Abstract
Background
Most fibromyalgia patients are seen in primary care (PC). However, the effectiveness of the treatments prescribed by general practitioners is usually minimal. The main objective of the present research is to assess the efficacy of structured psycho-educational intervention, combined with relaxation, developed to improve the quality of life of patients suffering fibromyalgia (FM). The second objective is to assess the cost-effectiveness of this multimodal intervention.
Method/Design
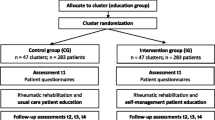
Design. Randomized controlled trial with a 12-month follow-up involving two groups, one of which is the intervention group that includes patients receiving a psychoeducational program and the other the control group consisting of patients treated for FM in the usual way.
Setting. Three urban PC centers in the province of Barcelona (Spain).
Sample. The total sample comprises 218 patients (over 18 years of age) suffering FM, selected from a database (Rheumatology service-Viladecans Hospital) of patients with this illness. Only those patients introduced in the database between the years 2005 and 2007 were included in the selection. Selected patients will be asked for written informed consent to participate in the study.
Intervention. Multi-component program including information about the illness, counselling about physical exercise and training in autogenic relaxation. The intervention consists of nine 2-hour sessions delivered during a two-month period. The pharmacological treatment prescribed by the physician was maintained in both groups.
Main variables. Sociodemographic characteristics, quality of life, use and cost of healthcare and social services.
Measures. Quality of life is to be measured with the FIQ and the EuroQol-5D, and the use of healthcare services with an adapted version of the Client Service Receipt Inventory (CSRI). These variables will be measured before the beginning of the program (baseline) and 1, 2, 6 and 12 months later.
Discussion
This research project is an attempt to demonstrate that a psycho-educational program implemented in the context of PC can produce a significant increase in the quality of life for patients with FM, as well as a decrease in the use of healthcare and social services, compared with usual care.
Trial registration
NCT00550966
Similar content being viewed by others
Background
Fibromyalgia (FM) is a chronic illness of unknown origin that provokes intense widespread pain and fatigue and affects people in the biological, psychological and social dimensions [1–3]. The diagnosis of FM is mainly clinical and the practitioner takes into account patient history, physical examination and laboratory evaluations. The American College of Rheumatology (ACR) established two major diagnostic criteria in 1990 [4]: first, a history of widespread pain for at least three months, and second, patient reporting of tenderness in at least 11 of 18 defined tender points when digitally palpated with about 4 Kg per unit area of force. The absence of reliable diagnostic tools has generated the need for employing subjective scales to assess the pain and fatigue of these patients [2].
The prevalence of FM in the general population is about 2–4%, and it is nine times more frequent in women than men [1, 3]. In PC consultations the prevalence is about 5–7% [5]. Given its high prevalence and morbidity, patients suffering FM present an elevated frequency of use index for healthcare resources.
Although the aetiology of FM is still unknown, it is probably multifactorial [6–9], which is why multidisciplinary and biopsychosocial approaches usually obtain better outcomes than symptomatic treatment alone [10–13]. The main goal of most treatments is to reduce muscular dysfunction and functional impotence caused by pain. Among pharmacological treatments, only a minority has demonstrated significant efficacy. As far as we know, there is evidence of the efficacy of amitriptyline and cyclobenzaprine, whereas studies focused on the efficacy of tramadol and selective serotonin re-uptake inhibitors have yielded only modest evidence [14].
Non-extenuating physical exercise and some relaxation therapies can also increase pain tolerance, producing a global improvement in the quality of life of fibromyalgia patients [15, 16]. Gowans et al [16] assessed physical functioning and mood state 6 and 12 months after the beginning of a supervised aerobic physical exercise program. These authors observed an improvement in participants' health when the program finished and 6 months later. Taggart et al [17] reported a satisfactory and significant increase in the quality of life of fibromyalgic patients after a 6-week relaxation program.
