 to 2010: a repeated cross-sectional survey. Lancet. 2012, 380: 908-915. 10.1016/S0140-6736(12)61034-4.
Van der Heide A, Onwuteaka-Philipsen BD, Rurup ML, Buiting HM, van Delden JJM, Hanssen-de Wolf JE, Janssen AGJM, Pasman HRW, Rietjens JAC, Prins CJM, Deerenberg IM, Gevers JKM, van der Maas PJ, van der Wal G: End-of-life practices in the Netherlands under the euthanasia act. N Engl J Med. 2007, 356: 1957-1965. 10.1056/NEJMsa071143.
ZonMW: Evaluation of law About Verification of Ending of Lives at Request and Assisted Suicide. 2007, Enschede: Print Partners Ipskamp, In Dutch
ZonMW: Study Concerning Cases of Deaths 2010. Euthanasia and Other Medical Decisions at the end of Life. 2010, Schultenprint: Zoetermeer, 2012-(In Dutch)
Ruijs CDM, Kerkhof AJFM, van der Wal G, Onwuteaka-Philipsen B: Symptoms, unbearability and the nature of suffering in terminal cancer patients dying at home: a prospective primary care study. BMC Fam Pract. 2013, 14: 201-10.1186/1471-2296-14-201.
Kenny NP: Responding to Requests for Euthanasia and Physician-Assisted Suicide. Palliative Care. Edited by: Emanuel LL, Librach SL. 2011, USA: Elsevier Saunders, 284-299. 2
Roland M, Rao SR, Sibbald B, Hann M, Harrison S, Walter A, Guthrie B, Desroches C, Ferris TG, Campbell EG: Professional values and reported behavior of doctors in the USA and the UK: quantitative survey. BMJ Qual Saf. 2011, 20: 515-521. 10.1136/bmjqs.2010.048173.
Colbert JA, Schulte J, Adler JN: Physician-assisted suicide-polling results. N Engl J Med. 2013, 369: e15-10.1056/NEJMclde1310667.
Cassel EJ: The nature of suffering and the goals of medicine. N Engl J Med. 1982, 306: 639-645. 10.1056/NEJM198203183061104.
Hudson PL, Schofield P, Kelly B, Hudson R, Street A, O’Çonnor M, Kristjanson LJ, Ashby M, Aranda S: Responding to desire to die statements from patients with advanced disease: recommendations for health professionals. Palliat Med. 2006, 20: 703-710. 10.1177/0269216306071814.
Foley KM: Competent care for the dying instead of physician-assisted suicide. N Engl J Med. 1997, 336: 54-58. 10.1056/NEJM199701023360109.
Ruijs CDM, Goedhart J, Kerkhof AJFM, van der Wal G, Onwuteaka-Philipsen BD: Recruiting end-of-life cancer patients in general practice in the Netherlands for a study on suffering and euthanasia requests. Fam Pract. 2011, 28: 689-695. 10.1093/fampra/cmr035.
Ruijs CDM, Onwuteaka-Philipsen BD, van der Wal G, Kerkhof AJFM: Unbearability of suffering at the end-of-life: the development of a new measuring device, the SOS-V. BMC Palliative Care. 2009, 8: 16-10.1186/1472-684X-8-16.
Walsh D, Donnely S, Rybicki L: The symptoms of advanced cancer: relationship to age, gender, and performance status in 1,000 patients. Support Care Cancer. 2000, 8: 175-179. 10.1007/s005200050281.
Homsi J, Walsh D, Rivera N, Rybicki LA, Nelson KA, LeGrand SB, Davis M, Naughton M, Gvozdjan D, Pham H: Symptom evaluation in palliative medicine: patient report vs systematic assessment. Support Care Cancer. 2006, 14: 444-453. 10.1007/s00520-005-0009-2.
Cleeland CS: Symptom burden: multiple symptoms and their impact as patient-reported outcomes. J Natl Cancer Inst Monogr. 2007, 37: 16-21.
Teunissen SCCM, Wesker W, Kruitwagen C, de Haes HCJM, Voest EE, de Graeff A: Symptom prevalence in patients with incurable cancer: a systematic review. J Pain Symptom Manage. 2007, 34: 94-104. 10.1016/j.jpainsymman.2006.10.015.
