Abstract
Background
Vertebral fractures in patients with cystic fibrosis (CF) may contribute to an accelerated decline in lung function and can be a contraindication to lung transplantation. In this study, we examined longitudinal change in bone mineral density (BMD) and the prevalence of vertebral fractures in adult CF patients, without lung-transplant, attending a Canadian specialty clinic.
Methods
Retrospective chart review of all patients attending an Adult Cystic Fibrosis Clinic at Hamilton Health Sciences in Hamilton, Canada. Forty-nine of 56 adults met inclusion criteria. Chest radiographs were graded by consensus approach using Genant's semi-quantitative method to identify and grade fractured vertebrae. Dual x-ray absorptiometry (DXA) scans were also reviewed.
Results
The mean age of the cohort was 25.2 years (SD 9.4), 43% were male. The mean body mass index (BMI) was 19.8 (2.8) for males and 21.7 (5.1) for females. At baseline, the rate of at least one vertebral fracture was 16.3%; rising to 21.3% (prevalent and incident) after a 3-year follow-up. The mean BMD T-or Z-scores at baseline were -0.80 (SD 1.1) at the lumbar spine, -0.57 (SD 0.97) at the proximal femur, and -0.71 (SD 1.1) at the whole body. Over approximately 4-years, the mean percent change in BMD was -1.93% at the proximal femur and -0.73% at the lumbar spine.
Conclusion
Approximately one in five CF patients demonstrated at least one or more vertebral fractures. Moderate declines in BMD were observed. Given the high rate of vertebral fractures noted in this cohort of adult CF patients, and the negative impact they have on compromised lung functioning, regular screening for vertebral fractures should be considered on routine chest radiographs.
Similar content being viewed by others
Background
Cystic Fibrosis (CF) is among the most common fatal autosomal recessive genetic diseases in the Caucasian population. Since those born with CF are now living significantly longer, there is a definite need to address a range of erging comorbid conditions, which were not previously considered for a CF population. Low bone mineral density (BMD) is common in adult CF patients and has been termed CF-related bone disease [1, 2]. The underlying etiology of low BMD is likely multi-factorial [1–4], however several reports support the hypothesis that the inflammatory response to chronic pulmonary infection plays a significant role in bone loss [1, 3, 5].
In non-CF populations, vertebral fractures are the most common type of osteoporotic fracture [6] and have important consequences, including increased risk for subsequent fracture [7–11], increased mortality [8, 12–15], and reduced quality of life [16–19]. In a CF population, a further consequence of a vertebral (thoracic) fracture is an accelerated decline in lung function (i.e. structural alteration of the chest wall) and contraindication to lung transplantation, an important treatment option for CF patients [1, 2]. As CF patients often have routine chest radiographs, screening for vertebral fracture may be an important consideration in this population.
The pathophysiology of CF-related bone disease is not well understood and there are few longitudinal reports on BMD and vertebral fracture. Previous studies in this area have examined CF patients cross-sectionally or only over a short term. Two recent cross-sectional studies found a high rate of vertebral fracture in general CF populations [20, 21].
In our Canadian cohort, the purpose of this study was to examine: 1) longitudinal changes in BMD and 2) the rate of vertebral fractures in adults with CF, who have moderate to severe respiratory impairment and who have not undergone lung-transplant.
Methods
Study population
All patients who attended the Adult Cystic Fibrosis Clinic at Hamilton Health Sciences, McMaster University Medical Centre (Hamilton, Canada) during 2002 were considered for this study. To be included, patients must have had at least one chest radiograph or DXA scan in previous years (completed as part of routine care in the CF clinic). Patients who were accepted on a lung-transplant list or had received a prior organ transplant were excluded. CF was confirmed by a positive sweat test and deoxyribonucleic acid (DNA) analysis. Of 56 individuals attending the clinic during 2002, four were excluded due to the unavailability of radiographic results, and three patients were excluded due to a past lung transplant. The final cohort consisted of 49 patients. The Institutional Review Board at McMaster University approved the study.
