Abstract
Background
The purpose of this clinical study is to evaluate the feasibility of using 2-mm laparoscopic instruments to perform an appendectomy in patients with clinically suspected acute appendicitis and compare the outcome of this mini-laparoscopic or "needlescopic" approach to the conventional laparoscopic appendectomy.
Methods
Two groups of patients undergoing appendectomy over 24 months were studied. In the first group, needlescopic appendectomy was performed in 15 patients by surgeons specializing in advanced laparoscopy. These patients were compared with the second or control group that included 21 consecutive patients who underwent laparoscopic appendectomy. We compared the patients' demographic data, operative findings, complications, postoperative pain medicine requirements, length of hospital stay, and recovery variables. Differences were considered statistically significant at a p-value < 0.05.
Results
Patient demographics, history of previous abdominal surgery, and operative findings were similar in both groups. There was no conversion to open appendectomy in either group. No postoperative morbidity or mortality occurred in either group. The needlescopic group had a significantly shorter mean operative time (p = 0.02), reduced postoperative narcotics requirements (p = 0.05), shorter hospital stay (p = 0.04), and quicker return to work (p = 0.03) when compared with the laparoscopic group.
Conclusions
We conclude that the needlescopic technique is a safe and effective approach to appendectomy. When performed by experienced laparoscopic surgeons, the needlescopic technique results in significantly shorter postoperative convalescence and a prompt recovery.
Similar content being viewed by others
Background
Mini-laparoscopy is an emerging area of minimally invasive surgery that involves the use of miniature (2-mm diameter) laparoscopic instruments. The premise of mini-laparoscopy is that smaller instruments cause less abdominal wall trauma and, consequently, minimize pain and the stress response to surgery [1]. Previous clinical studies have proved the feasibility of the mini-laparoscopic or needlescopic approach to certain laparoscopic procedures including cholecystectomy, antireflux surgery, and adrenalectomy [2–5]. These reports have documented the safety of mini-laparoscopy and its advantage in leading to rapid recovery, shorter hospital stay, and excellent cosmesis.
Laparoscopic appendectomy has incited considerable controversy since its evolution. However, a number of clinical trials have supported the belief that laparoscopic appendectomy decreases hospital stay and shortens recovery time when compared with open appendectomy [6–8]. Mini-laparoscopic appendectomy is the natural extension to the application of these smaller instruments to the diagnosis and treatment of acute appendicitis. Despite the growing interest in needlescopic appendectomy, published series are currently lacking, and studies have been recommended to validate or refute the potential advantages of this technique [1]. The objective of this retrospective clinical study is to examine the safety and efficacy of needlescopic appendectomy and compare its outcome with that of the conventional laparoscopic approach.
Methods
The study included patients older than age 18 years with the diagnosis of acute appendicitis. Patients were considered a candidate for appendectomy according to the standard indications for surgery and based on clinical evaluation, laboratory values, and diagnostic imaging. Patients with bleeding diathesis were excluded from the study. No definitive criteria were established to exclude patients from the mini-laparoscopic group; however, three patients, one with extreme morbid obesity and two with preoperatively documented abscesses, were denied the mini-laparoscopic approach. Experienced laparoscopic surgeons were available for each procedure, but surgeons with a dedicated laparoscopic practice were the only physicians performing the mini-laparoscopic appendectomies.
Two groups of patients were included in the study over the 24-month period. The medical records of patients entered into the study during the initial 10 months were reviewed retrospectively. For the subsequent 14 months, data were collected prospectively. The following were evaluated in each group: age, gender, body mass index, history of previous abdominal surgery, operative observations, operative time, complications, postoperative narcotics requirements, length of hospital stay, and length of time required for the patient to return to work or normal activity.
The mini-laparoscopic technique
The patient was positioned supine on a multi-positional operating table with the arms tucked. General anesthesia was induced, and a Foley catheter and orogastric tube were inserted. Intravenous antibiotics were administered as per the surgeon's preference.
The primary surgeon stood on the patient's left side with the assistant on the right. Initial entry into the abdomen was made via an open approach at the umbilicus. Typically, a 12-mm port was inserted at this location. The insufflation pressure was automatically regulated and maintained at 12 to 15 mmHg. Two millimeter trocars were inserted: [1] laterally in the right mid-abdomen, and [2] supra-pubically.
The abdomen was thoroughly explored, and the appendix was identified. Tilting the operating table to the patient's left and in a head-down position facilitated visualization of the right iliac fossa. The operation was performed with 2-mm instruments and a 10-mm scope. The appendix was freed from its inflammatory attachments. If needed, the cecum was mobilized to free a retrocecal appendix. As needed, the appendix was elevated by applying a 2-mm EndoLoop (Ethicon, Sommerville, NJ, USA) to the tip. This helped to visualize the appendiceal mesentery, which was transected with a stapler inserted through the umbilical port while visualization was maintained with a 2-mm scope. The linear cutting stapler was also used to divide the base of the appendix. The resected appendix was placed in an extraction sac and removed through the 12-mm port. The abdominal cavity was copiously irrigated, and the fluid was suctioned before completion of the procedure. Throughout the operation, when a clip, stapler, entrapment bag, or an irrigation/suction device was introduced into the abdomen, the 12-mm port was used and the 10-mm scope was temporarily exchanged for a 2-mm scope.
