Abstract
Background
Perforation of gut by sharp metallic objects is rare and rarer still is their migration to sites like liver. The symptoms may be non-specific and the discovery of foreign body may come as a radiological surprise to the unsuspecting clinician since the history of ingestion is difficult to obtain.
Case report
A unique case of a broken sewing needle in the liver causing a hepatic abscess and detected as a radiological surprise is presented. The patient had received off and on treatment for pyrexia for the past one year at a remote primary health center. Exploratory laparotomy along with drainage of abscess and retrieval of foreign body relieved the patient of his symptoms and nearly one-year follow up reveals a satisfactory recovery.
Conclusion
It is very rare for an ingested foreign body to lodge in the liver and present as a liver abscess. An ultrasound and a high clinical suspicion index is the only way to diagnose these unusual presentations of migrating foreign bodies. The management is retrieval of the foreign body either by open surgery or by percutaneous transhepatic approach but since adequate drainage of the abscess and ruling out of a fistulous communication between the gut and the liver is mandatory, open surgery is preferred.
Similar content being viewed by others
Background
It is not unusual to come across patients with perforation of gastrointestinal tract due to ingested foreign bodies in clinical practice, but the development of a secondary liver abscess is a rare condition. Recently our team successfully managed a patient with liver abscess produced secondary to a broken sewing needle penetration. There is only one previous published article, of Able et al. in 1971 [1]. The first case of hepatic abscess as a result of gastrointestinal perforation caused by a foreign body was published by Lambert in 1898[2]. The usual site of penetration is either stomach or duodenum and it is rare to get a history of ingestion in most of the cases.
Case report
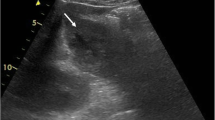
A 26 year old gentleman presented to the surgical wing with pain right upper abdomen and intermittent high grade fever with chills and rigors along with vomiting off and on for the last one year. There was no history of jaundice or urinary complaints. He had received treatment for his fever as a case of pyrexia of unknown origin at a remote district hospital in the form of antibiotics, antimalarial drugs and antipyretics with symptomatic relief after each episode. He was referred in view of the recurring and persisting symptoms and lack of facilities for ultrasound and other advanced investigations. Examination revealed a pale, febrile (temp:102*f) and toxic patient with tachycardia (pulse 110/mt), tachypnoea(R/R :20/mt). Abdomen was tense with tenderness in the right hypochondrium without any signs of peritoneal irritation. Liver was enlarged and tender. Blood chemistry was by and large within normal limits except for anaemia(Hb:9 gm%) and leucocytosis (Total count; 13000/cumm, polymorphs: 80%). Liver function tests were within normal limits except serum alkaline phosphatase which was raised, serum bilirubin and urine examination were normal. X-ray abdomen revealed a foreign body (? needle: fig 1) in the region of the liver. Ultrasound examination of the abdomen (fig 2) and contrast enhanced computed tomography scan(fig 3) confirmed the presence of a needle in the right lobe of the liver along with an abscess of the size 6.5 × 6 × 4 cm in the segment V(according to the Couinaud's nomenclature of liver segments). Patient was started on 3rd generation cephalosporins(Cefotaxime), Metronidazole and subjected to exploratory laparotomy which revealed multiple adhesions in the region of segment V of the liver with omentum and duodenum however no obvious fistulous communication between the biliary system and the stomach or duodenum could be appreciated. There was an abscess of the size of 6.5 × 6 × 4 cm in the segment V (five), about 200 cc of pus was drained and a broken sewing needle of the size 3 cm(fig 4) was retrieved. After a thorough peritoneal lavage using normal saline and packing the cavity with omentum, abdomen was closed leaving a tube drain in situ. Antibiotics were revised based on the subsequent culture sensitivity report that showed Sretptococcus pyogenes and E. Coli. Postoperative recovery was good and one year follow up reveals a satisfactory outcome. It could be suspected that an accidentally ingested broken sewing needle made its way in to the right lobe of the liver after penetration of the duodenum or stomach as was evident at laparotomy in the form of adhesions between the stomach, duodenum and omentum with the right lobe of liver.