Cassell EJ: The Nature of Suffering and the Goals of Medicine. 2004, New York: Oxford University Press, 2
Kleinman A: The Illness Narratives. Suffering, Healing & the Human Condition. 1988, USA: Basic Books
Kissane DW: The relief of existential suffering. Arch Intern Med. 2012, 172: 1501-1505. 10.1001/archinternmed.2012.3633.
Chochinov HM, Kristjanson LJ, Breitbart W, McClement S, Hack TF, Hassard T, Harlos M: Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: a randomised controlled trial. Lancet Oncol. 2011, 12: 753-762. 10.1016/S1470-2045(11)70153-X.
Frankl VE: Man’s Search for Meaning. 2004, Londen: Rider Books, 5
Yalom ID: Existential Psychotherapy. 1980, United States of America: Basic Books
Breitbart W, Rosenfeld B, Gibson C, Pessin H, Poppito S, Neson C, Tomarken A, Kosinsky Timm A, Berg A, Jacobsen C, Sorger B, Abbey J, Olden M: Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psychooncology. 2010, 19: 21-28. 10.1002/pon.1556.
Muskin PR: The patient-physician relationship. The request to die. Role for a psychodymamic perspective on physician-assisted suicide. JAMA. 1998, 279: 323-328. 10.1001/jama.279.4.323.
Kissane DW, Clarke DM: Demoralization syndrome-a relevant psychiatric diagnosis for palliative care. J Palliat Care. 2001, 17: 12-21.
Pessin H, Rosenfeld B, Breitbart W: Assessing psychological distress near the end of life. Am Behav Sci. 2002, 46: 357-372. 10.1177/000276402237769.
Sachs E, Kolva E, Pessin H, Rosenfeld B, Breitbart W: On sinking and swimming: the dialectic of hope, hopelessness, and acceptance in terminal cancer. Am J Hosp Palliat Care. 2012, 30: 121-127.
LeMay K, Wilson KG: Treatment of existential distress in life threatening illness: a review of manualized interventions. Clin Psychol Rev. 2008, 28: 472-493. 10.1016/j.cpr.2007.07.013.
Wilson KG, Chochinov HM, McPherson CJ, LeMay K, Allard P, Chary S, Gagnon PR, Macmillan K, De Luca M, O’Shea F, Kuhl D, Fainsinger RL: Suffering with advanced cancer. J Clin Oncol. 2007, 25: 1691-1697. 10.1200/JCO.2006.08.6801.
Boston P, Bruce A, Schreiber R: Existential suffering in the palliative care setting: an integrated literature review. J Pain Symptom Manage. 2011, 41: 604-618. 10.1016/j.jpainsymman.2010.05.010.
Block SD: Psychological considerations, growth, and transcendence at the end of life. The art of the possible. JAMA. 2001, 285: 2898-2905. 10.1001/jama.285.22.2898.
Strang P, Strang S, Hultborn R, Arnér S: Existential pain—an entity, a provocation, or a challenge?. J Pain Symptom Manage. 2004, 27: 241-250. 10.1016/j.jpainsymman.2003.07.003.
Morita T, Kawa M, Honke Y, Kohara H, Maeyama E, Kizawa Y, Akechi T, Uchitomi Y: Existential concerns of terminally ill cancer patients receiving specialized palliative care in Japan. Support Care Cancer. 2004, 12: 137-140. 10.1007/s00520-003-0561-6.
Breitbart W, Poppito S, Rosenfeld B, Vickers AJ, Li Y, Abbey J, Olden M, Pessin H, Lichtenthal W, Sjoberg D, Cassileth BR: Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. J Clin Oncol. 2012, 30: 1304-1309. 10.1200/JCO.2011.36.2517.
Shoemaker LK, Estfan B, Induru R, Walsh TD: Symptom management: an important part of cancer care. Clev Clin J Med. 2011, 78: 25-34. 10.3949/ccjm.78a.10053.
Jansen-van der Weide MC, Onwuteaka-Philipsen BD, van der Wal G: Granted, undecided, withdrawn and refused requests for euthanasia and physician-assisted suicide. Arch Intern Med. 2005, 165: 1698-1704. 10.1001/archinte.165.15.1698.
Haverkate I, Onwuteaka-Philipsen BD, van der Heide A, Kostense PJ, van der Wal G, van der Maas PJ: Refused and granted requests for euthanasia and assisted suicide in the Netherlands: interview study with structured questionnaire. BMJ. 2000, 321: 865-866. 10.1136/bmj.321.7265.865.