Another key component in current treatment of FM is the education of patients concerning their illness [18–20]. The main objective of educational programs is to increase skills in coping and healthy behaviour on the part of patients suffering FM. Scientific evidence has demonstrated that intensive education programs (between 6 and 17 sessions) improve pain symptoms, fatigue, insomnia and quality of life. These improvements continue 3 and 12 months later [14]. Furthermore, educational programs increase patient autonomy, reducing at the same time the consumption of medicines and use of healthcare services. The total cost of the continuous use of healthcare services by FM patients has not been estimated in Spain, but data from the USA reveal an annual cost of $2,274 per patient.
To date, it has not been demonstrated in Spain whether a multimodal program, combining autogenic relaxation and active healthcare education, produces a significant improvement in the quality of life of patients with FM. In addition, we do not know whether a multimodal program is more cost-effective than the treatment usually provided to these patients.
With this background, then, the main objective of the present research project will be to determine whether a multi-component psycho-educational program for treating FM leads to better quality of life (measured with the FIQ and the EuroQol-5D) at 1, 2, 6 and 12 months, than the usual care provided in Catalan Primary Health Care. The specific aims are to assess the degree of pain perceived by fibromyalgia patients attending the multimodal program, as well as the total direct costs (medication consumption and visits to public or private healthcare professionals) and indirect (work days lost), and cost-effectiveness associated with this psychoeducational intervention, compared to usual care.
Methods/Design
Design
Controlled trial with a random allocation of participants in two alternative branches:
1. Implementation of a multimodal psycho-educational program to improve quality of life in FM (intervention group).
2. Usual care of FM (control group).
Evaluation of treatment outcomes will be carried out at the patient level, with individual evaluation at baseline and 1, 2, 6, and 12 months after the beginning of the intervention.
Setting and study sample
Three primary health care centres (Viladecans-2, Gavà-1 and Gavà-2) in the province of Barcelona (Catalonia, Spain) voluntarily participated for the study. The sample pool (n = 530) comprises only those patients included in a FM database of the Viladecans Hospital for the years 2005 and 2006. In the event of a lack of participants, the plan is to recruit patients with FM included in the database during the year 2007.
Patients considered for inclusion will be those aged 18–75 years-old, contactable by telephone, who meet the diagnostic criteria of FM established by the ACR. The following patients will be excluded: those with a diagnosis not based on the ACR criteria, those with cognitive impairment or suffering from physical, mental/psychiatric limitations or a severe concurrent rheumatologic illness that impedes participation in the study evaluations, those who are not expected to live at least 12 months and those without schooling.
To calculate the sample size it was taken into account that we need to obtain a difference of at least 5 points in the FIQ between those that respond and those who are resistant to the intervention. The criterion of 5 points is based on two previous studies conducted with Spanish fibromyalgia patients [21, 22]. A total of 109 patients per condition is needed to conduct the study, assuming an alpha risk of 0.05 and a beta risk of < 0.20 in a bilateral contrast, a standard error of 12.1 reported in a previous study [21], and a 15% dropout rate.
Data collection and ethical aspects
First, patients that meet the inclusion criteria will be phoned by a research assistant who is a psychologist. Second, the research assistant will make an appointment with those patients that agree to participate in the study. Third, written consent will be obtained before the beginning of the study. Participants will be provided with a general overview of the aims and activities of the study. They will be also informed that they may choose to drop out at any time with the guarantee that they will continue to receive the treatment considered most appropriate by their physician. Patients in the control group will receive the treatment considered most appropriate by their physician.
Results will be monitored and most of data collected by means of standard questionnaires conducted in face-to-face interview by the research assistant, who has been trained in the administration of the instruments. The research assistant does not know which study group the patients being interviewed belong to ("blind"). Follow-up assessments shall take place at 1, 2, 6 and 12 months after the inclusion of the patient (see Table 1).