Conclusion and Discussion
Most ingested foreign bodies pass through the gastrointestinal tract uneventfully within one week[1, 3–7]. The reported incidence of foreign bodies penetrating the gut is less than 1%, the objects being pointed or sharp in most of the cases like tooth picks, sewing needles, dental plates, fish bones and chicken bones etc. [8, 9]. The most common sites of perforation of the gut by foreign bodies are ileocecal junction and recto sigmoid region. The foreign body migrating to liver and producing liver abscess is indeed rare with less than 20 cases reported in the world literature [9]. The classical presentation of hepatic abscess like fever, abdominal pain and jaundice is present in only a small number of patients and may be associated with features of cholangitis like high grade fever with chills and rigors and jaundice. Most patients have non specific symptoms such as anorexia, vomiting or weight loss with leucocytosis or increased transaminases, bilirubin or alkaline phosphatase[10–13] The migrating foreign body may remain silent for a long time and may only be discovered if there are features of infection or abscess formation. In one reported case of unexpected death the cause discovered on autopsy was a migrating foreign body(portion of chicken fibula) and the prolonged time course of illness, with relatively non specific symptoms and signs resulted in establishment of diagnosis only at autopsy[12]. Presentation of a migrating foreign body (tooth pick)as a granulomatous liver abscess has been reported one month after ingestion and it required a partial lateral resection of the granulomatous tumor to retrieve the foreign body and drain the abscess[14]. With no history of foreign body ingestion being usually available these patients have a delayed presentation and may get treated like any other case of pyrexia of unknown origin. The clinical suspicion index has to be high particularly in the absence of specific signs and symptoms. An ingested foreign body may be identified with plain X-ray abdomen, if radio opaque however ultrasound of the abdomen and computed tomography scans are essential in making an accurate localization of the foreign body embedded in the liver [15–20]. Although the site of penetration of the gut may not be ascertained in majority of cases, the usual site of perforation has been observed to be the stomach or duodenum and more commonly the foreign body is lodged in the left lobe of the liver for some unknown reasons (table 1)[9]. Streptococcus constellatus which is found in the mouths of healthy individuals, if grown in the culture of the pus drained from the abscess confirms that the foreign body has been ingested [9]. The recommended treatment is exploratory laparotomy to drain the liver abscess and retrieve the foreign body. There is however one case report of a liver foreign body being retrieved by percutaneous transhepatic approach[9]. The technique involved retrieval through a sinus tract(produced by using a fine fibroscope) using endoscopic forceps under ultrasound guidance.
References
Able RM, Fischer JE, Hendren WH: Penetration of the alimentary tract by a foreign body with migration to the liver. Arch Surg. 1971, 102: 227-28.
Lambert A: Abscess of the liver of unusual origin. NY Med J. 1898, 177-78.
Crankson SJ: hepatic foreign body in a child. Pediatr Surg Int. 1997, 12: 426-427. 10.1007/s003830050170.
Lofti M: Foreign body in the liver. Int Surg. 1976, 61: 228-
Ward A, Ribchester J: Management of ingested foreign bodies in childhood. BMJ. 1978, 4: 469-472.
McCanse DE, Kurchin A, Hmshaw JR: Gastrointestinal foreign bodies. Am J Surg. 1981, 142: 335-
Maleki M, Evans WE: Foreign body perforation of the intestinal tract. Report of 12 cases and review of literature. Arch Surg. 1970, 102: 227-228.
Theodoropoulou A, Roussomoustakaki M, Michalodimitrakis MN: Fatalliver abscess caused by a fish bone. Lancet. 2002, 359 (9310): 977-10.1016/S0140-6736(02)07999-0.
Kumar S, Gupta NM: Foreign bodies migrating from gut to liver. Indian J Gastroenterol. 2000, 19 (1): 42-
Tsui BC, Mossey J: Occult liver abscess following clinically unsuspected ingestion of foreign bodies. Can J Gastroenterol. 1997, 11 (5): 445-8.
Horii K, Yamazaki O, Matsuyama M: Successful Treatment of a Hepatic Abscess that Formed Secondary to Fish Bone Penetration by Percutaneous Transhepatic Removal Of Foreign Body: Report of a Case. Jpn J Surg. 1999, 29: 922-926. 10.1007/s005950050540.
de la Vega M, Rivero JC, Ruiz L, Suarez S: A fish bone in the liver. Lancet. 2001, 358: 982-10.1016/S0140-6736(01)06106-2.
Chen SM, Shen MT, Lo GH: Duodenal perforation with liver abscess caused by ingestion of a chicken bone. Chin J Gastroenterol. 1993, 10: 312-319.
Bloom RR, Nakano PH, Grey SW: Foreign bodies of the gastrointestinal tract. Am Surg. 1986, 52: 618-21.
Byard RW, Gilbert JD: Hepatic abscess formation and unexpected death:a delayed complication of occult intraabdominal foreign body. Am J Forensic Med Pathol. 2001, 22 (1): 88-91. 10.1097/00000433-200103000-00018.
Kanazawa S, Ishigaki K, Miyake T: a granulomatous liver abscess which developed after a tooth pick penetrated the intestinal tract: report of a case. Surg Today. 2003, 33 (4): 312-4. 10.1007/s005950300071.
Drnosvsek V, Fontanez-Garcia D, Wakabayashi MN, Plavsic BM: Gastrointestinal case of the day. Pyogenic liver abscess caused by perforation caused by a swallowed wooden toothpick. Radiographics. 1999, 19 (3): 820-2.
Broome CJ, Peck RJ: Hepatic abscess complicating foreign body perforation of the gastric antrum: an ultrasound diagnosis. Clin Radiol. 2000, 55: 242-43. 10.1053/crad.1999.0339.
Masunaga S, Abe M, Imura T: Hepatic abscess secondary to a fish bone penetrating the gastric wall: CT demonstration. Comp Med Imag Graph. 1991, 15: 113-116.
Strauss JE, Balthazar FJ, Naidieh DP: Jejunal perforation by a tooth pick: CT demonstration. J Comput Assist Tomogr. 1985, 9: 812-814.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2482/3/8/prepub
Acknowledgement
A written consent was taken from the patient regarding publication of this case report in the Biomed Central Journal
Author information
Authors and Affiliations
Corresponding authors
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Chintamani, Singhal, V., Lubhana, P. et al. Liver abscess secondary to a broken needle migration- A case report. BMC Surg 3, 8 (2003). https://doi.org/10.1186/1471-2482-3-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2482-3-8