Pearlman RA, Hsu C, Starks H, Back AL, Gordon JR, Bharucha AJ, Koenig BA, Battin MP: Motivations for physician-assisted suicide. Patient and family voices. J Gen Intern Med. 2005, 20: 234-239. 10.1111/j.1525-1497.2005.40225.x.
Loggers ET, Starks H, Shannon-Dudley M, Back AL, Appelbaum FR, Stewart FM: Implementing a death with dignity program at a comprehensive cancer center. N Engl J Med. 2013, 368: 1417-1424. 10.1056/NEJMsa1213398.
Rurup ML, Pasman HRW, Goedhart J, Deeg DJH, Kerkhof AJFM, Onwuteaka-Philipsen BD: Understanding why older people develop a wish to die. A qualitative interview study. Crisis. 2011, 32: 204-216.
Ganzini L, Dobscha SK, Heintz RT, Press N: Oregon physicians’ perceptions of patients who request assisted suicide and their families. J Palliat Med. 2003, 6: 381-390. 10.1089/109662103322144691.
Wilson KG, Chochinov HM, McPherson CJ, Skirko MG, Allard P, Chary S, Gagnon PR, Macmillan K, De Luca M, O’Shea F, Kuhl D, Fainsinger RL, Karam AM, Clinch JJ: Desire for euthanasia or physician assisted suicide in palliative cancer care. Health Psychol. 2007, 26: 314-323.
Chochinov HM: Thinking outside the box: depression, hope, and meaning at the end of life. J Palliat Care. 2003, 6: 973-977.
Khan L, Wong R, Li M, Zimmermann C, Lo C, Gagliese L, Rodin G: Maintaining the will to live of patients with advanced cancer. Cancer J. 2010, 16: 524-531. 10.1097/PPO.0b013e3181f45b90.
Chochinov HM, Tataryn D, Clinch JJ, Dudgeon D: Will to live in the terminally ill. Lancet. 1999, 354: 816-819. 10.1016/S0140-6736(99)80011-7.
Chochinov HM, Wilson KG, Enns M, Mowchun N, Lander S, Levitt M, Clinch JJ: Desire for death in the terminally ill. Am J Psychiatry. 1995, 152: 1185-1191.
Rodin G, Zimmermann C, Rydall A, Jones J, Shepherd FA, Moore M, Fruh M, Donner A, Gagliese L: The desire for hastened death in patients with metastatic cancer. J Pain Symptom Manage. 2007, 33: 661-674. 10.1016/j.jpainsymman.2006.09.034.
Breitbart W, Rosenfeld B, Pessin H, Kaim M, Funesti-Esch J, Galietta M, Nelson CJ, Brescia R: Depression, hopelessness, and desire for hastened death in terminally ill cancer patients with cancer. JAMA. 2000, 284: 2907-2911. 10.1001/jama.284.22.2907.
Ganzini L, Goy ER, Dobscha SK: Prevalence of depression and anxiety in patients requesting physicians’ aid in dying: cross sectional survey. BMJ. 2008, 337: a1682-10.1136/bmj.a1682.
Ruijs CDM, Kerkhof AJFM, van der Wal G, Onwuteaka-Philipsen BD: Depression and explicit requests for euthanasia in end-of-life cancer patients in primary care in the Netherlands: a longitudinal, prospective study. Fam Pract. 2011, 28: 393-399. 10.1093/fampra/cmr006.
Monforte-Royo C, Villavicencio-Chavez C, Tomas-Sabado J, Balaguer A: The wish to hasten death: a review of clinical studies. Psychooncology. 2011, 20: 795-804. 10.1002/pon.1839.
Hudson LP, Kristjanson LJ, Ashby M, Kelly B, Schofield P, Hudson R, Aranda S, O’Connor M, Street A: Desire for hastened death in patients with advanced disease and the evidence base of clinical guidelines: a systematic review. Palliat Med. 2006, 20: 693-701. 10.1177/0269216306071799.