Radiology review
The first and last available routine chest radiographs (separated by at least one year) taken between May 1996 and December 2003 were selected for each participant. Two board certified radiologists (authors MP and JO) independently reviewed chest radiographs (lateral and anterior posterior views) using a modified Genant's semi-quantitative method [22, 23]. This method distinguishes fractured vertebrae (grades 1, 2 and 3) from non-fractured vertebrae (grades 0 for no fracture, 0.5 for reduction of height of less than 20% or reduction in area of less than 10%). A deformity graded 1 and higher (excluding congenital or degenerative causes) indicates a reduction in vertebral height (anterior, posterior, or middle) of greater than or equal to 20–25%. Grade 1 is considered a mild fracture, Grade 2 a moderate fracture, and Grade 3 a severe fracture. Differences of scores between radiologists were resolved by consensus.
Bone densitometry
A medical physicist (author CW) reviewed all annual DXA scans of the lumbar spine, proximal femur (total region), and whole body taken during the study period. All DXA scans were performed on a Hologic QDR 4500A densitometer (Hologic Inc., Bedford, MA, USA). BMD measurements were reported in g/cm2, and T- or Z-scores. Expression of an adult BMD as a T-score incorporates the typical BMD loss from peak bone mass that is associated with aging as well as any BMD loss relative to an age-matched peer. By definition, a T-score is not applicable to children. Consequently for subjects aged 19 years or less, BMD values were expressed as Z-scores.
Clinical/laboratory variables
Research assistants abstracted clinical and demographic data from clinic charts for the nearest clinic visit within 9-months of both the baseline radiograph and DXA scan (i.e. if taken at non-coincident time periods). Data abstracted included height, weight; use of inhaled steroids, bisphosphonates, hormone replacement therapy, oral contraception, calcium and vitamin D supplements; laboratory tests and pulmonary functioning including forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC). Dietary calcium intake was not available. Charts were also reviewed for any evidence of oral corticosteroid use between the baseline and follow-up radiograph/DXA examinations and the cumulative number of milligrams taken was recorded.
Routine laboratory results were downloaded from the computerized hospital database. Phosphate, alkaline phosphatase, serum calcium, albumin, alanine aminotransferase (ALT), g-glutamyltransferase (GGT) and creatinine were measured with automatic analyzers. Commercially available kits (Nichols Institute Diagnostics, San Clemente, CA, USA) were used to measure parathyroid hormone (PTH; Nichols Advantage Bio-Intact PTH (1–84) immunometric assay) and 25-hydroxyvitamin D (25-OHD; Nichols Advantage 25-Hydroxyvitamin D assay).
Statistical analysis
Analyses were performed with SPSS (version 13.0; SPSS Inc., Chicago, IL, USA) and SAS/STAT (version 8.0; SAS Institute Inc., Cary, NC, USA) software packages. Clinical and laboratory variables are summarized as means and standard deviations, and medication/supplementation use (yes/no) as proportions. Due to deviations from normality and the small sample size of the fracture group, differences in baseline characteristics (continuous variables) between fracture versus non-fracture patients were determined by Mann-Whitney U-test. Fisher's exact test was used to examine differences between proportions.
For the BMD analysis, all individuals had two to five BMD measures during the course of the study. To incorporate all BMD measurements, a regression slope was calculated using all available measurements for each patient. The slope represents the average yearly bone mineral density change over the entire follow-up period for each patient. This analysis takes into account the differing numbers of BMD measurements and the length of follow-up for each patient. Separate analyses were performed for the lumbar spine, whole body, and proximal femur (average of right and left sides). Baseline BMD and variables that were significant in univariate analysis were included in multi-variable regression models to estimate percent BMD change per year. In all analyses, a 2-sided p-value of < 0.05 was considered significant.
Results
Overall, the mean age of the cohort was 25.2 years (SD 9.4), 43% were male. Seventy-five percent of the sample was between ages 15–31 years; 25% were ages 32–51 years. The median age was 23.0 years. Table 1 displays baseline patient characteristics for the fracture (prevalent/baseline) and non-fracture groups. The mean age of fracture patients was significantly higher than that of non-fracture patients (32.7 years versus 23.8). Males with vertebral fracture had significantly higher weight and body mass index (BMI) scores than those without. Several of the laboratory variables were higher in the fracture than non-fracture group (Table 1), however we lacked power to see this statistically. Creatinine was significantly higher in the fracture group.