Variables and instruments of measurement
The study protocol was approved by the research ethics committee of the Foundation Jordi Gol i Gorina (Barcelona) and consists of the following materials:
1. Sociodemographic characteristics: Gender, birth date, address, marital status, education level, work status.
2. History of the illness: age of onset, date of the first diagnosis, pharmacological treatments (oral antidepressants, benzodiazepines-hypnotics, muscular relaxants and non-steroid analgesic and anti-inflammatory medications) and non-pharmacological treatments (physical exercise, relaxation techniques, cognitive-behavioural therapy) received during the previous 6 months.
3. Questionnaire on chronic medical condition.
4. Fibromyalgia Impact Questionnaire (FIQ-Spanish version) [23]: Instrument that measures physical function, work, and well-being, and contains visual analogue scales (VAS) for pain, sleep, fatigue, stiffness, anxiety and depression. A total score may be obtained after normalization of some items (between 0–10) and adding them to the VAS. Total scores range between 0–80 (without job items), with a higher score indicating a negative impact.
5. EuroQoL-5D questionnaire (EQ-5D – Spanish version) [22]: Generic instrument of health-related quality of life. It has two parts: Part 1 records self-reported problems in each of five domains: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each domain is divided into three levels of severity corresponding to no problems, some problems, and extreme problems. Part 2 records the subject's self-assessed health on a Visual Analogue Scale (VAS); it is a vertical 10 cm line on which the best and worst imaginable health states score 100 and 0, respectively.
6. Client Service Receipt Inventory – adapted (CSRI – Spanish version) [24]: questionnaire for collecting information about use of healthcare and social care services, other economic impacts (such as time off work due to illness) and socio-demographic information. The variant used in this study was designed to collect retrospective data on service utilisation during the first and last six months after the beginning of the treatment.
Intervention program
Participants from the intervention group will undergo a multi-component psycho-educational program that deals with FM based on available scientific evidence. It includes measures and instruments that can be employed within the Catalan Primary Health Care, whereas the participants from the control group will receive only the treatment prescribed by their physician.
The intervention program consists of nine 2-hour sessions delivered during a two month period. Participants will be allocated in groups with a maximum of 18 subjects per group. All sessions will take place at the PC centres Gava-2 or Viladecans-2. The contents of each session are displayed in Table 2.
In order to avoid conversations concerning the psycho-educational program among patients from different groups, we will remind the participants from the intervention of the condition that they are not allowed to talk about the program with those persons that are not attending their group. Before baseline assessment, an explanatory note addressing this important issue will be delivered to the patients participating in the program.
Forecast execution dates
Initial recruitment of patients: September 2007
Deadline for recruitment of patients: November 2008
Deadline for period of patient monitoring: December 2009
Publication of results: 2010
Statistical analyses
Data collected will be analysed using SAS statistical analysis software (SAS Institute Inc. 1999. v8.0, 4th ed) and employing both quantitative and qualitative techniques.
First, the intervention and control groups will be compared in order to verify that there are no significant differences between them in socio-demographic terms, clinical baseline data, etc. We shall use mean and standard deviation (SD) in continuous variables and percentages in categorical variables. For comparisons we shall use the Student-T test for continuous variables and the Chi-square test for categorical variables. Non-parametric tests may also be used.
Given that we have one between-groups factor with two levels (2 Groups: Intervention and Control) and one within-subjects factor with five levels (Baseline and 4 follow-up assessments: 0, 1, 2, 6, and 12), a 2 × 5 mixed factorial ANOVA will be performed to study the effect of the psycho-educational program on the quality of life. Then, between-subjects planned comparisons may also be used (post-hoc comparisons with independent samples T-test). If we observe differences between groups in quality of life prior to treatment, one-way analyses of covariance will be carried out using baseline scores as a covariate). In addition, we shall carry out a logistic regression analysis taking the groups as dependent variable (the target variable is a categorical variable with two categories: Intervention and Control) and the collected measures as independent variables. This analysis will let us to know the association between the intervention and the cost of the healthcare resources, controlling for the rest of variables.