The conventional laparoscopic technique used three ports (two 5-mm and one 10-mm port). The needlescopic technique was considered converted if one or more of the 2-mm ports were converted to a 5-mm port.
Statistical methods
Statistical analysis was performed using Wilcox rank sum tests or student's t test for continuous or ordered discrete variables and Fisher's exact test for categorical variables. A p-value < 0.05 was considered significant.
Results
Study patients consisted of 15 consecutive patients undergoing needlescopic appendectomy and 21 consecutive patients undergoing conventional laparoscopic appendectomy over 24 months. Both groups were similar in age, gender, body mass index, and history of previous abdominal surgery (Table 1). There was no conversion to open appendectomy in either group and no conversion from a needlescopic to a conventional laparoscopic technique.
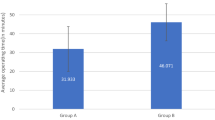
The gross intraoperative pathological findings were not statistically different when comparing the two groups (Table 2). The mean operative time was 55 minutes (range, 45–65 minutes) for the needlescopic group and 74 minutes (range, 38–120 minutes) for the laparoscopic group, statistically significantly less (p = 0.02) operative time for the needlescopic group.
No intra- or post-operative complications occurred with either technique. The mean in-hospital use of narcotic analgesia as measured in MSO4 equivalent was 11 mg in the patients who underwent needlescopic appendectomy compared with 34 mg in the laparoscopic group (p = 0.05). Other variables of postoperative recovery (length of hospital stay and time from operation to return to work or normal activity) were statistically significantly less in patients who underwent needlescopic appendectomy (Table 3).
Conclusions
In our experience, needlescopic appendectomy is a safe and feasible procedure. It appears to dimmish the consequences of the comparatively more invasive conventional laparoscopic appendectomy. This is reflected in the significantly reduced need for postoperative pain medications and an overall quicker recovery. Continued improvement in imaging and instrumentation is expected to further refine this technique and increase its utility.
References
Schauer PR, Ikramuddin S, Luketich JD: Minilaparoscopy. Semin Laparosc Surg. 1999, 6: 21-31.
Fuller PN: Microendoscopic surgery: a comparison of four microendoscopes and a review of the literature. Am J Obstet Gynecol. 1996, 174: 1757-1761.
Reardon PR, Kamelgard JI, Applebaum B, Rossman L, Brunicardi FC: Feasibility of laparoscopic cholecystectomy with miniaturized instrumentation in 50 consecutive cases. World J Surg. 1999, 23: 128-132.
Schauer PR, Ikramudin S, Nguyen NT, Luketich JD: Mini-laparoscopic antireflux surgery. SurgEndosc. 1998, 12: S42-
Gill IS, Soble JJ, Sung GT, Winfield HN, Bravo EL, Novick AC: Needlescopic adrenalectomy – the initial series: comparison with conventional laparoscopic adrenalectomy. Urology. 1998, 52: 180-186. 10.1016/S0090-4295(98)00185-X.
Nguyen DB, Silen W, Hodin RA: Appendectomy in the pre- and post-laparoscopic eras. J Gastrointest Surg. 1999, 3: 67-73. 10.1016/S1091-255X(99)80011-0.
Attwood SE, Hill AD, Murphy PG, Thornton J, Stephens RB: A prospective randomized trial of laparoscopic versus open appendectomy. Surgery. 1992, 112: 497-501.
Hellberg A, Rudberg C, Kullman E, Enochsson L, Fenyo G, Graffner H, Hallerback B, Johansson B, Anderberg B, Wenner J: Prospective randomized multicentre study of laparoscopic versus open appendectomy. Br J Surg. 1999, 86: 48-53. 10.1046/j.1365-2168.1999.00971.x.
Alvarez C, Voitk AJ: The road to ambulatory laparoscopic management of perforated appendicitis. Am J Surg. 2000, 179: 63-66. 10.1016/S0002-9610(99)00270-6.
Franklin ME, Balli J: Laparoscopic appendectomy. SAGES Mini/Office Laparoscopic Course Syllabus. 1998, April: 56-60.
Andersson RE, Hugander AP, Ghazi SH, Ravn H, Offenbartl SK, Nystrom PO, Olaison GP: Diagnostic value of disease history, clinical presentation, and inflammatory parameters of appendicitis. World J Surg. 1999, 23: 133-140.
Rosser JC, Palter SF, Rodas EB, Prosst RL, Rosser LE: Minilaparoscopy without general anesthesia for the diagnosis of acute appendicitis. J Soc Laparoendosc Surg. 1998, 2: 79-82.
Majeski J, Durst GG: Geriatric acute perforated appendicitis: atypical symptoms leading to a difficult diagnosis. South Med J. 1998, 91: 669-671.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2482/1/4/prepub
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing Interests
None declared.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mostafa, G., Matthews, B.D., Sing, R.F. et al. Mini-laparoscopic versus laparoscopic approach to appendectomy. BMC Surg 1, 4 (2001). https://doi.org/10.1186/1471-2482-1-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2482-1-4