At baseline, eight out of 49 patients (16.3%) had at least one prevalent Grade 1 fracture (Table 2). Multiple vertebral fractures were noted in four (8.2%) patients. A second radiograph was available for 47/49 patients. Neither of the two patients without a follow-up radiograph had a vertebral fracture noted at baseline. The mean follow-up between each patient's first and last radiograph was 3.3 years (SD 1.4). During this period, four new fractures occurred (incidence rate of 8.5%); three patients had a new first fracture, and one patient had an additional vertebral fracture since baseline (Table 2). The mean age at follow-up for patients with a new fracture was 35.6 years (SD 14.7) versus 28.1 years (SD 8.8) for patients with no fracture (not statistically significant but lacked power). One patient had a fracture at baseline that was not apparent at follow-up (two grade 0.5 fractures were noted instead of one grade 1 and one grade 0.5 as at baseline). Thus, at follow-up, the overall rate of at least one Grade 1 vertebral fracture (both incident and prevalent) increased to 21.3% of patients (10/47; Table 2).
During the study period, 14 of 47 (30%) patients had taken oral corticosteroids. The mean cumulative dose per patient was 1517 mg and the mean cumulative number of days taking oral corticosteroids was 37 (SD 21.3). One of these patients taking corticosteroids had a new incident fracture (cumulative corticosteroid dose of 3000 mg over 68 days) and the remainder had no prevalent or incident fractures. Three patients were taking a bisphosphonate; none had a prevalent or incident fracture. The rate of inhaled steroid use and Vitamin D supplementation at baseline was higher in the fracture group, however we likely lacked power to see a statistical difference (Table 1). Only two patients were taking calcium supplementation at baseline, although patients may have been taking a multivitamin and dietary calcium levels were monitored by the clinic nutritionist (results not available).
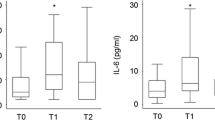
Bone mineral density
Table 3 presents mean BMD values in g/cm2 and T-or Z-scores (lumbar spine, proximal femur, and whole body sites) for all DXA measures during the study period (up to five for some patients). The mean BMD T-or Z-scores at baseline were -0.80 (SD 1.1) at the lumbar spine, -0.57 (SD 0.97) at the proximal femur, and -0.71 (SD 1.1) at the whole body. During the study period, 35 of 49 patients had at least two DXA scans; for these patients, the mean BMD percent change/year (adjusted) is presented in Table 4. Over a mean follow-up of 4.03 years (SD 1.45), the overall rate of bone loss was -0.73% at the lumbar spine, -1.93% at the proximal femur, and -0.40% at the whole body. One outlier who had a BMD change of +12%/year was left out of the lumbar spine analysis (the result was attributed to growth stage and a significant increase in BMI).
Although we did not have adequate sample size to make a meaningful comparison, we examined the longitudinal BMD change for patients who had a final DXA scan that was within one year of the follow-up chest radiograph (over 80% were performed within the same month). At the whole body, the crude mean percent BMD change over a mean follow-up of 4.1 years was -3.62% (SD 3.46) for fracture patients (incident or prevalent; N = 5), and -1.90% (SD 3.34) for non-fracture patients (N = 22). Correspondingly, at the lumber spine it was -3.69% (SD 8.21) for fracture patients (N = 5) and -1.01% (SD 4.59) for non-fracture patients (N = 23). At the proximal femur (average of right and left), it was -6.04 (SD 12.1) for fracture patients (N = 5) and -2.32 (SD 7.68) for non-fracture patients (N = 23).
Discussion
This study demonstrates that the prevalence of vertebral fracture in young adults (mean age 25.2, SD 9.4) with CF and without lung transplantation is similar to Canadian population-based rates of vertebral fracture in men and women over age 50 [24]. In the Canadian Multicentre Osteoporosis Study (CaMos), vertebral fracture rates in Canadians over age 50 were 21.5% for men and 23.5% for women. In our CF cohort, the overall rate of at least one vertebral fracture (prevalent and incident) at follow-up was 21.3% and multiple fractures occurred in four of these patients. The incidence of vertebral fractures over a mean follow-up of 3.3 years was 8.5% (10/47). Considering that the patients in our study were on average 25 plus years younger than CaMos participants, and that the CaMos study uses quantitative morphometry which may yield a higher estimate than the semi-quantitative approach (approximately double by one estimate) [25], the rate of vertebral fractures in adults with CF appears high.