Cost-utility analyses
Societal cost perspective will be used for the calculation of costs. Direct costs are going to be calculated by adding the costs derived from any medication and use of health-related services (general practitioner sessions, specialized medical sessions, emergency room sessions, and hospital in-patient stay). The cost of medications will be calculated by determining the price per milligram during the study, according to the International Vademecum (Red Book) 2007–2009, including value-added tax. Total costs of pharmacological treatment will be calculated by multiplying the price per milligram by the daily dose in milligrams and the number of days receiving such treatment. Costs derived from the use of health-related services will be calculated considering the SOIKOS unit costs database (25). Indirect costs will be calculated considering the days under sick leave and multiplying them by the minimum daily wage in Spain for 2007–2009. Finally, total costs are going to be calculated by adding direct and indirect costs.
In Spain, the National Healthcare Service (NHS) is financed by the general taxes levied by the state. In the municipalities where the study is carried out, it is administered by the autonomous government of Catalonia. Medical visits and hospital admissions are fully covered by the NHS. Medications prescribed are fully covered for retired persons, and partially for those still employed. Sick leave requires a physician's authorization, and patients unable to work continue receiving most of their salary.
When performing cost-utility analyses, two or more therapeutical options are compared in order to determine which one is the best for maximizing the benefits in light of the available resources [25, 26]. This is achieved by calculating the relationship between the costs of a given intervention (e.g. A) and its consequences, expressed in QALYs, compared with another (e.g. B). This relative value is called incremental cost-utility ratio (ICUR), and it expresses the relationship between the costs and effects of one intervention compared with another.
As the duration of the study is only 12 months, neither costs nor outcomes are subject to discounting [26]. Treatment costs during 12 months follow-up will be modelled by a multivariate gamma regression with a log link. Gamma modelling has been suggested as a suitable choice for analysing cost data, taking into account the skewing of the distribution of the cost data [27, 28]. QALYs gained in the first and last six months after the beginning of the program will be approximated by measuring the area under the curve (Figure 1).
In the Figure 1, d0–6 is the incremental treatment effect on change in EQ-5D utility score for the first 6 months and d6–12the incremental treatment effect on change in EQ-5D utility score for the last 6 months. These incremental treatment effects will be estimated using multivariate ordinary least squares regressions, adjusting for baseline differences among treatment groups. The covariates included in the models will be: age, gender, years of education, employment and marital status, baseline FIQ and EQ-5D utility scores, and type of medication prescribed. To address uncertainty in the ICUR sampling distribution, non-parametric bootstrapping with five thousand replications will be carried out for each treatment comparison [29].
Discussion
FM is a chronic illness that seriously alters the well-being of patients [1–3, 30]. One of the main expected contributions of the present project is that we will have the opportunity to assess not only whether a multimodal psycho-educational program is feasible in primary health care, but also whether it is more cost-effective than the usual care provided for FM in this context.
Although FM has an irregular course that causes oscillations in the patients' quality of life, the random assignment of the participants to the conditions will minimize the differences not produced by the intervention. Baseline comparisons between groups will permit detection of possible pre-treatment differences.
In our opinion, the application of the program in PC entails a low outlay because nursing personnel may be trained to develop the program, as in other recent educational programs developed for a number of chronic illnesses [31, 32].
References
Collado A, Alijotas J, Benito P, Alegre C, Romera M, Sanudo I, Martin R, Peri JM, Cots JM: Consensus report on the diagnosis and treatment of fibromyalgia in Catalonia. Med Clin (Barc). 2002, 118: 745-9.
Leza JC: Fibromyalgia: a challenge for neuroscience. Rev Neurol. 2003, 36: 1165-75.
Carmona L, Villaverde V, Hernández-García C, Ballina J, Gabriel R, Laffon A, EPISER Study Group: The prevalence of rheumatoid arthritis in the general population of Spain. Rheumatology (Oxford). 2002, 41: 88-95. 10.1093/rheumatology/41.1.88.
Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P: The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum. 1990, 33: 160-72. 10.1002/art.1780330203.
Bosch E, Sáenz N, Valls M, Viñolas S: Study of quality of life of patients with fibromyalgia: impact of a health education programme. Aten Primaria. 2002, 30: 16-21.