Mol A: The Logic of Care. Health and the Problem of Patient Choice. 2008, Oxon: Routledge, 1
Ponsioen BP: Deliberation between physician and patient concerning active euthanasia at the patient’s home. Ned Tijdschr Geneesk. 1997, 141: 921-924. Dutch, English abstract
Thulesius HO, Scott H, Helgesson G, Lynӧe N: De-tabooing dying control- a grounded theory study. BMC Palliative Care. 2013, 12: 13-10.1186/1472-684X-12-13.
Fried TR, Stein MD, O’Sullivan PS, Brock DW, Novack DH: Limits of patient autonomy. Physician attitudes and practices regarding life-sustaining treatments and euthanasia. Arch Intern Med. 1993, 153: 722-728. 10.1001/archinte.1993.00410060032006.
Hoglend P, Bogwald KP, Amlo S, Marble A, Ulberg R, Sjaastad MC, Sorbye O, Heyerdahl O, Johansson P: Transference interpretations in dynamic psychotherapy: do they really yield sustained effects?. Am J Psychiatry. 2008, 165: 763-771. 10.1176/appi.ajp.2008.07061028.
Karlsson M, Milberg A, Strang P: Dying cancer patients’ own opinions on euthanasia: an expression of autonomy? A qualitative study. Palliat Med. 2011, 26: 34-42.
Hamilton NG, Hamilton CA: Competing paradigms of response to assisted suicide requests in Oregon. Am J Psychiatry. 2005, 162: 1060-1064. 10.1176/appi.ajp.162.6.1060.
Lloyd-Williams M, Reeve J, Kissane D: Distress in palliative care patients: developing patient-centred approaches to clinical management. Eur J Cancer. 2008, 44: 1133-1138. 10.1016/j.ejca.2008.02.032.
Georges JJ, The AM, Onwuteaka-Philipsen BD, van der Wal G: Dealing with requests for euthanasia: a qualitative study investigating the experience of general practitioners. J Med Ethics. 2008, 34: 150-155. 10.1136/jme.2007.020909.
Henry M, Cohen SR, Lee V, Sauthier P, Provencher D, Drouin P, Gauthier P, Gotlieb W, Lau S, Drummond N, Gilbert L, Stanimir G, Sturgeon J, Chasen M, Mitchell J, Nuoxin Huang L, Ferland MK, Mayo N: Meaning-Making intervention (MMi) appears to increase meaning in life in advanced ovarian cancer: a randomized controlled pilot study. Psychooncology. 2010, 19: 1340-1347. 10.1002/pon.1764.
Watson M, Kissane D: Handbook of Psychotherapy in Cancer Care. 2011, Chichester: Wiley-Blackwell
Zhang B, Nilsson ME, Prigerson HG: Factors important to patients’ quality of life at the end of life. Arch Intern Med. 2012, 172: 1133-1142.
Phelps AC, Lauderdale KE, Alcorn S, Dillinger J, Balboni MT, van Wert M, VanderWeele TJ, Balboni TA: Addressing spirituality within the care of patients at the end of life: perspectives of patients with advanced cancer, oncologists, and oncology nurses. J Clin Oncol. 2012, 30: 2538-2544. 10.1200/JCO.2011.40.3766.
Maltoni M, Scarpi E, Rosati M, Derni S, Fabbri L, Martini F, Amadori D, Nanni O: Palliative sedation in end-of-life care and survival: a systematic review. J Clin Oncol. 2012, 30: 1378-1383. 10.1200/JCO.2011.37.3795.
Bruera E: Palliative sedation: when and how?. J Clin Oncol. 2012, 30: 1258-1259. 10.1200/JCO.2011.41.1223.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-684X/13/62/prepub
Acknowledgements
The study was supported by the Netherlands Organization for Scientific Research (NOW); the Aspasia program. We thank Janneke Goedhart who was the study coordinator of this research and administered most interviews. We thank Jos de Keijser for assessing the qualitative data. We thank Narayanswami Sreeram and Jennifer Ruijs for linguistic revision.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CR had the initial idea for this study and wrote the initial research proposal. AK, GW and BOP commented and contributed to the final research proposal. CR and BOP analyzed the data. CR wrote the paper, which was critically red by all authors. All contributors had access to all data and can take responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ruijs, C.D., van der Wal, G., Kerkhof, A.J. et al. Unbearable suffering and requests for euthanasia prospectively studied in end-of-life cancer patients in primary care. BMC Palliat Care 13, 62 (2014). https://doi.org/10.1186/1472-684X-13-62
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-684X-13-62