Patients with vertebral fracture were significantly older than their non-fracture counterparts (Table 1). Males with vertebral fractures had a greater BMI than those without fractures, although the mean BMI of both groups were in the healthy range.
Previous cross-sectional studies in CF patients with varied disease severity have found vertebral fracture rates of 17% to 26% [26, 27]. In a cohort of late-stage cystic fibrosis patients referred for lung transplantation, a review of chest radiographs revealed that 51% of patients had one or more unreported vertebral compression fractures (>20% anterior wedging), and 15% of patients had unreported rib fractures [28, 29].
Two recent cross-sectional studies of CF cohorts similar to our study (i.e. general, non-transplant), have also examined vertebral fractures in relation to BMD. A Canadian study [21] and Italian study [20] found a 7% and 27% vertebral fracture rate, respectively. In the former study, cross-sectional BMD was not related to fracture prevalence, and in the latter, cross-sectional BMD was actually higher in the fracture group. Although we were not able to adequately examine this issue due to small sample size, our data suggests that during the study period the crude rate of BMD loss was greater in the fracture than non-fracture group. Whether BMD loss (versus cross-sectional BMD) is predictive of fracture should be evaluated in a future longitudinal study.
In the general population, once peak bone mass has been reached, the rate of bone loss tends to be somewhat stable with age until the fifth and sixth decades [30]. In our cohort of young adults, we found moderate declines (i.e. -0.73, -1.93, -0.40 percent BMD change, adjusted) in bone loss at the lumbar spine, proximal hip, and whole body in both fracture and non-fracture patients over 4-years of follow-up. Our results exhibit a similar trend to Haworth et al. [31] who examined percent change in BMD over a 1-year follow-up. In that study, annual bone loss occurred particularly for adults >25 years (N = 57), where a decline of -1.9% and -1.5% occurred at the femoral neck and total hip (no loss was observed at the lumbar spine).
Bone quality as opposed to simply quantity or mass, and its relationship to fractures, requires further examination in CF patients. Increasingly, an emphasis on bone quality is emerging in osteoporosis research [32], and this may prove to be a particularly relevant topic to CF patients. BMD as measured by DXA may not adequately predict fracture risk in CF patients [20, 21]. Quantitative ultrasound (QUS) is another alternative that provides information on the structural organization of bone in addition to bone mass. QUS may be particularly applicable for patients with reduced bone quality such as patients with corticosteroid induced osteoporosis [33]. In a population-based, epidemiological study (men and women age 42–82 years), QUS of the calcaneum has also been shown to predict fracture risk [34].
Recently, Rossini et al. [35] examined whether QUS could discriminate between adult CF patients with and without vertebral fractures. In the cohort of 172 CF patients, mean age of 27 years, 44% were previously or currently taking oral corticosteroids. Approximately 1 in 3 patients had a vertebral deformity. Overall, only phalangeal QUS as opposed to calcaneal QUS or DXA measures were able to discriminate between patients with and without vertebral fractures. Thus, the hypothesis that CF patients have qualitative alterations in bone, which may be independent of BMD, appears warranted and requires further study.
Our study is limited by a number of factors. We relied on retrospective clinic data extending over a number of years. DXA scans and chest radiographs were considered coincident provided they were performed within one year of each other (however over 80% were within 1-month). The ages of the subjects in our study ranged from 15 to 51 years, with a median age of 23. Thus, both young and middle-aged adults were included, whose clinical and bone-related characteristics may differ.
One patient in our study had a grade 1 fracture indicated at baseline but not on the follow-up radiograph (instead it was graded 0.5). This is a potential problem of Genant's semi-quantitative method used in this study [22, 23]. Although this method is probably the most widely cited in osteoporosis studies, it depends on the recognition of the radiological signs of fracture by experienced observers [25]. There is considerable debate regarding the level of deformity and accuracy of reporting, particularly that with Genant's method the separation of the grades is not explicit [25]. Grade 1 is considered a fracture as per Genant's method; grade 0. 5 is an observable deformity but represents a reduction in height or area less than the criterion for fracture.