Sedó R, Ancochea J: A reflection on fibromyalgia. Aten Primaria. 2002, 29: 562-564.
Brecher LS, Cymet TC: A practical approach to fibromyalgia. J Am Osteopath Assoc. 2001, 101: S12-7.
Desmeules JA, Cedraschi C, Rapiti E, Baumgartner E, Finckh A, Cohen P, Dayer P, Vischer TL: Neurophysiologic evidence for a central sensitization in patients with fibromyalgia. Arthritis Rheum. 2003, 48: 1420-9. 10.1002/art.10893.
Nampiaparampil DE, Shmerling RH: A review of fibromyalgia. Am J Manag Care. 2004, 10: 794-800.
Lemstra M, Olszynski WP: The effectiveness of multidisciplinary rehabilitation in the treatment of fibromyalgia: a randomized controlled trial. Clin J Pain. 2005, 21: 166-74. 10.1097/00002508-200503000-00008.
Sprott H: What can rehabilitation interventions achieve in patients with primary fibromyalgia?. Curr Opin Rheumatol. 2003, 15: 145-50. 10.1097/00002281-200303000-00011.
Andollo I, Sánchez A, Grandes G: Inadequate analysis casts doubt on the benefits of health education in fibromyalgia [Abstract]. Aten Primaria. 2003, 31: 204-10.1157/13044280.
Denison B: Touch the pain away: new research on therapeutic touch and persons with fibromyalgia syndrome. Holist Nurs Pract. 2004, 18: 142-51.
Direcció General de Planificació i Avaluació Sanitaria. Departament de Salut. Generalitat de Catalunya: Nou model d'atenció a la fibromiàlgia i la síndrome de fatiga crònica. Barcelona. 2006
Schachter CL, Busch AJ, Peloso PM, Sheppard MS: Effects of short versus long bouts of aerobic exercise in sedentary women with fibromyalgia: a randomized controlled trial. Phys Ther. 2003, 83: 340-58.
Gowans SE, Dehueck A, Voss S, Silaj A, Abbey SE: Six-month and one-year follow-up of 23 weeks of aerobic exercise for individuals with fibromyalgia. Arthritis Rheum. 2004, 51: 890-8. 10.1002/art.20828.
Taggart HM, Arslanian CL, Bae S, Singh K: Effects of T'ai Chi exercise on fibromyalgia symptoms and health-related quality of life. Orthop Nurs. 2003, 22: 353-60. 10.1097/00006416-200309000-00013.
Cedraschi C, Desmeules J, Rapiti E, Baumgartner E, Cohen P, Finckh A, Allaz AF, Vischer TL: Fibromyalgia: a randomised, controlled trial of a treatment programme based on self management. Ann Rheum Dis. 2004, 63: 290-6. 10.1136/ard.2002.004945.
King SJ, Wessel J, Bhambhani Y, Sholter D, Maksymowych W: The effects of exercise and education, individually or combined, in women with fibromyalgia. J Rheumatol. 2002, 29: 2620-7.
Mannerkorpi K, Ahlmen M, Ekdahl C: Six- and 24-month follow-up of pool exercise therapy and education for patients with fibromyalgia. Scand J Rheumatol. 2002, 31: 306-10. 10.1080/030097402760375223.
Martínez JE, Ferraz MB, Inoe E, Atra E: Fibromyalgia versus rheumatoid arthritis: a longitudinal comparison of the quality of life. J Rheumatol. 1995, 22: 270-4.
Badia X, Roset M, Montserrat S, Herdman M, Segura A: The Spanish version of EuroQol: a description and its applications. European Quality of Life scale. Med Clin (Barc). 1999, 112 (Suppl 1): 79-85.
Rivera J, González T: The Fibromyalgia Impact Questionnaire: A validated Spanish version to assess the health status in women with fibromyalgia. Clin and Exp Rheumatol. 2004, 22: 554-60.
Knapp M, (PSSRU and Centre for Economics of Mental Health, Institute of Psychiatry, University of Kent): Economic Evaluation of Mental Health Care. 1995, Ashgate Publishing Group
Centro de Estudios de Economía de la Salud y Política Social: Base de Datos de Costes Soikos sanitarias. Barcelona. 2001
Drummond MF, Sculpher MJ, Torrance GW, O'Brien BJ, Stoddart GL: Methods for the Economic Evaluation of Health Care Programmes. 2005, New York: Oxford University Press, Third
Dodd S, Bassi A, Bodger K, Williamson P: A comparison of multivariable regression models to analyse cost data. J Eval Clin Pract. 2006, 12: 76-86. 10.1111/j.1365-2753.2006.00610.x.
Austin PC, Ghali WA, Tu JV: A comparison of several regression models for analysing cost of CABG surgery. Stat Med. 2003, 22: 2799-815. 10.1002/sim.1442.
Efron B, Tibshirani RJ: An introduction to the bootstrap. 1998, Boca Ratón, FL: Chapman and Hall/CRC, 2
Ejlertsson G, Edén L, Leden I: Predictors of positive health in disability pensioners: a population-based questionnaire study using Positive Odds Ratio. BMC Public Health. 2002, 2: 20-10.1186/1471-2458-2-20.
Laatikainen T, Dunbar JA, Chapman A, Kilkkinen A, Vartiainen E, Heistaro S, Philpot B, Absetz P, Bunker S, O'Neil A, Reddy P, Best JD, Janus ED: Prevention of Type 2 Diabetes by lifestyle intervention in an Australian primary health care setting: Greater Green Triangle (GGT) Diabetes Prevention Project. BMC Public Health. 2007, 7: 249-10.1186/1471-2458-7-249.
Drevenhorn E, Kjellgren KI, Bengtson A: Outcomes following a programme for lifestyle changes with people with hypertension. J Clin Nurs. 2007, 16: 144-51. 10.1111/j.1365-2702.2005.01493.x.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2474/9/2/prepub
Acknowledgements
The research project and AM's predoctoral contract are funded by a grant from the "Agència d'Avaluació de Tecnologia i Recerca Mèdiques" (AATRM 077/25/06). JVL is grateful to the "Ministerio de Sanidad y Consumo, Instituto de Salud Carlos III" (Red RD06/0018/0017) for a postdoctoral contract. We would like to acknowledge the FibroQol group the helpful assistance on data collection (Primary Health Centre Gavà 1: Francisco J. Gómez, José L. Caballé, Amelia Prieto, Elena Carrera, Eva Alonso, Laura Pérez, Nuria Gutiérrez, Rosa M. Aranzana, Montserrat Espuga, Jugo Jiménez, Elena Fina. Primary Health Centre Gavà 2: Mariona Soler, Emilia Caramés, Estíbaliz Redondo, Inma García, Ángel Espín, Carmen Almirall, Josep Verdú, Lola Ruiz, Margarita García, Marta Sanavia. Primary Health Centre Viladecans 2: María C. García, Alicia Valer, Noelia Esplugas, María D. González, Estefanía San Juan, Adela Viniegra, Caterina Calvet, Cristina Montblanc, Rosa Vilafáfila, Pere Simonet, Luis López, Rosa Ramírez, Aige, Ángela Muñoz, Carmen Bentue, Carmen Vallduriola, de los Heros, Delgado).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
RF is the principal investigator and developed the original idea for the research. The study design was made by RF, MTP, ASB, EB, MJ, CV and JMR. These authors, with the help of JVL and AM, designed and planned the intervention that is going to be evaluated. ASB and JVL developed the statistical methods. All authors have corrected draft versions and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Fernández, R., Peñarubia, M.T., Luciano, J.V. et al. Effectiveness of a psycho-educational program for improving quality of life of fibromyalgia patients. BMC Musculoskelet Disord 9, 2 (2008). https://doi.org/10.1186/1471-2474-9-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2474-9-2