Conclusion
Recent studies have examined bisphosphonates for the treatment of low bone mass in CF patients, demonstrating a substantial improvement in BMD after one year [36, 37]. Future studies should examine whether bisphosphonate or other treatment in CF patients also produces a consequent reduction in vertebral (and non-vertebral) fractures. Given the high rate of vertebral fractures noted in CF patients, and the potential negative impact they have on compromised lung functioning, regular screening for vertebral fractures should be considered on routine chest radiographs.
References
Aris RM, Merkel PA, Bachrach LK, Borowitz DS, Boyle MP, Elkin SL, Guise TA, Hardin DS, Haworth CS, Holick MF, Joseph PM, O'Brien K, Tullis E, Watts NB, White TB: Guide to bone health and disease in cystic fibrosis. J Clin Endocrinol Metab. 2005, 90: 1888-1896. 10.1210/jc.2004-1629.
Hecker TM, Aris RM: Management of osteoporosis in adults with cystic fibrosis. Drugs. 2004, 64: 133-147. 10.2165/00003495-200464020-00002.
Haworth CS, Selby PL, Webb AK, Martin L, Elborn JS, Sharples LD, Adams JE: Inflammatory related changes in bone mineral content in adults with cystic fibrosis. Thorax. 2004, 59: 613-617. 10.1136/thx.2003.012047.
Yankaskas JR, Marshall BC, Sufian B, Simon RH, Rodman D: Cystic fibrosis adult care: consensus conference report. Chest. 2004, 125: 1S-39S. 10.1378/chest.125.1_suppl.1S.
Ionescu AA, Nixon LS, Evans WD, Stone MD, Lewis-Jenkins V, Chatham K, Shale DJ: Bone density, body composition, and inflammatory status in cystic fibrosis. Am J Respir Crit Care Med. 2000, 162: 789-794.
Papaioannou A, Watts NB, Kendler DL, Yuen CK, Adachi JD, Ferko N: Diagnosis and management of vertebral fractures in elderly adults. Am J Med. 2002, 113: 220-228. 10.1016/S0002-9343(02)01190-7.
Black DM, Arden NK, Palermo L, Pearson J, Cummings SR: Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1999, 14: 821-828. 10.1359/jbmr.1999.14.5.821.
Hasserius R, Karlsson MK, Nilsson BE, Redlund-Johnell I, Johnell O: Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int. 2003, 14: 61-68. 10.1007/s00198-002-1316-9.
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, Berger M: Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000, 15: 721-739. 10.1359/jbmr.2000.15.4.721.
Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, Licata A, Benhamou L, Geusens P, Flowers K, Stracke H, Seeman E: Risk of new vertebral fracture in the year following a fracture. JAMA. 2001, 285: 320-323. 10.1001/jama.285.3.320.
Ross PD, Genant HK, Davis JW, Miller PD, Wasnich RD: Predicting vertebral fracture incidence from prevalent fractures and bone density among non-black, osteoporotic women. Osteoporos Int. 1993, 3: 120-126. 10.1007/BF01623272.
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA: Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999, 353: 878-882. 10.1016/S0140-6736(98)09075-8.
Cooper C, Atkinson EJ, Jacobsen SJ, O'Fallon WM, Melton LJ: Population-based study of survival after osteoporotic fractures. Am J Epidemiol. 1993, 137: 1001-1005.
Jalava T, Sarna S, Pylkkanen L, Mawer B, Kanis JA, Selby P, Davies M, Adams J, Francis RM, Robinson J, McCloskey E: Association between vertebral fracture and increased mortality in osteoporotic patients. J Bone Miner Res. 2003, 18: 1254-1260. 10.1359/jbmr.2003.18.7.1254.
Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B: Excess mortality after hospitalisation for vertebral fracture. Osteoporos Int. 2004, 15: 108-112. 10.1007/s00198-003-1516-y.
Adachi JD, Ioannidis G, Olszynski WP, Brown JP, Hanley DA, Sebaldt RJ, Petrie A, Tenenhouse A, Stephenson GF, Papaioannou A, Guyatt GH, Goldsmith CH: The impact of incident vertebral and non-vertebral fractures on health related quality of life in postmenopausal women. BMC Musculoskelet Disord. 2002, 3: 11-10.1186/1471-2474-3-11.
Cockerill W, Lunt M, Silman AJ, Cooper C, Lips P, Bhalla AK, Cannata JB, Eastell R, Felsenberg D, Gennari C, Johnell O, Kanis JA, Kiss C, Masaryk P, Naves M, Poor G, Raspe H, Reid DM, Reeve J, Stepan J, Todd C, Woolf AD, O'Neill TW: Health-related quality of life and radiographic vertebral fracture. Osteoporos Int. 2004, 15: 113-119. 10.1007/s00198-003-1547-4.
Hallberg I, Rosenqvist AM, Kartous L, Lofman O, Wahlstrom O, Toss G: Health-related quality of life after osteoporotic fractures. Osteoporos Int. 2004, 15: 834-841. 10.1007/s00198-004-1622-5.
Silverman SL, Minshall ME, Shen W, Harper KD, Xie S: The relationship of health-related quality of life to prevalent and incident vertebral fractures in postmenopausal women with osteoporosis: results from the Multiple Outcomes of Raloxifene Evaluation Study. Arthritis Rheum. 2001, 44: 2611-2619. 10.1002/1529-0131(200111)44:11<2611::AID-ART441>3.0.CO;2-N.
Rossini M, Del MA, Dal SF, Gatti D, Braggion C, James G, Adami S: Prevalence and correlates of vertebral fractures in adults with cystic fibrosis. Bone. 2004, 35: 771-776. 10.1016/j.bone.2004.05.009.
Stephenson A, Jamal S, Dowdell T, Pearce D, Corey M, Tullis E: Prevalence of vertebral fractures in adults with cystic fibrosis and their relationship to bone mineral density. Chest. 2006, 130: 539-544. 10.1378/chest.130.2.539.
Genant HK, Li J, Wu CY, Shepherd JA: Vertebral fractures in osteoporosis: a new method for clinical assessment. J Clin Densitom. 2000, 3: 281-290. 10.1385/JCD:3:3:281.
Genant HK, Jergas M: Assessment of prevalent and incident vertebral fractures in osteoporosis research. Osteoporos Int. 2003, 14 (Suppl 3): S43-S55.
Jackson SA, Tenenhouse A, Robertson L: Vertebral fracture definition from population-based data: preliminary results from the Canadian Multicenter Osteoporosis Study (CaMos). Osteoporos Int. 2000, 11: 680-687. 10.1007/s001980070066.
Lentle BC, Brown JP, Khan A, Leslie WD, Levesque J, Lyons DJ, Siminoski K, Tarulli G, Josse RG, Hodsman A: Recognizing and reporting vertebral fractures: reducing the risk of future osteoporotic fractures. Can Assoc Radiol J. 2007, 58: 27-36.
Conway SP, Morton AM, Oldroyd B, Truscott JG, White H, Smith AH, Haigh I: Osteoporosis and osteopenia in adults and adolescents with cystic fibrosis: prevalence and associated factors. Thorax. 2000, 55: 798-804. 10.1136/thorax.55.9.798.
Elkin SL, Fairney A, Burnett S, Kemp M, Kyd P, Burgess J, Compston JE, Hodson ME: Vertebral deformities and low bone mineral density in adults with cystic fibrosis: a cross-sectional study. Osteoporos Int. 2001, 12: 366-372. 10.1007/s001980170104.
Aris RM, Renner JB, Winders AD, Buell HE, Riggs DB, Lester GE, Ontjes DA: Increased rate of fractures and severe kyphosis: sequelae of living into adulthood with cystic fibrosis. Ann Intern Med. 1998, 128: 186-193.
Aris RM, Lester GE, Renner JB, Winders A, Denene BA, Lark RK, Ontjes DA: Efficacy of pamidronate for osteoporosis in patients with cystic fibrosis following lung transplantation. Am J Respir Crit Care Med. 2000, 162: 941-946.
Heaney RP, Abrams S, wson-Hughes B, Looker A, Marcus R, Matkovic V, Weaver C: Peak bone mass. Osteoporos Int. 2000, 11: 985-1009. 10.1007/s001980070020.
Haworth CS, Selby PL, Horrocks AW, Mawer EB, Adams JE, Webb AK: A prospective study of change in bone mineral density over one year in adults with cystic fibrosis. Thorax. 2002, 57: 719-723. 10.1136/thorax.57.8.719.
Licata AA: Clinical perspectives on bone quality in osteoporosis: effects of drug therapy. Drugs Aging. 2007, 24: 529-535. 10.2165/00002512-200724070-00001.
Daens S, Peretz A, de MV, Moris M, Bergmann P: Efficiency of quantitative ultrasound measurements as compared with dual-energy X-ray absorptiometry in the assessment of corticosteroid-induced bone impairment. Osteoporos Int. 1999, 10: 278-283. 10.1007/s001980050227.
Khaw KT, Reeve J, Luben R, Bingham S, Welch A, Wareham N, Oakes S, Day N: Prediction of total and hip fracture risk in men and women by quantitative ultrasound of the calcaneus: EPIC-Norfolk prospective population study. Lancet. 2004, 363: 197-202. 10.1016/S0140-6736(03)15325-1.
Rossini M, Viapiana O, Del MA, de TF, Gatti D, Adami S: Quantitative ultrasound in adults with cystic fibrosis: correlation with bone mineral density and risk of vertebral fractures. Calcif Tissue Int. 2007, 80: 44-49. 10.1007/s00223-006-0117-0.
Aris RM, Lester GE, Caminiti M, Blackwood AD, Hensler M, Lark RK, Hecker TM, Renner JB, Guillen U, Brown SA, Neuringer IP, Chalermskulrat W, Ontjes DA: Efficacy of alendronate in adults with cystic fibrosis with low bone density. Am J Respir Crit Care Med. 2004, 169 (1): 77-82. 10.1164/rccm.200307-1049OC.
Papaioannou A, Kennedy CC, Freitag A, Ioannidis G, O'Neill J, Webber C, Pui M, Berthiaume Y, Rabin HR, Paterson N, Jeanneret A, Matouk E, Villeneuve J, Nixon M, Adachi JD: Alendronate Once Weekly for the Prevention and Treatment of Bone Loss in Canadian Adult Cystic Fibrosis Patients (CFOS Trial). Chest. 2008
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2474/9/125/prepub
Acknowledgements
We thank Annette Wilkins and Janet Pritchard for their assistance with preparing this manuscript for submission, and Kristina Vinson for her assistance with data collection.
This study was funded by the Ontario Thoracic Society.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Alexandra Papaioannou:
Consulting Role: Amgen, Eli Lilly, Merck Frosst, Novartis, Proctor & Gamble, sanofi aventis
Clinical Trials: Eli Lilly, Merck, Novartis, Proctor & Gamble, sanofi-aventis
Jonathan D. Adachi:
Consulting Role: Amgen; Astra Zeneca, Eli Lilly; GlaxoSmithKline; Merck Frosst; Novartis; Proctor & Gamble; Roche; Sanofi Aventis; Servier
Clinical Trials: Eli Lilly; GlaxoSmithKline; Merck; Novartis; Pfizer; Proctor & Gamble; sanofi-aventis; Servier; Wyeth-Ayerst
Courtney Kennedy: none to declare
Andreas Freitag: none to declare
John O'Neill: none to declare
Margaret Pui: none to declare
Colin Webber: none to declare
Anjali Pathak: none to declare
Suzanne Hansen: none to declare
Rosamund Hennessey: none to declare
George Ioannidis: none to declare
Authors' contributions
AP and CK contributed to concept and design of study, analysis and interpretation; and preparation of the manuscript. AF, GI, JA, CW, JO, and MP contributed to concept and design of study, analysis and interpretation; and editing the final manuscript. AP, SH, and RH contributed to concept and design of study, patient recruitment, data collection, and editing the final manuscript. All authors gave final approval to the article submitted.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Papaioannou, A., Kennedy, C.C., Freitag, A. et al. Longitudinal analysis of vertebral fracture and BMD in a Canadian cohort of adult cystic fibrosis patients. BMC Musculoskelet Disord 9, 125 (2008). https://doi.org/10.1186/1471-2474-9-125
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2474-9-125